Abstract
Objective
To evaluate the impact of intrauterine insemination timing performed 24 or 36 h later following ovulation trigger on clinical pregnancy rate during ovulation induction with clomiphene citrate among infertile women was the objective of this study.
Methods
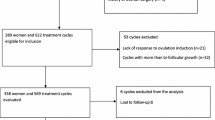
The medical records of 280 infertile patients who have underwent ovulation induction by using clomiphene citrate have been evaluated and cycle outcomes of the patients have been investigated specifically based on the timing of intrauterine insemination during the treatment cycle.
Results
The clinical pregnancy rate of the study group based on the timing of intrauterine insemination (24 vs. 36 h following hCG trigger) was found to be similar regardless of infertility type. The cycle day of which hCG trigger has been performed was found to be significantly longer for patients who have achieved clinical pregnancy than patients who have not got pregnant following the treatment cycle. Dominant follicle diameter has not been found to affect clinical pregnancy rate during treatment cycles with clomiphene citrate.
Conclusions
In this study, intrauterine insemination timing did not affect the cycle outcomes whether the procedure has been performed 24 or 36 h later following ovulation trigger with exogenous hCG utilization. The longer period of treatment cycle during ovulation induction with clomiphene citrate resulted with higher clinical pregnancy rate. Intrauterine insemination can be done successfully at either 24 or 36 h after hCG in clomiphene citrate stimulated cycles. This will allow more flexibility and convenience for both physicians and patients, especially during weekends.
Similar content being viewed by others
Background
Controlled ovarian stimulation (COS) with intrauterine insemination (IUI) is a widely used fertility treatment for couples to improve pregnancy rates with mild male factor, unexplained infertility, cervical factor, anovulation, minimal and mild endometriosis (Goverde et al. 2000). It is simple, relatively less invazive and expensive procedure than other forms of assisted reproductive technologies (Dodson and Haney 1991).
Many different time intervals have been suggested in ovulation induction cycles after hCG injection for the management of infertility so there has been uncertainty in the correct timing of insemination. In 1970’s Edwards and Steptoe showed that ovulation began at 36–38 h after an injection of hCG if the follicular development was adequate (Edwards and Steptoe 1974). However Yang et al. showed that intrauterine insemination can be done at any time between 1 and 48 h after hCG injection without affecting significantly pregnancy outcomes. This flexibility in COH-IUI cycles provides more convenience for both patients and clinic staff, especially during weekends (Yang et al. 2008). According to World Health Organization (WHO) analysis, ovulation occurs from 24 to 56 h after the onset of the LH surge, with a mean time of 32 h (World Health Organization 1980). However the surveillance of sperm in the cervix is up to 80 h after intercourse (Gould et al. 1984). A 2010 systematic review of trials that evaluated the effectiveness of different synchronization methods in stimulated and natural cycles for IUI in subfertile couples concluded the choice should be based on hospital facilities, medical staff, convenience for the patient, costs and drop-out levels as no method was clearly superior to another (Cantineau et al. 2010).
In this study, we aimed to evaluate the impact of IUI timing on pregnancy rates in clomiphene citrate/IUI cycles.
Methods
The protocol for the research project has been approved by the Ethics Committee of Zekai Tahir Burak Women’s Health Education and Research Hospital within which the work was undertaken and it conforms to the provisions of the Declaration of Helsinki (as revised in Tokyo 2004). The medical records of 280 infertile patients who have demonstrated at least one patent fallopian tube on hysterosalpingography and whose partners had normal spermiogram analysis results based on World Health Organization (WHO) 2010 criteria have been reviewed after excluding patients with endometriosis, medical comorbidities and hormonal disturbances. All patients have received clomiphene citrate treatment (50–150 mg/day orally starting on 3–5 cycle day of menstruation and lasting on 7–9 cycle days of menstruation) for ovulation induction followed by one intrauterine insemination procedure performed on 24 or 36 h after ovulation trigger by exogenous 10,000 IU intramuscular urinary hCG injection upon detection of a mature follicle with ≥17 mm diameter. Selection of daily dose of CC was decided by regarding the lowest effective dose which induces at least one dominant follicle during ovulation induction. The IUI attempts of the whole study group was ≤6 and ≤3 for PCOS and unexplained infertile patients respectively due to the ovulation induction policy of our institution by using oral CC treatment. The demographic features, infertility types, dominant follicle number, endometrial thickness on hCG day, hCG type (recombinant or urinary derived hCG) timing of intrauterine insemination and clinical pregnancy rates of the patients have been evaluated. Following the IUI procedures, the patients have not received vaginal progesterone supplementation for luteal support. A clinical pregnancy was defined as the presence of a gestational sac with accompanying fetal heartbeat by ultrasound at least 4 weeks after IUI. Statistical analysis was performed by using IBM SPSS Statistics Software (17.0, SPSS Inc., Chicago, IL, USA). Kolmogorov–Smirnov test has been used for evaluating the normality of the distributions of continuous variables. The parametric results were presented as mean ± standard deviation values and normal distributed values were compared by using the independent samples t test. Comparison of nonparametric data and parametric data without normal distribution have been made by using Mann–Whitney U test. Categorical variables were compared with Fisher’s exact or Pearson Chi square tests. p values <0.05 were considered statistically significant.
Results
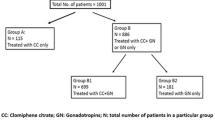
The age, basal (cycle day 3) FSH, mean mature follicle number and infertility duration was found as 26.4 ± 4.9, 6.6 ± 1.6, 1.55 ± 0.6 and 3.3 ± 2.0, respectively. Thirty-nine percent of the patients (N:110) have been diagnosed as polycystic ovary syndrome (PCOS) and 61 % of the patients (N:170) have been diagnosed as unexplained infertile. Clinical pregnancy rate per cycle was 12.7 % for PCOS patients and 11.2 % for unexplained infertile patients (p:0.69). The clinical pregnancy rate of the study group based on the timing of intrauterine insemination (24 vs. 36 h following hCG trigger) was found to be similar regardless of infertility type (p:0.97). Receiver Operating Characteristic (ROC) analysis of the mature follicle diameter and clinical pregnancy rate was found to be statistically nonsignificant (ROC AUC:0.48; p:0.79) (Fig. 1). The cycle day of which hCG trigger has been performed was found to be longer for patients who have achieved clinical pregnancy than patients who have not got pregnant following the treatment cycle (mean cycle day number: 14.1 ± 2.9 vs. 13.3 ± 2.5; ROC AUC:0.59; p:0.01) (Fig. 2).
Discussion
Intrauterine insemination with controlled ovarian hyperstimulation has been used over the years, as a treatment for mild male factor, anovulation and unexplained infertility (Goverde et al. 2000; Guzick et al. 1999). The time of administration of intrauterine insemination is the most critical factor. Regimens vary between centers and also between clinicians. Hence the correct timing of insemination to improve pregnancy is recently a debated issue.
Pryor et al. showed an improved pregnancy rate when IUI was performed with a time interval of 38–40 h (60 % pregnancy rate) as compared to shorter IUI interval (0 % pregnancy rate) after hCG. However, the small number of patients and the different sperm preparation techniques used between the two groups were the main limitations of the study. While 54 % of patients in the 38–40 h group had sperm prepared with a sperm swim-up technique, only 13 % of those in the 32–34 h group had this type of sperm preparation. Also the males in the Pryor study were all with spinal cord injury and had sperm recovered via vibratory stimulation. The sperm counts were low and the sperm preparation techniques may have been more of a deciding factor than was the timing of the IUI and may have accounted for the difference in pregnancy rates (Pryor et al. 2001).
There are some important factors affecting the outcome of COH-IUI. These factors include female age, tube malfunction, duration of infertility, endometrial thickness, number of mature follicles, various techniques of semen preparation, sperm motility and concentration (Campana et al. 1996; Duran et al. 2002; Khalil et al. 2001; Demir et al. 2011; Tomilson et al. 1996). In our study, we found no significant difference with respect to these parameters affecting the outcome among the groups. Also there was no relationship between the average mature follicle size and clinical pregnancy outcomes (ROC AUC:0.48; p:0.79). In this study, we have demonstrated that the longer the treatment cycle with clomiphene citrate, the higher the clinical pregnancy rate. This result could have been related to the delayed maturity of dominant follicles during clomiphene citrate treatment cycles. Patiently waiting for later hCG trigger during ovulation induction with CC followed by intrauterine insemination or detection of spontaneous LH surge on urine LH ovulation kit can potentially increase the clinical pregnancy rates regardless of the timing of intrauterine insemination.
Robb et al. (2004) showed no significant difference in pregnancy outcomes between IUIs performed at 24 versus 36 h after hCG with 182 clomiphene citrate/IUI cycles in 90 women. However the small numbers, low overall pregnancy rates and inclusion of various causes of female infertility diagnosis, including poor ovarian reserve, anovulatory, unexplained, anatomic, male factor are the possible weaknesses of the retrospective study. In our study the patients were divided in two groups. One hundred and ten (39 %) patients were polycystic ovary and one hundred and seventy (61 %) patients were unexplained. To homogenize the study groups, we excluded other possible causes of infertility. Clinical pregnancy rates per cycle was 12.7 % in PCOS group and 11.2 % was in unexplained group (p:0.69). There was also no significant difference in pregnancy outcomes whether hCG was administered at 24 or 36 h prior to IUI in clomiphene citrate stimulated cycles in both groups (p:0.97). Our results were consistent with Lewis, Wang and Claman’s (Lewis et al. 2006; Claman et al. 2004). In an other study, Ragni et al. (2004) showed significant increases in pregnancy rates when intrauterine insemination was performed during the preovulatory and periovulatory periods, but not the postovulatory period. In a retrospective study, Xu et al. have concluded that the female age, infertile duration, ovarian stimulation and follicle number, cause of infertility were the main factors affecting clinical pregnancy outcome. In the same study, the sperm density, and cycle numbers have been found to influence pregnancy outcome too but the insemination timing, and frequency have been found to exert little effect (Xu et al. 2013). In a prospective randomized trial, Rahman et al. (2010) have evaluated the clinical efficacy of double IUI over single IUI and no benefit of double IUI has been detected among unexplained infertile patients. Although the best application time and frequency for IUI procedures have not been detected, longer survival period of spermatozoa within the female genital tract, unlike oocyte, result with broader time interval preferences for successful IUI procedures. Future studies are needed for clarifying the best timing for IUI procedures to enhance pregnancy rates following ovulation induction.
To conclude, our data showed intrauterine insemination can be done successfully at either 24 or 36 h after hCG in clomiphene citrate stimulated cycles. This will allow more flexibility and convenience for both physicians and patients, especially for unnecessary obligation to perform IUI procedures on weekends.
Conclusion
In this study, our data showed intrauterine insemination timing did not affect the cycle outcomes whether the procedure has been performed 24 or 36 h later following ovulation trigger with exogenous hCG utilization. The longer period of treatment cycle during ovulation induction with clomiphene citrate resulted with higher clinical pregnancy rate. Intrauterine insemination can be done successfully at either 24 or 36 h after hCG in clomiphene citrate stimulated cycles. This will allow more flexibility and convenience for both physicians and patients, especially during weekends.
References
Campana A, Sakkas D, Stalberg A, Bianchi PG, Comte I, Pache T et al (1996) Intrauterine insemination: evaluation of the results according to the woman’s age, sperm quality, total sperm count per insemination and life table analysis. Hum Reprod 11:732–736
Cantineau AE, Janssen MJ, Cohlen BJ (2010) Synchronised approach for intrauterine insemination in subfertile couples. Cochrane Database Syst Rev (4):CD006942. doi:10.1002/14651858.CD006942.pub2
Claman P, Wilkie V, Collins D (2004) Timing intrauterine insemination either 33 or 39 hours after administration of human chorionic gonadotropin yields the same pregnancy rates as after superovulation therapy. Fertil Steril 82(1):13–16
Demir B, Dilbaz B, Cinar O, Karadag B, Tasci Y, Kocak M et al (2011) Factors affecting pregnancy outcome of intrauterine insemination cycles in couples with favourable female characteristics. J Obstet Gynaecol 31(5):420–423
Dodson WC, Haney AF (1991) Controlled ovarian hyperstimulation and intrauterine insemination for treatment of infertility. Fertil Steril 55:457–467
Duran HE, Morshedi M, Kruger T, Oehninger S (2002) Intrauterine insemination, a systematic review on determinants of success. Hum Reprod Update 8(4):373–384
Edwards RG, Steptoe PC (1974) Control of human ovulation, fertilization and implantation. Proc R Soc Med 67(9):932–935
Gould JE, Overstreet JW, Hanson FW (1984) Assessment of human sperm function after recovery from the female reproductive tract. Biol Reprod 31:888–894
Goverde AJ, McDonnell J, Vermeiden JP, Schats R, Rutten FF, Schoemaker J (2000) Intrauterine insemination or in vitro fertilisation in idiopathic subfertility and male subfertility: a randomised trial and cost-effectiveness analysis. Lancet 355(9197):13–18
Guzick DS, Carson SA, Coutifaris C, Overstreet JW, Factor-Litvak P, Steinkampf MP et al (1999) Efficacy of superovulation and intrauterine insemination in the treatment of infertility. N Engl J Med 340:177–183
Khalil MR, Rasmussen PE, Erb K, Laursen SB, Rex S, Westergaard LG (2001) Homologous intrauterine insemination: an evaluation of prognostic factors based on a review of 2473 cycles. Acta Obstet Gynecol Scand 80:74–81
Lewis V, Queenan J Jr, Hoeger K, Stevens J, Guzick DS (2006) Clomiphene citrate monitoring for intrauterine insemination timing: arandomized trial. Fertil Steril 85(2):401–406
Pryor JL, Kuneck PH, Blatz SM, Thorp C, Cornwell MT, Carrell DT (2001) Delayed timing of intrauterine insemination results in a significantly improved pregnancy rate in female partners of quadriplegic men. Fertil Steril 76:1130–1135
Ragni G, Somigliana E, Vegetti W (2004) Timing of intrauterine insemination: where are we? Fertil Steril 82(1):25–26
Rahman SM, Malhotra N, Kumar S, Roy KK, Agarwal A (2010) A randomized controlled trial comparing the effectiveness of single versus double intrauterine insemination in unexplained infertility. Fertil Steril 94(7):2913–2915. doi:10.1016/j.fertnstert.2010.06.082 (Epub 2010 Aug 1)
Robb PA, Robins JC, Thomas MA (2004) Timing of hCG administration does not affect pregnancy rates in couples undergoing intrauterine insemination using clomiphene citrate. J Natl Med Assoc 96(11):1431–1433
Tomilson MJ, Amissah-Arthur JB, Thompson KA, Kasraie JL, Bentick B (1996) Prognostic indicators for IUI: statistical model for IUI success. Hum Reprod 11(9):1892–1896
World Health Organization (1980) Temporal relationships between ovulation and defined changes in the concentration of plasma 17-β-estradiol, luteinizing hormone, follicle-stimulating hormone and progesterone. Am J Obstet Gynecol 138:383–390
Xu YY, Wang HY, Qiao J, Liu P, Chen XN, Ma CH et al (2013) Analysis of clinical factors affecting pregnancy rate of intrauterine insemination. Beijing Da Xue Xue Bao 45(6):887–891
Yang F, Jin H, Zhu LP (2008) Timing of IUI treatment after hCG administration 1–48 h affecting pregnancy rate. J Reprod Contrac 19(3):147–151
Authors’ contributions
OHY and SK made substantial contributions in writing and revising the manuscript. MKP, EI and SO made substantial contributions to acquisition, analysis and interpretation of data. MNC, YT and SE made substantial contributions to conception, design and final approval of the version to be published. All authors read and approved the final manuscript.
Acknowledgements
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. We, as authors of this original research study, disclose that we do not have any financial and personal relationships with other people or organizations that could inappropriately influence our work.
Competing interests
The authors declare that they have no competing interests.
Human and animal rights and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yumusak, O.H., Kahyaoglu, S., Pekcan, M.K. et al. Which is the best intrauterine insemination timing choice following exogenous hCG administration during ovulation induction by using clomiphene citrate treatment? A retrospective study. SpringerPlus 5, 1307 (2016). https://doi.org/10.1186/s40064-016-2992-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2992-9