Abstract
Purpose
This study aimed to identify the surgical-pathologic risk factors of lymph node metastasis (LNM) in patients with early stage squamous cell cervical cancer and to evaluate the potential efficacy of omitting pelvic lymphadenectomy.
Methods
A total of 276 patients with stage IA2, IB1, and IIA1 squamous cell cervical cancer receiving primary radical hysterectomy with pelvic lymphadenectomy were included in this study.
Results
The incidences of LNM in patients with stage IA2, IB1, and IIA1 squamous cell cervical cancer were 0 % (0/8), 17.4 % (36/207), and 29.5 % (18/61), respectively. The most common location of LNM was the obturator lymph node. Human papilloma virus 16 subtype was the most common infection in early stage squamous cell cervical cancer. Univariate analysis revealed that squamous cell carcinoma antigen (SCCAg) greater than 1.5 μg/L (p < 0.001), tumor size greater than 2 cm (p < 0.001), tumor size greater than 3 cm (p < 0.001), depth of stromal invasion (p < 0.001) and lymphovascular invasion (p < 0.001) were associated with LNM. Logistic regression analysis revealed that depth of stromal invasion {model 1 [p = 0.006; odds ratio (OR) 2.161; 95 % confidence interval (CI) 1.251–3.734], model 2 [p = 0.002; OR 2.344; 95 % CI 1.337–3.989]}, lymphovascular invasion [model 1 (p = 0.004; OR 2.967; 95 % CI 1.411–6.237), model 2 (p = 0.004; OR 2.978; 95 % CI 1.421–6.243)], and SCCAg greater than 1.5 μg/L [model 1 (p = 0.023; OR 2.431; 95 % CI 1.129–5.235), model 2 (p = 0.024; OR 2.418; 95 % CI 1.125–5.194)] were independently associated with LNM.
Conclusions
Pelvic lymphadenectomy may be omitted in patients with SCCAg lower than 1.5 μg/L, superficial stromal invasion and without lymphovascular invasion in stage IA2, IB1, IIA1 squamous cell cervical cancer.
Similar content being viewed by others
Background
Cervical cancer is a global public health problem and a significant cause of death among women in developing countries (Forouzanfar et al. 2011). The International Federation of Gynecology and Obstetrics (FIGO) recommends a clinical staging system for cervical cancer. Although lymph node status assessment does not change clinical stage, lymph node metastasis (LNM) is an independent factor in poor survival and relapse of cervical cancer (Pieterse et al. 2007; Ditto et al. 2013; Bai et al. 2015). Guidelines recommend radical hysterectomy with pelvic lymphadenectomy is the preferred treatment for early stage (FIGO IA2, IB1, IIA1) cervical cancer. However, pelvic lymphadenectomy is associated with potential risk of serious postoperative complication, such as nerve or vascular injury, lymphedema lymphedema in the lower limbs and pelvic lymph cysts with concomitant infection (Matsuura et al. 2006; Achouri et al. 2013; Kawamura et al. 2015).
One research suggest that the number of removed lymph nodes in pelvic lymphadenectomy pay no effect on the prognosis of patients with early stage cervical cancer with negative pelvic lymph nodes (Pieterse et al. 2007). Approximately 80 % of cervical cancer cases are squamous cell carcinomas. Non-squamous histology has been shown to be an independent prognostic factor for disease-free and overall survival compared with squamous cell carcinoma in cervical cancer with LNM (Kodama et al. 2006; Park et al. 2010). Thus, we speculate that pelvic lymphadenectomy may be avoided in patients with early cervical squamous cell cancer who are in low risk of LNM, to reduce associated morbidity of complete lymphadenectomy and long-term effects of postoperative complication, may help to improve the postoperative quality-of-life of patients.
Squamous cell carcinoma antigen (SCCAg) is the serum tumor marker most commonly used for clinical monitoring of cervical squamous cell cancer(Kim 2013). Elevated pre-treatment SCCAg levels correlate with LNM and a poor prognosis in cervical squamous cell cancer (van de Lande et al. 2009; Kawaguchi et al. 2013).
In the present study, we retrospectively reviewed the records of patients with stage IA2, IB1, and IIA1 cervical squamous cell cancer who received radical hysterectomy with pelvic lymphadenectomy. We examined the effect of clinicopathologic factors, also take preoperative serum SCCAg into account, on the risk for LNM to identify patients with low risk for whom pelvic lymphadenectomy may be omitted.
Methods
Patients
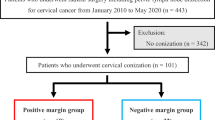
We retrospectively analyzed the data of patients with cervical cancer treated at the Department of Gynecological Oncology, Sun Yat-sen Memorial Hospital of Sun Yat-sen University between January 2012 and June 2015. This study included patients who met the following criteria: (1) FIGO IA2, IB1, or IIA1 cervical cancer and received radical hysterectomy with pelvic lymphadenectomy; (2) histological confirmed squamous cell carcinoma according to FIGO classification system; (3) no preoperative radiotherapy or chemotherapy. The study was performed in accordance with the Declaration of Helsinki and was approved by the ethics committee of the Sun Yat-sen Memorial Hospital of Sun Yat-sen University. All patients provided written consent for storage of their information in the hospital database and for use of this information in our research.
Surgical procedures
Radical hysterectomy included complete removal of the uterus, ovaries, Fallopian tubes, cervix, upper vagina and parametrium. A systematic lymphadenectomy consisted of dissections of lymph nodes in the common iliac, external iliac, internal iliac, obturator and deep inguinal areas, at both sides. The cranial, caudal, ventral, dorsal, lateral and medial boundaries of the lymphadenectomy were 3 cm above the bifurcation of the internal and external iliac arteries, the level of deep iliac circumflex vein, the level of peritoneum, the level of the obturator nerve, the inside of the psoas major muscle and the lateral border of ureter, respectively. Para-aortic lymphadenectomy was performed only in case of gross metastasis to the common iliac nodes or para-aortic nodes was suspected.
SCCAg assay
Serum samples were taken routinely at the patient’s initial visit before surgery for SCCAg analysis. Serum SCCAg levels were analyzed using an automated chemiluminescence immunoassay (CLIA) system (i2000, Abbott, USA) according to the manufacturer’s instructions. The recommended cutoff level of 1.5 ng/ml was applied. Ten patients had no serum SCCAg data.
Sample collection and HPV testing
The gynecologist rotated the disposable cervical cell collection brush clockwise 3–5 times at the cervical junction to collect exfoliated cervical cells. The cervical brush was removed, stored in preservation solution, and sent to laboratory to test immediately. HPV genotypes were detected using nucleic acid molecule flow-through PCR and membrane hybridization using gene chip technology with the 21HPV Genoarray Diagnostic Kit (Hybribio Inc, Guangzhou, China). HPV nucleic acid was extracted, and gene amplification and molecular hybridization were performed, according to the manufacturer’s instructions. There were 21 HPV subtypes tested simultaneously in a membrane including 13 types of high-risk HPVs (HPV-16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68), 5 low-risk HPVs (HPV-6, 11, 42, 43,and 44) and 3 HPVs that are common in Chinese people (HPV-53, 66, and CP8304). Twenty-four patients had no HPV testing data.
Statistical analysis
The relationship between clinical and pathological factors and LNM was examined by univariate analysis using the χ2 and Fisher’s exact probability tests. The independent effects of clinical and pathological factors on LNM were then determined by logistic regression analysis, in which factors that were statistically significant in univariate analysis. A p value <0.05 was considered significant for all analyses. SPSS software (version 16.0; IBM Corporation, Armonk, NY, USA) was used for statistical analysis.
Results
Clinicopathologic characteristics of patients
A total of 276 patients treated for squamous cell cervical cancer between January 2012 and June 2015 met criteria for inclusion in the present study. Table 1 summarizes the clinicopatholgic characteristics of the 276 patients who had early stage cervical squamous cell cancer with a median age of 49 years (range 22–80 years). One hundred and fifty-eight patients (57.2 %) were premenopausal and 118 patients (42.8 %) were postmenopausal. Staging indicated that 8 patients (2.9 %) had FIGO IA2, 207 patients (75.0 %) had FIGO IB1, and 61 patients (22.1 %) had FIGO IIA1. Two hundred and thirty-two patients (92 %) had positive HPV infection and 68 patients (25.6 %) with SCCAg greater than 1.5 μg/L. Analysis of histological grade indicated that 98.5 % patients (272/276) had moderately to poorly differentiated cancer. Seventy-nine patients (28.6 %) had deep-full thickness stromal invasion, and 129 patients (46.7 %) with lymphovascular invasion.
HPV infection
A total of 252 patients had HPV testing data. Two hundred and thirty-two patients (92.1 %) had positive HPV infection. There were 12 HPV subtypes (HPV-16, 18, 31, 33, 39, 51, 52, 56, 58, 66 and CP8304) as detected. Single HPV subtype infections accounted for 81.0 % (188/232) of the total number of infections, and multiple-subtype infections accounted for 19.0 % (44/232), including 14.2 % (33/232) of patients with a double infection, 4.7 % (11/232) of patients with a triple or more infection. The HPV16 subtype was the most common infection (n = 190, 81.9 %), followed by HPV58 (n = 19, 8.3 %), HPV52 (n = 18, 7.9 %), HPV18 (n = 16, 7.1 %), HPV 39 (n = 11, 4.7 %).
Lymph node metastasis
The patterns of lymph node metastasis are summarized in Table 2. The median number of dissected lymph nodes was 23 (range 10–52) (in Fig. 1). Fifty-four patients (19.6 %) had 99 positive lymph node metastasis. The incidences of LNM in patients with stage IA2, IB1, and IIA1 were 0 % (0/8), 17.4 % (36/207), and 29.5 % (18/61), respectively. Multiple (≥2) LNM was found in 10.9 % (30/276). Bilateral LNM was found in 4.7 % (13/276). Skip LNM was found in 1.1 % (3/276). The obturator lymph node was the most common location of lymph node metastasis (n = 50, 50.5 %), followed by the internal iliac lymph node (n = 16, 16.2 %), common iliac lymph node (n = 14, 14.1 %), external iliac lymph node (n = 11, 11.1 %), parametrial lymph node (n = 4, 4.0 %), inguinal lymph node(n = 3, 3.0 %) and para-aortic lymph node(n = 1, 1.0 %).
Univariate analysis of risk factors with LNM
Table 1 shows the results of univariate analysis of the correlation between clinicopathologic factors and LNM. Patients with SCCAg greater than 1.5 μg/L (p < 0.001), tumor size greater than 2 cm (p < 0.001), tumor size greater than 3 cm (p < 0.001), depth of stromal invasion (p < 0.001) and lymphovascular invasion (p < 0.001) were significantly associated with LNM. Age, menopausal status, FIGO stage, HPV infection status and histological grade were not associated with LNM (p > 0.05).
Multivariate analysis of risk factors with LNM
Table 3 shows multivariate analysis of the clinicopathological factors associated with the LNM in which factors that were statistically significant in univariate analysis using 2 models. The results showed that depth of stromal invasion {model 1 [p = 0.006; odds ratio (OR) 2.161; 95 % confidence interval (CI) 1.251–3.734], model 2 [p = 0.002; OR 2.344; 95 % CI 1.337–3.989]}, lymphovascular invasion [model 1 (p = 0.004; OR 2.967; 95 % CI 1.411–6.237), model 2 (p = 0.004; OR 2.978; 95 % CI 1.421–6.243)], and SCCAg greater than 1.5 μg/L [model 1 (p = 0.023; OR 2.431; 95 % CI 1.129–5.235), model 2 (p = 0.024; OR 2.418; 95 % CI 1.125–5.194)] were significantly and independently associated with LNM. Tumor size were not significantly associated with LNM (p > 0.05).
Discussion
In the present study, the incidences of LNM in patients with stage IA2, IB1, and IIA1 cervical squamous cell cancer were 0 % (0/8), 17.4 % (36/207), and 29.5 % (18/61), respectively. The result is similar to the previous studies that LNM in cervical cancer was found in 0–20.3 % of patients with stage IA2-IB1 and in 16–38.6 % of patients with stage IIA1 (Hongladaromp et al. 2014; Togami et al. 2014; Liu et al. 2015; Zhou et al. 2015). In patients without LNM, the number of removed lymph nodes in pelvic lymphadenectomy was not associated with 5-year disease-free survival (Suprasert et al. 2012). But there are some long-term postoperative complication of pelvic lymphadenectomy, the overall incidence of symptomatic postoperative lymphocysts was 34.5 % (Achouri et al. 2013), and the incidence of lower-limb lymphedema increased over time, 12.9 % at 1 year, 20.3 % at 5 years, and 25.4 % at 10 years (Hareyama et al. 2015), both of which significantly harmed the quality-of-life. However, compared to undergoing open surgery, pelvic lymphadenectomy had a less impact on patients undergoing laparoscopic surgery, less blood loss, a lower transfusion rate, less lymphocele infection and other complications (Xiao and Zhang 2015; Bogani et al. 2014). Nevertheless, it means more than 60 % of patients in early stage cervical cancer without LNM will derive no benefit from pelvic lymphadenectomy and that it may be safely avoided in such patients. It is important to identify factors associated with the risk of LNM to reduce unnecessary pelvic lymphadenectomy.
Results of our multivariate analysis suggested that in 276 patients with stage IA2, IB1, and IIA1 cervical squamous cell cancer who received radical hysterectomy with pelvic lymphadenectomy, SCCAg greater than 1.5 μg/L, deep-full thickness stromal invasion and lymphovascular invasion were significant and independent factors for LNM, while tumor size were not significantly associated with LNM (p > 0.05).
Several studies found that lymphovascular invasion, and deep stromal invasion were statistically independently associated with LNM in early stage cervical cancer (Bai et al. 2015; Li et al. 2015; Zhou et al. 2015). One research demonstrated that patients with cervical cancer and found that stage IIA and advanced histological grade increased the risk for LNM (Li et al. 2012). Another also studied patients with stage IA–IIB squamous cell cervical cancer and found lymphovascular invasion, parametrial invasion, and depth of stromal invasion were identified as independent clinicopathological risk factors for LNM (Liu et al. 2015). But they did not analysis the SCCAg data. It had been found that SCCAg greater than 1.65 μg/L can predict LNM more accurately in stage IB1 (76 %) than in stage IIA (53 %) (van de Lande et al. 2009). In our study, SCCAg greater than 1.5 μg/L was significant and independent factors for LNM in stage IA2, IB1, and IIA1 squamous cell cervical cancer.
One prior study by Togami investigated patients with stage IA2-IIB cervical cancer and found that parametrial involvement and primary tumor size greater than 2 cm increased the risk of LNM (Togami et al. 2014). A survey by the Japan Clinical Oncology Group found that in patients with stage IB1 with clinical tumor diameter ≤2 cm, which available by magnetic resonance imaging (MRI) or specimens by cone biopsy, had less LNM and more favorable 5-year overall survival (Kato et al. 2015).As MRI is a more accurate noninvasive modality for preoperative evaluation of tumor size compared with pelvic examination (Zhang et al. 2014), in our study, tumor size which was evaluated by pelvic examination was not an independent factor for LNM.
Sentinel lymph node (SLN) mapping and biopsy has already been used in cervical cancer. A systematic review reported that SLN biopsy has the highest detection rate when 99 mTc is used in combination with blue dye (97 %), and a sensitivity of 92 % (van de Lande et al. 2007). However, the detection of sentinel lymph nodes requires an injection of technetium or blue dye and frozen section analysis. The sensitivities of SLN in diagnosing micrometastases were 81 % and the false negative rate of intra-operative frozen section examination was up to 44 % (Slama et al. 2013), while another study from Canada reported that intra-operative frozen examination of SLN accurately predicts the status of pelvic lymph nodes. The sensitivity for the detection of macro and micrometastatic disease was 88.9 % and negative predictive value was 98.8 % (Martínez et al. 2013). Recently, Indocyanine green (ICG), has been introduced in SLN mapping. A meta-analysis found that ICG SLN mapping had higher overall and bilateral detection rates while compared with blue dyes, and there was no difference while compared with combination of blue dyes and 99mTc (Ruscito et al. 2016). A study from Italy also found that in women with early stage cervical cancer, bilateral mapping was achieved in 98.5 % for ICG and 76.3 % for Tc-99m with blue dye (Buda et al. 2016). Undergoing laparoscopic surgery, ICG SLN mapping in cervical cancer also provided high overall and bilateral detection rates (Imboden et al. 2015). However, compared to patients with uterus in situ, SLN mapping in occult cervical cancer patients has lower detection rates, these patients needed proper management (Papadia et al. 2016). A diagnostic review found that early stage cervical cancer patients (FIGO IA2, IB1, IIA1) who had bilateral negative SLN result had a residual risk of 0.08 % (1/1257) on occult metastases, recommended not to perform a full pelvic lymphadenectomy in these patients (Tax et al. 2015). Further research should be made in order to standardize this method and confirm whether SLN biopsy can be used to replace pelvic lymphadenectomy for patients with early stage cervical cancer.
The retrospective nature of this study is its major limitation. Moreover, it was a single-center study and the sample was small, so our patients should not be considered representative of the general population. However, although SCC-Ag was one preoperative clinicopathologic factor in the prediction of LNM, depth of stromal invasion and lymphovascular invasion was evaluated after conization but mainly on the basis of postoperative factors.
Conclusions
In conclusion, depth of stromal invasion, lymphovascular invasion and SCCAg greater than 1.5 μg/L were risk factors with LNM in patients with stage IA2, IB1, and IIA1 squamous cell cervical cancer. We propose pelvic lymphadenectomy maybe ommitted in patients with superficial stromal invasion, SCCAg lower than 1.5 μg/L and without lymphovascular invasion and thereby reduce the incidence of postoperative complications. More studies are needed to confirm our findings.
Abbreviations
- LNM:
-
lymph node metastasis
- HPV:
-
human papilloma virus
- SCCAg:
-
squamous cell carcinoma antigen
- FIGO:
-
The International Federation of Gynecology and Obstetrics
References
Achouri A, Huchon C, Bats AS, Bensaid C, Nos C, Lécuru F (2013) Complications of lymphadenectomy for gynecologic cancer. Eur J Surg Oncol EJSO 39:81–86
Bai H, Yuan F, Wang H, Chen J, Cui Q, Shen K (2015) The potential for less radical surgery in women with stage IA2–IB1 cervical cancer. Int J Gynecol Obstet 130:235–240
Bogani G, Cromi A, Uccella S, Serati M, Casarin J, Pinelli C, Ghezzi F (2014) Laparoscopic versus open abdominal management of cervical cancer: long-term results from a propensity-matched analysis. J Minim Invas Gyn 21:857–862
Buda A, Papadia A, Zapardiel I et al (2016) From conventional radiotracer Tc-99m with blue dye to indocyanine green fluorescence: a comparison of methods towards optimization of sentinel lymph node mapping in early stage cervical cancer for a laparoscopic approach. Ann Surg Oncol. doi:10.1245/s10434-016-5227-y
Ditto A, Martinelli F, Lo Vullo S, Reato C, Solima E, Carcangiu M, Haeusler E, Mariani L, Lorusso D, Raspagliesi F (2013) The role of lymphadenectomy in cervical cancer patients: the significance of the number and the status of lymph nodes removed in 526 cases treated in a single institution. Ann Surg Oncol 20:3948–3954
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, Naghavi M (2011) Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet 378:1461–1484
Hareyama H, Hada K, Goto K, Watanabe S, Hakoyama M, Oku K, Hayakashi Y, Hirayama E, Okuyama K (2015) Prevalence, classification, and risk factors for postoperative lower extremity lymphedema in women with gynecologic malignancies. Int J Gynecol Cancer 25:751–757
Hongladaromp W, Tantipalakorn C, Charoenkwan K, Srisomboon J (2014) Locoregional spread and survival of stage IIA1 versus stage IIA2 cervical cancer. Asian Pac J Cancer APJCP 15:887–890
Imboden S, Papadia A, Nauwerk M, McKinnon B, Kollmann Z, Mohr S, Lanz S, Mueller MD (2015) A comparison of radiocolloid and indocyanine green fluorescence imaging, sentinel lymph node mapping in patients with cervical cancer undergoing laparoscopic surgery. Ann Surg Oncol 22:4198–4203
Kato T, Takashima A, Kasamatsu T, Nakamura K, Mizusawa J, Nakanishi T, Takeshima N, Kamiura S, Onda T, Sumi T, Takano M, Nakai H, Saito T, Fujiwara K, Yokoyama M, Itamochi H, Takehara K, Yokota H, Mizunoe T, Takeda S, Sonoda K, Shiozawa T, Kawabata T, Honma S, Fukuda H, Yaegashi N, Yoshikawa H, Konishi I, Kamura T (2015) Clinical tumor diameter and prognosis of patients with FIGO stage IB1 cervical cancer (JCOG0806-A). Gynecol Oncol 137:34–39
Kawaguchi R, Furukawa N, Kobayashi H, Asakawa I (2013) Posttreatment cut-off levels of squamous cell carcinoma antigen as a prognostic factor in patients with locally advanced cervical cancer treated with radiotherapy. J Gynecol Oncol 24:313
Kawamura I, Hirashima Y, Tsukahara M, Mori K, Kurai H (2015) Microbiology of pelvic lymphocyst infection after lymphadenectomy for malignant gynecologic tumors. Surg Infect 16:244–246
Kim B (2013) Squamous cell carcinoma antigen in cervical cancer and beyond. J Gynecol Oncol 24:291
Kodama J, Seki N, Ojima Y, Nakamura K, Hongo A, Hiramatsu Y (2006) Prognostic factors in node-positive patients with stage IB-IIB cervical cancer treated by radical hysterectomy and pelvic lymphadenectomy. Int J Gynecol Obstet 93:130–135
Li D, Cai J, Kuang Y, Cao J, Wang Z (2012) Surgical-pathologic risk factors of pelvic lymph node metastasis in stage Ib1–IIb cervical cancer. Acta Obstet Gynecol Scand 91:802–809
Li X, Yin Y, Sheng X, Han X, Sun L, Lu C, Wang X (2015) Distribution pattern of lymph node metastases and its implication in individualized radiotherapeutic clinical target volume delineation of regional lymph nodes in patients with stage IA to IIA cervical cancer. Radiat Oncol 10:40
Liu Y, Zhao LJ, Li MZ, Li MX, Wang JL, Wei LH (2015) The number of positive pelvic lymph nodes and multiple groups of pelvic lymph node metastasis influence prognosis in stage IA–IIB cervical squamous cell carcinoma. Chin Med J Peking
Martínez A, Mery E, Filleron T, Boileau L, Ferron G, Querleu D (2013) Accuracy of intraoperative pathological examination of SLN in cervical cancer. Gynecol Oncol 130:525–529
Matsuura Y, Kawagoe T, Toki N, Tanaka M, Kashimura M (2006) Long-standing complications after treatment for cancer of the uterine cervix—clinical significance of medical examination at 5 years after treatment. Int J Gynecol Cancer 16:294–297
Papadia A, Imboden S, Fink A, Gasparri ML, Bolla D, Mueller MD (2016) Accuracy of sentinel lymph node mapping after previous hysterectomy in patients with occult cervical cancer. Ann Surg Oncol 23:2199–2205
Park J, Kim D, Kim J, Kim Y, Kim Y, Nam J (2010) Further stratification of risk groups in patients with lymph node metastasis after radical hysterectomy for early-stage cervical cancer. Gynecol Oncol 117:53–58
Pieterse QD, Kenter GG, Gaarenstroom KN, Peters AAW, Willems SM, Fleuren GJ, Trimbos JBMZ (2007) The number of pelvic lymph nodes in the quality control and prognosis of radical hysterectomy for the treatment of cervical cancer. Eur J Surg Oncol EJSO 33:216–221
Ruscito I, Gasparri ML, Braicu EI, Bellati F, Raio L, Sehouli J, Mueller MD, Panici PB, Papadia A (2016) Sentinel node mapping in cervical and endometrial cancer: indocyanine green versus other conventional dyes—a meta-analysis. Ann Surg Oncol
Slama J, Dundr P, Dusek L, Cibula D (2013) High false negative rate of frozen section examination of sentinel lymph nodes in patients with cervical cancer. Gynecol Oncol 129:384–388
Suprasert P, Charoenkwan K, Khunamornpong S (2012) Pelvic node removal and disease-free survival in cervical cancer patients treated with radical hysterectomy and pelvic lymphadenectomy. Int J Gynecol Obstet 116:43–46
Tax C, Rovers MM, de Graaf C, Zusterzeel PLM, Bekkers RLM (2015) The sentinel node procedure in early stage cervical cancer, taking the next step; a diagnostic review. Gynecol Oncol 139:559–567
Togami S, Kamio M, Yanazume S, Yoshinaga M, Douchi T (2014) Can pelvic lymphadenectomy be omitted in stage IA2 to IIB uterine cervical cancer? Int J Gynecol Cancer 24:1072–1076
van de Lande J, Torrenga B, Raijmakers PGHM, Hoekstra OS, van Baal MW, Brölmann HAM, Verheijen RHM (2007) Sentinel lymph node detection in early stage uterine cervix carcinoma: a systematic review. Gynecol Oncol 106:604–613
van de Lande J, Davelaar EM, von Mensdorff-Pouilly S, Water TJ, Berkhof J, van Baal WM, Kenemans P, Verheijen RHM (2009) SCC-Ag, lymph node metastases and sentinel node procedure in early stage squamous cell cervical cancer. Gynecol Oncol 112:119–125
Xiao M, Zhang Z (2015) Total laparoscopic versus laparotomic radical hysterectomy and lymphadenectomy in cervical cancer. Medicine 94:e1264
Zhang W, Zhang J, Yang J, Xue H, Cao D, Huang H, Wu M, Cui Q, Chen J, Lang J, Shen K (2014) The role of magnetic resonance imaging in pretreatment evaluation of early-stage cervical cancer. Int J Gynecol Cancer 24:1292–1298
Zhou J, Ran J, He Z, Quan S, Chen Q, Wu S, Sun J (2015) Tailoring pelvic lymphadenectomy for patients with stage IA2, IB1, and IIA1 uterine cervical cancer. J Cancer 6:377–381
Authors’ contributions
Conception and design: ZL, YW, TY. Acquisition of data (e.g., acquired and managed patients): ZL, YW, TY, JY, JL. Analysis and interpretation of data (statistical analysis, biostatistics, computational analysis): ZL, YW, TY, QC. Writing, review, and/or revision of the manuscript: ZL, YW, TY. All authors read and approved the final manuscript.
Acknowledgements
The Project Supported by Guangdong Science and Technology Foundation (Grant No. 2013B021800234).
Competing interests
The authors declare that they have no competing interests.
Ethical standards
The authors confirm that this study has been approved by the appropriate ethical committees related to the institution in which it was performed.
Informed consent
All patients gave their informed consent prior to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yaxian Wang and Tingting Yao contributed equally to this work
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wang, Y., Yao, T., Yu, J. et al. Can pelvic lymphadenectomy be omitted in patients with stage IA2, IB1, and IIA1 squamous cell cervical cancer?. SpringerPlus 5, 1262 (2016). https://doi.org/10.1186/s40064-016-2927-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2927-5