Abstract
Background
We report a rare case of a patient with a hypopharyngeal metastasis from breast cancer.
Case presentation
Isolated breast cancer metastasis to the hypopharynx has been previously reported in only one autopsy case. Herein, we report a 56-year-old woman with metastases to the hypopharynx almost 24 years after receiving a mastectomy and chemotherapy to treat primary breast carcinoma. We believe that she is the first patient to be treated for metastatic breast carcinoma to the hypopharynx. The hypopharyngeal tumor reduced in size after administration of an oral aromatase inhibitor. The patient has remained alive with a preserved larynx for three years.
Conclusions
Breast cancer metastasis to the hypopharynx is an extremely rare event.
Similar content being viewed by others
Background
In women, breast cancer is diagnosed in approximately 23 % of all cancer cases, which is the highest proportion amongst all cancer types and accounts for approximately 7.6 million deaths worldwide each year. Approximately 90 % of these deaths are due to metastatic dissemination of the disease (Cummings et al. 2014). In one study, the most common sites of the first metastasis of breast cancer were the bone (35 %), lungs (23 %), skin (22 %), and regional lymph nodes (16 %) during an average observation period of 3.6 years (range 0.8–6.4 years) (Kamby et al. 1988). The incidence of metastatic carcinoma in the hypopharynx is extremely low. To our knowledge, only one autopsy case has been previously reported (Nguyen and Weitzner 1983).
Here, we report a case of dormant breast carcinoma metastasis to the hypopharynx. We also evaluated E-cadherin and VEGFR2 expression levels and methylation statuses in order to help elucidate the mechanism of dormant ER-positive breast cancer metastasis in this case.
Case presentation
A 56-year-old woman had undergone a mastectomy with axillary lymph node dissection at 32 years of age (T2N1M0). She received tamoxifen for 2 years after surgery. When she was 42 years old, she was diagnosed with lung metastasis from the breast cancer, and a right upper lung lobe resection and lymph node dissection were performed. Images of the invasive ductal breast carcinoma that was resected when the patient was 32 years old and the lung metastasis from the breast cancer that was resected when the patient was 42 years old are shown in Fig. 1a and b, respectively.
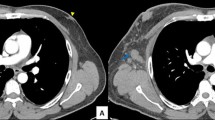
More than 10 years after the lung resection, when the patient was 56 years old, she was referred to our hospital after complaining of dyspnea on exertion. She had a 3-month history of weight loss and a left neck mass. On hypopharyngoscopy, a tumor lesion was found in the left anterior wall of the hypopharynx, and the patient experienced bilateral vocal cord paralysis (Fig. 2a). A contrast-enhanced computed tomography (CT) scan of the neck revealed a 24-mm heterogeneously enhanced tumor that extended through the left anterior wall of the hypopharynx (Fig. 2b). We performed a tracheostomy, hypopharyngeal biopsy, and lymph node extraction. Moreover, fluorodeoxyglucose positron emission tomography revealed high-level accumulation in the primary tumor, with a maximum standardized uptake value of 5.6, and metastatic neck lymph nodes. There was no evidence of a primary lung tumor or other distant metastases (Fig. 2c).
a On a hypopharyngeal fiberscopic image, a tumor was observed in the postcricoid area (a white arrow). b On a contrast-enhanced computed tomography scan of the neck before treatment, an enhanced tumor was observed in the postcricoid area of the hypopharynx (a white arrow). c On a fluorodeoxyglucose positron emission tomography scan of the neck before treatment, an enhanced tumor was observed in the hypopharynx (a black arrow) and the left side of the neck (arrowhead)
A pathologist analyzed the hypopharyngeal biopsy sample (Fig. 3a, b) and diagnosed the neck lymph node lesion as a hypopharyngeal metastasis from breast cancer. The biopsy sample was estrogen receptor (ER)-positive, progesterone receptor (PR)-positive, and human epidermal growth factor receptor type 2 (HER2)-negative (Fig. 3c–f). The patient completed oral aromatase inhibitor therapy and has remained alive after laryngeal preservation and hypopharyngeal tumor resection for the past 3 years. There was no evidence of any other active disease. The patient responded well, but she showed no objective improvement in laryngeal nerve function with a tracheostomy tube. This patient provided written informed consent under a protocol approved by the Institutional Review Boards at the Hamamatsu University School of Medicine.
Hematoxylin-eosin staining (H&E) and immunohistochemical studies. a Microscopic photos of the hypopharyngeal biopsy specimen (H&E). b The hypopharyngeal biopsy sample was diagnosed as metastatic breast carcinoma after positive ER immunostaining. c Microscopic photos of the lymph node specimen (H&E). d Positive ER immunostaining. e Positive progesterone receptor immunostaining. f Positive mammaglobin immunostaining
E-cadherin, VEGF-A, and VEGFR2 expression and methylation analyses
We sought to determine a mechanism leading to metastasis by focusing on E-cadherin, vascular endothelial growth factor A (VEGF-A), and vascular endothelial growth factor receptor 2 (VEGFR2). We examined E-cadherin, VEGF-A, and VEGFR2 protein expression levels. On immunohistochemical analysis, the neck lymph node lesion strongly expressed E-cadherin (Fig. 4a), VEGF-A (Fig. 4b), and VEGFR2 (Fig. 4c). Genomic DNA was extracted from the neck lymph nodes using the QIAamp DNA FFPE Tissue Kit (QIAGEN, Hilden, Germany). Bisulfite modification of genomic DNA converts unmethylated cytidine residues to uradine residues that are then converted to thymidine residues during subsequent polymerase chain reaction (PCR) (Misawa et al. 2015). The primers listed in Table 1 were used to analyze E-cadherin and VEGFR2 methylation statuses. The PCR products were separated by electrophoresis through a 9 % polyacrylamide gel and stained with ethidium bromide. For E-cadherin and VEGFR2, only unmethylated alleles were detected (Fig. 4c). Neck lymph node tumors without E-cadherin and VEGFR2 promoter methylation exhibited relatively robust protein expression levels. DNA methylation and mRNA expression data for invasive breast carcinomas were collected from MethHC: a database of DNA methylation and gene expression in human cancer (http://methhc.mbc.nctu.edu.tw/php/index.php) in April 2016 (Fig. 5) (Huang et al. 2015).
a E-cadherin was expressed in the lymph node specimen. b Positive VEGF-A receptor immunostaining. c Positive VEGFR2 receptor immunostaining. d Electrophoresis of methylation-specific PCR products that were amplified using DNA from the lymph node specimen. The results show that only unmethylated alleles of CDH1 and VEGFR2 were detected. M methylated alleles, UnM unmethylated alleles, B water blank
DNA methylation and expression data from the TCGA database of invasive breast carcinoma. a Distribution of E-cadherin DNA methylation between breast cancer samples and normal samples (P < 0.005). b A representative result showing the inverse correlation between DNA methylation at the E-cadherin CpG site and E-cadherin expression in breast cancer. The Spearman rank correlation coefficient (corr) is shown. c Comparison of VEGFR2 gene expression in tumor samples and matched normal samples (P < 0.005). d The relationship between DNA methylation and mRNA expression of the VEGFR2 gene
Discussion
Metastatic breast cancer causes symptoms that differ based on the location of the metastasis (Weng et al. 2014). This patient was referred to our hospital after complaining of dyspnea upon exertion. The metastatic breast cancer was difficult to diagnose from the observation of the mucosal hypopharyngeal surface. To ascertain distant metastatic breast carcinoma, immunohistochemistry should be performed to detect specific mark-ers (Kamby et al. 1988) (Weng et al. 2014). At least two types of markers must be evaluated: markers that are expressed similarly in the original and metastatic lesions and markers that can be used to differentiate between metastatic lesions and surrounding components (Zhang et al. 2013).
Approximately 20–40 % of patients with ER-positive breast cancer eventually develop recurrences in distant organs, and half of these events occur at least 5 years after diagnosis of the primary tumor. This phenomenon is especially pronounced in patients with ER-positive breast cancer, suggesting that E-positive cancer cells may remain dormant for a protracted period, despite adjuvant therapy (Zhang et al. 2013). Late recurrence is thought to be to the result of cancerous cells becoming activated from a dormant state, in which little or no de novo DNA transcription occurs and minimal protein translation from RNA occurs only to maintain the vegetative functions that sustain cell viability (Meltzer 1990). These findings suggest that the presence of certain cellular receptors may correlate with biological behavior of tumors, as manifested by differences in response to therapy and metastatic distributions.
Many human metastatic breast cancer lesions express membranous E-cadherin, whereas their paired primary tumors are E-cadherin-negative (Chao et al. 2010). Although E-cadherin re-expression and accompanying morphological changes have been achieved, any subsequent full or partial mesenchymal to epithelial transition has not been adequately assessed (Chao et al. 2012). E-cadherin re-expression due to loss of methylation suggests a functional mechanism by which the microenvironment modulates the mesenchymal to epithelial phenotypic switch (Taylor et al. 2014; Wendt et al. 2011).
VEGF-A and VEGFR2 are often co-expressed in breast cancer and potentially affect cellular pathways and the expression levels of key proteins that are targeted by endocrine therapy, such as ER (Mele et al. 2010). Expression of tumor-specific VEGFR2 is a predictive marker for response to tamoxifen in breast cancer patients (Ryden et al. 2005a). Elevated VEGF-A and VEGFR2 expression levels are associated with poor prognosis and poor response to tamoxifen therapy, suggesting that the combination of anti-hormone treatment with an anti-angiogenic strategy should be tested in clinical trials (Patel et al. 2010; Ryden et al. 2005b).
Patients with ER-positive breast cancers generally have a more favorable clinical outcomes, better prognoses, and better patterns of recurrence. Anti-estrogens, such as tamoxifen, and aromatase inhibitors, such as letrozole, can effectively control the disease and induce tumor responses in a large proportion of patients (Milani et al. 2014). For many years, tamoxifen was the most widely used first-line hormonal therapy for post-menopausal patients with hormone-sensitive advanced or metastatic breast cancer. Aromatase inhibitors, which have shown superior efficacy in advanced disease when compared with tamoxifen, have now largely replaced tamoxifen as first-line therapy in postmenopausal women (Riemsma et al. 2010).
Conclusions
In conclusion, hypopharyngeal metastasis of breast cancer is extremely rare. This case highlights the importance of immunohistochemical analysis in hypopharyngeal tumor diagnosis. ER, VEGF, and VEGFR2 expression levels are used when prescribing aromatase inhibitors as adjuvant treatment for postmenopausal patients. The patient in this study is currently alive after laryngeal preservation and hypopharyngeal tumor resection 3 years ago. E-cadherin and VEGFR2 expression levels and methylation statuses may be used to improve our understanding of ER-positive breast cancer reactivation after dormancy. However, these associations should be interpreted with caution because we have examined only one case.
References
Chao YL, Shepard CR, Wells A (2010) Breast carcinoma cells re-express E-cadherin during mesenchymal to epithelial reverting transition. Mol Cancer 9:179. doi:10.1186/1476-4598-9-179
Chao Y, Wu Q, Acquafondata M, Dhir R, Wells A (2012) Partial mesenchymal to epithelial reverting transition in breast and prostate cancer metastases. Cancer Microenviron 5(1):19–28. doi:10.1007/s12307-011-0085-4
Cummings MC, Simpson PT, Reid LE, Jayanthan J, Skerman J, Song S, McCart Reed AE, Kutasovic JR, Morey AL, Marquart L, O’Rourke P, Lakhani SR (2014) Metastatic progression of breast cancer: insights from 50 years of autopsies. J Pathol 232(1):23–31. doi:10.1002/path.4288
Huang WY, Hsu SD, Huang HY, Sun YM, Chou CH, Weng SL, Huang HD (2015) MethHC: a database of DNA methylation and gene expression in human cancer. Nucleic acids research 43(Database issue):D856–D861. doi:10.1093/nar/gku1151
Kamby C, Ejlertsen B, Andersen J, Birkler NE, Rytter L, Zedeler K, Rose C (1988) The pattern of metastases in human breast cancer. Influence of systemic adjuvant therapy and impact on survival. Acta Oncol 27(6A):715–719
Mele T, Generali D, Fox S, Brizzi MP, Bersiga A, Milani M, Allevi G, Bonardi S, Aguggini S, Volante M, Dogliotti L, Bottini A, Harris A, Berruti A (2010) Anti-angiogenic effect of tamoxifen combined with epirubicin in breast cancer patients. Breast Cancer Res Treat 123(3):795–804. doi:10.1007/s10549-010-1063-0
Meltzer A (1990) Dormancy and breast cancer. J Surg Oncol 43(3):181–188
Milani A, Geuna E, Mittica G, Valabrega G (2014) Overcoming endocrine resistance in metastatic breast cancer: current evidence and future directions. World J Clin Oncol 5(5):990–1001. doi:10.5306/wjco.v5.i5.990
Misawa K, Misawa Y, Kondo H, Mochizuki D, Imai A, Fukushima H, Uehara T, Kanazawa T, Mineta H (2015) Aberrant methylation inactivates somatostatin and somatostatin receptor type 1 in head and neck squamous cell carcinoma. PLoS One 10(3):e0118588. doi:10.1371/journal.pone.0118588
Nguyen CH, Weitzner S (1983) Metastatic carcinoma of breast in the hypopharynx. South Med J 76(12):1590–1591
Patel RR, Sengupta S, Kim HR, Klein-Szanto AJ, Pyle JR, Zhu F, Li T, Ross EA, Oseni S, Fargnoli J, Jordan VC (2010) Experimental treatment of oestrogen receptor (ER) positive breast cancer with tamoxifen and brivanib alaninate, a VEGFR-2/FGFR-1 kinase inhibitor: a potential clinical application of angiogenesis inhibitors. Eur J Cancer 46(9):1537–1553. doi:10.1016/j.ejca.2010.02.018
Riemsma R, Forbes CA, Kessels A, Lykopoulos K, Amonkar MM, Rea DW, Kleijnen J (2010) Systematic review of aromatase inhibitors in the first-line treatment for hormone sensitive advanced or metastatic breast cancer. Breast Cancer Res Treat 123(1):9–24. doi:10.1007/s10549-010-0974-0
Ryden L, Jirstrom K, Bendahl PO, Ferno M, Nordenskjold B, Stal O, Thorstenson S, Jonsson PE, Landberg G (2005a) Tumor-specific expression of vascular endothelial growth factor receptor 2 but not vascular endothelial growth factor or human epidermal growth factor receptor 2 is associated with impaired response to adjuvant tamoxifen in premenopausal breast cancer. J Clin Oncol 23(21):4695–4704. doi:10.1200/JCO.2005.08.126
Ryden L, Stendahl M, Jonsson H, Emdin S, Bengtsson NO, Landberg G (2005b) Tumor-specific VEGF-A and VEGFR2 in postmenopausal breast cancer patients with long-term follow-up. Implication of a link between VEGF pathway and tamoxifen response. Breast Cancer Res Treat 89(2):135–143. doi:10.1007/s10549-004-1655-7
Taylor DP, Clark A, Wheeler S, Wells A (2014) Hepatic nonparenchymal cells drive metastatic breast cancer outgrowth and partial epithelial to mesenchymal transition. Breast Cancer Res Treat 144(3):551–560. doi:10.1007/s10549-014-2875-0
Wendt MK, Taylor MA, Schiemann BJ, Schiemann WP (2011) Down-regulation of epithelial cadherin is required to initiate metastatic outgrowth of breast cancer. Mol Biol Cell 22(14):2423–2435. doi:10.1091/mbc.E11-04-0306
Weng B, Wang Q, Lin S, Lu Y (2014) Nasal cavity metastasis of breast cancer: a case report and review of the literature. Int J Clin Exp Pathol 7(10):7028–7033
Zhang XH, Giuliano M, Trivedi MV, Schiff R, Osborne CK (2013) Metastasis dormancy in estrogen receptor-positive breast cancer. Clin Cancer Res 19(23):6389–6397. doi:10.1158/1078-0432.CCR-13-0838
Authors’ contributions
CI, KM and KS performed the operation and evaluated the patient. SE and DM revised the manuscript and evaluated the patient. AI, MM, YM, TY and HM reviewed the chart and published literature. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Ms. Yuko Mohri for her excellent technical support.
Competing interests
The authors declare that they have no competing interests.
Patient consent
The patient consented to the submission of this case report (IRB of Hamamatsu University School of Medicine).
Author information
Authors and Affiliations
Corresponding author
Additional information
Chisako Izumi and Kiyoshi Misawa contributed equally to this work as first authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Izumi, C., Misawa, K., Endo, S. et al. Late recurrence of breast carcinoma metastasis to the hypopharynx: a case report. SpringerPlus 5, 599 (2016). https://doi.org/10.1186/s40064-016-2226-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2226-1