Abstract
Purpose
The aim of this study was to identify factors that predict favorable functional outcomes in elderly patients with large-vessel occlusion acute ischemic stroke (LVO-AIS) who underwent mechanical thrombectomy (MT).
Methods
We conducted a retrospective observational study using the prospectively maintained Bigdata Observatory for Stroke of China (BOSC) to identify eligible patients who underwent MT for LVO-AIS at four comprehensive stroke centers between August 2019 and February 2022. Inclusion criteria included patients aged 80 years or older with a baseline modified Rankin Scale (mRS) 0–2, baseline National Institutes of Health Stroke Scale (NIHSS) > 6, baseline Alberta Stroke Program Early CT Score (ASPECTS) > 6 who received treatment within 24 h from symptom onset. Pertinent demographic, clinical, and procedural variables were collected. Multivariable regression analyses were performed to identify predictors of favorable long-term functional outcomes, defined as mRS 0–2 at 90 days.
Results
A total of 63 patients were included in the study with a mean age of 83 years. Patients with previous diagnosis of atrial fibrillation were more likely to have a favorable functional outcome (OR 2.09, 95% CI 2.09–407.33, p = 0.012), while a higher baseline NIHSS was associated with a less favorable functional outcome (OR 0.64, 95% CI 0.46–0.89, p = 0.007). In addition, there was an observed trend suggesting an association between higher baseline ASPECTS and favorable functional outcomes. This association did not reach statistical significance (OR 2.49, 95% CI 0.94–6.54, p = 0.065).
Conclusion
In this study, we identified factors that predicted a favorable functional outcome in elderly LVO-AIS patients undergoing MT. A higher baseline NIHSS decreased the odds of mRS 0–2 at 90 days, whereas a history of atrial fibrillation increased the odds of a favorable functional outcome. These results emphasize the complex relationship between clinical factors and functional recovery in this vulnerable population.
Similar content being viewed by others
Introduction
Mechanical thrombectomy (MT) stands as the first-line treatment for patients with acute ischemic stroke (AIS) due to proximal large-vessel occlusion (LVO) in the anterior and posterior circulation within 24 h from symptom onset [1,2,3]. The evidence supporting its overwhelming benefit is underscored by numerous clinical trials, individual patient data-based meta-analysis, and the strong recommendations in global guidelines [4,5,6]. Despite the established benefits of mechanical thrombectomy for acute ischemic stroke, elderly patients have been underrepresented in clinical trials, leading to uncertainty about the efficacy and safety of this intervention in this age group.
When compared to medical treatment alone, elderly adults benefit from MT [7]. However, prior studies have consistently found that rates of favorable outcomes are lower than those seen in younger patients [8, 9]. This discrepancy likely arises from a combination of factors, including age-related physiological and anatomic characteristics, such as decreased resilient brain tissue and collateral status, and a higher prevalence of medical comorbidities as well as neurological and systemic post-procedural complications [10,11,12].
There is a significant research gap regarding the efficacy and safety of mechanical thrombectomy in patients aged 80 years and older, as they were underrepresented in pivotal clinical trials. Understanding predictors of favorable outcomes in this population is crucial for improving patient selection and optimizing treatment strategies. This study seeks to address this gap by identifying predictors of favorable outcomes in this specific population.
Methods
The study protocol received approval from the Institutional Review Board of Foshan Sanshui District People’s Hospital institutional review board. All procedures involving human participants were conducted in accordance with the institutional and/or national research committee standards, and followed the principles outlined in the 1964 Declaration of Helsinki and its subsequent amendments, or comparable ethical standards.
In this retrospective observational study, we included consecutive patients diagnosed with LVO-AIS, who underwent MT at four comprehensive stroke centers between August 2019 and February 2022. These patients were part of the Bigdata Observatory Platform for Stroke of China (BOSC). Our inclusion criteria included patients aged 80 years or older with a baseline modified Rankin Scale (mRS) 0–2 and Computed Tomography Angiography (CTA)-defined LVO-AIS, National Institutes of Health Stroke Scale (NIHSS) score on presentation of > 6, baseline Alberta Stroke Program Early CT Score (ASPECTS) > 6, who received treatment within 24 h from stroke onset or time from last known well. Patients with incomplete follow-up information were excluded from the study (Fig. 1).
Data collection
We collected the past medical history, baseline information, initial premorbid modified Rankin Scale (mRS), door-to-needle time (DNT), stroke onset-to-needle time (ONT), door-to-puncture time (DPT), last-known normal-to-puncture time (LKNPT), door-to-recanalization time (DRT), and treatment with intravenous thrombolysis (IV-tPA). Procedural variables included site of vessel occlusion, complications, and the modified Thrombolysis In Cerebral Infarction (mTICI) score post thrombectomy. Follow-up variables included parenchymal hematoma type 1 (PH1), parenchymal hematoma type 2 (PH2), symptomatic intracerebral hemorrhage (sICH, defined as the SITS-MOST protocol) [13], mRS at 90 days, length of stay, and hospitalization costs. Successful reperfusion was defined as mTICI 2b-3, and favorable functional outcome was defined as mRS 0–2 at 90 days.
Patients were asked to attend a follow-up visit with a specialist in the neurology clinic 90 days after MT. For patients who could not come to the hospital, outcome information (mRS or death) was followed up by telephone contact between nurses and patients’ family members. Demographic and clinical data and procedural variables data were collected by two specialists in neurology using the hospital electronic medical records. Cerebral baseline imaging was performed on multi-slice computed tomography (non-contrast CT and CT-angio) or magnetic resonance imaging (MRI with diffusion-weighted imaging [DWI], time-of-flight [TOF], and fluid-attenuated inversion recovery [FLAIR]) to confirm acute cerebral Ischemia.
Statistical analysis
Statistical analyses were performed using IBM SPSS version 27 (IBM-Armonk, NY). We used descriptive statistics to summarize the variables collected. We then reported continuous variables as means (SD) or medians (IQR), and categorical variables as counts and percentages. We used histograms to assess normality of variables’ distribution. We compared continuous variables with the Mann–Whitney U or Student’s t test, and categorical variables with the chi-squared or Fisher’s exact test. Multivariable regression models were used to examine predictors of favorable outcome. The results were considered statistically significant at a two-sided alpha level of ≤ 0.05. Variables with a p value < 0.1 in the univariable analyses were included in the subsequent multivariable regression analysis.
Results
Description of the sample
Of the 555 patients initially evaluated, we excluded 487 patients younger than 80 years old. Five patients were excluded due to loss to follow-up. In our final analysis, 63 patients met the inclusion criteria and were included in our study (Fig. 1).
The mean (SD) age was 82.98 ± 3.02 years, and 39.6% of the participants were males. Notably, patients with a favorable functional outcome had higher rates of atrial fibrillation (87.5 vs. 46.8%), MCA-M1 site of occlusion (68.8 vs. 36.8%), and better rates of successful recanalization (93.8 vs. 72.3%) in comparison to patients with an unfavorable functional outcome. Conversely, they had lower rates of CAD (6.3 vs. 31.9%), ICA and tandem lesions (6.2 vs. 25.5%, and 6.3 vs. 27.7%, respectively), and a lower median baseline NIHSS (13 vs. 18). The median baseline ASPECTS was similar between both groups, although patients with favorable functional outcomes had a higher IQR ([8, 9] vs. [7,8,9]. Detailed results are shown in Table 1.
Predictors of favorable outcome
In the multivariable analysis, we included the following variables as candidate predictors: CAD, atrial fibrillation, baseline NIHSS, baseline ASPECTS, successful recanalization, and vessel occlusion site. Patients with a previous diagnosis of atrial fibrillation had greater odds of achieving a favorable functional outcome (OR 2.09, 95% CI 2.09–407.33, p = 0.012), while a higher baseline NIHSS reduced these odds (OR 0.64, 95% CI 0.46–0.89, p = 0.007). Moreover, although there was an observable trend suggesting a link between higher baseline ASPECTS and favorable functional outcome, this association did not attain statistical significance (OR 2.49, 95% CI 0.94–6.54, p = 0.065). (Table 2).
Discussion
In this study of AIS-LVO in elderly patients, we observed that a higher baseline NIHSS was a predictor of lower rates of favorable functional outcome at 90 days, while a prior diagnosis of atrial fibrillation was associated with higher rates of favorable functional outcomes.
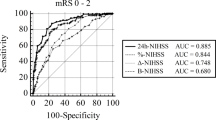
Prior research has shown that older age is a negative predictor of functional outcomes following mechanical thrombectomy [14,15,16]. When specific selection criteria are used, however, Goyal et al. reported that in a small subgroup of elderly patients, the use of mechanical thrombectomy was beneficial compared to intravenous thrombolysis alone [4]. Several studies have explored the treatment risks and benefits of mechanical thrombectomy in elderly patients [17,18,19,20]. For example, a recent study from the Endovascular Treatment in Ischemic Stroke (ETIS) registry showed that patients older than 80 years of age undergoing mechanical thrombectomy had higher mortality rates compared to patients aged 18–80 (34.3% vs 20%) and lower chances of achieving a good functional outcome (20.5% vs. 44.4%) [21]. Our cohort showed similar findings, with a high mortality rate (39.68%) and a relatively small number of patients (20.4%) achieving mRS 0–2 at 90 days(Fig. 2). Although many predictors of worse outcomes after AIS-LVO have been already described, understanding the potentially differential effects in older age is critical to increasing the beneficial effect of MT in this group [11, 12].
In accordance with previous studies, the severity of the ischemic event, as indicated by the NIHSS, showed a significant correlation with adverse outcomes [22, 23]. While this effect has been widely described across the general population, it is important to recognize that advancing age can translate into diminished physiological resilience. Consequently, even in cases where we might expect higher NIHSS among elderly patients, a higher NIHSS continues to stand as a vital prognostic feature for clinical deterioration post-MT.
Conversely, despite anticipated higher rates of AF among the elderly, our identification of AF as an independent predictor of functional outcomes is contrary to prior reports. Most studies have consistently reported that, regardless of age, individuals with acute LVO attributed to AF tend to experience unfavorable clinical outcomes post-MT, compared to those without AF [24, 25]. The prevailing hypothesis attributes this finding to a greater concurrence of comorbidities and cardiovascular risk factors in AF patients [10, 26]. Moreover, the decreased utilization of intravenous thrombolysis stemming from prior treatment with oral anticoagulants could contribute to worse outcomes in AF patients. It is an interesting observation that in our study, where these disparities are controlled for, non-AF patients did not have superior functional outcomes. In our cohort, 30.55% of patients with a diagnosis of AF received MT. Furthermore, 77.78% of these patients had successful recanalization. Clot composition due to AF might favor the chances of better and faster recanalization during MT, which could explain a favorable aspect of this disease in the context of AIS-LVO [27]. Prior studies have also shown that thrombectomy in AF-related strokes achieved a higher proportion of first-pass effect (FPE), defined as achieving a complete recanalization with a single thrombectomy device pass, compared to non-AF-related strokes [28]. Faster and more complete vessel recanalization, in turn, correlates with better clinical outcomes—as demonstrated by multi-center prospective studies comparing outcomes in FPE to non-FPE patients. [29]. In our cohort, elderly patients with unfavorable outcomes had higher, albeit not statistically significant, rates of baseline hypertension and ICA and tandem occlusions, and lower rates of successful recanalization, which may reflect a higher relative incidence of ICAD-related AIS-LVO. Hence, while prior research has shown that AF-related strokes are associated with worse functional outcomes in the general population, AF-related strokes in elderly patients are associated with favorable functional outcomes likely, in part, due to better recanalization rates [24, 25].
Nonetheless, our study has certain limitations. First, the small sample size of 63 patients limits the generalizability of our findings. This is inherently constrained due to the relative scarcity of elderly patients undergoing MT. Larger studies are necessary to validate these results and ensure their applicability to broader populations. Second, important variables like rates of symptomatic ICH, type of anesthesia, and collateral status were not available for inclusion in our analysis. Thirdly, the lack of blinding in outcome adjudication introduces a potential source of bias.
Despite these limitations, our findings contribute valuable insights to the scarce medical literature focused specifically on elderly Chinese patients. Future prospective and randomized studies should evaluate the safety and efficacy of mechanical thrombectomy accounting for the predictors of favorable functional outcomes described in this and other studies.
Conclusions
Our study sheds light on the predictive factors associated with functional outcomes in elderly Chinese patients with AIS-LVO who undergo MT. Higher baseline NIHSS scores were associated with reduced odds of mRS 0–2 at 90 days, whereas a history of atrial fibrillation was associated with higher rates of favorable functional recovery. These findings underscore the complex interplay between clinical variables and outcomes in this vulnerable population. As we move forward, large prospective trials are needed to validate these predictors, consequently informing the tailored management of these patients and improving optimal outcomes.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Liu L, Chen W, Zhou H, Duan W, Li S, Huo X, et al. Chinese stroke association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc Neurol. 2020;5:159–76.
Klein P, Herning A, Drumm B, Raymond J, Abdalkader M, Siegler JE, et al. Basilar artery occlusion thrombectomy technique: an international survey of practice patterns. Stroke: Vascu Int Neurol. 2023. https://doi.org/10.1161/SVIN.03.suppl_1.006.
Alemseged F, Nguyen TN, Alverne FM, Liu X, Schonewille WJ, Nogueira RG. Endovascular therapy for basilar artery occlusion. Stroke. 2023;54:1127–37.
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Jovin TG, Nogueira RG, Lansberg MG, Demchuk AM, Martins SO, Mocco J, et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (aurora): a systematic review and individual patient data meta-analysis. Lancet. 2022;399:249–58.
Edwards C, Drumm B, Siegler JE, Schonewille WJ, Klein P, Huo X, et al. Basilar artery occlusion management: specialist perspectives from an international survey. J Neuroimaging. 2023;33:422–33.
Castonguay AC, Zaidat OO, Novakovic R, Nguyen TN, Taqi MA, Gupta R, et al. Influence of age on clinical and revascularization outcomes in the north american solitaire stent-retriever acute stroke registry. Stroke. 2014;45:3631–6.
Rezai MK, Dalen I, Advani R, Fjetland L, Kurz KD, Sandve KO, et al. Thrombectomy in large vessel occlusion stroke-does age matter? Acta Neurol Scand. 2022;146:628–34.
Zaidat OO, Liebeskind DS, Jadhav AP, Ortega-Gutierrez S, Nguyen TN, Haussen DC, et al. Impact of age and alberta stroke program early computed tomography score 0 to 5 on mechanical thrombectomy outcomes: analysis from the stratis registry. Stroke. 2021;52:2220–8.
Wu W, Pitton Rissardo J, Nguyen TN, Mofatteh M, Wei H, Liebeskind DS, et al. Effect of atrial fibrillation on outcomes in patients with anterior circulation occlusion stroke receiving endovascular therapy. Front Aging Neurosci. 2023;15:1160265.
Chen Y, Zhou S, Yang S, Mofatteh M, Hu Y, Wei H, et al. Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front Neurosci. 2022;16:1034472.
Winovich DT, Longstreth WT Jr, Arnold AM, Varadhan R, Zeki Al Hazzouri A, Cushman M, et al. Factors associated with ischemic stroke survival and recovery in older adults. Stroke. 2017;48:1818–26.
Fu CH, Chen CH, Lin CH, Lee CW, Lee M, Tang SC, et al. Comparison of risk scores in predicting symptomatic intracerebral hemorrhage after endovascular thrombectomy. J Form Med Assoc = Taiwan Yi Zhi. 2022;121:1257–65.
Ospel JM, Brown S, Kappelhof M, van Zwam W, Jovin T, Roy D, et al. Comparing the prognostic impact of age and baseline national institutes of health stroke scale in acute stroke due to large vessel occlusion. Stroke. 2021;52:2839–45.
Fonarow GC, Reeves MJ, Zhao X, Olson DM, Smith EE, Saver JL, et al. Age-related differences in characteristics, performance measures, treatment trends, and outcomes in patients with ischemic stroke. Circulation. 2010;121:879–91.
Rezai MK, Advani R, Dalen I, Fjetland L, Kurz KD, Kurz MW. Endovascular thrombectomy in the elderly: do radiological and clinical outcomes differ from those in younger patients? a prospective single-center experience. Cerebrovascu Dis. 2019;47:65–71.
Chen H, Jindal G, Miller TR, Gandhi D, Chaturvedi S. Stroke thrombectomy in the elderly: efficacy, safety, and special considerations. Stroke: Vascu Int Neurol. 2023. https://doi.org/10.1161/SVIN.122.000634.
Meyer L, Alexandrou M, Flottmann F, Deb-Chatterji M, Abdullayev N, Maus V, et al. Endovascular treatment of very elderly patients aged >/=90 with acute ischemic stroke. J Am Heart Assoc. 2020;9: e014447.
Slawski DE, Salahuddin H, Shawver J, Kenmuir CL, Tietjen GE, Korsnack A, et al. Mechanical thrombectomy in elderly stroke patients with mild-to-moderate baseline disability. Interv Neurol. 2018;7:246–55.
Sallustio F, Koch G, Motta C, Diomedi M, Alemseged F, D’Agostino VC, et al. Efficacy and safety of mechanical thrombectomy in older adults with acute ischemic stoke. J Am Geriatr Soc. 2017;65:1816–20.
Finitsis S, Epstein J, Richard S, Bourcier R, Sibon I, Dargazanli C, et al. Age and outcome after endovascular treatment in anterior circulation large-vessel occlusion stroke: Etis registry results. Cerebrovasc Dis. 2020;50:68–77.
Irvine HJ, Battey TW, Ostwaldt A-C, Campbell BC, Davis SM, Donnan GA, et al. Early neurological stability predicts adverse outcome after acute ischemic stroke. Int J Stroke. 2016;11:882–9.
Saver JL, Altman H. Relationship between neurologic deficit severity and final functional outcome shifts and strengthens during first hours after onset. Stroke. 2012;43:1537–41.
Hayden DT, Hannon N, Callaly E, Chróinín DN, Horgan G, Kyne L, et al. Rates and determinants of 5-year outcomes after atrial fibrillation–related stroke. Stroke. 2015;46:3488–93.
Steger C, Pratter A, Martinek-Bregel M, Avanzini M, Valentin A, Slany J, et al. Stroke patients with atrial fibrillation have a worse prognosis than patients without: data from the Austrian stroke registry. Eur Heart J. 2004;25:1734–40.
LaMori JC, Mody SH, Gross HJ, daCosta DM, Patel AA, Schein JR, et al. Burden of comorbidities among patients with atrial fibrillation. Ther Adv Cardiovasc Dis. 2013;7:53–62.
Lin C-J, Luo C-B, Chien C, Chang F-C, Lin C-J, Lee I-H, et al. Better endovascular mechanical thrombectomy outcome in atrial fibrillation patients with acute ischemic stroke: a single-center experience. J Chin Med Assoc. 2020;83:756–60.
Pillai P, Bush SJ, Kusuma Y, Churilov L, Dowling RJ, Luu VD, Davis SM, Mitchell PJ, Yan B. Atrial fibrillation is associated with higher first pass effect following thrombectomy for large vessel occlusion. J Neurointerv Surg. 2023. https://doi.org/10.1136/jnis-2023-020512.
Di Maria F, et al. Identifying the predictors of first-pass effect and its influence on clinical outcome in the setting of endovascular thrombectomy for acute ischemic stroke: Results from a multicentric prospective registry. Int J Stroke. 2021;16(1):20–8. https://doi.org/10.1177/1747493020923051.
Acknowledgements
We thank all our colleagues for data collection and patients’ contribution.
Funding
The project was supported by Foshan Science and Technology Bureau (Grant No. 2320001006321), Foshan the 14th Five-Year Plan Key Discipline Foundation.
Author information
Authors and Affiliations
Contributions
QL and MF contributed equally in this study. QL and MF: Conceived the idea, Data curation, Formal analysis, Investigation, Methodology, Visualization, Drafted the original manuscript, Review and Editing. MG, AA, AD and FP: Methodology and Revison. JC, LZL, WL, JM, SJ, YL, LJL: Data curation. YC: Formal analysis. YS and SY: Final manuscript review, process guidance and supervision. All authors have made substantial contributions to this study and approved the final version of manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The research related to human use has been complied with all the relevant national regulations, institutional policies, and has been approved by the Foshan Sanshui People’s Hospital review board. Informed consent was obtained from all research participants to perform EVT according to local regulations.
Competing interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, Q., Feng, M., Galecio-Castillo, M. et al. Predictors of favorable functional outcomes for elderly patients undergoing endovascular thrombectomy for acute ischemic stroke. Eur J Med Res 29, 429 (2024). https://doi.org/10.1186/s40001-024-02027-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-02027-8