Abstract
Background
Urinary incontinence (UI) is closely related to obesity. The aim of this study is to evaluate the association of a novel anthropometric indicator weight-adjusted-waist index (WWI) with UI.
Methods
This cross-sectional study used the data from National Health and Nutrition Examination Survey (NHANES) 2001–2018. Weighted multivariable logistic regression was used to evaluate the relationship between WWI and three types of UI [stress UI (SUI), urgency UI (UUI), and mixed UI (MUI)]. The receiver operating characteristic (ROC) curve and Delong et al.’s test were utilized for comparison of the predictive capability for UI between WWI and body mass index (BMI), waist circumference (WC).
Results
A total of 41,614 participants were included in this study, of whom 23.57% had SUI, 19.24% had UUI, and 9.43% had MUI. In the fully adjusted model, WWI was positively associated with three types of UI [SUI: odds ratio (OR) = 1.19, 95%Confidence interval (CI) 1.13–1.25; UUI: OR = 1.18, 95%CI 1.13–1.24; MUI: OR = 1.19, 95%CI 1.11–1.27, all p < 0.001]. Compared to the lowest WWI interval, the positive correlation between WWI and UI still existed in the highest WWI group after converting WWI to a categorical variable by quartiles (SUI: OR = 1.52, 95%CI 1.35–1.71, p < 0.001; UUI: OR = 1.50, 95%CI 1.33–1.69, p < 0.001; MUI: OR = 1.55, 95%CI 1.32–1.83, p < 0.001). WWI had a stronger prediction for three types of UI than BMI and WC (all p < 0.001).
Conclusion
A higher WWI was linked with an increased likelihood of three types of UI (SUI, UUI, and MUI) in the United State population. Compared to BMI and WC, WWI had a stronger predictive power for UI. WWI may be a better adiposity parameter for evaluating UI.
Similar content being viewed by others
Introduction
Urinary incontinence (UI) is a common disease worldwide and is defined as the involuntary loss of urine [1]. On a global scale, the prevalence of UI exhibited a positive connection with advancing age, whereby up to 30% to 40% of elderly women acknowledged experiencing UI [2]. A National Health and Nutrition Examination Survey (NHANES) cross-sectional study indicated that 17.1% of American women aged 20 years or older complaint of moderate-to-severe UI [3]. It demonstrated that UI had a documented prevalence of 11% among men aged 60–64 years, escalating to 31% in men aged 85 years and above [4]. UI is mainly classified as stress urinary incontinence (SUI), urgency urinary incontinence (UUI), and mixed urinary incontinence (MUI) [5]. Based on the International Continence Society, SUI is defined as involuntary urine leakage during coughing, sneezing, or physical exertion. UUI is described as involuntary urine loss associated with urgency. MUI is expressed as the complaint of involuntary loss of urine associated with urgency and with effort, exertion, coughing, or sneezing [6]. UI is a common health problem that affects the daily life of many people and imposes a huge economic burden on society [7]. Numerous risk factors contribute to UI, including but not limited to aging, childbirth complications, medications, sedentary behavior, and obesity [2].
Obesity is a severe public health threat with a significantly increased prevalence worldwide [8]. Ward et al. predicted that almost half of American adults will have obesity by 2030 [9]. Some traditional adiposity indicators such as body mass index (BMI) and waist circumference (WC) are widely used to evaluate the degree of obesity. However, there are some limitations in the assessment of obesity using these common parameters. For instance, the inability of BMI to distinguish body fat and lean mass resulted in limited diagnostic accuracy in individuals with intermediate BMI ranges [10]. WC is considered a simple and convenient indicator for evaluating abdominal or central obesity and reflect the visceral adiposity tissue [11]. However, the strong correlation between WC and BMI resulted in that WC was not free from the impact of BMI [12]. Weight-adjusted-waist index (WWI) was proposed by Park et al. [13] as a novel adiposity indicator and calculated as WC (cm)/weight (kg)1/2. WWI had a good predictive performance for cardiometabolic disorders, cardiovascular mortality, and all-cause mortality [13]. Moreover, Kim et al. indicated that WWI was positively related to fat mass whereas negatively associated with muscle mass in participants older than 65 years old [14].
Epidemiological surveys demonstrated that obesity is regarded as an independent risk factor for the prevalence of UI. A meta-epidemiology study indicated that middle-aged and older women with overweight (25 kg/m2 ≤ BMI < 30 kg/m2) and obesity (30 kg/m2 ≤ BMI < 35 kg/m2) had a higher risk of UI [15]. Park et al. showed that visceral obesity may be stronger associated with UI compared with overall obesity [16]. Choi et al. demonstrated that there was an association between a chronic increase in BMI and a higher risk of UI in the later stages of life. In addition, the increased duration of being either overweight or obese resulted in more severe symptoms of UI [17]. However, to our knowledge, the association between WWI and the risk of UI has not been investigated. Therefore, it is necessary to explore the relationship between WWI and three types of UI (SUI, UUI, and MUI) using the data obtained from the NHANES database ranging from 2001 to 2018.
Materials and methods
Study description and population
The analyzed data in this cross-sectional study were collected from NHANES, a population-based survey conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS). NHANES is designed to assess the health and nutritional status of the United States population. The integration of in-home interviews and physical examinations represents a distinctive characteristic of the survey methodology. The component of in-home interview encompasses demographics, socioeconomic status, dietary habits, and health-related information. The physical examinations comprise medical, dental, and physiological assessments, as well as laboratory tests, all administered by qualified medical professionals. The NHANES used a complex stratified multistage probability design to obtain a representative sample of the resident civilian non-institutionalized U.S. population [18]. More detailed information can be accessed at https://www.cdc.gov/nchs/nhanes/index.htm.
We enrolled survey individuals who completed the examination of body measures and the questionnaire on kidney conditions from nine NHANES cycles 2001–2018 at first, since the examination of body measures provided the WC and body weight data for the calculation of WWI and the questionnaire on kidney conditions included the interview for the evaluation of UI. The participant exclusion criteria were as follows: (1) participants without complete WC and weight data; (2) participants without answering the interview about assessing the condition of UI; (3) participants with missing data on other potential covariates.
Measurement of WWI
In this study, WWI was considered an exposure variable calculated as WC (cm) divided by the square root of weight (kg) [13]. The information on WC and weight was available in the section “Body Measures” of the NHANES examination data. As a novel adiposity index, an elevated WWI reveals a more severe degree of obesity. WWI was designed as continuous and categorical variables in analyses. The categorical WWI was divided into four subgroups (Q1–Q4) based on the WWI quartiles.
Assessment of UI
There were two questions evaluating the conditions of UI in NHANES. If participants had answered yes to the question “During the past 12 months, have you leaked or lost control of even a small amount of urine with an activity like coughing, lifting or exercise?”, they were defined as stress UI (SUI). If survey individuals had responded yes to the question “During the past 12 months, have you leaked or lost control of even a small amount of urine with an urge or pressure to urinate and you couldn't get to the toilet fast enough?”, they were defined as urgency UI (UUI). Participants who answered yes to both the above questions were considered mixed UI (MUI).
Covariates of interest
In this study, gender, age, race/ethnicity, education level, marital status, the family poverty income ratio (PIR), BMI, physical activity (vigorous/moderate), smoking status, alcohol intaking, diabetes, and hypertension were set as the covariates of interest. Numerous missing covariates for the family PIR (n = 3265) and alcohol intaking (n = 604) were designed as missing value categories to avoid further reducing huge samples in our study, and the missing value categories were designed as dummy variables in regression models. If participants engaged in any vigorous activities including running, lap swimming, aerobics classes, or brisk bicycling for a duration of at least 10 min during the past 30 days that resulted in heavy sweating, or notable increases in breathing or heart rate, they were set as having vigorous activities. Participants who did moderate activities such as brisk walking, leisurely bicycling, golf, and dancing for a minimum of 10 min, resulting in only light sweating or a slight to moderate elevation in breathing or heart rate during the past 30 days were designed as having moderate activities. If survey individuals had smoked at least 100 cigarettes throughout their entire life and smoked every day or some days at the time of the questionnaire, they were defined as current smokers. Participants who smoked at least 100 cigarettes in their entire life and did not smoke when taking the questionnaire were set as former smokers. Additionally, if individuals answered that they smoked less than 100 cigarettes during their lifetime, they were considered nonsmokers. Participants were categorized as drinkers and nondrinkers (whether had at least 12 alcohol drinks per year). If participants were diagnosed with diabetes by doctors before the interview or their fasting plasma glucose was ≥ 126 mg/dL, they were regarded as having diabetes. If doctors told survey individuals that they had hypertension, or participants were taking a prescription for hypertension, or their systolic blood pressure was ≥ 140 mmHg, or their diastolic blood pressure was ≥ 90 mmHg, they were considered having hypertension.
Statistical analysis
In the current study, considering the NHANES complex multistage sampling design, appropriate sampling weights, stratification, and clustering were utilized in all statistical analyses. Continuous variables were presented as weighted mean and standard error (SE), and categorical variables were expressed as weighted proportions. To compare the differences among four groups divided by WWI quartiles, a survey-weighted linear regression for continuous variables and a survey-weighted Chi-square test for categorical variables were used in the baseline characteristics table.
The association between WWI and UI was accessed by multivariable logistic regressions in three different models. Model 1, no covariates were adjusted; Model 2 was adjusted for gender, age, and race; Model 3 was adjusted for gender age, race, BMI, education level, marital status, the family PIR, smoking status, alcohol intaking, vigorous activity, moderate activity, diabetes, and hypertension. In subgroup analysis, stratified multivariable logistic regression models were utilized to explore the relationship between WWI and UI in different subgroups. The predictive capability of WWI, BMI and WC for UI was evaluated by the receiver operating characteristic (ROC) curve and the area under curve (AUC). Delong et al.’s test [19] was used to compare the difference in AUC between WWI and BMI, WC. A two-sided p value of < 0.05 was considered statistically significant. All statistical analyses were conducted using EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc.) and statistical software packages R (http://www.R-project.org; The R Foundation).
Results
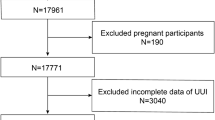
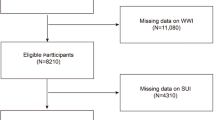
A total of 47,954 participants who completed the examination of body measures and the questionnaire on kidney conditions were enrolled at first. We excluded participants with missing WWI data (n = 2947), incomplete UI data (n = 3154), missing covariates data [missing BMI data (n = 123), education level (n = 33), marital status (n = 17), hypertension (n = 12), diabetes (n = 13), vigorous activity (n = 7), moderate activity (n = 10), and smoking status (n = 24)]. Finally, 41,614 survey individuals were included in this study (Fig. 1).
Participant characteristics
The weighted baseline characteristics are shown in Table 1. A total of 41,614 participants (48.81% males and 51.19% females, weighted proportions) with a weighted mean (SE) age of 46.98 (0.20) years were enrolled in this study. Of these participants, 23.57% had a self-reported history of SUI, 19.24% complained of UUI, and 9.43% had MUI. WWI was set as four categories (7.59–10.47, 10.48–11.05, 11.06–11.63, and 11.64–15.70) by the quartiles. Participants with an elevated WWI quartile had a higher prevalence of all types of UI (all p < 0.001).
Association between WWI and UI
Weighted multivariable logistic regression models were used to evaluate the relationship between WWI and UI in crude, minimally, and fully adjusted models (Model 1, Model 2, and Model 3, respectively), and WWI was designed as a continuous and categorical variable (Q1–Q4) in the analysis. In model 3, a one-unit increase in WWI was related to the higher odds of all types of UI [SUI: odds ratio (OR) = 1.19, 95%Confidence interval (95%CI) 1.13–1.25; UUI: OR = 1.18, 95%CI 1.13–1.24; MUI: OR = 1.19, 95%CI 1.11–1.27, all p < 0.001, Table 2]. In addition, the further analysis indicated that survey individuals in the highest WWI quartile (Q4) had increased risks of all types of UI than those in the lowest WWI quartile (Q1) in model 3 (SUI: OR = 1.52, 95%CI 1.35–1.71; UUI: OR = 1.50, 95%CI 1.33–1.69; MUI: OR = 1.55, 95%CI 1.32–1.83, all p for trend < 0.001, Table 2).
Subgroup analysis
Subgroup analysis was conducted to explore the potential factors affecting the relationship between WWI and UI. As shown in Fig. 2a, gender, age, and BMI potentially affect the association between WWI and SUI with full adjustment of all covariates except the stratified factor itself (all p for interaction < 0.05). Additionally, in stratified multivariable logistic regression for UUI and MUI (Fig. 2b, c, respectively), stronger relationships were observed in male participants than in females (both p for interaction < 0.001). Furthermore, WWI was still significantly positively correlated with the prevalence of three types of UI in all analyzed subgroups. Detailed information has been shown in Fig. 2.
Subgroup analysis for the correlation between WWI and three types of UI. Stratified factors included gender, age, BMI, smoking status, diabetes, and hypertension. All analyses were adjusted by gender, age, race, education, marital status, the family PIR, BMI, hypertension, diabetes, vigorous activity, moderate activity, smoking status, and alcohol intaking, except the stratified factor itself
The predictive performance of WWI, BMI, and WC for UI
The AUC values of three adiposity indicators for predicting three types of UI were shown: 0.638 vs. 0.578 vs. 0.542 (WWI vs. BMI vs. WC for SUI); 0.640 vs. 0.583 vs. 0.587 (WWI vs. BMI vs. WC for UUI); 0.663 vs. 0.599 vs. 0.580 (WWI vs. BMI vs. WC for MUI). WWI had the highest AUC value for predicting all types of UI among the three anthropometric indexes (Table 3). The ROC curve and Delong et al.’s test compared the differences in AUC values for predicting all types of UI between WWI and BMI, WC and found that WWI had a better predictive ability for UI than BMI and WC (all p < 0.001) (Fig. 3).
Discussion
In the current study, we used the data from the NHANES database 2001–2018 to investigate the relationship between WWI and UI in the United State non-institutionalized residents. The results demonstrated that a higher WWI was associated with a greater risk of three types of UI. Additionally, regarding WWI as a categorical variable, the strong positive association between WWI and the prevalence of three types of UI was still observed. Furthermore, subgroup analysis indicated that gender, age, and BMI were potential factors for the association between WWI and SUI, and gender was the effect modifier for the relationship between WWI and UUI, MUI. Moreover, in all subgroups, WWI was significantly positively linked with the increased likelihood of UI. Lastly, the ROC curve and Delong et al.’s test were used to evaluate the predictive power of WWI, BMI, and WC for UI, and found that WWI had a better predictive performance for three types of UI.
It has been shown that some factors are closely associated with the incidence of UI, including but not limited to age, parity, obesity, diabetes mellitus, the history of hysterectomy or pelvic surgery, and cardiorespiratory diseases [20]. While obesity has been confirmed as a recognized risk factor of UI, the connection between obesity and UI is not clear. It is speculated that elevated body weight increases abdominal pressure, and after that bladder pressure and urethral mobility increase, which results in SUI [21]. Additionally, obesity increases abdominal pressure, consequently exacerbating detrusor instability, leading to UUI [22]. Many studies investigated the positive association between obesity and UI. The Finnish National Nocturia and Overactive Bladder Study showed that obesity was connected with a higher risk of SUI (OR = 1.9, 95%CI 1.2–3.0) and UUI (OR = 3.0, 95%CI 1.2–7.4) in women [23]. An elderly EXERNET multi-center study found that compared to women without UI, higher BMI, body fat percentage, and WC were observed in postmenopausal females elder than 65 years old with UI (all p < 0.05) [24]. According to a Korean National Health and Nutrition Examination Survey, Park et al. used dual energy X-ray absorptiometry (DEXA) to evaluate the association between obesity and UI and discovered that many adiposity indexes were positively correlated with UI in women [25]. In addition, central obesity is closely associated with UI. Han et al. demonstrated that a positive relationship between SUI and abdominal obesity was observed in Korean women [26]. A cross-sectional survey including 19,024 women in China showed that central obesity (WC ≥ 80 cm of women) was considered a potential risk factor for SUI [27]. Furthermore, loss of muscle mass was also related to UI. Erdogan et al. indicated that UI was independently related to sarcopenia when muscle mass was adjusted by weight and to low muscle mass when muscle mass was adjusted by weight or BMI [28]. A prospective observational cohort study found that women aged 70 or older had higher odds of new or persistent SUI if their muscle grip strength decreased by 5% or more (adjusted OR = 1.60, p = 0.04) [29]. Parker-Autry et al. demonstrated that compared to women without incident UI, women with incident UI had greater odds of sarcopenia development (OR = 1.70, 95%CI 1.0–2.9) [30]. It has been reported that WWI was positively associated with abdominal obesity, including total abdominal fat area, subcutaneous fat area, and visceral fat area [31]. Moreover, the negative correlation between WWI and muscle mass has been proven [14, 31]. WWI as a novel anthropometric indicator has the capability to reveal the association between obesity and UI. Therefore, it is reasonable to assume that an elevated WWI was linked to a greater likelihood of UI.
There are various anthropometric indexes assessing adiposity levels and BMI is the most widely used obesity parameter. However, it has been shown that BMI does not have the power to differentiate between lean mass and body fat percentage [32]. In addition, BMI cannot evaluate the locations of body fat deposition, leading to the inability of assessing abdominal obesity [33]. Moreover, BMI has a poor sensitivity for detecting obesity when BMI is no less than 30 kg/m2 [34]. Furthermore, the concept of the obesity paradox reveals that a higher BMI is correlated with a lower risk of cardiovascular events and better survival in patients with coronary artery disease [35]. Therefore, the limitations of BMI cannot be ignored while using it to evaluate obesity. WC as a simple indicator is used to evaluate central obesity. A cross-sectional study conducted for older women in southern Brazil demonstrated that compared to the lowest WC group (WC ≤ 79 cm), the odds of UI had a greater increase in the 79–86 cm group (OR: 1.98, 95%CI 1.13–1.45), the 86–94 cm group (OR: 2.07, 95%CI 1.16–3.69), and the highest WC group (WC > 94 cm) (OR: 2.24, 95%CI 1.26–3.99), revealing that WC was considered a significant obesity indicator for UI [36]. A cross-sectional survey in Korea showed that WC may be a more sensitive predictor for the relationship between obesity and UI in the elderly than BMI [37]. However, the obesity paradox was also observed when WC was used to explore the association between obesity and the clinical outcomes of heart failure [38]. These limitations of regular obesity indicators suggested that a more clinically applicable index was currently strongly needed. WWI proposed by standardizing WC based on body weight was positively correlated with cardiometabolic morbidity and mortality [13], indicating the phenomenon ‘obesity paradox’ was not obvious when WWI was utilized to assess obesity. Additionally, WWI is calculated with a simple formula, resulting in a convenient application in clinical examination. Moreover, in our study, the significantly stronger prediction for three types of UI was identified with WWI than BMI and WC. Therefore, WWI as a novel anthropometric index evaluating central obesity is greatly positively related to the odds of UI and has good predictive power for UI. More studies are needed to confirm whether WWI has a stronger prediction for the likelihood of other diseases than other traditional obesity indicators.
Our study used a large sample of data obtained from the NHANES database and took the sampling design and weighting into consideration for representing the general population in the United State. However, there are some limitations in the current study. First, due to the cross-sectional nature of this study, the causal association between WWI and UI cannot be explored. In addition, the NHANES database only represents the population in the U.S. and the association between WWI and UI is needed to be verified in different national populations by more investigations. Moreover, due to the limitation of questionnaire design for UI within the NHANES database, participants self-reported symptoms and history related to the three types of UI during interviews. This methodology likely resulted in an underestimation of the actual number of UI among individuals. Due to differences in participants' interpretation of questions, variations in educational background, and other potential factors, the design of self-reported questionnaire may have an impact on differences in survey individuals’ subjective assessment of their health statuses, thereby potentially introducing bias into the data analysis process. The utilization of a binary response format questionnaire within the database to evaluate patients with UI may increase bias because of subjective factors and overlook the variations in the severity of UI across the population. The binary and self-reporting assessment in this database warrants significant attentions. Lastly, although we adjusted several potential covariates in the current study, we could not entirely eliminate the impact of other conceivable confounding factors.
Conclusion
To our knowledge, this is the first cross-sectional study exploring the relationship between WWI and UI in the United State adult population. In the current study, an elevated WWI was associated with a higher likelihood of UI. In addition, WWI had a stronger predictive power for UI compared to BMI and WC, indicating that WWI may be a better anthropometric index to evaluate UI. However, our findings are needed to be investigated by more prospective studies.
Availability of data and materials
Publicly available datasets were analyzed in the present study. All detailed data can be found here: www.cdc.gov/nchs/nhanes/.
References
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318(16):1592–604.
Vaughan CP, Markland AD. Urinary incontinence in women. Ann Intern Med. 2020;172(3):Itc17–32.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8.
Gacci M, Sakalis VI, Karavitakis M, Cornu JN, Gratzke C, Herrmann TRW, et al. European Association of Urology Guidelines on male urinary incontinence. Eur Urol. 2022;82(4):387–98.
Muth CC. Urinary incontinence in women. JAMA. 2017;318(16):1622.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Ganz ML, Smalarz AM, Krupski TL, Anger JT, Hu JC, Wittrup-Jensen KU, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75(3):526–32.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–50.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32(6):959–66.
Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020;49(3):810–23.
Mahmoud I, Al-Wandi AS, Gharaibeh SS, Mohamed SA. Concordances and correlations between anthropometric indices of obesity: a systematic review. Public Health. 2021;198:301–6.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8(1):16753.
Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. 2021;50(3):780–6.
Shang X, Fu Y, Jin X, Wang C, Wang P, Guo P, et al. Association of overweight, obesity and risk of urinary incontinence in middle-aged and older women: a meta epidemiology study. Front Endocrinol (Lausanne). 2023;14:1220551.
Park S, Baek KA. Association of general obesity and abdominal obesity with the prevalence of urinary incontinence in women: cross-sectional secondary data analysis. Iran J Public Health. 2018;47(6):830–7.
Choi JM, Jiang J, Chang J, Ziogas A, Jiang L, Anton-Culver H. eImpact of lifetime obesity on urinary incontinence in the women’s health initiative. J Urol. 2022;207(5):1096–104.
Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, et al. National Health and Nutrition Examination Survey: sample design, 2007–2010. Vital Health Stat 2. 2013;160:1–23.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Aoki Y, Brown HW, Brubaker L, Cornu JN, Daly JO, Cartwright R. Urinary incontinence in women. Nat Rev Dis Primers. 2017;3:17042.
Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182(6 Suppl):S2-7.
Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS. Weight loss: a novel and effective treatment for urinary incontinence. J Urol. 2005;174(1):190–5.
Vaughan CP, Auvinen A, Cartwright R, Johnson TM 2nd, Tähtinen RM, Ala-Lipasti MA, et al. Impact of obesity on urinary storage symptoms: results from the FINNO study. J Urol. 2013;189(4):1377–82.
Moreno-Vecino B, Arija-Blázquez A, Pedrero-Chamizo R, Alcázar J, Gómez-Cabello A, Pérez-López FR, et al. Associations between obesity, physical fitness, and urinary incontinence in non-institutionalized postmenopausal women: the elderly EXERNET multi-center study. Maturitas. 2015;82(2):208–14.
Park YW, Lee JH. Female urinary incontinence and obesity assessed by anthropometry and dual-energy X-ray absorptiometry: analysis from the 2008–09 Korean National Health and Nutrition Examination Survey. Low Urin Tract Symptoms. 2019;11(2):O28-o33.
Han MO, Lee NY, Park HS. Abdominal obesity is associated with stress urinary incontinence in Korean women. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(1):35–9.
Zhu L, Lang J, Liu C, Han S, Huang J, Li X. The epidemiological study of women with urinary incontinence and risk factors for stress urinary incontinence in China. Menopause. 2009;16(4):831–6.
Erdogan T, Bahat G, Kilic C, Kucukdagli P, Oren MM, Erdogan O, et al. The relationship between sarcopenia and urinary incontinence. Eur Geriatr Med. 2019;10(6):923–9.
Suskind AM, Cawthon PM, Nakagawa S, Subak LL, Reinders I, Satterfield S, et al. Urinary incontinence in older women: the role of body composition and muscle strength: from the health, aging, and body composition study. J Am Geriatr Soc. 2017;65(1):42–50.
Parker-Autry C, Houston DK, Rushing J, Richter HE, Subak L, Kanaya AM, et al. Characterizing the functional decline of older women with incident urinary incontinence. Obstet Gynecol. 2017;130(5):1025–32.
Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH. Associations between weight-adjusted waist index and abdominal fat and muscle mass: multi-ethnic study of atherosclerosis. Diabetes Metab J. 2022;46(5):747–55.
Poirier P. Adiposity and cardiovascular disease: are we using the right definition of obesity? Eur Heart J. 2007;28(17):2047–8.
Franzosi MG. Should we continue to use BMI as a cardiovascular risk factor? Lancet. 2006;368(9536):624–5.
Romero-Corral A, Somers VK, Sierra-Johnson J, Jensen MD, Thomas RJ, Squires RW, et al. Diagnostic performance of body mass index to detect obesity in patients with coronary artery disease. Eur Heart J. 2007;28(17):2087–93.
Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–78.
Krause MP, Albert SM, Elsangedy HM, Krinski K, Goss FL, daSilva SG. Urinary incontinence and waist circumference in older women. Age Ageing. 2010;39(1):69–73.
Kim IH, Chun H, Kwon JW. Gender differences in the effect of obesity on chronic diseases among the elderly Koreans. J Korean Med Sci. 2011;26(2):250–7.
Clark AL, Fonarow GC, Horwich TB. Waist circumference, body mass index, and survival in systolic heart failure: the obesity paradox revisited. J Card Fail. 2011;17(5):374–80.
Acknowledgements
None.
Funding
This work was supported by Sichuan Science and Technology Program (2022YFS0133 and 2022NSFSC1526).
Author information
Authors and Affiliations
Contributions
SC, XH, and YT performed the data analysis. SC, YW, YT, KW, and WY collected the data. SC XH and XL designed this study and drafted and reviewed the manuscript. All authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Research Ethics Review Board of the National Center for Health Statistics. All methods and procedures were conducted in accordance with the relevant guidelines and regulations (Declaration of Helsinki). The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cao, S., Hu, X., Tang, Y. et al. Weight-adjusted-waist index is positively associated with urinary incontinence: results from the National Health and Nutrition Examination Survey (NHANES) 2001–2018. Eur J Med Res 29, 368 (2024). https://doi.org/10.1186/s40001-024-01971-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01971-9