Abstract
Purpose
Respiratory dysfunction is one of the most frequent symptoms observed during sepsis reflecting hypoxemia and/or acidosis that may be assessed by the ROX index (ratio of oxygen saturation by pulse oximetry/fraction of inspired oxygen to respiratory rate). This study aimed to describe the relationship between the prehospital ROX index and 30-day mortality rate among septic shock patients cared for in the prehospital setting by a mobile intensive care unit (MICU).
Methods
From May 2016 to December 2021, 530 septic shock patients cared for by a prehospital MICU were retrospectively analysed. Initial ROX index value was calculated at the first contact with MICU. A Cox regression analysis after propensity score matching was performed to assess the relationship between 30-day mortality rate and a ROX index ≤ 10.
Results
Pulmonary, digestive and urinary sepsis were suspected among 43%, 25% and 17% patients, respectively. The 30-day overall mortality reached 31%. Cox regression analysis showed a significant association between 30-day mortality and a ROX index ≤ 10: adjusted hazard ratio of 1.54 [1.08–2.31], p < 0.05.
Conclusions
During the prehospital stage of septic shock patients cared for by a MICU, ROX index is significantly associated with 30-day mortality. A prehospital ROX ≤ 10 value is associated with a 1.5-fold 30-day mortality rate increase. Prospective studies are needed to confirm the ability of prehospital ROX to predict sepsis outcome since the prehospital setting.
Similar content being viewed by others
Background
Every year sepsis concern more than 50 million people worldwide despite research performed during the last 40 years. Sepsis still remains a major health problem [1,2,3] with an increasing incidence and high morbidity and mortality despite of recent advances in its management [1, 4,5,6,7,8,9]. Every year nearly 11 million deaths worldwide are due to sepsis [3]. The overall sepsis mortality rate still reaches 30% at 28 days but is higher, i.e., 50% for the most severe form of sepsis, i.e., septic shock [10, 11].
Since 2017, the World Health Assembly and the World Health Organization adopted resolutions to improve, prevent, diagnose, and sepsis management [12] to reduce health impact of sepsis.
Sepsis recognition and severity assessment are mainly based on clinical judgement and scoring [13]. When the resources are scarce, e.g., in the extra hospital setting, the initial sepsis diagnose is often difficult while it is widely admitted that early detection and treatment instauration improve patient outcome [14,15,16]. Due to the lack of a clinical sign specificity for sepsis, scores and indexes were developed and are widely used to help or guide physicians in the daily bedside decision-making process.
Sepsis may lead to multi-organ dysfunction including cardiovascular, respiratory, renal, neurological, hematological, and hepatic dysfunctions. Independently of its origin, sepsis induces a metabolic acidosis caused by renal injury and tissue hypoperfusion and/or hypoxemia related to organs dysfunction [17,18,19]. The respiratory dysfunction is one of the most frequent observed during sepsis and septic shock. Hypoxemia and/or acidosis induce as respiratory rate increase and partial pressure of oxygen (PaO2/FiO2) decrease. Beyond these pathophysiological considerations, in and out of hospital epidemiological studies report sepsis mainly comes from respiratory (50%) and digestive (25%) and less frequently from urinary tract (5%) [20,21,22].
The clinical usefulness of the ROX index, oxygen saturation divided by the inspired oxygen concentration (FiO2), and then by the respiratory rate, was described first in 2016 [23] among patients suffering from pulmonary disease and confirmed by other studies [24, 25]. Recently, Lee et al. reported that the ROX index was lower in non-survivors with a ROX index cutoff less than or equal to 10 suggesting that the ROX index could be used as a prognostic marker in sepsis among adult patients admitted to the emergency department with a sepsis or septic shock diagnosis [26].
This retrospective study aims to describe the relationship between prehospital ROX index and 30-day mortality rate among septic shock patients cared for in prehospital setting by a mobile intensive care unit (MICU).
Methods
Patients
As previously reported [27], in France prehospital emergency medical service is named SAMU (Urgent Medical Aid Service). SAMU is a phone call centre responding to the patients’ complaints [28] to determine the best care pathway. For life-threatening emergencies, a mobile intensive care unit (MICU) may be dispatched to the scene [29].
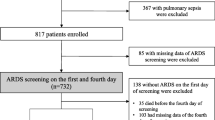
From May 2016 to December 2021, prehospital septic shock patients according to the 2012 sepsis-2 conference criteria [30] extrinsically applied by the MICU physicians of 9 French hospital centres (Necker-Enfants malades Hospital, Lariboisière Hospital, La Pitié Salpêtrière Hospital, Hotel Dieu Hospital, APHP, Paris—France; The Paris Fire Brigade Paris—France; The Toulouse University Health Centre, Toulouse—France and the Castres Hospital, Castres—France), were retrospectively analyzed. Patients younger than 18 years, and/or pregnant, and/or with serious comorbid conditions with an unknown prehospital life support and/or with guardianship or curatorship were not included in the dataset [31]. The operative sepsis-2 definition considering a septic shock a condition of refractory hypotension despite vascular filling or normotension with hypoperfusion signs was chosen because prehospital lactatemia assessment is not possible in all French MICU.
Patients’ demographic characteristics, presumed prehospital origin of sepsis, the first recorded MICU contact prehospital and the last prehospital vital sign values [systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP)] were collected for the dataset. Heart rate (HR), pulse oximetry (SpO2), respiratory rate (RR), body core temperature, and Glasgow coma scale (GCS), plasma blood glucose concentration, duration of prehospital care, and prehospital treatments delivered (ABT type and dose, fluid volume expansion type and dose, as well as catecholamine type and dose, mechanical ventilation) collected for the dataset. Comorbidities reflecting the underlying condition [32] were also reported: hypertension, coronary heart disease, chronic cardiac failure, chronic renal failure, chronic obstructive pulmonary disease, history of cancer, diabetes mellitus were also collected to take into account. Body mass index (BMI) was calculated by dividing weight (kg) by [height (m) * height (m)].
Length of stay (LOS) in the ICU, in-hospital LOS and 30-day mortality were retrieved from medical reports in case of in-hospital death or by call when the patient was discharged from the hospital. The Simplified Acute Physiology Score (SAPS-2) was calculated 24 h after ICU admission [33].
The ROX index was calculated by dividing the initial values, e.g., at the first MICU contact of prehospital patient’s pulse oximetry prior any oxygen supplementation, by the inspired oxygen concentration (FiO2), and then by the RR [23].
To minimize data abstraction bias [34], the data collection was performed by a single investigator (RJ) using a standardized abstraction template established prior the study. To minimise transcription errors, two investigators (TF and PG) re-check the data and identified no error.
Ethical considerations
The study was approved by the French Society of Anaesthesia and Intensive Care ethics committee on December 12th, 2017 (Ref number: IRB 00010254-2017-026). According to the French law, this non-interventional retrospective observational study the ethical committee waived consent of patients.
Statistical analysis
Results are expressed as mean with standard deviation and interquartile range [Q1–Q3], and as absolute value and percentage depending on the type of variable.
ROX index was analyzed as a continuous variable and as qualitative variable using a threshold of ROX ≤ 10 for abnormal value according to Lee et al. study reporting that a ROX index ≤ 10 is an independent prognostic factor for 28-day mortality in patients with sepsis or septic shock admitted to the emergency department [26] suggesting that ROX index could be useful for sepsis prognostication.
To reduce the effect of confounders on 30-day mortality and on ROX calculation, a propensity score matching was performed to balance the differences in baseline characteristics between patients with prehospital ROX ≤ 10 and those with prehospital ROX > 10 [35]. The propensity score was estimated using logistic regression based on potential confounders on 30-day mortality and on ROX calculation: age, chronic cardiac failure, chronic renal failure, chronic obstructive pulmonary disease, coronary heart disease, BMI, history of cancer, diabetes mellitus, SAPS-2, prehospital fluid expansion [31] and prehospital antibiotic therapy (ABT) administration [9]. The nearest neighbour matching method was used to match patients based on the logit of the propensity score [35]. The balance of covariates after matching was assessed by absolute mean differences with a threshold of 10% [36].
Imbalance matching was assessed with standardized mean deviation. Baseline characteristics were compared between cases and controls by paired tests in the matched sample.
In the propensity score-matched cohort, a survival analysis using Cox proportional hazard regression was used to compare 30-day mortality rate according to a prehospital ROX ≤ 10 and a prehospital ROX > 10. Proportional hazards assumption was verified for each Cox model variable by Kaplan–Meier curves and the log-rank test. Results are expressed by an adjusted Hazard ratio (HRa) with 95 percent confidence intervals [95 CI].
All tests were two-sided with a statistically significant p value of < 0 0.05. All analyses were performed using R 3.4.2 (http://www.R-project.org; the R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
Five-hundred and thirty septic shock patients among which 341 patients were male gender (64%) with a mean age of 69 ± 15 years cared for by a MICU were retrospectively analyzed. The mean SAPS-2 score was 60 ± 21. The median length of stay in a hospital was 10 [5–18] days and the ICU length of stay was 4 [2–8] days (Table 1).
Pulmonary, digestive and urinary infections were suspected in 43%, 25% and 17% of the cases, respectively (Table 2).
The 30-day overall mortality rate reached 31% (165 patients).
Among the 132 patients (25%) who received prehospital ABT, 98 patients (74%) received a 3rd generation cephalosporin (40% cefotaxime and 60% ceftriaxone) without any reported adverse event related to prehospital ABT administration.
All patients received crystalloids infusion for prehospital hemodynamic optimization with a median fluid expansion volume of 750 [500–1000] ml. Norepinephrine infusion was delivered to 155 patients (29%) with a median dose of 1.0 [0.5–2.0] mg h−1 (Table 1).
Main measurement
In the overall population, the mean initial ROX was 15.81 ± 5.94 and 117 patients (22%) had a prehospital ROX ≤ 10. Table 1 reports the comparison between patients with prehospital ROX ≤ 10 and prehospital ROX > 10 before propensity score matching.
After propensity score matching for prehospital ROX ≤ 10, 68 patients with a prehospital ROX ≤ 10 were compared with 57 patients with a prehospital ROX > 10. Comparisons are reported in Table 3 and the absolute mean differences between subgroups after propensity score matching are depicted in Fig. 1.
Using Cox regression analysis on matched population, we observed a significant association between 30-day mortality and prehospital ROX ≤ 10 with an aHR of 1.54 [1.08–2.31] (p < 0.05). Cox regression analysis results are summarized in Table 4.
Figure 2 depicts Kaplan–Meier curves after confounder adjustment for 30-day survival between prehospital ROX > 10 and prehospital ROX ≤ 10 after matching (Fig. 2).
Discussion
In this study, we report a significant association between 30-day mortality and prehospital ROX index. An initial prehospital ROX index < 10 is associated with a 1.5-fold 30-day mortality increase among septic shock patients cared for by a MICU in the prehospital setting.
Early identification of septic patients at risk of poorer evolution and an high mortality is crucial because they are those who most need and most benefit from an early, aggressive therapeutic management, one of the key-element allowing sepsis mortality decrease [14].
Excluding shock, for sepsis severity assessment, clinical signs may be not sufficient because of their lack sensitivity and specificity. Consequently, to try to fill this gap, scoring was developed [13]. Initial scoring was based on clinical signs and thereafter, biological elements were added to improve performances. The most-known scores for sepsis are SOFA and SAPS-2 scores [33, 37], both developed and validated in the ICU and in the ED. However, both, SOFA and SAPS-2, because requiring biological results needing few hours to be established, are not usable in prehospital practice, where the resources are scarce. To solve this issue, qSOFA score has been proposed [14] but its validity still remains under debate [38, 39]; to date, no score is validated in the prehospital setting [40, 41]. More recently, biomarker addition to scores was proposed to improve efficiency. Lactatemia is validated [42] and recognized as useful biomarker for sepsis severity and risk of mortality assessment [43], despite lactate point of care testing validity is, to date, not widely available easily in the out-of-hospital setting. Base excess and bicarbonate plasma level appears to be alternatives to lactate [44], by reflecting tissue hypoperfusion, but have not been evaluated in the prehospital setting.
Because the ROX index is a simple clinical tool, obtained in real time, easily, noninvasively measurable clinically or with a simple monitoring system, it appears to be helpful for physicians’ daily practices. Although the ROX threshold varies according to study populations [23, 26, 45], it appears that a higher value is associated with a worse prognosis. The ROX index evaluation presents the advantage not being influenced to subjectivity contrary to skin mottling score and capillary refill time assessment [46]. However, currently respiratory rate evaluation is not accurate, especially for the less sick patients [47] and could limit the ROX index use in daily practice. To improve respiratory rate accuracy measurement, devices allowing a continuous measurement [48], and smartphone applications were developed and are now available for in and out-of-hospital practice [49].
Limitations
This study presents limitations. First, this is a retrospective analysis. Second, bias from misclassification of covariates might exist, because data were manually extracted from prehospital and in-hospital medical reports. Third, the statistical analysis does not allow any conclusion on causality. Fourth, this study focused only patients with shock, not all patients with sepsis. Finally, we only assessed the association between 30-day mortality and the first ROX index measured after MICU contact before any oxygen supplementation and did not evaluate the dynamic change in the ROX index.
Beyond all these limitations, the ROX index appears to be useful since the prehospital setting to, earlier, screen septic shock patients with a higher risk of poorer outcome.
Conclusions
Among septic shock patients cared for by a prehospital MICU, a significant association between ROX index and 30-day mortality exists. A 1.5-fold 30-day mortality increase is observed when the prehospital ROX is lower or equal than 10. Further prospective studies are needed to confirm these preliminary results and evaluate the ability of prehospital ROX to predict sepsis outcome since the prehospital setting.
Availability of supporting data
Data will be made available on reasonable request.
Abbreviations
- SS:
-
Septic shock
- MICU:
-
Mobile intensive care unit
- aHR:
-
Adjusted hazard ratio
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- SAMU:
-
Urgent Medical Aid Service
- SMUR:
-
Mobile Emergency and Resuscitation Service
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MAP:
-
Mean arterial pressure
- HR:
-
Heart rate
- SpO2 :
-
Pulse oximetry
- RR:
-
Respiratory rate
- GCS:
-
Glasgow coma scale
- LOS:
-
Length of stay
- SOFA:
-
Sequential Organ Failure Assessment
- qSOFA:
-
Quick Sequential Organ Failure Assessment
- SAPS-2:
-
Simplified Acute Physiology Score
- FiO2 :
-
Inspired oxygen concentration
- BMI:
-
Body mass index
References
Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–72.
Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41(5):1167–74.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet. 2020;395(10219):200–11.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European society of intensive care medicine. Intensive Care Med. 2014;40(12):1795–815.
Luhr R, Cao Y, Soderquist B, Cajander S. Trends in sepsis mortality over time in randomised sepsis trials: a systematic literature review and meta-analysis of mortality in the control arm, 2002–2016. Crit Care. 2019;23(1):241.
Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318(13):1241–9.
Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014;42(3):625–31.
Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311(13):1308–16.
Peake SL, Delaney A, Bailey M, Bellomo R, et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371(16):1496–506.
Ferrer R, Artigas A, Levy MM, Blanco J, Gonzalez-Diaz G, Garnacho-Montero J, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299(19):2294–303.
Nguyen HB, Van Ginkel C, Batech M, Banta J, Corbett SW. Comparison of predisposition, insult/infection, response, and organ dysfunction, acute physiology and chronic health evaluation II, and mortality in emergency department sepsis in patients meeting criteria for early goal-directed therapy and the severe sepsis resuscitation bundle. J Crit Care. 2012;27(4):362–9.
ASSEMBLY SWH. Improving the prevention, diagnosis and clinical management of sepsis. 2017.
Guirgis FW, Jones L, Esma R, Weiss A, McCurdy K, Ferreira J, et al. Managing sepsis: electronic recognition, rapid response teams, and standardized care save lives. J Crit Care. 2017;40:296–302.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
Chen AX, Simpson SQ, Pallin DJ. Sepsis guidelines. N Engl J Med. 2019;380(14):1369–71.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–143.
Jung B, Martinez M, Claessens YE, Darmon M, Klouche K, Lautrette A, et al. Diagnosis and management of metabolic acidosis: guidelines from a French expert panel. Ann Intensive Care. 2019;9(1):92.
Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348(2):138–50.
Madias NE. Lactic acidosis. Kidney Int. 1986;29(3):752–74.
Brun-Buisson C, Meshaka P, Pinton P, Vallet B, EPISEPSIS Study Group. EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004;30(4):580–8.
Jouffroy R, Gilbert B, Tourtier JP, Bloch-Laine E, Ecollan P, Boularan J, et al. Prehospital bundle of care based on antibiotic therapy and hemodynamic optimization is associated with a 30-day mortality decrease in patients with septic shock. Crit Care Med. 2022;50(10):1440–8.
Jouffroy R, Gilbert B, Hassan A, Tourtier JP, Bloch-Laine E, Ecollan P, et al. Adequacy of probabilistic prehospital antibiotic therapy for septic shock. Am J Emerg Med. 2022;53:80–5.
Roca O, Messika J, Caralt B, Garcia-de-Acilu M, Sztrymf B, Ricard JD, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016;35:200–5.
Bilan N, Dastranji A, Ghalehgolab BA. Comparison of the SpO2/FiO2 ratio and the PaO2/FiO2 ratio in patients with acute lung injury or acute respiratory distress syndrome. J Cardiovasc Thorac Res. 2015;7(1):28–31.
Chen W, Janz DR, Shaver CM, Bernard GR, Bastarache JA, Ware LB. Clinical characteristics and outcomes are similar in ARDS diagnosed by oxygen saturation/FiO2 ratio compared with PaO2/FiO2 ratio. Chest. 2015;148(6):1477–83.
Lee CU, Jo YH, Lee JH, Kim J, Park SM, Hwang JE, et al. The index of oxygenation to respiratory rate as a prognostic factor for mortality in sepsis. Am J Emerg Med. 2021;45:426–32.
Jouffroy R, Gilbert B, Tourtier JP, Bloch-Laine E, Ecollan P, Bounes V, et al. Impact of prehospital antibiotic therapy on septic shock mortality. Prehosp Emerg Care. 2020;25:1–8.
Jouffroy R, Saade A, Muret A, Philippe P, Michaloux M, Carli P, et al. Fluid resuscitation in pre-hospital management of septic shock. Am J Emerg Med. 2018;36(10):1754–8.
Adnet F, Lapostolle F. International EMS systems: France. Resuscitation. 2004;63(1):7–9.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228.
Jouffroy RGB, Gueye P, Tourtier JP, Bloch-laine E, et al. Prehospital hemodynamic optimisation is associated with a 30-day mortality decrease in patients with septic shock. Am J Emerg Med. 2021;45:105–11.
Salvatore F. The shift of the paradigm between ageing and diseases. Clin Chem Lab Med. 2020;58(10):1635–44.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Gearing RE, Mian IA, Barber J, Ickowicz A. A methodology for conducting retrospective chart review research in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2006;15(3):126–34.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. 1996;22(7):707–10.
Askim A, Moser F, Gustad LT, Stene H, Gundersen M, Asvold BO, et al. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality—a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resusc Emerg Med. 2017;25(1):56.
Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care. 2017;21(1):73.
Jouffroy R, Saade A, Carpentier A, Ellouze S, Philippe P, Idialisoa R, et al. Triage of septic patients using qSOFA criteria at the SAMU regulation: a retrospective analysis. Prehosp Emerg Care. 2018;22(1):84–90.
Jouffroy R, Saade A, Ellouze S, Carpentier A, Michaloux M, Carli P, et al. Prehospital triage of septic patients at the SAMU regulation: comparison of qSOFA, MRST, MEWS and PRESEP scores. Am J Emerg Med. 2018;36(5):820–4.
Leguillier T, Jouffroy R, Boisson M, Boussaroque A, Chenevier-Gobeaux C, Chaabouni T, et al. Lactate POCT in mobile intensive care units for septic patients? A comparison of capillary blood method versus venous blood and plasma-based reference methods. Clin Biochem. 2018;55:9–14.
Kushimoto S, Akaishi S, Sato T, Nomura R, Fujita M, Kudo D, et al. Lactate, a useful marker for disease mortality and severity but an unreliable marker of tissue hypoxia/hypoperfusion in critically ill patients. Acute Med Surg. 2016;3(4):293–7.
Jouffroy R, Laney M, Leguillier T, Nivet-Antoine V, Beaudeux JL. Comparison of blood gas results obtained on Abbott i-Stat(R) and on radiometer ABL 800 Flex(R) analyzers impact for the clinical decision. Ann Biol Clin. 2022;80(6):521–5.
Candel BGJ, de Groot B, Nissen SK, Thijssen W, Lameijer H, Kellett J. The prediction of 24-h mortality by the respiratory rate and oxygenation index compared with National Early Warning Score in emergency department patients: an observational study. Eur J Emerg Med. 2023;30(2):110–6.
Jouffroy R, Saade A, Tourtier JP, Gueye P, Bloch-Laine E, Ecollan P, et al. Skin mottling score and capillary refill time to assess mortality of septic shock since pre-hospital setting. Am J Emerg Med. 2019;37(4):664–71.
Loughlin PC, Sebat F, Kellett JG. Respiratory rate: the forgotten vital sign-make it count! Jt Comm J Qual Patient Saf. 2018;44(8):494–9.
McCartan TA, Worrall AP, Conluain RO, Alaya F, Mulvey C, MacHale E, et al. The effectiveness of continuous respiratory rate monitoring in predicting hypoxic and pyrexic events: a retrospective cohort study. Physiol Meas. 2021;42(6): 065005.
Nakitende I, Namujwiga T, Dunsmuir D, Ansermino JM, Wasingya-Kasereka L, Kellett J. Respiratory rates observed over 15 seconds compared with rates measured using the RRate app. Practice-based evidence from an observational study of acutely ill adult medical patients during their hospital admission. Acute Med. 2020;19(1):15–20.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
RJ conceived the study, prepared the initial protocol, analysed data and drafted the manuscript. RJ, TF, BG, ST, EBL, PE, JB, VB, BV and PG collected data. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the French Society of Anaesthesia and Intensive Care ethics committee on December 12th, 2017 (Ref number: IRB 00010254-2017-026). According to the French law, the French Society of Anaesthesia and Intensive Care ethics committee on December 12th, 2017 (Ref number: IRB 00010254-2017-026) waived consent of patients.
Consent for publication
All authors consent for publication.
Competing interests
No author have conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jouffroy, R., Fabre, T., Gilbert, B. et al. Association between prehospital ROX index with 30-day mortality among septic shock. Eur J Med Res 29, 304 (2024). https://doi.org/10.1186/s40001-024-01902-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01902-8