Abstract
Background
Anemia is a frequently reported and commonly documented issue in intensive care units. In surgical intensive care units, more than 90% of patients are found to be anemic. It is a hematologic factor that contributes to extended mechanical ventilation, sepsis, organ failure, longer hospitalizations in critical care units, and higher mortality. Thus, this study aimed to determine the incidence and identify factors associated with anemia in elective surgical patients admitted to the surgical intensive care unit.
Methods
A retrospective follow-up study involving 422 hospitalized patients was carried out between December 2019 and December 2022 in the surgical intensive care unit after elective surgery at Tikur-Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Data were gathered from the patients’ charts, and study participants were chosen using methods of systematic random sampling. SPSS 26 (the statistical software for social science, version 26) was used to analyze the data. Bivariable and multivariable binary logistic regression were used to examine associations between variables.
Results
The incidence of anemia in elective surgical patients admitted to the intensive care unit was 69.9% (95% CI 65.4–74.5%). American Society of Anesthesiologists’ class III (ASA III) [AOR: 8.53, 95% CI 1.92–13.8], renal failure [AOR:2.53, 95% CI (1.91–5.81)], malignancy [AOR: 2.59, 95% CI (1.31–5.09)], thoracic surgery [AOR: 4.07, 95% CI (2.11–7.87)], urologic surgery [AOR: 6.22, 95% CI (2.80–13.80)], and neurosurgery [AOR: 4.51, 95% CI (2.53–8.03)] were significantly associated with anemia in surgical patients admitted to the intensive care unit.
Conclusion
More than two-thirds of the intensive care unit-admitted surgical patients experienced anemia. An American Society of Anesthesiologists’ (ASA III score), renal failure, malignancy, thoracic surgery, urologic surgery, and neurosurgery were significantly associated with this condition. Early identification helps to institute preventive and therapeutic measures.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) defines anemia as having a hemoglobin level of less than 13 g/dl (hematocrit 39) in males and less than 12 g/dl (hematocrit 36) in non-pregnant women. A reduced number of red blood cells results in a decreased ability of the blood to transfer oxygen to the tissues because hemoglobin is essential for carrying oxygen [1].
Anemia is highly prevalent and frequently observed in intensive care unit (ICU) -admitted patients after surgery. Approximately 67% (2/3) of patients admitted to the ICU on the day of admission have hemoglobin (Hb) less than 12 g/dl and 97% of patients in the ICU have protracted noticeable anemia [2]. In developing countries, the frequency of anemia is significant due to low socioeconomic status and inadequate healthcare services [3].
ICU anemia is strongly linked to poor surgical patient outcomes, including a higher risk of oxygen depletion (reduced blood oxygen-carrying capacity), blood transfusion, extended ICU stays, surgical site infections, resource consumption, prolonged need for mechanical ventilation, more complicated surgery, and advanced treatment [4, 5]. Furthermore, studies show increased requirements for re-intubation and weaning failure in those patients who are anemic [6].
Anemia in ICU-admitted patients poses challenges in both patient management and patient outcomes. This hematologic risk factor raises patient mortality and morbidity. Its adverse outcomes include congestive heart failure, respiratory failure, hypoxia, cardiac arrest, multi-organ failure, chronic kidney disease, failure of weaning from a mechanical ventilator, prolonged hospitalization, infection, and a greater chance of dying [7,8,9]. Anemia is also a great burden for anesthetists and anesthesiologists, as hemoglobin is one of the clinical parameters that determine anesthesia choice and service delivery to the patient [10].
Different techniques were tried to cope with patients with anemia as part of the management plan. Most of the time, anemia in ICU-admitted patients is managed by transfusing packed red blood cells, which improves oxygen delivery to the tissue and decreases tissue hypoxia [11].
However, the transfusion of blood to critically ill patients is potentially dangerous and carries a risk. As blood-transfused patients are immune-compromised most of the time, they are more likely to develop blood transfusion-related complications. Some of the reported complications following transfusion include ALI (acute lung injury), organ dysfunction, systemic infections, and death [12, 13]. Transfusion also increases hospital stay and resource consumption [14].
If anemia exists without obvious factors and if the patient is on certain medications, treatment can be done by withholding the drugs and putting the patient on corticosteroids [5].
However, anemia is an illness that can be treated and prevented and is frequently managed with fewer adverse effects without the need for blood transfusions if it is identified early to decrease blood transfusion and transfusion-related complications [15].
Even though anemia is highly prevalent in ICU-admitted patients, few studies have been conducted to investigate factors associated with it. Therefore, the purpose of this study was to ascertain the incidence of anemia and the factors associated with it in elective adult surgical patients admitted to ICU. It is advantageous for doctors and anesthetists to illustrate various anemia-related factors to lower the risk of transfusions, enhance clinical management, and enhance the quality of anesthesia and surgery.
Methods
Study design, period, and setting
A retrospective follow-up study involving 422 hospitalized patients was carried out between December 2019 and December 2022 in the surgical intensive care unit after elective surgery at Tikur-Anbessa Specialized Hospital (TASH), Addis Ababa, Ethiopia.
Inclusion and exclusion criteria
Inclusion criteria
All patients 18 years of age and above who underwent elective surgery and were admitted to the surgical ICU have been included.
Exclusion criteria
-
No records of baseline hemoglobin or hematocrit
-
Hemolytic anemia as a direct cause of ICU admission
-
Congenital causes of anemia such as sickle cell
-
Patients on treatments for anemia were excluded from the study.
Operational definitions
Hematocrit: the proportion of red blood cells in the blood. Healthy adults typically have hematocrits between 36 and 48% for women and 39–52% for men [16].
Hemoglobin: is a protein that contains iron in RBCs and is responsible for providing oxygen to the cells. It ranges from 12–16 for females and 13–17 for males [16].
Prolonged ICU stay: patients who are admitted to the ICU and stay for more than 8 days [17].
Post-surgery: the period starting from the immediate termination of surgery and till discharge [18].
Postsurgical anemia: is defined as anemia after surgery measured in terms of reduction of hemoglobin less than 13 g/dl for males and less than 12 g/dl for females according to the WHO [19].
Post-surgical anemia in the ICU: anemia developed during any period in the intensive care unit stay [20].
Sample size determination
In the research area, the incidence of anemia among patients hospitalized in the surgical intensive care unit (ICU) and the associated risk factors were unknown. Using the single population formula, the sample size was determined with a 5% margin of error at a 95% confidence interval and a 50% incidence of anemia in surgical patients admitted to the intensive care unit:
In this case, n = (1.96)2 0.5 (1–0.5)/ (0.05)2 = 384, where z, 1.96; p, 0.5; CI, 95%; w, margin of error = 0.05.
To account for the non-response rate, we added 10% of the n (i.e., 384 + 38 = 422); as a result, 422 surgical patients who were hospitalized in the intensive care unit were included in the study.
Sampling technique
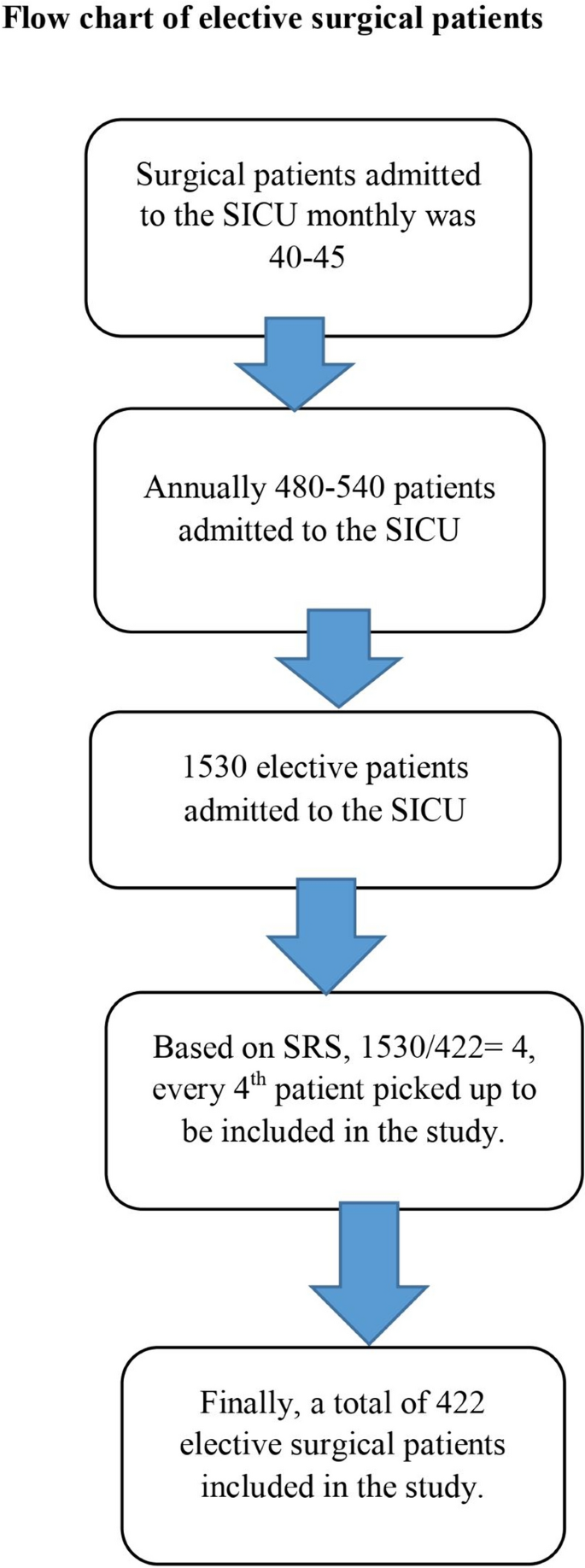
The study participants were chosen using a systematic random sampling technique. The number of surgical patients admitted to the surgical ICU monthly was 40–45 patients. So, on average, 480 to 540 patients are admitted to the surgical ICU annually. Three years of data were taken retrospectively to establish the incidence of anemia and to search out the risk factors. Thus, in 3 years, 1530 patients were admitted to the surgical intensive care unit.
The sampling interval was based on systematic random sampling, and it was 1530/422 = 4. Therefore; every fourth patient was picked up to be included in the study (Fig. 1).
Data collection procedure
Data has been collected from the patient’s chart by using a structured checklist. The questionnaire was designed to collect data on socio-demographic variables (age, sex, and residency), hematologic measurements (hemoglobin and hematocrit), previous surgery, medical status (hypertension, diabetes mellitus, renal failure, cancer, RVI, and heart failure), and drug history (Beta-blocker, calcium channel blocker, ACEIs, HAARTs, and chemotherapies). Blood loss, duration of surgery, duration on a mechanical ventilator, duration of ICU stays, and type of anesthesia employed were also investigated in patients’ medical charts.
Data processing and analysis
Before being imported into Epidata version 4.6 and exported to SPSS version 26 for analysis, the data was first checked, coded, and entered. The collinearity diagnosis test (variance inflation factors, or VIF) and tolerance were used to screen for multicollinearity. The study employed binary logistic regression analysis to investigate potential relationships between the independent factors and the outcome variable. Variables in bivariable regression with a p-value less than 0.2 are added to multivariable logistic regression to assess the strength of the association. Lastly, variables are considered statistically significant if their p-value is less than 0.05. The model's fitness was evaluated using the Hosmer–Lemeshow goodness of fit test. The continuous variables were expressed using the mean and standard deviation. The categorical data have been expressed using percentages and continuous data using mean.
Results
Socio-demographic and clinical characteristics of study participants
This study was conducted on a total of 422 patients who were admitted to the ICU after elective surgery. Of the total study participants, 174 (41.2%) were men, 229 (54.3%) were from rural areas with a mean age of 48 (± 17.7) years. The duration of surgery with mean ± standard deviation was 5.13 ± 1.25 h. The mean time of surgical patients waiting on mechanical ventilators and in the ICU was 8.0 ± 6 and 8.9 ± 6.6 days, respectively. The average volume of blood loss during the surgical procedure was 1380 (± 855) milliliters. Of those surgical patients, the majority of patients were ASA II (58.5%) (Table 1).
Coexisting conditions and medical histories of patients admitted to the intensive care unit following elective surgery
Of the total study participants, 148 (35.1%), 90 (21.3%), and 84 (19.9%) study participants had histories of hypertension, cancer, and two or more diseases, respectively. Regarding treatment factors, 107 (25.4%), 102 (24.2%), 96 (22.7%), and 71 (16.8%) had histories of two or more medications, ACEIs, calcium channel blockers, and chemotherapies, respectively (Table 2).
Incidence of anemia in surgical intensive care unit
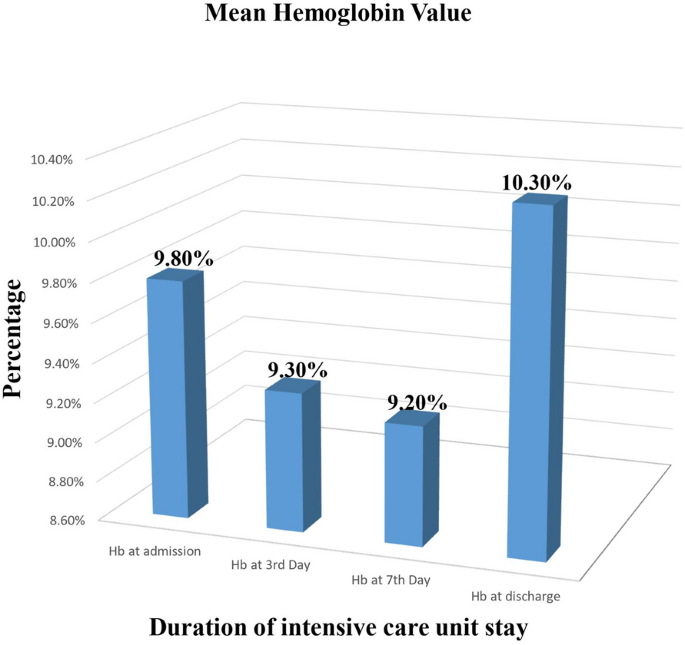
This study found that among patients hospitalized in the surgical intensive care unit following elective surgery, the overall incidence of anemia was 69.9% (95% CI 65.4% to 74.5%). The lowest and highest hemoglobin was noted on the seventh day of ICU admission (9.2 g/dl) and at the time of discharge (10.3 g/dl) respectively (Fig. 2).
Factors associated with anemia in surgical ICU admitted patients
In a bi-variable logistic regression analysis, ASA class, renal failure, malignancy, heart failure, calcium channel blockers, ACE inhibitors, chemotherapy, thoracic surgery, urologic surgery, and neurologic surgery were discovered to be substantially associated with anemia (p-value < 0.2) and were candidates for multivariable logistic regression analysis. In multivariate logistic regression, ASA class III, renal failure, malignancy, thoracic surgery, urologic surgery, and neurologic surgery were found to have a significant association with the outcome variable (Table 3).
Discussion
According to this study, the incidence of anemia in elective surgical ICU-admitted patients was 69.9% (95% CI 65.4% to 74.5%). The lowest hemoglobin level was noted on the seventh day of ICU admission (9.2 g/dl).
This study’s findings were consistent with those of other researches in Germany showing that 66.9% of ICU-admitted surgical patients had anemia (i.e. mean hemoglobin level less than 10 g/dl) during their ICU admission, and there was further decrement in mean hemoglobin level as the ICU stay increased [21].
Similarly, a Polish study found that nearly all patients became anemic during the first three days after ICU admission, and as many as 66% of patients were anemic on the day of admission [13]. Our study also showed that the first three days of ICU admission had a significant impact on hemoglobin concentration, with the biggest drops in hemoglobin occurring during this time and continuing to decline thereafter.
In contrast, the incidence of anemia at admission in our study was higher than the findings of the studies conducted in Greece (43.1%) [22], in Spain (63.31%) [4], in Western Europe (63%) [23], in the United States (57.8%) [24], and in Canada (61.3%) [25]. These differences might happen as a result of the fact differences in sample size and clinical characteristics of the study participants.
The incidence of anemia in our study was lower than in studies in India, reaching 97% within a week of ICU admission with hemoglobin or hematocrit levels below 12 g/dl (36%) [2]. This difference might have occurred because of differences in sample size and inclusion–exclusion criteria.
Further reports in Germany show the frequency of anemia in ICU-admitted patients was 98%, which is too high [26]. This variety has occurred because the study participants they included in this investigation were all on mechanical ventilators.
In Niger, the incidence of anemia in patients admitted to surgical ICU was 86.9% [27]. This was also high as compared with our result. This difference might be due to the inclusion of both emergency and elective surgical patients in their study.
According to this study, ASA physical status III, renal failure, cancer, thoracic, urologic, and neurologic surgery were found to be significantly associated with the incidence of anemia.
Compared to those patients with ASA I and II, patients with ASA status III had an 8.5 times increased risk of developing anemia. Other studies confirmed the ASA physical status class with preexisting co-morbidities increases adverse postoperative surgical outcomes [28]. As the physical status class of ASA increases, postoperative adverse events like morbidity and mortality increase too [28, 29]. As ASA class increases, coexisting medical conditions increase, the stage of disease may advance, and immunity declines resulting in decreased activity of reticuloendothelial cells which contributes to the development of anemia.
According to this study, the risk of developing anemia in surgical patients admitted to ICU was 2.5 times higher in patients with renal failure as compared with those patients without renal failure. This conclusion is consistent with research gained by other authors. Although anemia can occur at various stages of chronic kidney disease (CKD), the incidence of anemia and the severity of CKD are strongly correlated [30].
Renal hormones such as erythropoietin, which regulates the bone marrow's production of red blood cells, are thought to play a role in renal failure. As kidney disease progresses, other factors that lower red cell survival and inhibit marrow erythropoiesis may also contribute to anemia [30].
In our study, anemia was 2.6 times more likely to develop in patients having a history of malignancy than in patients who hadn’t a history of malignancy. Similar studies demonstrated that individuals admitted to the ICU with cancer had a higher frequency of anemia [31].
Compared to patients who were not having thoracic surgery, we found that patients who were having thoracic surgery were four times more likely to experience ICU anemia. Studies support the conclusions we have made. After undergoing pulmonary surgery, a retrospective examination of 465 patients in China revealed that 75.3% of patients in the intensive care unit had a postoperative anemia diagnosis [32]. This is also true in patients undergoing cardiac surgery in which the prevalence of anemia is high [33].
Patients who had undergone urologic surgery were 6.2 times more likely to develop anemia in the ICU than those who had not undergone urologic surgery. According to different studies, anemia is significantly associated with urologic surgery, and the magnitude is even higher in renal transplant surgeries [34, 35].
ICU anemia was frequently encountered in patients undergoing neurologic surgery, 4.5 times more frequently than in those who hadn’t undergone neurologic surgery. As evidenced by different published reports, anemia is a common scenario in patients undergoing neurologic surgery after ICU admission. This is supported by a study [36, 37].
The possible postulated mechanisms of anemia after surgery are described below. Anemia during surgery is a typical clinical scenario. Anemia that develops postoperatively resembles chronic illness anemia and is likely due to the impact that inflammatory mediators generated both before and after surgery have on the growth and survival of RBCs [38, 39].
Strengths and limitations of the study
Strengths
-
Most of the studies on anemia were pre-operative and cross-sectional studies, so this study identifies the incidence and factors associated with anemia postoperatively after patients have been admitted to the surgical ICU using cohort studies.
-
This study provides insights and clues about the incidence and associated factors of anemia in ICU-admitted elective surgical patients for future research; as such studies are limited in the area.
Limitations
In this study, we used secondary data, and as a result, some important information regarding factors associated with anemia (e.g., nutritional status and living conditions) was not found during the chart review.
Conclusion
Among surgical patients admitted to the ICU, the incidence of anemia is high. The majority of surgical intensive care unit admitted patients exhibit anemia during their course of stay. ASA physical status class III, renal failure, malignancy, thoracic surgery, urologic surgery, and neurologic surgery significantly increase the likelihood of anemia in surgical patients who are hospitalized in the intensive care unit (ICU). So, early screening and the institution of therapeutic measures are necessary to reduce the adverse effects of anemia. Preoperative screening of ASA physical status and medical conditions, early identifications and treatment of patients with comorbidities before surgery, and minimizing modifiable factors (i.e. duration of surgery and intraoperative blood loss) help to reduce the incidence of anemia in surgical patients admitted to ICU.
Data availability
If a legitimate request is made, the corresponding author will provide the data sets utilized and analyzed during the study.
Abbreviations
- ALI:
-
Acute lung injury
- ASA:
-
American Society of Anesthesiologists
- CBC:
-
Complete blood count
- DHS:
-
Demographic Health Survey
- Hb:
-
Hemoglobin
- HCT:
-
Hematocrit
- ICU:
-
Intensive care unit
- IRB:
-
Institutional review board
- PBM:
-
Patient blood management
- RBC:
-
Red blood cell
- SICU:
-
Surgical intensive care unit
- SPSS:
-
Statistical Package for Social Sciences
- SRS:
-
Systematic random sampling
- TASH:
-
Tikur Anbessa Specialized Hospital
- WHO:
-
World Health Organization
References
Buttarello M. Laboratory diagnosis of anemia: are the old and new red cell parameters useful in classification and treatment, how? Int J Lab Hematol. 2016;38:123–32.
Rawal G, Kumar R, Yadav S, Singh A. Anemia in intensive care: a review of current concepts. J Crit Care Med. 2016;2(3):109–14.
Prasanth R. Prevalence of anemia in both developing and developed countries around the world. World J Anemia. 2017;1(2):40–3.
Juárez-Vela R, Andrés-Esteban EM, Gea-Caballero V, Sánchez-González JL, Marcos-Neira P, Serrano-Lázaro A, et al. Related factors of anemia in critically ill patients: a prospective multicenter study. J Clin Med. 2022;11(4):1031.
Renard D, Rosselet A. Drug-induced hemolytic anemia: pharmacological aspects. Transfus Clin Biol. 2017;24(3):110–4.
Kim J, Curran BP, Du AL, Gabriel RA, Du A. The association of primary anesthesia type with postoperative transfusion in anemic patients undergoing primary total joint arthroplasty. Cureus. 2022. https://doi.org/10.7759/cureus.24496.
Kim J, Shin S, Han K, Lee K, Kim J, Choi Y, et al. Relationship between socioeconomic status and anemia prevalence in adolescent girls based on the fourth and fifth Korea national health and nutrition examination surveys. Eur J Clin Nutr. 2014;68(2):253–8.
Tesfaye TS, Tessema F, Jarso H. Prevalence of anemia and associated factors among “apparently healthy” urban and rural residents in Ethiopia: a comparative cross-sectional study. J Blood Med. 2020;11:89–96.
Song X, Liu X-Y, Wang H-R, Guo X-Y, Kashani KB, Ma P-L. Association between anemia and ICU outcomes. Chin Med J. 2021;134(14):1744–6.
Cherry-Bukowiec JR, Engoren M, Wiktor A, Raghavendran K, Napolitano LM. Hepcidin and anemia in surgical critical care: a prospective cohort study. Crit Care Med. 2018;46(6):e567–74.
Vincent J-L, Jaschinski U, Wittebole X, Lefrant J-Y, Jakob SM, Almekhlafi GA, et al. Worldwide audit of blood transfusion practice in critically ill patients. Crit Care. 2018;22:1–9.
Fritsch SJ, Dreher M, Simon T-P, Marx G, Bickenbach J. Haemoglobin value and red blood cell transfusions in prolonged weaning from mechanical ventilation: a retrospective observational study. BMJ Open Respir Res. 2022;9(1): e001228.
Jati SAW, Aditianingsih D, George Y, Risadayanti R. Effect of hemoglobin levels on the success of weaning and extubation processes in critical patients with mechanical ventilation: a systematic review, Bali. J Anesthesiol. 2023;7(4):197–201.
Prin M, Rui S, Pan S, Kadyaudzu C, Mehta PS, Li G, et al. Anemia at intensive care unit admission and hospital mortality among patients at a referral hospital in Malawi. Am Surg. 2021;87(8):1334–40.
Shander A, Lobel GP, Javidroozi M. Anesthesia for patients with anemia. Anesthesiol Clin. 2016;34(4):711–30.
Zeleke MB, Shaka MF, Anbesse AT, Tesfaye SH. Anemia and its determinants among male and female adolescents in Southern Ethiopia: a comparative cross-sectional study. Anemia. 2020;2020:3906129.
Hermans G, Van Aerde N, Meersseman P, Van Mechelen H, Debaveye Y, Wilmer A, et al. Five-year mortality and morbidity impact of prolonged versus brief ICU stay: a propensity score matched cohort study. Thorax. 2019;74(11):1037–45.
Bowyer A, Royse C. Postoperative recovery and outcomes—what are we measuring and for whom? Anaesthesia. 2016;71:72–7.
Muñoz M, Acheson A, Bisbe E, Butcher A, Gómez-Ramírez S, Khalafallah A, et al. An international consensus statement on the management of postoperative anaemia after major surgical procedures. Anaesthesia. 2018;73(11):1418–31.
Kalra SK, Thilagar B, Khambaty M, Manjarrez E. Post-operative anemia after major surgery: a brief review. Curr Emerg Hosp Med Rep. 2021;9(3):89–95.
Zuther M, Rübsam M-L, Zimmermann M, Zarbock A, Hönemann C. Improved diagnosis of iron deficiency anemia in the critically ill via fluorescence flowcytometric hemoglobin biomarkers. Cells. 2022;12(1):140.
Aydogan M, Ucar M, Yücel A, Karakas B, Gok A, Togal T. Effects of iron deficiency on transfusion requirements in critically ill patients: a preliminary observational study. Crit Care. 2015;19:1–201.
Anand S, Burkenroad A, Glaspy J. Workup of anemia in cancer. Clin Adv Hematol Oncol. 2020;18:640–6.
Warner MA, Hanson AC, Frank RD, Schulte PJ, Go RS, Storlie CB, et al. Prevalence of and recovery from anemia following hospitalization for critical illness among adults. JAMA Netw Open. 2020;3(9):e2017843.
James TE, Barty R, Liu Y, Rochwerg B, Heddle N, Siegal DM. Blood loss due to laboratory testing in critical care patients: a retrospective cohort study. Blood. 2018;132:4885.
Ghiani A, Sainis A, Sainis G, Neurohr C. Anemia and red blood cell transfusion practice in prolonged mechanically ventilated patients admitted to a specialized weaning center: an observational study. BMC Pulm Med. 2019;19(1):1–9.
Kron AT, Collins A, Cserti-Gazdewich C, Pendergrast J, Webert K, Lieberman L, et al. A prospective multi-faceted interventional study of blood bank technologist screening of red blood cell transfusion orders: the START study. Transfusion. 2021;61(2):410–22.
Li G, Walco JP, Mueller DA, Wanderer JP, Freundlich RE. Reliability of the ASA physical status classification system in predicting surgical morbidity: a retrospective analysis. J Med Syst. 2021;45:1–8.
Rosa F, Tortorelli A, Quero G, Galiandro F, Fiorillo C, Sollazzi L, et al. The impact of preoperative ASA-physical status on postoperative complications and long-term survival outcomes in gastric cancer patients. Eur Rev Med Pharmacol Sci. 2019;23(17):7383–90.
Habib A, Ahmad R, Rehman S. Hematological changes in chronic renal failure patients and the effect of hemodialysis on these parameters. Int J Res Med Sci. 2017;5(11):4998–5003.
Assi HI, Halim NA, Alameh I, Khoury J, Nahra V, Sukhon F, et al. Outcomes of patients with malignancy admitted to the intensive care units: a prospective study. Crit Care Res Pract. 2021;2021:1.
Lang Z, Wu Y, Bao M. Coagulation status and surgical approach as predictors of postoperative anemia in patients undergoing thoracic surgery: a retrospective study. Front Surg. 2021;8: 744810.
Dhir A, Tempe DK. Anemia and patient blood management in cardiac surgery—literature review and current evidence. J Cardiothorac Vasc Anesth. 2018;32(6):2726–42.
Jun KW, Cho J, Kim MH, Hwang JK, Park SC, Moon IS, et al. Changes in hemostatic factors after kidney transplantation: a retrospective cohort study. Medicine. 2021;100(36): e27179.
Bamgbola OF. Spectrum of anemia after kidney transplantation: pathophysiology and therapeutic implications. Clin Transplant. 2016;30(10):1185–94.
Vanhala H, Junttila E, Kataja A, Huhtala H, Luostarinen T, Luoto T. Incidence and associated factors of anemia in patients with acute moderate and severe traumatic brain injury. Neurocrit Care. 2022;37(3):629–37.
Kisilevsky A, Gelb A, Bustillo M, Flexman A. Anaemia and red blood cell transfusion in intracranial neurosurgery: a comprehensive review. Br J Anesthesia. 2018;120(5):988–98.
Shander A, Kaufman M, Goodnough LT. How i treat anemia in the perisurgical setting. Blood. 2020;136(7):814–22.
Tanner L, Neef V, Raimann FJ, Störmann P, Marzi I, Lefering R, et al. Influence of anemia in severely injured patients on mortality, transfusion and length of stay: an analysis of the TraumaRegister DGU®. Eur J Trauma Emerg Surg. 2022;48(4):2741–9.
Acknowledgements
We express our gratitude to Addis Ababa University (AAU) for providing us with the necessary ethical clearance and approval to carry out this study. We would also like to thank all of the data collectors for their incredibly hard work during the data collection procedures.
Funding
The governmental, private, or nonprofit sectors did not provide any grants or other financial assistance for this work.
Author information
Authors and Affiliations
Contributions
H.B. contributed to the idea and planning of the research, data collection, analysis, and interpretation. Scientific advice on the study design, data analysis, and paper writing provided by W.A. and L.H. N.Z. contributed to the manuscript’s development and revision of the research. Data collection, critical manuscript revision for significant intellectual content, and manuscript approval for publication were all completed by B.Y. and A.F. The authors all agreed to take responsibility for all parts of the work and read and approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study received approval from Addis Ababa University's ethical institutional review board. The study was carried out following the 1994 Helsinki Declaration and its subsequent revisions.
Consent for publication
Not applicable.
Conmpeting interests
There are no conflicting interests that the authors declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wubet, H.B., Mengistu, L.H., Gobezie, N.Z. et al. The incidence and factors associated with anemia in elective surgical patients admitted to a surgical intensive care unit: a retrospective cohort study. Eur J Med Res 29, 290 (2024). https://doi.org/10.1186/s40001-024-01887-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01887-4