Abstract
Purpose
Sepsis is a global public health burden. The sequential organ failure assessment (SOFA) is the most commonly used scoring system for diagnosing sepsis and assessing severity. Due to the widespread use of endotracheal intubation and sedative medications in sepsis, the accuracy of the Glasgow Coma Score (GCS) is the lowest in SOFA. We designed this multicenter, cross-sectional study to investigate the predictive efficiency of SOFA with or without GCS on ICU mortality in patients with sepsis.
Methods
First, 3048 patients with sepsis admitted to Peking Union Medical College Hospital (PUMCH) were enrolled in this survey. The data were collected from June 8, 2013 to October 12, 2022. Second, 18,108 patients with sepsis in the eICU database were enrolled. Third, 2397 septic patients with respiratory system ≥ 3 points in SOFA in the eICU database were included. We investigated the predictive efficiency of SOFA with or without GCS on ICU mortality in patients with sepsis in various ICUs of PUMCH, and then we validated the results in the eICU database.
Main results
In data of ICUs in PUMCH, the predictive efficiency of SOFA without GCS (AUROC [95% CI], 24 h, 0.724 [0.688, 0.760], 48 h, 0.734 [0.699, 0.769], 72 h, 0.748 [0.713, 0.783], 168 h, 0.781 [0.747, 0.815]) was higher than that of SOFA with GCS (AUROC [95% CI], 24 h, 0.708 [0.672, 0.744], 48 h, 0.721 [0.685, 0.757], 72 h, 0.735 [0.700, 0.757], 168 h, 0.770 [0.736, 0.804]) on ICU mortality in patients with sepsis, and the difference was statistically significant (P value, 24 h, 0.001, 48 h, 0.003, 72 h, 0.004, 168 h, 0.005). In septic patients with respiratory system ≥ 3 points in SOFA in the eICU database, although the difference was not statistically significant (P value, 24 h, 0.148, 48 h, 0.178, 72 h, 0.132, 168 h, 0.790), SOFA without GCS (AUROC [95% CI], 24 h, 0.601 [0.576, 0.626], 48 h, 0.625 [0.601, 0.649], 72 h, 0.639 [0.615, 0.663], 168 h, 0.653 [0.629, 0.677]) had a higher predictive efficiency on ICU mortality than SOFA with GCS (AUROC [95% CI], 24 h, 0.591 [0.566, 0.616], 48 h, 0.616 [0.592, 0.640], 72 h, 0.628 [0.604, 0.652], 168 h, 0.651 [0.627, 0.675]).
Conclusions
In severe sepsis, it is realistic and feasible to discontinue the routine GCS for SOFA in patients with a respiratory system ≥ 3 points, and even better predict ICU mortality.
Key messages
-
SOFA is the most commonly used scoring system for diagnosing sepsis and assessing severity. Due to the widespread use of endotracheal intubation and sedative medications in sepsis, the accuracy of GCS is the lowest in SOFA. We designed this multicenter, cross-sectional study to investigate the predictive efficiency of SOFA with or without GCS on ICU mortality in patients with sepsis.
-
In severe sepsis, it is realistic and feasible to discontinue the routine GCS for SOFA in patients with a respiratory system ≥ 3 points, and even better predict ICU mortality.
Similar content being viewed by others
Introduction
Sepsis is organ dysfunction due to severe infection and is one of the leading causes of death and critical illness worldwide [1, 2]. Without timely and effective intervention, mortality of sepsis can rapidly exceed 30–35% [3]. The sequential organ failure assessment (SOFA) is the most commonly used scoring system for diagnosing sepsis and assessing severity [4,5,6]. Due to the widespread use of endotracheal intubation and sedative medications in sepsis, the use of best guess methods or the continuation of pre-intubation recordings may overestimate the central nervous system function, thus affecting the prediction efficiency of SOFA [7]. In a study on the effects of levosimendan on acute organ dysfunction in sepsis, SOFA that does not include Glasgow Coma Score (GCS) was tried, and there was no significant decrease in evaluation efficiency [8]. With the above in mind, we designed this study to investigate the predictive efficiency of SOFA with or without GCS on ICU mortality in patients with sepsis in various ICUs of Peking Union Medical College Hospital (PUMCH), and then we validated the results in the eICU database.
Methods
Study design
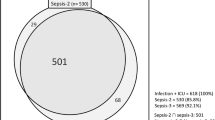
This was an observational, retrospective study. In this survey, 3048 patients with sepsis admitted to PUMCH were enrolled. The data were collected from June 8, 2013 to October 12, 2022. The basic information of patients with sepsis in PUMCH were shown in Table 1. The eICU Database is a freely available multi-center database for critical care research. In the eICU database, 18,108 patients with sepsis were selected as validation set. The basic information of patients with sepsis in the eICU database were shown in Additional file 3: Table S1. Sepsis was diagnosed on the basis of the third international consensus definitions for sepsis and septic shock. Patient inclusion and exclusion criteria were provided in the Additional file 2: Fig. S1.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The datasets supporting the conclusions of this article are included within the article (see Additional file 1).
Variables and measurements
Patients included in this study had completed SOFA during their ICU period. SOFA and GCS were completed by ICU nurses who were trained and qualified in critical care medicine. In this study, the best guess method based on clinical experience was used for GCS in patients receiving sedation. SOFA and GCS were performed within 24 h, 48 h, 72 h, and 168 h respectively and the worst results during the observation period were collected.
We first investigated the predictive efficiency of SOFA with or without GCS on ICU mortality in patients with sepsis in various ICUs of PUMCH, and then we validated the results in the eICU database.
Ethical considerations
The current study was reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology Guidelines. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The trial protocol was approved by the Central Institutional Review Board at Peking Union Medical College Hospital (NO. SK1828), and individual consent for this analysis was waived. There was no identifying or protected health information included in the analyzed dataset.
Data analysis
All statistical analyses were performed in SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Continuous variables were expressed as media (P25, P75). The area under the receiver operating characteristic curves (AUROCs) were used to evaluate the performance of variables at different time scales to predict ICU mortality. DeLong’s test was used to compare the differences in AUROCs. All p values were 2-tailed, and a p-value < 0.05 was considered statistically significant.
Results
In data of ICUs in PUMCH, the predictive efficiency of SOFA without GCS (AUROC [95% CI], 24 h, 0.724 [0.688, 0.760], 48 h, 0.734 [0.699, 0.769], 72 h, 0.748 [0.713, 0.783], 168 h, 0.781 [0.747, 0.815]) was higher than that of SOFA with GCS (AUROC [95% CI], 24 h, 0.708 [0.672, 0.744], 48 h, 0.721 [0.685, 0.757], 72 h, 0.735 [0.700, 0.757], 168 h, 0.770 [0.736, 0.804]) on ICU mortality in patients with sepsis, and the difference was statistically significant (P value, 24 h, 0.001, 48 h, 0.003, 72 h, 0.004, 168 h, 0.005) (Fig. 1).
We tried to validate this result in the eICU database. A total of 18,108 patients with sepsis were included. However, no identical results were observed. In eICU database, the predictive efficiency of SOFA without GCS (AUROC [95% CI], 24 h, 0.669 [0.657, 0.681], 48 h, 0.678 [0.666, 0.690], 72 h, 0.684 [0.673, 0.695], 168 h, 0.694 [0.683, 0.705]) was lower than that of SOFA with GCS (AUROC [95% CI], 24 h, 0.692 [0.681, 0.703], 48 h, 0.705 [0.694, 0.716], 72 h, 0.714 [0.703, 0.725], 168 h, 0.726 [0.715, 0.737]) on ICU mortality in patients with sepsis (P value, 24 h, < 0.001, 48 h, < 0.001, 72 h, < 0.001, 168 h, < 0.001) (Fig. 2).
By comparison, we found that the distribution of the included populations was significantly different. SOFA scores, GCS scores, and SOFA scores without GCS in PUMCH were higher than those in the eICU population (Fig. 3). We also found 1769 of the 3048 patients with sepsis were intubated in PUMCH database while 833 of the 18,108 patients with sepsis were intubated in the eICU database.
Considering that a considerable number of sepsis patients admitted to various ICUs of PUMCH were intubated and transferred after the patients developed consciousness disorders, we narrowed the range of eICU data to the range of respiratory system ≥ 3 points in SOFA for more accurate comparison. A total of 2397 septic patients with respiratory system ≥ 3 points in SOFA in the eICU database were included. All patients in this subgroup were intubated. We observed that in this subgroup of patients with sepsis in the eICU database, although the difference was not statistically significant (P value, 24 h, 0.148, 48 h, 0.178, 72 h, 0.132, 168 h, 0.790), SOFA without GCS (AUROC [95% CI], 24 h, 0.601 [0.576, 0.626], 48 h, 0.625 [0.601, 0.649], 72 h, 0.639 [0.615, 0.663], 168 h, 0.653 [0.629, 0.677]) had a higher predictive efficiency on ICU mortality than SOFA with GCS (AUROC [95% CI], 24 h, 0.591 [0.566, 0.616], 48 h, 0.616 [0.592, 0.640], 72 h, 0.628 [0.604, 0.652], 168 h, 0.651 [0.627, 0.675]) (Fig. 4).
Discussion
As the most widely used SOFA in the sepsis diagnosis and treatment related scoring system, efforts to further improve and optimize it have never stopped [9,10,11]. At present, there are many controversies about the application of SOFA in clinical practice, especially the accuracy of the GCS is the lowest in SOFA [12]. In the initial validation, the best guess method based on clinical experience was used in patients receiving sedation [13]. Other studies continued the last GCS recorded prior to endotracheal intubation until a neurological examination could be performed in patients without sedation. If no value is recorded before intubation, a score of 15 is assumed [14]. However, the timing of intubation is critically dependent on the judgment of the clinician, and a considerable proportion of intubation is due to the patient's impaired consciousness [15]. The central nervous system is an important organ involved in sepsis, and the incidence of sepsis associated encephalopathy is as high as 70%, and its function is constantly and dynamically changing during the course of sepsis [16, 17], a simple approach of best guess or continuing pre-intubation recording may not be appropriate. Central nervous system function is heavily dependent on the normal function of other organs, and there are varying degrees of impaired consciousness in shock, hypoxia [18], liver failure [19], and renal failure [20], so placing central nervous system on the same level as other organs may bias the scoring results in assessment of the severity of sepsis.
With the rise of big data analysis and artificial intelligence technology, the method of machine learning has been widely studied and applied in sepsis patients with massive monitoring data [21,22,23]. The above situation puts forward higher requirements for the wide application of automatic data collection systems in clinical practice, and the lack of GCS scores as subjective scores often affects the automatic generation of SOFA scores [24], so the search for a more objective SOFA scoring system has become an urgent problem to be solved in clinical practice.
From our study, the use of SOFA without GCS did not affect its predictive efficiency for ICU mortality of sepsis. Even the data from PUMCH showed that SOFA without GCS was significantly better in predictive efficiency, and the difference was statistically significant. In the eICU database, we also observed the same phenomenon in sepsis patients with respiratory system ≥ 3 points in SOFA. Therefore, it is reasonable to believe that it is realistic and feasible to discontinue the routine GCS for SOFA in patients with a respiratory system ≥ 3 points.
There are several limitations to this study. First, similar to digestive system, impaired central nervous function is an important aspect of multi-organ dysfunction, but there are still lack of biomarkers that can represent the function of this system. Simply eliminating the assessment of central nervous function is not the best choice for organ function assessment, and seeking objective indicators to represent its function is a problem that needs to be solved in future research. Second, this was an observational, retrospective study and therefore, prone to selection bias. Third, there are multiple outcome indicators in sepsis, such as mortality, survival time, duration of mechanical ventilation, and length of ICU stay. This study only analyzed ICU mortality [25], which may bias the results. Third, in studies of mortality, 28-day mortality [26, 27] or 30-day mortality [28] may be more objective options, and only ICU mortality [27] was analyzed in this study due to constraints.
Conclusion
In severe sepsis, it is realistic and feasible to discontinue the routine GCS for SOFA in patients with a respiratory system ≥ 3 points, and even better predict ICU mortality.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and Additional files.
Abbreviations
- SOFA:
-
Sequential organ failure assessment
- GCS:
-
Glasgow Coma Score
- PUMCH:
-
Peking Union Medical College Hospital
References
Bracht H, Hafner S, Weiss M. Sepsis update: definition and epidemiology. Anasthesiol Intensivmed Notfallmed Schmerzther. 2019;54(1):10–20. https://doi.org/10.1055/a-0625-5492.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10. https://doi.org/10.1001/jama.2016.0287.
Vincent JL, Jones G, David S, Olariu E, Cadwell KK. Frequency and mortality of septic shock in Europe and North America: a systematic review and meta-analysis. Crit Care. 2019;23(1):196. https://doi.org/10.1186/s13054-019-2478-6.
Schertz AR, Lenoir KM, Bertoni AG, Levine BJ, Mongraw-Chaffin M, Thomas KW. Sepsis prediction model for determining sepsis vs SIRS, qSOFA, and SOFA. JAMA Netw Open. 2023;6(8): e2329729. https://doi.org/10.1001/jamanetworkopen.2023.29729.
Wang X, Guo Z, Chai Y, Wang Z, Liao H, Wang Z, Wang Z. Application prospect of the SOFA score and related modification research progress in sepsis. J Clin Med. 2023. https://doi.org/10.3390/jcm12103493.
Ohbe H, Sasabuchi Y, Doi K, Matsui H, Yasunaga H. Association between levels of intensive care and in-hospital mortality in patients hospitalized for sepsis stratified by sequential organ failure assessment scores. Crit Care Med. 2023;51(9):1138–47. https://doi.org/10.1097/CCM.0000000000005886.
Lind ML, Rosas MM, McFarland L, Taylor L, Olson S, Pergam SA. Limits of the Glasgow Coma Scale when assessing for sepsis in allogeneic hematopoietic cell transplant recipients. Nurs Res. 2021;70(5):399–404. https://doi.org/10.1097/NNR.0000000000000521.
Gordon AC, Perkins GD, Singer M, McAuley DF, Orme RM, Santhakumaran S, Mason AJ, Cross M, Al-Beidh F, Best-Lane J, et al. Levosimendan for the prevention of acute organ dysfunction in sepsis. N Engl J Med. 2016;375(17):1638–48. https://doi.org/10.1056/NEJMoa1609409.
Lee HJ, Ko BS, Ryoo SM, Han E, Suh GJ, Choi SH, Chung SP, Lim TH, Kim WY, Kwon WY, et al. Modified cardiovascular SOFA score in sepsis: development and internal and external validation. BMC Med. 2022;20(1):263. https://doi.org/10.1186/s12916-022-02461-7.
Khwannimit B, Bhurayanontachai R, Vattanavanit V. Ability of a modified Sequential Organ Failure Assessment score to predict mortality among sepsis patients in a resource-limited setting. Acute Crit Care. 2022;37(3):363–71. https://doi.org/10.4266/acc.2021.01627.
Rhee C, Zhang Z, Kadri SS, Murphy DJ, Martin GS, Overton E, Seymour CW, Angus DC, Dantes R, Epstein L, et al. Sepsis surveillance using adult sepsis events simplified eSOFA criteria versus sepsis-3 sequential organ failure assessment criteria. Crit Care Med. 2019;47(3):307–14. https://doi.org/10.1097/CCM.0000000000003521.
Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23(1):374. https://doi.org/10.1186/s13054-019-2663-7.
Tallgren M, Backlund M, Hynninen M. Accuracy of Sequential Organ Failure Assessment (SOFA) scoring in clinical practice. Acta Anaesthesiol Scand. 2009;53(1):39–45. https://doi.org/10.1111/j.1399-6576.2008.01825.x.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–36. https://doi.org/10.1378/chest.100.6.1619.
Piva S, Bertoni M, Gitti N, Rasulo FA, Latronico N. Neurological complications of sepsis. Curr Opin Crit Care. 2023;29(2):75–84. https://doi.org/10.1097/MCC.0000000000001022.
Pan S, Lv Z, Wang R, Shu H, Yuan S, Yu Y, Shang Y. Sepsis-induced brain dysfunction: pathogenesis, diagnosis, and treatment. Oxid Med Cell Longev. 2022;2022:1328729. https://doi.org/10.1155/2022/1328729.
Ren C, Yao RQ, Zhang H, Feng YW, Yao YM. Sepsis-associated encephalopathy: a vicious cycle of immunosuppression. J Neuroinflammation. 2020;17(1):14. https://doi.org/10.1186/s12974-020-1701-3.
Coppler PJ, Elmer J. Novel pupillary assessment in post anoxic coma. Resuscitation. 2022;176:66–7. https://doi.org/10.1016/j.resuscitation.2022.05.016.
Gibbs JT, Louissaint J, Tapper EB. Rate of successful extubation in mechanically ventilated patients with cirrhosis and hepatic coma. Dig Dis Sci. 2022;67(11):5336–44. https://doi.org/10.1007/s10620-022-07400-3.
Kafle DR, Sah RP, Karki DR. Non traumatic coma in the intensive care unit: etiology and prognosis. Kathmandu Univ Med J (KUMJ). 2021;19(75):371–4.
Yang R, Han D, Zhang L, Huang T, Xu F, Zheng S, Yin H, Lyu J. Analysis of the correlation between the longitudinal trajectory of SOFA scores and prognosis in patients with sepsis at 72 hour after admission based on group trajectory modeling. J Intensive Med. 2022;2(1):39–49. https://doi.org/10.1016/j.jointm.2021.11.001.
Pan X, Xie J, Zhang L, Wang X, Zhang S, Zhuang Y, Lin X, Shi S, Shi S, Lin W. Evaluate prognostic accuracy of SOFA component score for mortality among adults with sepsis by machine learning method. BMC Infect Dis. 2023;23(1):76. https://doi.org/10.1186/s12879-023-08045-x.
Fleuren LM, Klausch TLT, Zwager CL, Schoonmade LJ, Guo T, Roggeveen LF, Swart EL, Girbes ARJ, Thoral P, Ercole A, et al. Machine learning for the prediction of sepsis: a systematic review and meta-analysis of diagnostic test accuracy. Intensive Care Med. 2020;46(3):383–400. https://doi.org/10.1007/s00134-019-05872-y.
Schenck EJ, Hoffman KL, Cusick M, Kabariti J, Sholle ET, Campion TR Jr. Critical carE Database for Advanced Research (CEDAR): an automated method to support intensive care units with electronic health record data. J Biomed Inform. 2021;118: 103789. https://doi.org/10.1016/j.jbi.2021.103789.
Do SN, Dao CX, Nguyen TA, Nguyen MH, Pham DT, Nguyen NT, Huynh DQ, Hoang QTA, Bui CV, Vu TD, et al. Sequential Organ Failure Assessment (SOFA) Score for predicting mortality in patients with sepsis in Vietnamese intensive care units: a multicentre, cross-sectional study. BMJ Open. 2023;13(3): e064870. https://doi.org/10.1136/bmjopen-2022-064870.
Baldira J, Ruiz-Rodriguez JC, Ruiz-Sanmartin A, Chiscano L, Cortes A, Sistac DA, Ferrer-Costa R, Comas I, Villena Y, Larrosa MN, et al. Use of biomarkers to improve 28-day mortality stratification in patients with sepsis and SOFA ≤6. Biomedicines. 2023. https://doi.org/10.3390/biomedicines11082149.
Gaini S, Relster MM, Pedersen C, Johansen IS. Prediction of 28-days mortality with sequential organ failure assessment (SOFA), quick SOFA (qSOFA) and systemic inflammatory response syndrome (SIRS): a retrospective study of medical patients with acute infectious disease. Int J Infect Dis. 2019;78:1–7. https://doi.org/10.1016/j.ijid.2018.09.020.
Wang XW, Niu XG, Li JX, Zhang SS, Jiao XF. SOFA score can effectively predict the incidence of sepsis and 30-day mortality in liver transplant patients: a retrospective study. Adv Ther. 2019;36(3):645–51. https://doi.org/10.1007/s12325-019-0889-z.
Acknowledgements
The authors would like to thank all participants and staff. The China National Critical Care Quality Control Center Group consists of the following persons: Yongjun Liu, Yan Kang, Jing Yan, Erzhen Chen, Bin Xiong, Bingyu Qin, Kejian Qian, Wei Fang, Mingyan Zhao, Xiaochun Ma, Xiangyou Yu, Jiandong Lin, Yi Yang, Feng Shen, Shusheng Li, Lina Zhang, Weidong Wu, Meili Duan, Linjun Wan, Xiaojun Yang, Jian Liu, Zhen Wang, Lei Xu, Zhenjie Hu, Longxiang Su, Congshan Yang.
Funding
National Natural Science Fund of China (No. 81801901), the National Key R&D Program of China (No. 2020YFC0861000), the China Medical Board (No. CMB 20–381) and the National High Level Hospital Clinical Research Funding (2022-PUMCH-B-115).
Author information
Authors and Affiliations
Consortia
Contributions
Data curation: Lu Wang, Xudong Ma, Guanghua Zhou, Sifa Gao, Wei Pan, Jieqing Chen, Longxiang Su, Huaiwu He, Yun Long, Ting Shu and Xiang Zhou. Formal analysis: Xudong Ma, and Sifa Gao. Methodology: Xiang Zhou, Zhi Yin and Ting Shu. Project administration: Xiang Zhou, and Ting Shu. Resources: Lu Wang, Xudong Ma, and Guanghua Zhou. Supervision: Xiang Zhou, Xudong Ma, Guanghua Zhou, and Sifa Gao. Validation: Xiang Zhou, Zhi Yin and Ting Shu. Writing—original draft: Lu Wang, Xiang Zhou, Zhi Yin and Ting Shu.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The trial protocol was approved by the Central Institutional Review Board at Peking Union Medical College Hospital (NO. SK1828) and individual consent for this retrospective analysis was waived.
Consent for publication
All authors have agreed to publish it.
Competing interests
The authors declare that they have no competing interests. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies.
Additional file 2.
Patient inclusion and exclusion criteria.
Additional file 3: Table S1.
Basic information of patients with sepsis in eICU database.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, L., Ma, X., Zhou, G. et al. SOFA in sepsis: with or without GCS. Eur J Med Res 29, 296 (2024). https://doi.org/10.1186/s40001-024-01849-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01849-w