Abstract
Background
The purpose of this study was to investigate the correlation between novel anthropometric indices, specifically the body shape index (ABSI) and body roundness index (BRI), and the prevalence of kidney stone disease (KSD) within the general population of the United States (U.S.).
Methods
This study employed a cross-sectional analysis of participants in the National Health and Nutrition Examination Survey from 2007 to 2020. Various statistical methods, including multivariable logistic regression analysis, restricted cubic spline (RCS) plot curve, receiver operating characteristic (ROC) curves, and subgroup analysis, were utilized to examine the association between ABSI and BRI and the risk of KSD.
Results
A total of 39,251 individuals were included in the study. First, the RCS plot presented that a linear positive association was found between ABSI and BRI and KSD risk. Second, the results of the multivariable logistic regression analysis revealed that, compared to the lowest quartile, the adjusted odds ratios (with 95% confidence intervals) for the prevalence of KSD across the quartiles of ASBI and BRI were 0.94 (0.67, 1.30), 1.55 (1.15, 2.10), and 1.74 (1.28, 2.35), respectively, in the fully adjusted model. Third, the ROC curve demonstrated that the area under the curve of ABSI, and BRI was significantly higher than traditional anthropometry or body composition measures, including BMI and waist circumference.
Conclusions
The findings of our study indicate that the discriminant ability of ABSI and BRI for KSD is significantly superior to that of BMI and waist circumference. Consequently, ABSI and BRI have the potential to more accurately identify an individual’s risk of developing KSD in a clinical setting.
Similar content being viewed by others
Introduction
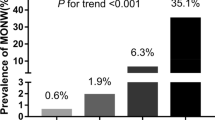
Kidney stone disease (KSD) is characterized by the abnormal accumulation of crystalline substances, such as uric acid, calcium oxalate, and calcium phosphate, within the renal calyces, renal pelvis, and the junction of the renal pelvis and the ureter [1]. Meanwhile, KSD is a prevalent condition in urology treatment, affecting approximately 1–20% of the global population. This disease often leads to kidney colic, urinary system infection, and kidney function impairment, posing significant risks to public health [2]. There are approximately 5% of women and 12% of men in the United States who will develop KSD during the course of their lifetimes, and the prevalence of KSD has been rising in both sexes [3]. In addition, recent research indicates a rise in the 12-month cumulative incidence of KSD among Americans, increasing from 0.6% in 2005 to 0.9% in 2015 [4]. The financial burden associated with KSD is substantial, with an estimated expenditure of $2 billion in 2000, and projections suggest that by 2030, the cost of treating KSD will surpass $4.5 billion [5].
With the advancement of research into KSD, it has been found that it is closely related to sex, age, race, body mass index (BMI), hypertension, diabetes, smoking, and the metabolic syndrome [6]. The shift in dietary patterns resulting from improved living standards has led to a rise in the prevalence of overweight and obesity among individuals [7]. Investigations have demonstrated a positive correlation between BMI and the incidence of KSD, indicating that being overweight or obese heightens the susceptibility to this disease [8]. Previous studies have predominantly employed BMI as a primary measure for evaluating obesity. The problem is, however, that it does not accurately reflect actual obesity levels and the distribution of body fat on an individual basis. However, BMI does not adequately reflect the distribution of abdominal fat [9]. Hence, a range of innovative anthropometric measurements, such as waist-to-height ratio (WHtR), waist-to-hip ratio (WHR), body roundness index (BRI), visceral adiposity index (VAI), and a body shape index (ABSI), have been proposed to enhance the assessment of both visceral adipose quantity and abdominal obesity severity [10]. Among them, ABSI serves as a numerical index designed to evaluate body shape and fat distribution in individuals, incorporating waist circumference, height, and weight to derive the index value [11]. ABSI was developed with the intention of offering supplementary insights beyond BMI by specifically examining the distribution of adipose tissue. Research findings have indicated that individuals with elevated waist circumference and central obesity, characterized by excessive fat accumulation around the abdomen, may face an augmented susceptibility to various health ailments, including cardiovascular disease and type 2 diabetes [12,13,14]. Meanwhile, Thomas et al. put forth the body roundness index (BRI) as a prospective metric for assessing visceral adiposity tissue and overall body fat percentage [15]. Furthermore, the effectiveness of the body roundness index (BRI) as a dependable indicator of metabolic syndrome has been demonstrated in diverse populations and ethnic groups [16]. Wang J et al. discovered a positive correlation between the prevalence of kidney stone disease (KSD) and the visceral adiposity index (VAI), suggesting that a lower VAI is associated with a reduced risk of future kidney stone formation [17]. Moreover, Lee MR and colleagues also unveiled that waist-to-height ratio (WHtR), waist-to-hip ratio (WHR), and VAI were all linked to a higher prevalence of KSD and an increased likelihood of developing incident KSD. Consequently, these variables possess potential as prognostic indicators within the clinical domain for the emergence of KSD [18]. However, there is a lack of research on the correlation between ABSI, and BRI and prevalence of KSD in United States (U.S.) adults. Consequently, we undertook this cross-sectional study to evaluate the connection between ABSI, and BRI, and the susceptibility to KSD in the U.S., utilizing data derived from the National Health and Nutrition Examination Survey (NHANES) database. This endeavor aims to facilitate healthcare practitioners in their assessment of KSD risk. In addition, we also identified and compared the discriminating power of novel anthropometric measures as a KSD risk screening tool, calculating the best cutoff values for these measures to help healthcare professionals assess KSD risk.
Materials and methods
Study population
Based on a stratified multistage random sampling design, the NHANES is a nationally representative cross-sectional survey, which to reflect the civilian noninstitutionalized resident population information, conducted in the American. Data for this study were obtained from the NHANES surveys conducted between 2007 and 2020 year. In total, 72,367 patients were admitted, of whom 44,002 had KSD data available. Then, we excluded 4751 participants with missing the novel anthropometric indices, including a body shape index (ABSI), and body roundness index (BRI) data. Ultimately, we included 39,251 participants in our study (Fig. 1). Participants in the NHANES study signed informed consent forms and the protocols were approved by the National Center For Health Statistics Research Ethics Review Board [19]. The NHANES website (https://www.cdc.gov/nchs/nhanes/) provides information about the survey design, methods, population, and data.
Anthropometric measurements
Using standardized techniques and equipment, experienced examiners measured basic anthropometric measurements at the mobile examination center, including body height (BH), weight (BW), and waist circumference (WC). Among them, WC was measured at the superior border of the iliac crests. The ABSI and BRI were calculated according to the previous published formulae [20] as follows:
KSD measurement
A questionnaire called KIQ026 was completed by all participants at baseline. The question in the questionnaire was “Have you ever had a kidney stone?”. A history of kidney stones was considered to be present in participants who replied "Yes". Those participants who said “no” to the question of whether they had had a kidney stone were assumed to have not had one. NHANES CAPI system with built-in consistency checks ensured the quality and effectiveness of this question. More details are documented in the NHANES Laboratory/Medical Technician Procedures Manual.
Covariates
The following covariates were included in the study: race/ethnicity (Other Hispanic, Non-Hispanic White, Mexican American, Non-Hispanic Black, and Other Race—Including Multi-Racial), age, sex, family poverty income ratio (PIR), marital status (having a partner, no partner, and unmarried), education level (less than high school, high school, and more than high school), smoke status (no, former, and now), drinking status (no, former, mild, moderate, and heavy), the complication of hypertension, and diabetes mellitus (DM), BMI, WC, ABSI, BRI, mean energy intake, total water intake, urine albumin, total cholesterol (TC), urine creatinine, fast glucose (FBG), uric acid (UA), triglyceride (TG), serum creatinine (Scr), urea albumin creatinine ratio (uACR), blood urea nitrogen (BUN), high-density lipoprotein-cholesterol (HDL-C), and estimated glomerular filtration rate (eGFR). For more information about the variables in this study, please refer to www.cdc.gov/nchs/nhanes/.
Statistical analysis
In this study, all statistical analyses were conducted using R version 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria) and SPSS version 23.0 (SPSS Inc., Chicago, IL, USA). To qualify as statistically significant, P value < 0.05 had to be met. All estimates were calculated by accounting for NHANES sample weights. The characteristics of the participants were subclassified based on ABSI quartiles (Q1: 0.0576–0.078; Q2: 0.079–0.082; Q3: 0.083–0.085; and Q4: 0.086–0.112), BRI quartiles (Q1: 1.049–3.903; Q2: 3.904–5.205; Q3: 5.206–6.820; and Q4: 6.821–23.483), BMI quartiles (Q1: 15.02–24.50; Q2: 24.51–28.20; Q3: 28.21–32.90; and Q4: 32.91–82.00), and WC quartiles (Q1: 61.10–88.30; Q2: 88.31–98.50; Q3: 98.51–109.75; and Q4: 109.76–178.00). Variables that are continuous are expressed in terms of means (standard deviations, SDs) and variables that are categorical are expressed in terms of numbers (%). We used weighted Student’s t test or one-way ANOVA methods (continuous variables) and weighted Chi-square tests method (categorical variables) to calculate differences between groups. An analysis of multivariate logistic regression was used to investigate the association of ABSI, BRI, BMI, and WC with KSD risk. First, model 1 was adjusted for sex and age. Second, model 2 was adjusted for model 1 variables plus education level, race/ethnicity, marital status, smoke status, family PIR, drink status, the complication of DM, and hypertension. Finally, model 3 was adjusted for model 2 variables plus total water intake, FBG, TC, urine creatinine, UA, HDL-C, mean energy intake, BUN, urine albumin, Scr, uACR, TG, and eGFR, as our final model.
Results
Baseline characteristics
We computed that the number of participants in this research may be representative of the total population of 216,538,371 in the United States. Table 1 shows the baseline characteristics of the research participants in detail and the incidence of KSD in this group was 10.1%. There is a significant difference in age, marital status, sex, the complication of hypertension, smoker, race/ethnicity, work activity, BMI, the complication of DM, urine albumin, waist circumference, alcohol user, FBG, eGFR, TG, BUN, Scr, HDL, UA, urine creatinine, uACR, ABSI, and BRI among non-KSD group, and KSD group.
Association between ABSI, and BRI and KSD
The RCS plot illustrated that ABSI, BRI, BMI, and waist circumference were positively correlated with risk of KSD (P for nonlinearity > 0.05, Figs. 2A, B, 3A, B). In addition, Table 2 shows the findings of multivariate logistic regression analysis for the relationship between ABSI, and BRI and prevalence of KSD. After adjusting for confounding factors, compared with the lowest quartiles (Q1) of ABSI, and BRI, the odds ratios (ORs) with 95% confidence intervals (CIs) for KSD across the quartiles were 0.968 (0.575, 1.630), 1.092 (0.584, 2.044), and 1.453 (0.625, 3.376), as well as 1.196 (0.717, 1.994), 1.148 (0.603, 2.187), and 1.761 (0.690, 4.492), respectively. In addition, we also presented the findings of multivariate logistic regression analysis for the association of BMI, WC with prevalence of KSD (Table 3).
Discrimination ability of different anthropometric measures
We performed ROC curve to evaluate the abilities of two novel anthropometric measures in discriminating individuals with KSD. The ROC curve analysis showed that the discriminant ability of ABSI, and BRI for KSD was significantly higher than BMI, and waist circumference (Fig. 4). The area under curves of ABSI, BRI, BMI, and WC were 0.594, 0.589, 0.558, and 0.582, respectively.
Subgroup analyses
Subgroup analysis, stratified by age, sex, hypertension, and DM were undertaken to explore the association between ABSI, BRI, BMI, and WC with KSD risk. The stratified analysis revealed that ABSI with risk of KSD was observed in participants who older than 60 years, without or with hypertension, male or female, and with DM (Additional file 1: Fig. S1, and Additional file 5: Table S1). The positive liner association of BRI with KSD was found among participants in all ages and was male or female, without or with hypertension, and without or with DM (Additional file 2: Fig. S2, and Additional file 6: Table S2). In addition, we further performed subgroup analysis to examine the correlation between BMI, and WC with KSD risk (Additional file 7: Table S3, and Additional file 7: Table S4; Additional file 3: Fig. S3, and Additional file 4: Fig. S4). Associations of BMI and waist circumference and prevalence of KSD were consistent with BRI in different subgroups.
Discussion
There exist two prevalent metrics for assessing body shape, namely, BMI and WC. Nevertheless, BMI encounters a limitation in its inability to discern between fat mass and fat-free mass, whereas WC exhibits a bias against individuals of varying sizes, thereby diminishing its reliability [21,22,23]. Consequently, ABSI and BRI have emerged as novel anthropometric approaches to gauge both the extent of abdominal obesity and the quantity of visceral adipose tissue in conjunction with BMI and waist circumference. This study represents the initial investigation into the correlation between the recently developed anthropometric indices, ABSI and BRI, and the prevalence of KSD within the broader U.S. population. Our findings indicate a positive association between ABSI and BRI and the prevalence of KSD. Specifically, individuals with higher ABSI and BRI values exhibited a greater likelihood of experiencing KSD compared to those with lower ABSI and BRI values. Furthermore, when comparing these novel anthropometric indicators with traditional measures such as BMI and waist circumference, we observed a significantly higher predictive capacity of ABSI and BRI in discerning the likelihood of developing KSD. Based on our research findings, it is suggested that ABSI and BRI could play a crucial role in the management of risk associated with KSD. Currently, there is a dearth of studies investigating the correlation between ABSI and the prevalence of KSD. Nevertheless, prior research has established a strong link between obesity and the likelihood of developing KSD [24]. For instance, Ye Z et al. demonstrated that overweight or obesity, in conjunction with an unhealthy metabolic status, significantly heightens the risk of KSD within the general population of the U.S. [25]. Furthermore, Yuan S. et al. employed a Mendelian randomization analysis to propose a causal relationship between a high BMI and an augmented risk of KSD [26]. Similarly, Rahman IA et al. demonstrated an association between hypertension, DM, obesity, dyslipidemia, and an elevated likelihood of developing KSD [27]. In addition, when compared to the control group, patients with nephrolithiasis had significantly higher visceral adiposity indexes (VAI) [28]. Consequently, our hypothesis posits that the rise in ABSI and BRI among participants correlates with an increased prevalence of these conditions, ultimately resulting in a higher incidence of KSD. Lee MR and colleagues discovered that BRI exhibited a significant correlation with an increased prevalence of KSD and the emergence of incident KSD within the Chinese Taiwan population, thus potentially serving as predictive indicators for KSD development in clinical settings [18]. Nevertheless, investigations exploring the association between BRI and KSD in other populations remain lacking. Huang H. et al. also discovered that perirenal fat thickness is a noteworthy predictive factor for the development and recurrence of KSD in a Chinese population, suggesting its potential utility in risk stratification during follow-up periods [29]. Consequently, reducing the prevalence of obesity, particularly abdominal obesity, may have a crucial role in preventing KSD. Furthermore, ABSI and BRI exhibit superior discriminant capabilities in predicting KSD compared to BMI and waist circumference. Therefore, we speculated that abdominal obesity is more closely associated with the occurrence of KSD.
Utilizing a substantial sample population from the NHANES database spanning from 2007 to 2020, the present study's outcomes contribute supplementary evidence supporting the utilization of ABSI and BRI as tools for identifying populations susceptible to KSD in primary prevention. Nevertheless, it is imperative to acknowledge the limitations inherent in our study. First, due to its cross-sectional design and the characteristics of the included population, this investigation is unable to establish a temporal causal relationship between ABSI, BRI, and the prevalence of KSD. Second, our study employed rigorous control measures for influential confounders, including kidney function and total water intake, during the implementation of our multivariable logistic regression analysis and RCS model to assess the prevalence of KSD. Nonetheless, it is important to acknowledge the potential existence of other unadjusted confounding factors. Third, due to constraints imposed by the NHANES database, we were unable to access radiological examinations of the patients (kidney–ureter–bladder radiography, ultrasound, computed tomography), stone analysis reports, and hospitalization reports from 2007–2020 years. Fourth, in the subgroup analysis, there were differences in the number of KSD and non-KSD groups that may affect this relationship between ABSI, as well as BRI and KSD. Finally, whether the conclusion in the present study based on U.S. participants could be applicable to other populations need to be further explored in the future work.
Conclusion
In summary, the study found a positive correlation between the ABSI, BRI, BMI, and waist circumference and the risk of KSD. Furthermore, the discriminant ability of ABSI and BRI in predicting KSD was significantly superior to that of BMI and waist circumference. More attention should be paid to anthropometric indices, especially novel anthropometric indices, to better prevent and treat of KSD.
Availability of data and materials
Survey data are available for data consumers and researchers all across the globe on the internet (https://www.cdc.gov/nchs/nhanes/).
References
Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y. Epidemiology of stone disease across the world. World J Urol. 2017;35(9):1301–20.
Abufaraj M, Xu T, Cao C, Waldhoer T, Seitz C, D’Andrea D, et al. Prevalence and trends in kidney stone among adults in the USA: analyses of National health and nutrition examination survey 2007–2018 data. Eur Urol Focus. 2021;7(6):1468–75.
Coe FL, Evan A, Worcester E. Kidney stone disease. J Clin Invest. 2005;115(10):2598–608.
Hill AJ, Basourakos SP, Lewicki P, Wu X, Arenas-Gallo C, Chuang D, et al. Incidence of kidney stones in the United States: the continuous national health and nutrition examination survey. J Urol. 2022;207(4):851–6.
Becerra AZ, Khusid JA, Sturgis MR, Fink LE, Gupta M, Konety BR, et al. Contemporary assessment of the economic burden of upper urinary tract stone disease in the United States: analysis of one-year health care costs, 2011–2018. J Endourol. 2022;36(4):429–38.
Song W, Hu H, Ni J, Zhang H, Zhang H, Yang G, et al. The relationship between ethylene oxide levels in hemoglobin and the prevalence of kidney stones in US adults: an exposure-response analysis from NHANES 2013–2016. Environ Sci Pollut Res Int. 2023;30(10):26357–66.
Siener R. Nutrition and kidney stone disease. Nutrients. 2021;13(6):1917.
Chou YH, Su CM, Li CC, Liu CC, Liu ME, Wu WJ, et al. Difference in urinary stone components between obese and non-obese patients. Urol Res. 2011;39(4):283–7.
Piqueras P, Ballester A, Durá-Gil JV, Martinez-Hervas S, Redón J, Real JT. Anthropometric indicators as a tool for diagnosis of obesity and other health risk factors: a literature review. Front Psychol. 2021;12: 631179.
Wu LD, Kong CH, Shi Y, Zhang JX, Chen SL. Associations between novel anthropometric measures and the prevalence of hypertension among 45,853 adults: a cross-sectional study. Front Cardiovasc Med. 2022;9:1050654.
Krakauer NY, Krakauer JC. Association of body shape index (ABSI) with hand grip strength. Int J Environ Res Public Health. 2020;17(18):6797.
Qiao T, Luo T, Pei H, Yimingniyazi B, Aili D, Aimudula A, et al. Association between abdominal obesity indices and risk of cardiovascular events in Chinese populations with type 2 diabetes: a prospective cohort study. Cardiovasc Diabetol. 2022;21(1):225.
Xing Z, Peng Z, Wang X, Zhu Z, Pei J, Hu X, et al. Waist circumference is associated with major adverse cardiovascular events in male but not female patients with type-2 diabetes mellitus. Cardiovasc Diabetol. 2020;19(1):39.
Anari R, Amani R, Latifi SM, Veissi M, Shahbazian H. Association of obesity with hypertension and dyslipidemia in type 2 diabetes mellitus subjects. Diabetes Metab Syndr. 2017;11(1):37–41.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring). 2013;21(11):2264–71.
Rico-Martín S, Calderón-García JF, Sánchez-Rey P, Franco-Antonio C, Martínez Alvarez M, Sánchez Muñoz-Torrero JF. Effectiveness of body roundness index in predicting metabolic syndrome: a systematic review and meta-analysis. Obes Rev. 2020;21(7): e13023.
Wang J, Yang Z, Bai Y, Yin S, Cui J, Xiao Y, et al. Association between visceral adiposity index and kidney stones in American adults: a cross-sectional analysis of NHANES 2007–2018. Front Nutr. 2022;9: 994669.
Lee MR, Ke HL, Huang JC, Huang SP, Geng JH. Obesity-related indices and its association with kidney stone disease: a cross-sectional and longitudinal cohort study. Urolithiasis. 2022;50(1):55–63.
Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999–2010. Vital and health statistics Ser 1, Programs and collection procedures. 2013; (56):1–37.
Su WY, Chen IH, Gau YC, Wu PY, Huang JC, Tsai YC, et al. Metabolic syndrome and obesity-related indices are associated with rapid renal function decline in a large taiwanese population follow-up study. Biomedicines. 2022;10(7):1744.
Wang YF, Tang Z, Guo J, Tao LX, Liu L, Li HB, et al. BMI and BMI changes to all-cause mortality among the elderly in Beijing: a 20-year cohort study. Biomed Environ Sci. 2017;30(2):79–87.
Böhm A, Heitmann BL. The use of bioelectrical impedance analysis for body composition in epidemiological studies. Eur J Clin Nutr. 2013;67(Suppl 1):S79-85.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working group on visceral obesity. Nat Rev Endocrinol. 2020;16(3):177–89.
Carbone A, Al Salhi Y, Tasca A, Palleschi G, Fuschi A, De Nunzio C, et al. Obesity and kidney stone disease: a systematic review. Min Urol Nefrol. 2018;70(4):393–400.
Ye Z, Wu C, Xiong Y, Zhang F, Luo J, Xu L, et al. Obesity, metabolic dysfunction, and risk of kidney stone disease: a national cross-sectional study. Aging male. 2023;26(1):2195932.
Yuan S, Larsson SC. Assessing causal associations of obesity and diabetes with kidney stones using Mendelian randomization analysis. Mol Genet Metab. 2021;134(1–2):212–5.
Rahman IA, Nusaly IF, Syahrir S, Nusaly H, Mansyur MA. Association between metabolic syndrome components and the risk of developing nephrolithiasis: a systematic review and bayesian meta-analysis. F1000 Res. 2021;10:104.
Sönmez MG, Kılınç MT, Göksoy İ, Kozanhan B, Aydın A, Balasar M, et al. Visceral adiposity index in kidney stone patients who have undergone surgery. Central Eur J Urol. 2022;75(2):191–8.
Huang H, Chen S, Zhang W, Wang T, Bai P, Xing J, et al. High perirenal fat thickness predicts a greater risk of recurrence in Chinese patients with unilateral nephrolithiasis. Ren Fail. 2023;45(1):2158870.
Acknowledgements
Thanks to all the volunteers who took part in the NHANES.
Funding
The project was supported by the Research Fund of Anhui Medical University (2022xkj060), and Research Fund of Anhui Provincial Translational Medicine (2021zhyx-C73).
Author information
Authors and Affiliations
Contributions
XH, and NY contributed to the hypothesis development and to the drafting of the manuscript; XL, and ZZ were responsibility for the data analysis. FJ, and GL contributed to the data interpretation and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All NHANES participants provided written informed consent and the National Center for Health Statistics obtained institutional review board approval prior to data collection. Because NHANES data are de-identified and publicly available, the analysis presented here was exempt from IRB review.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
RCS curve of the association of ABSI with KSD stratified by A age, B sex; C hypertension, and D DM. RCS, restricted cubic spline; ABSI, a body shape index; KSD, kidney stone disease; DM, diabetes mellitus
Additional file 2: Figure S2.
RCS curve of the association of BRI with KSD stratified by A age, B sex; C hypertension, and D DM. RCS, restricted cubic spline; BRI, body roundness index; KSD, kidney stone disease; DM, diabetes mellitus.
Additional file 3: Figure S3.
RCS curve of the association of BMI with KSD stratified by A age, B sex; C hypertension, and D DM. RCS, restricted cubic spline; BMI, body mass index; KSD, kidney stone disease; DM, diabetes mellitus.
Additional file 4: Figure S4.
RCS curve of the association of waist circumference with KSD stratified by A age, B sex; C hypertension, and D DM. RCS, restricted cubic spline; KSD, kidney stone disease; DM, diabetes mellitus.
Additional file 5: Table S1.
Subgroups analysis for the associations of ABSI with prevalence of KSD.
Additional file 6: Table S2.
Subgroups analysis for the associations of BRI with prevalence of KSD.
Additional file 7: Table S3.
Subgroups analysis for the associations of BMI with prevalence of KSD.
Additional file 8: Table S4.
Subgroups analysis for the associations of waist circumference with prevalence of KSD.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, X., Li, X., Ye, N. et al. Association of novel anthropometric indices with prevalence of kidney stone disease: a population-based cross-sectional study. Eur J Med Res 29, 204 (2024). https://doi.org/10.1186/s40001-024-01743-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01743-5