Abstract
Background
The diagnostic process for fibrotic interstitial lung disease (F-ILD) is notably intricate, necessitating a multidisciplinary discussion to achieve consensus based on both clinical and radiological features. This study investigated the shared and distinctive long-term mortality predictors among the two primary phenotypes of F-ILD, namely idiopathic pulmonary fibrosis (IPF) and connective tissue disease-associated interstitial lung disease (CTD-ILD).
Methods
We included patients with F-ILD diagnosed from December 2018 to December 2019 and conducted follow-up assessments until February 2023. Age, gender, usual interstitial pneumonia (UIP) pattern, gender–age–physiology (GAP) score, modified Medical Research Council (mMRC) dyspnea score, antifibrotic agent use, pulmonary function test parameters, and six-minute walking test (6MWT) parameters were recorded at baseline and used as mortality predictors in a multivariate Cox regression model.
Results
We enrolled 104 ILD patients. The survival rate of non-IPF patients was more than twice that of IPF patients (78.9% vs. 34%, p < 0.001), and the survival rate of patients with a GAP score of 0–2 was more than twice that of patients with a score of > 2 (93.2% vs. 36.6%, p < 0.001). Older age, male gender, definite UIP pattern, higher GAP score, higher mMRC dyspnea score, lower forced expiratory volume in one second/forced vital capacity (FEV1/FVC), shorter 6MWT distance, and lower initial and final SpO2 were also associated with higher long-term mortality (p < 0.05). In multivariable analysis, only a GAP score of > 2 (hazard ratio [HR]:16.7; 95% confidence interval [CI] 3.28–85.14; p = 0.001) and definite UIP pattern (HR: 4.08; 95% CI 1.07–15.5; p = 0.039) were significantly associated with overall mortality.
Conclusion
The long-term mortality rate of IPF patients was higher than that of CTD-ILD patients. The GAP score and UIP patterns were significant mortality predictors for both IPF and CTD-ILD patients.
Similar content being viewed by others
Background
Fibrotic interstitial lung diseases (F-ILDs) are a miscellaneous group of disorders with the hallmark of lung scaring or fibrosis [1], which compromises the respiratory system’s oxygenation and diffusing capacity for carbon monoxide (DLCO) [2]. There are over 200 F-ILDs, many of which share clinical, radiological, and pathological characteristics. Major etiologies of F-ILDs include idiopathic conditions like idiopathic interstitial pneumonia and idiopathic pulmonary fibrosis (IPF) [3], as well as connective tissue disease-associated ILDs (CTD-ILDs) like those linked to rheumatoid arthritis [4].
Idiopathic pulmonary fibrosis is one of the most aggressive ILDs and currently lacks a definitive cure. In IPF, excessive fibroblast proliferation leads to increased deposition of extracellular matrix proteins, especially collagen. This exacerbates recurrent scarring and fibrosis of the lung parenchyma, increasing pulmonary rigidity. Consequently, the ability to take up oxygen and exchange gases is impaired. Prognosis after an IPF diagnosis is poor, with a median survival of 2–3 years. The etiology of IPF remains uncertain, and there are no effective treatments that significantly improve patient outcomes [5]. Furthermore, the nosological validity of IPF itself is debated. Some advocate splitting it into different subtypes with unique responses to tailored therapies, while others promote lumping IPF with other advancing fibrotic lung diseases that share common pathogenetic mechanisms and disease progression [6]. These advancements suggest a trend towards precision-based methodologies in comprehending and treating ILD, emphasizing individualized therapeutic strategies and nuanced classifications. [7].
Patients with IPF often face significant comorbidities that impact their overall health and quality of life. Depression is a common comorbidity, as highlighted by Tzouvelekis et al. [8], which emphasizes its detrimental impact on the wellbeing of individuals with IPF. Additionally, there is a notable association between IPF and an increased risk of lung cancer, as detailed by Karampitsakos et al. [9] and further corroborated by the DIAMORFOSIS survey [10]. These studies underscore the need for comprehensive care strategies that address not only the pulmonary condition but also the accompanying comorbidities to improve the overall prognosis and quality of life for patients with IPF.
Given the extensive pathological and prognostic diversity of ILDs combined with clinical and radiological mimicry, multidisciplinary discussion (MDD) between experts, including pulmonologists, radiologists, pathologists, and rheumatologists, is critical for accurate ILD diagnosis as highlighted by the American Thoracic Society and European Respiratory Society since 2001 [11]. Recently published guidelines and epidemiological studies further emphasize the necessity and value of MDDs in ILD management [12, 13]. Compared to individual physician diagnoses, MDD enhances diagnostic confidence and inter-observer agreement between ILD specialists [14, 15].
Several prospective ILD registries have been initiated in North America and Europe [16,17,18]. Well-designed patient registries can provide real-world data on clinical practice, outcomes, safety, cost-effectiveness and guideline compliance. They elucidate the disease course and inform clinical decision-making [19,20,21]. However, few epidemiological studies on ILDs exist in Asia [22]. In addition, many registries focus solely on IPF, with limited data on other fibrotic ILDs like CTD-ILDs and non-IPF disorders [23]. The gender–age–physiology (GAP) score, modified Medical Research Council (mMRC) dyspnea scale, ventilatory efficiency slope, six-minute walk test (6MWT) distance, DLCO, and arterial CO2 pressure at maximal exercise may be predictors of mortality [24,25,26]. The SENSCIS [27] and INBUILD [28] trials showed the benefits of treatment with antifibrotics for systemic sclerosis-ILD, CTD-ILDs, and progressive non-IPF fibrotic ILDs. Thus, registries that include both IPF and non-IPF patients are warranted. Identification of prognostic factors across fibrotic lung diseases is critical for early introduction of antifibrotics and rehabilitation [29, 30].
The Registry of Interstitial Lung Diseases (REGILD) is a prospective, single-center registry study enrolling IPF and non-IPF populations in central Taiwan. Every patient enrolled in the REGILD registry is evaluated by MDD experts, including 3 pulmonologists, 3 rheumatologists, 2 radiologists, and 2 pathologists. CTD-ILD patients constitute a large cohort among non-IPF patients in the REGILD. Thus, our objective was to examine both common and unique long-term mortality predictors in IPF and CTD-ILD patients within a real-world prospective setting, emphasizing the significance of Multidisciplinary Discussion (MDD) in F-ILD diagnosis.
Methods
Study design, patient enrollment, and ethics
The REGILD is a prospective, single-center registry study that includes newly diagnosed patients with F-ILD, encompassing both IPF and non-IPF ILD patients. It is based at the Integrated Care Center for ILD at Taichung Veterans General Hospital, a tertiary referral center in Taiwan. Between December 2018 and December 2019, patients with F-ILDs confirmed with high-resolution computed tomography (HRCT) were enrolled after review by a multidisciplinary (MDD) team of expert pulmonologists, rheumatologists, radiologists, and pathologists. IPF patients were categorized as “definite,” “probable,” or “indeterminate” for IPF according to American Thoracic Society/European Respiratory Society/Japanese Respiratory Society/Latin American Thoracic Association guidelines [31]. F-ILD patients with diagnoses of established connective tissue disease were classified as CTD-ILD. Patients meeting criteria for interstitial pneumonia with autoimmune features (IPAF) were classified as IPAF.13 The exclusion criteria were age < 20 years and the presence of HIV infection. All enrolled patients provided written informed consent. This study complied with the Declaration of Helsinki and was approved by Taichung Veterans General Hospital Ethics Committee (approval number CE18325B, December 18, 2018) (Additional file 1: Fig. S1).
Protocol for assessment of ILD in the REGILD cohort
The index day was defined as the day the patient signed the informed consent form. On the same day, participants completed the mMRC dyspnea scale questionnaire. Within 1 week of enrollment, participants underwent pulmonary function testing (PFT) and the 6MWT. Baseline demographic data, including age and gender, were recorded. The clinical data collected comprised presenting symptoms, physical examination findings, and antifibrotic medication use. The GAP score was calculated for each patient [3].
PFT and 6MWT procedure
Forced vital capacity (FVC) and the DLCO were obtained from spirometry results according to the recommendations of the American Thoracic Society [32]. The 6MWT was performed according to the guidelines of the American Thoracic Society [33]. The patients were instructed to walk as far as possible within 6 min between two orange traffic cones placed 30 m apart in a corridor. Data on oxygen saturation (SpO2) and the distance walked in 6 min were obtained.
Follow-up
The patients were followed up for mortality at yearly intervals. The cut-off date for death was February 1, 2023. The annual and overall incidences of mortality were recorded.
Statistical analysis
Descriptive analysis was performed with absolute numbers and relative frequencies of categorical data. Continuous variables were presented as median (interquartile range [IQR]) for non-parametric data. The Mann–Whitney U test was used to compare continuous variables. The chi-square test and Fisher’s exact test were used to compare categorical variables. Univariate and multivariate Cox proportional hazards regression models were used to examine possible factors of mortality. Kaplan–Meier estimates and log-rank tests were used to calculate mortality rates. Statistical analyses were performed using SPSS Statistics (version 22; IBM Corporation, Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
Results
Baseline characteristics and pulmonary physiology
Table 1 shows the characteristics of the patients in the registry. One hundred and four participants were enrolled: 33 (31.7%) were IPF and 71 (68.3%) were CTD-ILD. Their median age was 63 (IQR 58–69.8) years; most (61.5%) were females, and the majority (58.7%) had a definite usual interstitial pneumonia (UIP) pattern. The cohort had a median GAP score of 3 (IQR 1–3) and their median 6MWT was 446 (IQR 379.5–504.8) meters. Only 32 (30.8%) patients received antifibrotic medications. During a median follow-up duration of 4.1 (IQR 3.4–4.4) years, the annual mortality rate increased by about 6%, the 4-year mortality rate was 27.9%, and the overall mortality rate was 31.7%.
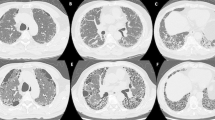
Table 2 compares demographic characteristics of IPF patients and CTD-ILD patients. Compared to patients with CTD-ILD, patients with IPF were older and more often male. In our registry, among patients without IPF, the most common CTD was idiopathic inflammatory myositis (35.5%), followed by primary systemic sclerosis (29.0%) and IPAF (12.7%). The proportion with UIP patterns on HRCT scans was higher in the IPF (81.8%) than in the CTD-ILD (47.9%) group (p = 0.002). This was refined with 14.1% (10 out of 71) and classified as a definite UIP pattern and 33.8% (24 out of 71) to a probable UIP pattern in accordance with the latest guidelines [3]. The median GAP score of the IPF group was 3 (IQR = 2–4.5), compared to 2 of the CTD-ILD group (IQR = 1–3, p < 0.001). The mMRC dyspnea score was higher in the IPF group than in the CTD-ILD group (1 [IQR = 1–3] vs. 1 [IQR = 0–1], p = 0.014). The proportion of patients receiving antifibrotic agents was higher in the IPF group than in the CTD-ILD group (60.6% vs. 16.9%, p < 0.001).
In this cohort, baseline FVC, forced expiratory volume in one second (FEV1), and DLCO (% predicted) data did not differ significantly between groups. The CTD-ILD group had greater 6MWT distances than the IPF group. SpO2 before and after the 6MWT did not differ significantly between the IPF and CTD-ILD groups. More than half of the participants in both groups had a nadir SpO2 of < 90%. At the end of follow-up, 60.6% of IPF patients were deceased compared to only 18.3% of CTD-ILDs patients (p < 0.001).
Primary outcome of overall mortality
Of the 104 patients, 33 died by the cutoff date of February 1, 2023; 20 had IPF and 13 had CTD-ILD (Table 3). Older age, male sex, IPF, UIP pattern, high GAP score, high mMRC score, and use of pulmonary fibrosis drugs were associated with higher mortality (p < 0.001). The long-term mortality of patients with lower FEV1/FVC, shorter 6-min walking distance, and lower initial and final SpO2 was higher (p < 0.05; Table 3).
The overall survival rate of CTD-ILD patients was more than twice that of IPF patients (78.9% vs. 34%, p < 0.001; Fig. 1). The overall survival rate of patients with a GAP score of 0–2 was also significantly higher than that of patients who scored > 2 (93.2% vs. 36.6%, p < 0.001; Fig. 2). Likewise, the overall survival rate of patients with a non-definite UIP pattern was significantly higher than that of patients with a definite UIP pattern (83.2% vs, 51.2%, p < 0.001; Fig. 3).
Univariate and multivariate analyses of factors associated with overall mortality
Cox proportional hazards regression analysis of mortality is shown in Table 4. In univariate analyses, higher age, male gender, IPF, definite UIP pattern, higher GAP score, higher mMRC dyspnea score, lower DLCO (% predicted), lower 6MWT distance, lower initial SpO2, lower SpO2 after 6MWT, and lower nadir SpO2 were significantly associated with mortality. In the multivariate analysis, only a GAP score > 2 (hazard ratio [HR] 16.7, 95% CI 3.28–85.14, p = 0.001) and definite UIP pattern (HR 4.08, 95% CI 1.07–15.5, p = 0.039) were significantly associated with overall mortality.
Discussion
In this prospective cohort study, we recorded baseline clinical, physiological, and radiological characteristics of patients with IPF and CTD-ILDs and followed them up for more than four years. The long-term mortality rates of patients with IPF, definite UIP pattern, and a GAP score of > 2 were significantly higher than those of patients with CTD-ILDs, non-definite UIP pattern, and a GAP score of 0–2. Nevertheless, in the multivariate analysis of factors potentially associated with mortality, the GAP score and definite UIP pattern were the only significant predictors of overall mortality.
Although the study cohort had relatively advanced disease, as indicated by the GAP score, PFT, and 6MWT parameters, only one third of the cohort, most of them belonging to the IPF group, received antifibrotic medications. This may explain the paradoxically higher proportion of antifibrotic receivers (54.5%) in the mortality group. The early start of antifibrotic medication for ILD patients is of fundamental importance. The rate of decline in lung function was similar in both IPF groups with preserved or reduced lung function; antifibrotic treatment was effective in both groups. Therefore, antifibrotic medications should be started for IPF, irrespective of symptoms or lung function [34]. The use of antifibrotic medications to treat many non IPF-ILDs was recently recommended [34]. In Taiwan, two antifibrotic medications—nintedanib and pirfenidone—are currently reimbursed by National Health Insurance for patients with IPF and interstitial lung disease associated with systemic sclerosis [35].
In our study, the long-term mortality of patients with IPF was higher than that of patients with CTD-ILD, confirming previous research showing worse prognosis of IPF [36]. The median survival of patients with IPF is 2–5 years after diagnosis [3], while CTD-ILD patients tend to have more favorable outcomes [36]. The mechanisms underlying this difference in mortality remain unclear but are likely to be related to differences in pathogenesis between IPF and CTD-ILD [36].
Importantly, our study demonstrated that the GAP score and UIP pattern on imaging are significant predictors of long-term mortality in both IPF and CTD-ILD. These common prognostic factors could be applied to ILD patients regardless of whether they have IPF or CTD-ILD. The GAP model predicting mortality risk based on gender, age, and physiology was originally developed for IPF [3]. However, previous studies and our findings show that the GAP score is also a predictor of mortality across other ILD subtypes including CTD-ILD [37]. On the other hand, the UIP pattern predicts worse prognosis in both IPF and CTD-ILD [38, 39]. That the GAP score and UIP pattern can be used in prognostication for all ILD patients underscores key commonalities in disease behavior between IPF and CTD-ILD.
Identification of these shared mortality predictors is crucial because it could prompt earlier interventions like treatment with antifibrotics or enrollment in pulmonary rehabilitation across ILD subtypes. Such measures could potentially prolong patients’ lives. Specifically, physicians should closely monitor the results of function tests like DLCO for decreases signifying progression, even in patients with CTD-ILD. Declines in physiology scores factor into worsening GAP scores; therefore, maintaining function is imperative. With further validation, these predictors could be incorporated into clinical decision tools guiding screening, follow-up, and treatment protocols to improve patient outcomes.
Our study has limitations that warrant further consideration. As a single-center study with only 104 patients, its sample size and generalizability are limited. Inclusion of longitudinal PFT and radiological data could have provided deeper insights into mortality predictors. Nonetheless, our findings offer a useful perspective on long-term prognostication in fibrotic ILDs. Moving forward, larger multicenter collaborations, such as the PROgressive Fibrosing lung diseasES.network, may enable more robust prognostic modeling.
Conclusion
The long-term mortality rate of IPF patients was higher than that of CTD-ILD patients. The GAP score and UIP patterns were significant mortality predictors for both IPF and CTD-ILD patients. While validation of these findings with larger cohorts is warranted, they could help physicians and decision-makers to take more effective steps, such as earlier start of antifibrotic medications, for managing ILD patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
22 February 2024
The values in Table 4 which was incorrectly processed with bold font was changed to regular font.
Abbreviations
- 6MWT:
-
6-Minute walking test
- CTD-ILD:
-
Connective tissue disease-associated interstitial lung disease
- DLCO:
-
Diffusing capacity for carbon monoxide
- F-ILD:
-
Fibrotic interstitial lung disease
- GAP:
-
Gender–age–physiology
- HR:
-
Hazard ratio
- HRCT:
-
High-resolution computed tomography
- IPF:
-
Idiopathic pulmonary fibrosis
- IQR:
-
Interquartile range
- IPAF:
-
Interstitial pneumonia with autoimmune features
- FEV1/FVC:
-
Lower forced expiratory volume in one second/forced vital capacity
- mMRC:
-
Modified Medical Research Council
- MDD:
-
Multidisciplinary discussion
- REGILD:
-
Registry of Interstitial Lung Diseases
- UIP:
-
Usual interstitial pneumonia
References
George PM, Spagnolo P, Kreuter M, Altinisik G, Bonifazi M, Martinez FJ, et al. Progressive fibrosing interstitial lung disease: clinical uncertainties, consensus recommendations, and research priorities. Lancet Respir Med. 2020;8:925–34.
Kumar DP. Assessment and follow-up of interstitial lung disease. Indian J Rheumatol. 2021;16:S69-78.
Raghu G, Remy-Jardin M, Richeldi L, Thomson CC, Inoue Y, Johkoh T, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2022;205:e18–47.
Zamora-Legoff JA, Krause ML, Crowson CS, Ryu JH, Matteson EL. Progressive decline of lung function in rheumatoid arthritis-associated interstitial lung disease. Arthritis Rheumatol. 2017;69:542–9.
Spagnolo P, Kropski JA, Jones MG, Lee JS, Rossi G, Karampitsakos T, et al. Idiopathic pulmonary fibrosis: disease mechanisms and drug development. Pharmacol Ther. 2021;222:107798.
Wells AU, Brown KK, Flaherty KR, Kolb M, Thannickal VJ. What’s in a name? That which we call IPF, by any other name would act the same. Eur Respir J. 2018;51:1800692.
Karampitsakos T, Juan-Guardela BM, Tzouvelekis A, Herazo-Maya JD. Precision medicine advances in idiopathic pulmonary fibrosis. EBioMedicine. 2023;95:104766.
Tzouvelekis A, Karampitsakos T, Kourtidou S, Bouros E, Tzilas V, Katsaras M, et al. Impact of depression on patients with idiopathic pulmonary fibrosis. Front Med. 2020;7(7):29.
Karampitsakos T, Spagnolo P, Mogulkoc N, Wuyts WA, Tomassetti S, Bendstrup E, et al. Lung cancer in patients with idiopathic pulmonary fibrosis: a retrospective multicentre study in Europe. Respirology. 2023;28:56–65.
Tzouvelekis A, Antoniou K, Kreuter M, Evison M, Blum TG, Poletti V, et al. The DIAMORFOSIS (DIAgnosis and Management Of lung canceR and FibrOSIS) survey: international survey and call for consensus. ERJ Open Res. 2021;7:00529–2020.
American Thoracic S, European Respiratory S. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165:277–304.
Sharif R. Overview of idiopathic pulmonary fibrosis (IPF) and evidence-based guidelines. Am J Manag Care. 2017;23:S176–82.
Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–48.
Flaherty KR, King TE Jr, Raghu G, Lynch JP 3rd, Colby TV, Travis WD, et al. Idiopathic interstitial pneumonia: what is the effect of a multidisciplinary approach to diagnosis? Am J Respir Crit Care Med. 2004;170:904–10.
Sanduzzi Zamparelli S, Sanduzzi Zamparelli A, Bocchino M. The evolving concept of the multidisciplinary approach in the diagnosis and management of interstitial lung diseases. Diagnostics (Basel). 2023;13:2437.
Kaul B, Cottin V, Collard HR, Valenzuela C. Variability in global prevalence of interstitial lung disease. Front Med. 2021;8:751181.
Fischer A, Antoniou KM, Brown KK, Cadranel J, Corte TJ, du Bois RM, et al. An official European Respiratory Society/American Thoracic Society research statement: interstitial pneumonia with autoimmune features. Eur Respir J. 2015;46:976–87.
Hambly N, Farooqi MM, Dvorkin-Gheva A, Donohoe K, Garlick K, Scallan C, et al. Prevalence and characteristics of progressive fibrosing interstitial lung disease in a prospective registry. Eur Respir J. 2022;60:2102571.
Gliklich RE, Dreyer NA, Leavy MB. Registries for evaluating patient outcomes: a user’s guide. 4th ed. Rockville: Agency for Healthcare Research and Quality (US); 2020.
Barczi E, Starobinski L, Kolonics-Farkas A, Eszes N, Bohacs A, Vasakova M, et al. Long-term effects and adverse events of nintedanib therapy in idiopathic pulmonary fibrosis patients with functionally advanced disease. Adv Ther. 2019;36:1221–32.
Guler SA, Zumstein P, Berezowska SA, Pöllinger A, Geiser T, Funke-Chambour M. Idiopathic pulmonary fibrosis in a Swiss interstitial lung disease reference centre. Swiss Med Wkly. 2018;148:w14577.
Ye Y, Hubbard R, Li GHY, Ho SC, Sing CW, Cheung CL, et al. Validation of diagnostic coding for interstitial lung diseases in an electronic health record system in Hong Kong. Pharmacoepidemiol Drug Saf. 2022;31:519–23.
Fisher J, Kolb M, Algamdi M, Morisset J, Johannson K, Shapera S, et al. Baseline characteristics and comorbidities in the CAnadian REgistry for Pulmonary Fibrosis. BMC Pulm Med. 2019;19:1–9.
Cheng Y-Y, Lin S-Y, Chang S-T, et al. Cardiopulmonary Exercise Test, mMRC and GAP score can Predict 1-year Mortality in Patients with Idiopathic Pulmonary Fibrosis: a Prospective Study. 15 Feb 2021,PREPRINT (Version 1) available at Research Square https://doi.org/10.21203/rs.3.rs-192679/v1.
Mancuzo EV, Soares MR, Pereira CAdC. Six-minute walk distance and survival time in patients with idiopathic pulmonary fibrosis in Brazil. J Bras Pneumol. 2018;44:267–72.
Mena-Vázquez N, Rojas-Gimenez M, Romero-Barco CM, Manrique-Arija S, Francisco E, Aguilar-Hurtado MC, et al. Predictors of progression and mortality in patients with prevalent rheumatoid arthritis and interstitial lung disease: a prospective cohort study. J Clin Med. 2021;10:874.
Distler O, Highland KB, Gahlemann M, Azuma A, Fischer A, Mayes MD, et al. Nintedanib for systemic sclerosis-associated interstitial lung disease. N Engl J Med. 2019;380:2518–28.
Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SL, Inoue Y, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med. 2019;381:1718–27.
Matsuo S, Okamoto M, Ikeuchi T, Zaizen Y, Inomoto A, Haraguchi R, et al. Early intervention of pulmonary rehabilitation for fibrotic interstitial lung disease is a favorable factor for short-term improvement in health-related quality of life. J Clin Med. 2021;10:3153.
Sugino K, Ono H, Watanabe N, Ando M, Tsuboi E, Homma S, et al. Efficacy of early antifibrotic treatment for idiopathic pulmonary fibrosis. BMC Pulm Med. 2021;21:1–10.
Ley B, Ryerson CJ, Vittinghoff E, Ryu JH, Tomassetti S, Lee JS, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Inter Med. 2012;156:684–91.
Beydon N, Davis SD, Lombardi E, Allen JL, Arets HG, Aurora P, et al. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J Respir Crit Care Med. 2007;175:1304–45.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Rai DK, Tripathi S. Antifibrotic in interstitial lung diseases: when, where, and how long? Lung India. 2022;39:491–4.
Cheng SL, Sheu CC, Chian CF, Hsu JY, Kao KC, Hang LW, et al. NICEFIT—a prospective, non-interventional, and multicentric study for the management of idiopathic pulmonary fibrosis with antifibrotic therapy in Taiwan. Biomedicines. 2022;10:2362.
Oliveira RP, Ribeiro R, Melo L, Grima B, Oliveira S, Alves JD. Connective tissue disease-associated interstitial lung disease. Pulmonology. 2022;28:113–8.
Ryerson CJ, Vittinghoff E, Ley B, Lee JS, Mooney JJ, Jones KD, et al. Predicting survival across chronic interstitial lung disease: the ILD-GAP model. Chest. 2014;145:723–8.
Lynch DA, Godwin JD, Safrin S, Starko KM, Hormel P, Brown KK, et al. High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med. 2005;172:488–93.
Mononen ME, Kettunen HP, Suoranta SK, Kärkkäinen MS, Selander TA, Purokivi MK, et al. Several specific high-resolution computed tomography patterns correlate with survival in patients with idiopathic pulmonary fibrosis. J Thorac Dis. 2021;13:2319–30.
Acknowledgements
The editorial assistance was provided to the authors by Nova Journal Experts.
Funding
This study was supported by Taichung Veterans General Hospital (TCVGH-1127307D; TCVGH-1123104D; TCVGH-1128303D; TCVGH-1123510C & TCVGH-1123511C).
Author information
Authors and Affiliations
Contributions
YWL conceived and designed the study, analyzed and interpreted the data, and drafted the manuscript. MCL conceived and designed the study, analyzed and interpreted the data, and drafted the manuscript. YCW acquired the data. CYH acquired the data. WNH analyzed and interpreted the data. YHC analyzed and interpreted the data. PKF conceived and designed the study, analyzed and interpreted the data, drafted the manuscript, revised the manuscript, validated the data, and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study complied with the Declaration of Helsinki and was approved by the Taichung Veterans General Hospital Ethics Committee (approval number CE18325B, December 18, 2018). A written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Study flowchart outlining the total number of cases during the study period.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liao, YW., Liu, MC., Wu, YC. et al. Factors influencing long-term outcomes in fibrotic interstitial lung disease (F-ILD) diagnosed through multidisciplinary discussion (MDD): a prospective cohort study. Eur J Med Res 29, 91 (2024). https://doi.org/10.1186/s40001-024-01673-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01673-2