Abstract
Background
Underdiagnosis of migraine causes a significant health burden, including lower quality of life, excessive medication use, and a delay in effective treatment. The purpose of this study was to evaluate migraine diagnosis accuracy and to review the treatment approaches used by neurologists in the Baltic states.
Methods
The research was conducted as an anonymous e-survey with four cases in March and April 2021.
Results
119 practicing adult neurologists have participated. The migraine diagnostic accuracy was 63.2%. The most commonly used diagnostic criteria were moderate/severe pain, unilateral pain, and disruption of daily activities. Diagnostic accuracy did not differ significantly between neurologists who always use ICHD-3 criteria and those who don’t (68.4% vs. 58.5%, p = 0.167). It was higher in neurologists who were working in headache centers (91.7% vs. 60.9%, p = 0.012), and was related to a higher percentage of migraine diagnoses in all consulted headache patients (R2 = 0.202, adjusted R2 = 0.195, p < 0.001), prophylaxis with onabotulinumtoxin A [OR = 4.332, 95% Cl (1.588–11.814)], and anti-CGRP monoclonal antibodies [OR = 2.862, 95% Cl (1.186–6.907)].
Conclusions
Migraine diagnostic accuracy is improved through practical patient counseling and modern treatment prescription. Although the neurologists in the Baltic states follow current European guidelines, there is room for improvement in diagnostic accuracy to reduce migraine burden.
Similar content being viewed by others
Background
There are many up-to-date resources available to learn how to recognize migraine effectively, including international [1] and national guidelines, and other easy-to-use recommendations [2]. According to the Global Burden of Diseases study, 3.07 billion people worldwide suffer from headaches, with migraine accounting for 43.37% of the total [3]. Nevertheless, in many parts of the world, migraine remains underdiagnosed and undertreated [4, 5]. In one Italian study, out of 953 migraine patients referred to headache center only 26.8% had a previous migraine diagnosis [6]. In another study conducted in the United States, 80% of 2991 sinusitis-related headache patients were instead diagnosed with migraine and 8% fulfilled diagnostic criteria for possible migraine diagnosis during the study [7]. Moreover, only 12.4% of 266 migraine patients were previously diagnosed with migraine in the Russian survey [8]. Reasons for insufficient migraine diagnosis include low awareness among the patients [9], insufficient knowledge of migraine between the doctors [10, 11], a lack of biological migraine markers, and the patient history being the sole basis of migraine diagnosis [1]. In addition, it has been demonstrated that headache subspecialization is not highly prestigious or attractive among neurologists [12,13,14]. Insufficient migraine diagnosis results in poor quality of life, economic burden, medication overuse and increases the risk of chronic migraine, comorbidities, and treatment refractoriness [15, 16]. Furthermore, it leads to a delay in seeking out available modern treatment [17].
Despite the fact that general practitioners should be able to identify and treat the majority of migraine cases, in the Baltic states migraine diagnosis is most commonly made by a neurologist. Furthermore, the Baltic countries lack specialized headache clinics, and access to modern migraine treatment varies greatly between the states. For example, Lithuania is unique in that the state fully reimburses two monoclonal antibodies against calcitonin-gene-related peptide (CGRP) or its receptor (fremanezumab, erenumab), allowing for effective migraine treatment, whereas onabotulinumtoxin A treatment for chronic migraine is only reimbursed in Estonia. In addition, even acute migraine treatment is not reimbursed in Latvia.
The three major gaps in headache care quality include overutilization of neuroimaging, underuse of preventive therapies, and inappropriate acute headache treatment. Lifting The Burden (LTB) and European Headache Federation (EHF) developed a set of headache service quality indicators, with accurate diagnosis being one of the nine major quality domains required for optimal headache care [18]. The panel of experts has formulated a multidimensional definition of quality of headache care: “good quality care achieves accurate diagnosis and individualized management, has appropriate referral pathways, educates patients about their headaches and their management, is convenient and comfortable, satisfies patients, is efficient and equitable, assesses outcomes and is safe.” [18, 19]. As part of a collaborative project between LTB and EHF, the service quality evaluation program tested these nine indicators in specialized headache centers and at the primary care level while also establishing standards of excellence for specialized headache centers [20]. The research has revealed that diagnostic inaccuracies were the most prevalent in primary care, where a significant proportion of patients received non-specific ICD-10 codes such as R51 (“headache”) rather than specific headache diagnoses. In contrast, ICHD-3 terminology was used in more than 90% of cases in specialized headache centers [18]. An analogous situation was observed with the recording of headache histories (especially time profiles) and the use of headache calendars and diaries, which were more accurate in specialized headache centers than in primary care [20].
The aim of this study was to compare the answers to theoretical questions about diagnostic criteria and their actual application in the four clinical cases that were presented to assess the accuracy of migraine diagnosis and to review the treatment approaches employed by neurologists in the Baltic states. The study's hypothesis was that practical migraine patient counseling and modern treatment prescription, rather than theoretical knowledge of International Classification of Headache Disorders third edition (ICHD-3) criteria, improves migraine diagnostic accuracy.
Methods
We designed a questionnaire for this cross-sectional study that included the following sections: (1) demographic information (age, sex, occupation, years of practice, workplace type), (2) headache diagnosis-related information (the number of patients with headache in general and migraine among all consultations, the use of ICHD-3 criteria [1], types of migraine that one finds difficult to diagnose), (3) four clinical cases (with provided five most likely diagnoses, and single choice answer), and (4) questions related to the use of pharmacological and non-pharmacological migraine treatment and evaluation of its efficacy. The full questionnaire is presented in Additional file 1. The four clinical cases (two cases of migraine without aura, one case of migraine with aura, and one case of chronic migraine with medication overuse headache) were created following diagnostic criteria of ICHD-3 by a panel of three highly experienced headache specialists. The first clinical case of migraine without aura included all four migrainous headache characteristics according to ICHD-3 (unilateral, pulsating, moderate intensity, aggravated by physical activity) followed by one accompanying symptom (photo-/phonophobia). The second clinical case of migraine without aura included only two migrainous headache characteristics i.e., the bare minimum required for migraine diagnosis (severe intensity and aggravation by physical activity) followed by one accompanying symptom (nausea). The third clinical case of migraine with aura included typical aura symptoms (gradually appearing and fully reversible visual, sensory, and language symptoms with a total duration of 1 h) followed by non-migrainous headache or no headache. The fourth clinical case of chronic migraine with medication overuse headache included a typical duration and frequency of headache (almost every day, being severe 15 days per month, for many years), three migrainous headache characteristics (pulsating, severe intensity, aggravated by physical activity), one accompanying symptom (nausea) and the overuse of non-opioid painkiller combination with caffeine (15 days per month).
An advisory panel of neurologists from each Baltic State (Estonia, Latvia, Lithuania) assessed the initial survey. Some small improvements were made during the assessment. A pilot version was completed by a group of 10 neurologists with no further adjustments. The final anonymous online questionnaire was distributed through various neurology organizations (Lithuanian Society of Neurology, Estonian Headache Society, Estonian Ludvig Puusepp Society of Neurologists and Neurosurgeons, Latvian Society of Neurology). Participants were included in the study if they were neurologists currently practicing adult neurology. The study was conducted in the Baltic States from March 12 to April 13, 2021.
The survey completion was voluntary, and no financial incentive was received by the study participants. None of the involved organizations received any funding for the distribution of the survey. Since the data acquired was anonymous and without the ability to identify a specific person, no ethics approval was sought. Ethics approval was deemed unnecessary by Vilnius Regional Biomedical Research Ethics Committee with respect to the General Data Protection Regulation Principle 26. All participants consented to participate by marking confirmation in the e-survey that they agree to the use of their anonymous data for scientific publication. According to Article 2 of the Republic of Lithuania's Law on Ethics of Biomedical Research, no particular informed consent was necessary, as affirmed by the Vilnius Regional Biomedical Research Ethics Committee, since anonymous surveys are not considered biomedical research.
Statistical analysis
Values were expressed as counts and frequencies for qualitative variables and as means or medians for quantitative variables, depending on the normality of the distribution. A statistical comparison between the three Baltic countries was done. Categorical variables were compared using the χ2 test (Pearson’s Chi-square or Fisher’s exact test when appropriate). The Kruskal–Wallis H test was used to compare non-parametric variables. Linear regression analysis was applied to identify the associations between independent quantitative variables and the diagnostic accuracy of migraine. We calculated unadjusted and adjusted R2, p values. The relationship between the independent categorical variables and correct answers in all clinical cases was assessed with logistic regression analysis. Odds ratios (OR), 95% confidence intervals (CI), and p values were computed. All statistical analyses were performed using IBM SPSS Statistics for Windows, V.20.0. For all comparisons, p < 0.05 was considered statistically significant.
Results
In total, 119 neurologists participated in the study, of them 76 (63.9%) from Lithuania, 30 (25.2%) from Latvia and 13 (10.9%) from Estonia. The proportion of neurologists who participated in the study compared to all neurologists with an active license at the time of the study was 17.7% (76/429) in Lithuania, 15.6% (30/192) in Latvia, and 10.2% (13/128) in Estonia. 74.8% of participants were female, the median age of participants was 52.0 ± 13 years (27–74), and the median duration of work experience was 22.0 ± 14 years (1–52). 88.2% of all participants worked in an outpatient clinic, 7.6% of all neurologists worked in a specialized headache center. Estonian neurologists worked in specialized headache centers more frequently (30.8%, p = 0.004). Neurologists' experience with migraine diagnosis in their clinical practice is presented in Table 1.
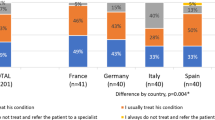
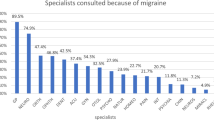
The three most commonly used migraine diagnostic criteria in clinical practice were: moderate/severe pain, unilateral pain, and disruption of daily activities (Fig. 1). Respondents indicated that vestibular migraine, persistent aura without infarction, episodic syndromes that may be associated with migraine, and chronic migraine were the most difficult-to-diagnose migraine types (Fig. 2).
There was a significant difference in the use of onabotulinumtoxin A and anti-CGRP monoclonal antibodies for prophylactic treatment of migraine between the Baltic states (Table 2).
The most commonly used migraine oral prophylaxis drugs were propranolol, amitriptyline, and topiramate, whereas lisinopril, candesartan, and coenzyme Q10 were the most commonly listed as never used (Fig. 3). Figure 4 depicts respondents' perception of the safety and efficacy of prophylactic migraine treatment.
The average number of correct clinical case answers was 2.53 ± 1.10. The total migraine diagnostic accuracy was found to be 63.2% (301/476), see Table 3.
A diagnostic accuracy was found to be significantly higher in neurologists who are working in specialized headache centers (91.7% vs. 60.9%, p = 0.012), diagnosing migraine in more than 50% of their headache patients (78.4% vs. 59.8%, p = 0.009), prescribing triptans (64.8% vs. 25.0%, p = 0.009), prescribing oral migraine prophylaxis (64.7% vs. 39.3%, p = 0.043). Diagnostic accuracy did not differ significantly between neurologists who always use ICHD-3 diagnostic criteria for migraine diagnosis and those who do not (68.4% vs. 58.5%, p = 0.167).
Linear regression models showed that the number of correct diagnoses was related to the percentage of migraine diagnoses in all consulted headache patients (R2 = 0.202, adjusted R2 = 0.195, p < 0.001), the younger age of neurologist (R2 = 0.092, adjusted R2 = 0.085, p = 0.001), and the shorter clinical work experience (R2 = 0.104, adjusted R2 = 0.096, p < 0.001). Significant logistic regression findings related to correct answers in all clinical cases included the use of onabotulinumtoxin A [OR = 4.332, 95% Cl (1.588–11.814)], the prescription of neuromodulation treatment [OR = 2.595, 95% Cl (1.011–6.657)], the prescription of anti-CGRP treatment [OR = 2.862, 95% Cl (1.186–6.907)] and the use of disability and/or other headache-specific scales in clinical practice [OR = 3.266, 95% Cl (1.278–8.344)].
Discussion
This is the first study to explore the diagnostic accuracy of migraine between neurologists in the Baltic States. While we must acknowledge the lack of validation, one of the strengths of our research is that it evaluates a practical approach to migraine diagnosis through clinical case solution rather than merely testing knowledge of ICHD-3 criteria. In addition, we collected data on the prescription of preventive treatment in daily practice and assessed neurologists' perspectives on migraine prevention. The hypothesis of our research has been confirmed as the diagnostic accuracy of migraine did not differ significantly between neurologists who always use ICHD-3 diagnostic criteria and those who do not (68.4% vs. 58.5%, p = 0.167). Nevertheless, despite being statistically insignificant, the difference of almost 10% may still be important clinically. The number of correct clinical case diagnoses was related to the higher percentage of migraine diagnoses in all consulted headache patients, the use of onabotulinumtoxin A, neuromodulation, and the prescription of anti-CGRP treatment. To the best of our knowledge, there have been no analogous studies in the literature concerning the migraine diagnostic accuracy by neurologists. Somewhat similar studies included physical therapists [21] and general practitioners [22, 23]. Nevertheless, the aforementioned studies used significantly different case vignettes and/or answer structures, and the presented diagnostic accuracy among different specialties cannot be compared.
The overall diagnostic accuracy of migraine among neurologists was found to be 63.2%. The diagnostic accuracy ranged from 50.8% in Latvia, to 65.5% in Lithuania and 78.9% in Estonia. The higher accuracy of Estonian neurologists could be explained by the fact that the majority of respondents worked in a more specialized headache center. Only 18.5% of respondents in their clinical practice diagnose migraine in over 50% of their headache patients. The small proportion of migraine diagnosis in everyday practice reflects the discrepancy between the actual migraine prevalence and the number of clinically diagnosed migraine. Therefore, a paradigm that has been formulated back in 2002 by Sheftell and Tepper should be remembered by many: “[…] episodes of disabling headache, with a stable pattern over years, should be viewed as migraine until proven otherwise.” [24].
In our study, the three most common symptoms used to diagnose migraine were pain intensity, location (unilateral), and headache impact on daily activities. Only one of these symptoms (disruption of daily activities) is used in “ID Migraine”—a validated migraine screening tool (the other two being nausea and photophobia) [25]. It was found by meta-analysis that “ID Migraine” is characterized by pooled sensitivity of 0.84 and specificity of 0.76 [26], whereas in a validation study [25], headache intensity and unilateral location were the two least specific symptoms for a migraine diagnosis. Nevertheless, the statement of consistent use of ICHD-3 criteria for migraine diagnosis was not found to be significantly associated with higher migraine diagnostic accuracy in our study. The responses regarding the use of the ICHD-3 criteria and the selection of the most important clinical criteria for migraine diagnosis partially contradicted the clinical case answers. The first case of migraine without aura had the highest diagnostic accuracy (87.4%), as it met all four diagnostic pain criteria. In contrast, 58% of neurologists did not recognize the second case's severe headache and associated vomiting as a migraine, most likely due to the lack of pulsating quality and unilateral location. Consequently, in the real world, such patients suffering from severe headache attacks would be left without migraine diagnosis and appropriate treatment. Another discrepancy can be seen between the second and fourth cases: while respondents indicated that chronic migraine was more difficult to diagnose than migraine without aura, the diagnostic accuracy of chronic migraine was higher in presented clinical cases. In summary, the use of clinical case challenges has the potential to increase the likelihood of detecting diagnostic errors. However, because there was no comparator group in this study, this conclusion is speculative.
Triptans are rarely used in the Baltic countries. Although a lack of reimbursement may account for the lower percentage of triptan use in Latvia, an analysis of the remaining data suggests that triptans might be preferentially used for severe attacks only. Propranolol, amitriptyline, and topiramate were the most commonly used migraine oral prophylaxis drugs by neurologists in the Baltic states. The use of these drugs is in accordance with the latest, but still in need of updating, European Federation of Neurological Societies' migraine treatment guidelines [27]. As many as 70.6% of neurologists indicated they had never prescribed candesartan, one of the most commonly prescribed drugs in Scandinavian countries near the Baltic States, and 42.9% indicated they had never prescribed venlafaxine. These two drugs were shown to be effective in migraine prevention much later than propranolol, amitriptyline, and topiramate. Therefore, such result could be attributed to a lack of latest knowledge about preventative migraine treatment.
Finally, different drug reimbursement laws between the Baltic states may have resulted in disparities in modern preventive treatment. All respondents rated anti-CGRP monoclonal antibodies as not only the most effective, but also one of the safest migraine treatments. While Lithuanian neurologists have extensive experience with erenumab and fremanezumab due to drug reimbursement for several years now, numerous studies, including meta-analyses [28, 29], have also confirmed the efficacy and safety of anti-CGRP treatment. On the other hand, neuromodulation had received the most neutral answers in both characteristics of safety and efficacy. In authors’ opinion, this could be explained by the lower availability (no reimbursement in any of the Baltic states), novelty of external trigeminal nerve stimulation and non-invasive vagal nerve stimulation, and thus a lack of knowledge and experience with this treatment approach.
There are several limitations to our research. Firstly, merely 10 to 17% of neurologists with active licenses in the respective Baltic state participated in the study. The small number of respondents, as well as non-response bias due to the nature of electronic surveys (older respondents and those with limited knowledge of information technology may have been excluded), may significantly limit the generalizability of our study's findings. Secondly, since no additional diagnoses had to be provided in clinical cases, closed-ended questions could have resulted in greater diagnostic accuracy. In addition, no feedback questions were asked in the survey, i.e., respondents were not questioned as to why the diagnosis of migraine was not selected, which would aid in the more accurate preparation of educational materials for neurologists. Finally, we did not use a validated data collection method, and the clinical case creation was limited to an expert panel.
Conclusion
This is the first study to explore the diagnostic accuracy of migraine and treatment used by neurologists in the Baltic states. The results of our research show that the treatment used by neurologists complies with the latest European guidelines on effective migraine treatment. Nevertheless, to improve the quality of life of migraine patients, it is not enough for neurologists to know what treatment should be prescribed—a sufficient number of patients must also receive it. To achieve this goal, it is necessary to improve migraine diagnostic accuracy as well as to increase the use of effective acute and preventive migraine treatment.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Olesen J. Headache classification committee of the international headache society (IHS) the international classification of headache disorders. Cephalalgia. 2018;38:1–211. https://doi.org/10.1177/0333102417738202.
Eigenbrodt AK, Ashina H, Khan S, Diener HC, Mitsikostas DD, Sinclair AJ, et al. Diagnosis and management of migraine in ten steps. Nat Rev Neurol. 2021;17:501–14. https://doi.org/10.1038/S41582-021-00509-5.
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Buse DC, Armand CE, Charleston L, Reed ML, Fanning KM, Adams AM, et al. Barriers to care in episodic and chronic migraine: Results from the Chronic Migraine Epidemiology and Outcomes Study. Headache. 2021;61:628–41. https://doi.org/10.1111/HEAD.14103.
Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204. https://doi.org/10.1016/S0140-6736(20)30925-9.
Cevoli S, D’amico D, Martelletti P, Valguarnera F, del Bene E, de Simone R, et al. Underdiagnosis and undertreatment of migraine in italy: a survey of patients attending for the first time 10 headache centres. Cephalalgia. 2009;29:1285–93. https://doi.org/10.1111/J.1468-2982.2009.01874.X.
Schreiber CP, Hutchinson S, Webster CJ, Ames M, Richardson MS, Powers C. Prevalence of migraine in patients with a history of self-reported or physician-diagnosed “sinus” headache. Arch Intern Med. 2004;164:1769–72. https://doi.org/10.1001/ARCHINTE.164.16.1769.
Lebedeva ER, Kobzeva NR, Gilev DV, Olesen J. The quality of diagnosis and management of migraine and tension-type headache in three social groups in Russia. Cephalalgia. 2016;37:225–35. https://doi.org/10.1177/0333102416642603.
Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe—evidence from the Eurolight study. J Headache Pain. 2018. https://doi.org/10.1186/S10194-018-0839-1.
Ahmed ZA, Faulkner LR. Headache education in adult neurology residency: a survey of program directors and chief residents. Headache. 2016;56:871–7. https://doi.org/10.1111/HEAD.12822.
Do TP, Dømgaard M, Stefansen S, Kristoffersen ES, Ashina M, Hansen JM. Barriers and gaps in headache education: a national cross-sectional survey of neurology residents in Denmark. BMC Med Educ. 2022. https://doi.org/10.1186/S12909-022-03299-6.
Kristoffersen ES, Winsvold BS, Faiz KW. Prestige of neurological disorders among future neurologists in Norway. Acta Neurol Scand. 2019;139:555–8. https://doi.org/10.1111/ANE.13087.
Jokubaitis M, Kõrv J, Karelis G, Jatužis D, Vaitkus A, Ryliškienė K. Subspecialty training of neurology residents and junior neurologists in the Baltic States. Eur J Neurol. 2021;28:3584–90. https://doi.org/10.1111/ENE.14978.
Glavind M, Kristensen H, Thien Do P, Pozo-Rosich P, Faisal AM, et al. Interest in and exposure to headache disorders among neurology residents in Denmark: a nationwide cross-sectional survey. Acta Neurol Scand. 2022;146:568–72. https://doi.org/10.1111/ANE.13681.
Viticchi G, Falsetti L, Bartolini M, Buratti L, Ulissi A, Baldassari M, et al. Migraine: incorrect self-management for a disabling disease. Neurol Int. 2018;10:24–7. https://doi.org/10.4081/NI.2018.7510.
Lublóy Á. Economic burden of migraine in Latvia and Lithuania: direct and indirect costs. BMC Public Health. 2019;19:1–26. https://doi.org/10.1186/S12889-019-7461-2/TABLES/10.
Peres MFP, Swerts DB, de Oliveira AB, Silva-Neto RP. Migraine patients’ journey until a tertiary headache center: an observational study. J Headache Pain. 2019;20:1–8. https://doi.org/10.1186/S10194-019-1039-3/TABLES/7.
Lenz B, Katsarava Z, Gil-Gouveia R, Karelis G, Kaynarkaya B, Meksa L, et al. Headache service quality evaluation: implementation of quality indicators in primary care in Europe. J Headache Pain. 2021;22:1–12. https://doi.org/10.1186/S10194-021-01236-4/FIGURES/3.
Peters M, Perera S, Loder E, Jenkinson C, Gouveia RG, Jensen R, et al. Quality in the provision of headache care. 1: systematic review of the literature and commentary. J Headache Pain. 2012;13:437–47. https://doi.org/10.1007/S10194-012-0466-1.
Schramm S, Uluduz D, Gouveia RG, Jensen R, Siva A, Uygunoglu U, et al. Headache service quality: evaluation of quality indicators in 14 specialist-care centres. J Headache Pain. 2016;17:1–14. https://doi.org/10.1186/S10194-016-0707-9/TABLES/5.
Dale PC, Thomas JC, Hazle CR. Physical therapist clinical reasoning and classification inconsistencies in headache disorders: a United States survey. J Man Manip Ther. 2019;28:28–40. https://doi.org/10.1080/10669817.2019.1645414.
De Diego EV, Lanteri-Minet M. Recognition and management of migraine in primary care: influence of functional impact measured by the headache impact test (HIT). Cephalalgia. 2005;25:184–90. https://doi.org/10.1111/J.1468-2982.2004.00820.X.
de Klippel N, Jansen JP, Carlos JS. Survey to evaluate diagnosis and management of headache in primary care: headache management pattern programme. Curr Med Res Opin. 2008;24:3413–22. https://doi.org/10.1185/03007990802547139.
Sheftell FD, Tepper SJ. New paradigms in the recognition and acute treatment of migraine. Headache. 2002;42:58–69. https://doi.org/10.1046/J.1526-4610.2002.02015.X.
Lipton RB, Dodick D, Sadovsky R, Kolodner K, Endicott J, Hettiarachchi J, et al. A self-administered screener for migraine in primary care: the ID migraine validation study. Neurology. 2003;61:375–82. https://doi.org/10.1212/01.WNL.0000078940.53438.83.
Cousins G, Hijazze S, van de Laar FA, Fahey T. Diagnostic accuracy of the ID migraine: a systematic review and meta-analysis. Headache. 2011;51:1140–8. https://doi.org/10.1111/J.1526-4610.2011.01916.X.
Evers S, Áfra J, Frese A, Goadsby PJ, Linde M, May A, et al. EFNS guideline on the drug treatment of migraine—revised report of an EFNS task force. Eur J Neurol. 2009;16:968–81. https://doi.org/10.1111/J.1468-1331.2009.02748.X.
Soni P, Chawla E. Efficacy and safety of anti-calcitonin gene-related peptide monoclonal antibodies for treatment of chronic migraine: a systematic review and network meta-analysis. Clin Neurol Neurosurg. 2021;209:106893. https://doi.org/10.1016/J.CLINEURO.2021.106893.
Shi M, Guo J, Li Z, Sun H, Yang X, Yang D, et al. Network meta-analysis on efficacy and safety of different anti-CGRP monoclonal antibody regimens for prophylaxis and treatment of episodic migraine. Neurol Res. 2021;43:932–49. https://doi.org/10.1080/01616412.2021.1940672.
Acknowledgements
We would like to thank all neurologists who participated in this study.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Contributions
MJ wrote and revised the manuscript. GV designed methodology, created survey, translation, collected data from Lithuania and performed statistical analysis. LZ and MB created survey, reviewed the written manuscript, and provided critical review and commentary. ALR translated survey, collected and scrubbed data from Estonia. GS and DŽ translated survey, collected, and scrubbed data from Latvia. KR generated research idea, created survey, provided critical review and commentary, supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since the data acquired was anonymous and without the ability to identify a specific person, no ethics approval was sought. Ethics approval was deemed unnecessary by Vilnius Regional Biomedical Research Ethics Committee with respect to the General Data Protection Regulation Principle 26.
Consent for publication
All participants consented to participate by marking confirmation in the e-survey that they agree to the use of their anonymous data for scientific publication. According to Article 2 of the Republic of Lithuania's Law on Ethics of Biomedical Research, no particular informed consent was necessary, as affirmed by the Vilnius Regional Biomedical Research Ethics Committee, since anonymous surveys are not considered biomedical research.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Complete survey of the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jokubaitis, M., Vrublevska, G., Zvaune, L. et al. Accuracy of migraine diagnosis and treatment by neurologists in the Baltic states: e-survey with clinical case challenge. Eur J Med Res 28, 600 (2023). https://doi.org/10.1186/s40001-023-01555-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01555-z