Abstract
Background
The main problem of positron emission tomography/computed tomography (PET/CT) for lymph node (LN) staging is the high false positive rate (FPR). Thus, we aimed to explore a clinico-biological-radiomics (CBR) model via machine learning (ML) to reduce FPR and improve the accuracy for predicting the hypermetabolic mediastinal–hilar LNs status in lung cancer than conventional PET/CT.
Methods
A total of 260 lung cancer patients with hypermetabolic mediastinal–hilar LNs (SUVmax ≥ 2.5) were retrospectively reviewed. Patients were treated with surgery with systematic LN resection and pathologically divided into the LN negative (LN-) and positive (LN +) groups, and randomly assigned into the training (n = 182) and test (n = 78) sets. Preoperative CBR dataset containing 1738 multi-scale features was constructed for all patients. Prediction models for hypermetabolic LNs status were developed using the features selected by the supervised ML algorithms, and evaluated using the classical diagnostic indicators. Then, a nomogram was developed based on the model with the highest area under the curve (AUC) and the lowest FPR, and validated by the calibration plots.
Results
In total, 109 LN− and 151 LN + patients were enrolled in this study. 6 independent prediction models were developed to differentiate LN− from LN + patients using the selected features from clinico-biological-image dataset, radiomics dataset, and their combined CBR dataset, respectively. The DeLong test showed that the CBR Model containing all-scale features held the highest predictive efficiency and the lowest FPR among all of established models (p < 0.05) in both the training and test sets (AUCs of 0.90 and 0.89, FPRs of 12.82% and 6.45%, respectively) (p < 0.05). The quantitative nomogram based on CBR Model was validated to have a good consistency with actual observations.
Conclusion
This study presents an integrated CBR nomogram that can further reduce the FPR and improve the accuracy of hypermetabolic mediastinal–hilar LNs evaluation than conventional PET/CT in lung cancer, thereby greatly reducing the risk of overestimation and assisting for precision treatment.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Lobectomy with mediastinal systematic lymph node dissection (SND) is standard surgical strategy for lung cancer [1, 2]. Nevertheless, the significance of SND is controversial. The American College of Surgeons Oncology Group Z0030 trial revealed that there was no survival difference between patients with non-small cell lung cancer (NSCLC) who had SND or systematic sampling, with the 5-year disease-free survival rates were 68% and 69%, respectively (p > 0.05) [3]. Ishiguro et al. [4] and Ray et al. [5] also reported the similar findings: SND did not provide additional survival benefit. Central to avoid “overtreatment” (i.e., unnecessary SND) and provide a more precise and individualized lymph node (LN) dissection strategy is an accurate evaluation of node status at the mediastinal and hilar levels, especially the negative status [6].
The negative predictive value (NPV) of invasive endoscopic techniques is still unsatisfactory currently due to the difficulty of the selection suspected LN caused by the anatomical complexity of mediastinum, the location and size of LN, and the poor repeatability, etc. [7, 8]. Non-invasive imaging techniques, including chest computed tomography (CT) and [18F]-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT, are commonly used for LN staging [9]. PET/CT evidently has significantly higher accuracy than CT, especially with the superior NPV greater than 85% [10]. However, the main problem of PET/CT evaluation is the false-positive (FP) findings caused by non-specific FDG uptake in non-neoplastic processes such as granulomas or other inflammatory diseases, especially when intrapulmonary lesions and mediastinal–hilar LNs are both FDG-positive, with the false positive rate (FPR) of 19 ~ 22% [11, 12]. The resulting overestimation of FP LNs would have a major impact on the patient’s further treatment strategy, including unnecessary resection of benign nodules and inappropriate exclusion of surgical treatment. Thus, FP FDG studies for LN staging are inevitable.
Previous radiomics analyses based on PET/CT have demonstrated the great potential of assessing the lymph node metastasis (LNM) in lung cancer using the machine learning (ML) algorithms to exhaust the full underlying information of non-invasive medical images [13,14,15]. However, only a few radiomics researches have focused on the evaluation of hypermetabolic mediastinal–hilar LNs status [16]. The results in our previous study also indicated the feasibility of PET/CT radiomics in achieving “pathology-like” diagnosis non-invasively in lung cancer. Furthermore, we found that clinico-biological-radiomics (CBR) data could evaluate the tumor heterogeneity more comprehensively due to the combination of multi-scale characteristics of tumors [17]. Multi-scale and high-dimensional features need appropriate filter strategies to reduce redundancy while ensuring model effectiveness [18]. On the basis of successfully screening features and establishing excellent models using the least absolute shrinkage and selection operator (Lasso) algorithm in our previous study, we added the minimum-redundancy maximum-relevance (mRMR) algorithm before Lasso to initially narrow the range of redundant and irrelevant features in this study, which contributed to the robustness of research.
Thus, the purpose of this study was to seek a more reliable, scalable and non-invasive biomarker-based CBR data via ML algorithms to reduce the FPR and improve the accuracy for predicting the hypermetabolic mediastinal–hilar LNs status in lung cancer.
Methods
Patients
This retrospective study reviewed the charts of 1280 patients with single pulmonary nodule examined by [18F]FDG-PET/CT scanning less than 30 days before curative surgery between January 2018 and December 2022, and finally identified 260 patients of resectable T1–4 lung cancer with complete baseline clinico-biological information. The retrospective study was approved by the Ethics Committee of Shanghai Proton and Heavy Ion Center, and informed consent was waived.
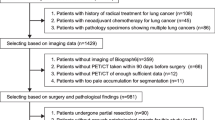
The specific inclusion criteria were as follows: (1) both the single intrapulmonary lesion and mediastinal–hilar LNs were FDG-positive with the maximum standardized uptake value (SUVmax) ≥ 2.5 [19, 20], the size of lesion > 1.0cm while the short axis diameter of target LNs > 0.5cm to ensure the quality of image and radiomics data; (2) first pathologically diagnosed of a primary lung cancer [21]; (3) postoperative pathological (p) N staging determined by SND as pN0-2 (N0: no regional LN involvement, N1: ipsilateral peribronchial, interlobar, or hilar LN involvement, N2: ipsilateral mediastinal LN involvement) [22]. The exclusion criteria included the following: (1) anti-tumor therapy before PET/CT examination or surgery; (2) lobectomy without SND; (3) distant metastasis; (4) poor image quality. The patient recruitment process is presented in Fig. 1.
Finally, totally 260 consecutive lung cancer patients were enrolled in this study, comprising 205 males and 55 females (mean age, 62.15 ± 8.62 years, range, 27–81 years), as summarized in Table 1. Among these included patients, the most common histologic subtype was adenocarcinoma (n = 145, 55.77%), followed by squamous cell carcinoma (n = 96, 36.92%). Rarer cases of small cell lung cancer (n = 11, 4.23%), large cell carcinoma (n = 6, 2.31%) and sarcomatoid carcinoma (n = 2, 0.77%) were reported. The patients were pathologically divided into the LN negative (LN−, pN0, n = 109) and positive (LN + , pN1-2, n = 151) groups, and assigned to a training (n = 182) and test (n = 78) sets by the random split-sample (7:3) method. Baseline clinico-biological data of each patient were reviewed and recorded.
[ 18 F]FDG-PET/CT image protocol
All included patients with a blood glucose levels < 8.7 mmol/L fasted for at least 6 h before the [18F]FDG-PET/CT scan. The scanning protocols of this retrospective study conducted in the single center were consistent with our previous study [17], and complied with the standard clinical scanning protocols [23]. The details of image acquisition process are given in Additional file 1 and “Methods” section.
Tumor segmentation and analysis
The target lesions in this study were hypermetabolic single primary tumor and mediastinal–hilar LNs. The volume of interest (VOI) of each primary tumor was segmented by two separated experienced nuclear medicine physicians on the PET images using the gradient-based semi-automatic contouring algorithm, named “PET_Edge”, on the Medical Image Merge software (MIM, version 6.5.4, https://www.mimsoftware.com) without knowing the pathology determined by consensus. PET_Edge has been confirmed to be the most accurate and consistent method for tumor segmentation than manual and constant threshold methods [24, 25]. Then, six metabolic parameters including minimum SUV (SUVmin), SUVmax, SUVmean, metabolic tumor volume (MTV), and total lesion glycolysis (TLG) were automatically measured from each VOI.
The highest SUVmax of LNs was also recorded for each patient, simultaneously, the size of the LN with the highest SUVmax was measured with the nodal enlargement criterion of greater than 1.0 cm in short axis diameter on a transverse CT image of the fused PET/CT [10].
Quantitative radiomics feature extraction
Subsequently, a total of 1702 quantitative radiomics features for each VOI were automatically extracted and calculated from the PET (n = 851) and CT (n = 851) images using the “PyRadiomics” module [26], respectively. The radiomic features were divided into four groups: (1) shape (n = 14); (2) intensity (n = 18); (3) texture (n = 75, 24 Gy level co-occurrence matrix (GLCM), 14 Gy level dependence matrix (GLDM), 16 Gy level run length matrix (GLRLM), 16 Gy level size zone matrix (GLSZM), and 5 neighboring gray tone difference matrix (NGTDM)); and (4) wavelet-based (W) features obtained from the filters (H: high pass filter, L: low pass filter) applied in the x, y, z directions (n = 744). The feature extraction and its definition were in accordance with the Imaging Biomarker Standardization Initiative [27], and its details are described in Additional file 1: Table S1.
Features dimension reduction and selection
So far, we have constructed a CBR dataset containing 1738 multi-scale features (25 clinico-biological features, 11 conventional image features, and 1702 radiomics features) for all included patients. The processes of features dimension reduction and selection were performed using the classical supervised ML algorithms in the training set. Firstly, the features with intra- and inter-class correlation coefficients (ICC) < 0.8 were excluded due to the poor consistency and reproducibility. Then, we performed the mRMR algorithm to preliminarily narrow the range of redundant and irrelevant features, and selected the top 50 features. Finally, the Lasso algorithm with tenfold cross-validation was applied to further screen the optimal features for prediction model development.
Prediction models and individualized nomogram development and evaluation
The models for predicting the hypermetabolic mediastinal–hilar LNs status in lung cancer were developed by the multivariable regression with the Akaike’s information criterion (AIC), with prediction scores (pre-scores) of each model calculated for each patient by the linear fusion of the selected non-zero features weighted by their coefficients. The performance and clinical utility of these models were evaluated and compared by the receiver-operator characteristic curve (ROC) analysis, DeLong test, and decision curve analysis (DCA) in both the training and test sets. The area under the curve (AUC) with 95% confidence interval (CI), sensitivity, specificity, accuracy, positive predictive value (PPV), negative predictive value (NPV), FPR, and false negative rate (FNR) were calculated for each model.
For models with similar overall AUC and accuracy, a lower FPR is more clinically relevant for this study. Thus, we developed an individualized nomogram to visually quantify the risk of hypermetabolic mediastinal–hilar LNs metastasis on the basis of prediction model corresponded to this rule. Calibration curves were plotted to assess the agreement between the actual probability and predicted probability of the nomogram by bootstrapping (1000 bootstrap resamples) in both the training and test sets.
Statistical analysis
All data analysis in this study was performed on the R software (version 4.2, http://www.r-project.org). The following packages “mRMRe”, “glmnet”, “pROC” and “rmda” were applied for mRMR, Lasso, ROC, and DCA analyses, respectively. The “rms” package was used to construct nomogram and calibration curves. Numerical data with normal distribution were expressed as mean ± standard deviation (SD) and compared using an independent t-test, while one with non-normal distribution was expressed as median (interquartile range) and compared using a Mann–Whitney U test. Categorical data were described as counts and their percentages, and compared using Fisher’s exact test or χ2 test. A two-sided p value < 0.05 was considered statistical significance. The study process was systematically evaluated using the radiomics quality score (RQS, range − 8 to + 36 points, https://www.radiomics.world/rqs) [28].
Results
The quality of this study was good with the RQS of 20 (55.56%) (Additional file 1), which was better than the average of PET/CT radiomics-based lung cancer researches, all of which scored below 50% [29].
Clinico-biological and conventional image characteristics of patients
In total, 260 lung cancer patients with both the hypermetabolic primary tumor and mediastinal–hilar LNs were eventually enrolled in this study, including 109 LN− and 151 LN + patients. The patients’ statistically significant clinico-biological-image (CBI) features in the training set are presented in Table 2, while the comparison results of a total of 36 CBI features between LN- and LN + patients in the total, training, and test sets are provided in Additional file 1: Table S2.
LN− patients were more likely to be elderly ones with lighter body weight, while LN + patients were more likely to be younger ones with higher body weight (p < 0.05). Simultaneously, LN + patients generally had higher level of carbohydrate antigen (CA) 153 and higher positive rate of carcinoembryonic antigen (CEA) (cut-off value: 5.2 ng/ml) than LN− patients (p < 0.05). The SUVmax and size of LN were significantly related to the LN status in both the training and test sets (p < 0.05). There were no significant differences in other clinical characteristics (such as gender and smoking status), biological factors (such as other conventional lung cancer tumor markers levels and status, and tumor histological types), and PET/CT image features (such as the size, location and all metabolic parameters of primary tumor) between the LN− and LN + patients according to the univariate analysis (p > 0.05).
Features selection and prediction models development
Two independent prediction models have been established based on the SUVmax and size of hypermetabolic mediastinal–hilar LNs, respectively. Their combination was considered as the diagnostic efficacy of PET/CT. The CBI Model was developed via 4 valuable clinical and biological features selected only using Lasso algorithm due to the low dimensionality of CBI sub-dataset with 34 features (n = 25 + 11–2) (Fig. 2a). Subsequently, 19 PET/CT radiomics features were selected from the radiomics sub-dataset (n = 1702) by the ICC rule, mRMR and Lasso algorithms sequentially in the training set (Fig. 2b), and then 10 radiomics features were confirmed by the multivariable regression with the AIC to establish the Radiomics (Rad) Model. Similarly, the CBR Model was built using the most valuable 7 clinical, biological, image, and radiomics features for predicting the hypermetabolic mediastinal–hilar LNs status in the training set (Fig. 2c). The Pre-scores of each model for each patient were calculated using the following formulas:
Features selection for prediction models using Lasso algorithm using tenfold cross-validation in the training set. The X-axis showed log (λ), and the Y-axis showed the model misclassification rate. The dotted vertical lines were drawn at the optimal values using the minimum criteria and the 1-se criteria, respectively. The 4, 19, and 7 features with non-zero coefficients were initially indicated for CBI Model (a), Rad Model (b), and CBR (c), respectively, according to the 1-se criteria
Pre-score (LN SUVmax) = − 2.79 + 0.57*LN SUVmax.
Pre-score (LN Enlarged) = − 0.62 + 1.84*LN Enlarged (Negative: 0, Positive: 1).
Pre-score (LN_PET/CT) = − 2.68 + 0.50* LN SUVmax + 0.56* LN Enlarged.
Pre-score (CBI Model) = 1.70–0.07*Age + 0.03*Weight (Kg) + 0.04*CA153 (U/mL) + 0.65*CEA status (Negative: 0, Positive: 1).
Pre-score (Rad Model) = − 381.80 + 4.71e−09*PET_WLLH_GLCM_Cluster Shade + 312.10*PET_WHLL_GLRLM_Short Run Emphasis + 5.31* PET_WHLH_GLDM_Large Dependence Low Gray Level Emphasis − 2.23e–10*PET_WHHL_GLCM_Cluster Prominence + 71.66*PET_WHHL_GLCM_Informational Measure of Correlation 2 (Imc2) − 4.26* CT_shape_Surface Volume Ratio (SVR) + 0.03*CT _first order_90 Percentile − 0.04*CT_GLDM_Large Dependence Low Gray Level Emphasis + 0.33*CT_WLHH_first order_Median − 3.00*CT_WHHL_GLCM_MCC.
Pre-score (CBR Model) = − 88.38 + 0.57*LN SUVmax + 0.57*LN Enlarged − 0.12*Age + 0.91*CEA status + 90.95*PET_WHHL_GLCM_Imc2 − 2.06* CT_ shape_SVR + 0.38*CT_WLLH_GLDM_Dependence Entropy.
LN + patients generally had higher Pre-scores in all prediction models than those in LN− patients (p < 0.05, Fig. 3).
Violin plot of 6 prediction models for LN− (blue) and LN + (red) patients in training set (a). The black line running up and down through the violin diagram represented the range from the smallest non-outlier value to the largest non-outlier value. The waterfall plot of the CBR Model was used to visualize the distribution of the Pre-scores of individual LN− and LN + patients (b)
Prediction models evaluation and comparison
The performance of these 6 prediction models to discriminate LN− from LN + is shown in Fig. 4a, b. All the prediction models were significantly associated with the hypermetabolic mediastinal–hilar LN status, while the DeLong test showed that the CBR Model, which consisted of 1 clinical factor, 1 biological marker, 2 conventional PET/CT image features, 1 PET and 2 CT radiomics parameters, presented the lowest FPR and optimal discrimination among these models in both the training set (FPR of 12.82%, AUC of 0.90, and accuracy of 84.07%) and test set (FPR of 6.45%, AUC of 0.89, and accuracy of 82.05%) (both p < 0.05) (Table 3).
Receiver-operating characteristic analysis of models for predicting LNs status in the training set (a) and (b), respectively. Decision curve analysis of prediction models in the training set (c). The X-axis represented the threshold probability that was where the expected benefit of treatment was equal to the expected benefit of avoiding treatment. The Y-axis represented the net benefit. The grey and black line represented the hypothesis that all lung cancer patients were LN + and LN−, respectively
Compared to the PET/CT, the CBR Model’s FPR decreased by 9.08%, while the AUC and accuracy separately increased by 8.43% and 11.69% in the training set. In the test set, the FPR of CBR Model was consistent with that of PET/CT, but its AUC and accuracy were significantly higher than PET/CT, with an increase of 17.11% and 16.37%, respectively.
The DCA also showed that the CBR Model was the most reliable clinical treatment tool for predicting the LN status in lung cancer when the threshold probability was greater than 18% (Fig. 4c).
Individualized nomogram development and evaluation
According to the above results, an individualized nomogram based on the CBR Model’s risk factors was successfully developed for the visualization. The nomogram’s score and probability threshold for predicting LNM were 0.19 and 0.55, respectively (Fig. 5a). The calibration curves demonstrated a good agreement between the prediction of the LNM probability by the nomogram and the actual observation in both the training and test sets (Fig. 5b, c). Then, physicians could perform a pretherapeutic individualized prediction of the LNM risk to develop more reasonable and effective treatment plans for patients (Fig. 6).
The nomogram was developed using the risk factors of CBR Model in the training set (a). The probability of each predictor could be converted into scores according to the first scale at the top of the nomogram. After adding up the corresponding prediction probability at the bottom of the nomogram was the risk of LNM. The nomogram’s score and probability threshold for predicting LNM were 0.19 and 0.55, respectively. Calibration curves showed the actual probability corresponded closely to the prediction of nomogram in training (b) and test (c) sets, respectively
Example of nomogram clinical use. The preoperative whole-body PET/CT of this 61-year-old female with negative CEA status indicated the primary tumor was located in the right upper lobe (purple circle), with hypermetabolic mediastinal–hilar LNs (red square and arrows), and without distant metastasis (a–c). After completing the radiomics process (b, c) and applying the nomogram (d), the LNM probability of this patient was 0.12 (< 0.55), indicating a low risk of LNM. The pathological result of lobectomy with SND confirmed the negative status of mediastinal–hilar LN (0/7). The nomogram could improve the accuracy of hypermetabolic mediastinal–hilar LNs evaluation in lung cancer
Discussion
In this study, we successfully explored a CBR nomogram incorporating multi-scale features, which held a more excellent performance in non-invasively N staging for lung cancer patients with hypermetabolic mediastinal–hilar LNs than conventional PET/CT, thereby greatly reducing the risk of overestimation and assisting for precision treatment.
Growing evidence suggests that radiomics integrated general CBI features achieve higher diagnostic efficacy than using them alone [30,31,32]. Thus, the clinico-biological factors of patients, PET/CT radiomics data of primary tumors, and image features of hypermetabolic mediastinal–hilar LNs were all applied to develop the prediction model in this study. Furthermore, on the basis of successfully screening features and establishing excellent models using a single ML algorithm (Lasso) in our previous study [17], we applied a combination of ML algorithms (mRMR + Lasso) to ensure the predictive performance of the model while minimizing the number of selected features to improve the model interpretability in the present study. The prediction performance of CBR Model with only 7 features established in this study was comparable to that of Combined Model with 14 features established in previous study. The result confirmed the feasibility of this approach.
Accurately identifying FP LNs is more challenging than assessing all LNs in lung cancer. To the best of our knowledge, only Ouyang et al. attempted a similar study using ML strategy [16]. They found that PET radiomics extracted from hypermetabolic mediastinal–hilar LNs integrated with CT image features could identify true and false positives of LNM in patients with non-small cell lung cancer with the highest AUC of 0.87. However, they mainly focused the role of LNs and did not concern the effect of the primary tumor. In this study, the CBR Model was developed using both the characteristics of the tumor and LNs, and validated to have more excellent potential in differentiating LN− (pN0) from LN + (pN1-2) patients in lung cancer (AUCs of 0.90 and 0.89 in the training and test sets, respectively). Moreover, the incorporating PET radiomics feature “WHHL_GLCM_Imc2” for characterizing tumor texture heterogeneity and CT radiomics feature “shape_SVR” for measuring tumor shape of CBR Model have also been selected in the Radiomics Model, indicating the robustness of these two features with high repeatability and reproducibility, which has also been confirmed in previous researches [33,34,35]. LN + patients generally had higher WHHL_GLCM_Imc2 and lower shape_SVR values than those in LN− patients (p < 0.05), suggesting that these two features were related to the tumor invasiveness, leading to a higher risk of LNM.
The accuracy of histologic staging of hypermetabolic LNs is also related to the clinico-biological-image factors. Patients’ age has been proven to be an independent risk factor, which means younger patients were more prone to having LNM, consistent with the positive status of pretherapeutic serum CEA [36]. Compared to conventional image tools, PET/CT is a significantly more accuracy non-invasive diagnostic procedure for LN staging in lung cancer, although it also has FP FDG-uptake in benign LNs [37]. Metastatic LNs generally have higher FDG uptake and bigger size than FP LNs (p < 0.05). However, it was difficult to achieve satisfactory prediction performance only using these conventional image parameters with the relatively higher AUC of 0.83. The efficiency of non-invasive LN prediction would increase by 8.43% in the case of CBR Model application. Simultaneously, the FPR of CBR Model for hypermetabolic mediastinal–hilar LNs evaluation was also outstanding with a decrease of 32.53 ~ 41.73% than previous clinical trials with the FPR of 19 ~ 22% [11, 12].
Furthermore, we generated an integrated nomogram on the basis of the CBR Model for facilitating its use in clinical practice. Then, the physicians could perform a preoperative individualized prediction of the LNM risk with this easy-to-use scoring tool, which could provide a non-invasive and accurate approach for patients who were unwilling or unable to undergo biopsy to develop more reasonable and effective treatment plans. The DCA also showed the nomogram added more benefit than either the treat-all-patients as LN− or the treat-all-patients as LN + , which was more valuable for the current trend toward personalized medicine [38, 39].
This study still has some limitations. Firstly, this retrospective study was conducted in a single center, which was the main cause of the decrease in RQS and also led to patient selection bias. It is necessary to design another prospective, multi-center, and large-cohort study to further validate the performance and generalization ability of the CBR Model in the real-world clinical settings [40]. Secondly, there is no significant statistical difference in primary tumor size, histologic type and metabolic parameters between LN− and LN + patients, consistent with the report [41]. This may be related to the weakened role of primary tumor in cases the included patients with both hypermetabolic tumor and LNs, equivalent to subgroup analysis. The sample size of patients, including ones with FDG-negative LNs, will be expanded to verify this hypothesis in further works. Thirdly, the radiomics analysis in this study only applied for primary tumor with semi-automatic segmentation, not LNs. This is due to the fact that larger tumors are more suitable for VOI segmentation that contribute to the robustness of study. The automatic segmentation approaches [42, 43] suitable for full volume VOI will be continually explored in future work.
In conclusion, an integrated CBR nomogram was successfully developed and validated in our study, which could further reduce the FPR and improve the accuracy of hypermetabolic mediastinal–hilar LNs evaluation in lung cancer than conventional PET/CT, thereby greatly reducing the risk of overestimation and assisting for precision treatment.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIC:
-
Akaike’s information criterion
- AUC:
-
Area under curve
- CA:
-
Carbohydrate antigen
- CBI:
-
Clinico-biological-image
- CBR:
-
Clinico-biological-radiomics
- CEA:
-
Carcinoembryonic antigen
- CI:
-
Confidence interval
- DCA:
-
Decision curve analysis
- FDG:
-
Fluorodeoxyglucose
- FNR:
-
False negative rate
- FP:
-
False-positive
- FPR:
-
False positive rate
- GLCM:
-
Gray level co-occurrence matrix
- GLDM:
-
Gray level dependence matrix
- GLRLM:
-
Gray level run length matrix
- GLSZM:
-
Gray level size zone matrix
- ICC:
-
Intra- and inter-class correlation coefficient
- Lasso:
-
Least absolute shrinkage and selection operator
- LN:
-
Lymph node
- LNM:
-
Lymph node metastasis
- ML:
-
Machine learning
- mRMR:
-
Minimum-redundancy maximum-relevance
- MTV:
-
Metabolic tumor volume
- NGTDM:
-
Neighboring gray tone difference matrix
- NPV:
-
Negative predictive value
- NSCLC:
-
Non-small cell lung cancer
- PET/CT:
-
Positron emission tomography/computed tomography
- PPV:
-
Positive predictive value
- Pre-score:
-
Prediction score
- Rad:
-
Radiomics
- ROC:
-
Receiver-operating characteristic
- RQS:
-
Radiomics quality score
- SD:
-
Standard deviation
- SND:
-
Systematic lymph node dissection
- SUV:
-
Standardized uptake value
- SVR:
-
Surface volume ratio
- TLG:
-
Total lesion glycolysis
- VOI:
-
Volume of interest
References
Watanabe S, Asamura H. Lymph node dissection for lung cancer significance, strategy, and technique. J Thorac Oncol. 2009;4(5):652–7. https://doi.org/10.1097/JTO.0b013e31819cce50.
Duma N, Santana-Davila R, Molina JR. Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc. 2019;94(8):1623–40. https://doi.org/10.1016/j.mayocp.2019.01.013.
Darling GE, Allen MS, Decker PA, Ballman K, Malthaner RA, Inculet RI, Jones DR, McKenna RJ, Landreneau RJ, Rusch VW, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg. 2011;141(3):662–70. https://doi.org/10.1016/j.jtcvs.2010.11.008.
Ishiguro F, Matsuo K, Fukui T, Mori S, Hatooka S, Mitsudomi T. Effect of selective lymph node dissection based on patterns of lobe-specific lymph node metastases on patient outcome in patients with resectable non-small cell lung cancer: a large-scale retrospective cohort study applying a propensity score. J Thorac Cardiovasc Surg. 2010;139(4):1001–6. https://doi.org/10.1016/j.jtcvs.2009.07.024.
Ray MA, Smeltzer MP, Faris NR, Osarogiagbon RU. Survival after mediastinal node dissection, systematic sampling, or neither for early stage NSCLC. J Thorac Oncol. 2020;15(10):1670–81. https://doi.org/10.1016/j.jtho.2020.06.009.
Zhang Y, Deng C, Zheng Q, Qian B, Ma J, Zhang C, Jin Y, Shen X, Zang Y, Guo Y, et al. Selective mediastinal lymph node dissection strategy for clinical T1N0 invasive lung cancer: a prospective, multicenter, clinical trial. J Thorac Oncol. 2023. https://doi.org/10.1016/j.jtho.2023.02.010.
Tournoy KG, De Ryck F, Vanwalleghem L, Praet M, Vermassen F, Van Maele G, van Meerbeeck JP. The yield of endoscopic ultrasound in lung cancer staging: does lymph node size matter? J Thorac Oncol. 2008;3(3):245–9. https://doi.org/10.1097/JTO.0b013e3181653cbb.
de Margerie-Mellon C, de Bazelaire C, de Kerviler E. Image-guided biopsy in primary lung cancer: why, when and how. Diagn Interv Imaging. 2016;97(10):965–72. https://doi.org/10.1016/j.diii.2016.06.016.
Osarogiagbon RU, Van Schil P, Giroux DJ, Lim E, Putora PM, Lievens Y, Cardillo G, Kim HK, Rocco G, Bille A, et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: overview of challenges and opportunities in revising the nodal classification of lung cancer. J Thorac Oncol. 2023;18(4):410–8. https://doi.org/10.1016/j.jtho.2022.12.009.
De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R, Turna A, Van Schil P, Venuta F, Waller D, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2014;45(5):787–98. https://doi.org/10.1093/ejcts/ezu028.
Gould MK, Kuschner WG, Rydzak CE, Maclean CC, Demas AN, Shigemitsu H, Chan JK, Owens DK. Test performance of positron emission tomography and computed tomography for mediastinal staging in patients with non-small-cell lung cancer—a meta-analysis. Ann Intern Med. 2003;139(11):879–92. https://doi.org/10.7326/0003-4819-139-11-200311180-00013.
Al-Sarraf N, Gately K, Lucey J, Wilson L, McGovern E, Young V. Lymph node staging by means of positron emission tomography is less accurate in non-small cell lung cancer patients with enlarged lymph nodes: analysis of 1145 lymph nodes. Lung Cancer. 2008;60(1):62–8. https://doi.org/10.1016/j.lungcan.2007.08.036.
Zheng K, Wang XR, Jiang CZ, Tang YX, Fang ZH, Hou JL, Zhu ZH, Hu S. Pre-operative prediction of mediastinal node metastasis using radiomics model based on F-18-FDG PET/CT of the primary tumor in non-small cell lung cancer patients. Front Med. 2021. https://doi.org/10.3389/fmed.2021.673876.
Dai M, Wang N, Zhao XM, Zhang JY, Zhang ZQ, Zhang JM, Wang JF, Hu YJ, Liu YN, Zhao XJ, et al. Value of presurgical F-18-FDG PET/CT radiomics for predicting mediastinal lymph node metastasis in patients with lung adenocarcinoma. Cancer Biotherapy Radiopharm. 2022. https://doi.org/10.1089/cbr.2022.0038.
Laros SSA, Dickerscheid DBM, Blazis SP, van der Heide JA. Machine learning classification of mediastinal lymph node metastasis in NSCLC: a multicentre study in a Western European patient population. Ejnmmi Physics. 2022. https://doi.org/10.1186/s40658-022-00494-8.
Ouyang ML, Wang YR, Deng QS, Zhu YF, Zhao ZH, Wang L, Wang LX, Tang K. Development and validation of a F-18-FDG PET-based radiomic model for evaluating hypermetabolic mediastinal-hilar lymph nodes in non-small-cell lung cancer. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.710909.
Ren C, Zhang J, Qi M, Zhang J, Zhang Y, Song S, Sun Y, Cheng J. Machine learning based on clinico-biological features integrated (18)F-FDG PET/CT radiomics for distinguishing squamous cell carcinoma from adenocarcinoma of lung. Eur J Nucl Med Mol Imaging. 2021;48(5):1538–49. https://doi.org/10.1007/s00259-020-05065-6.
Avanzo M, Wei L, Stancanello J, Vallières M, Rao A, Morin O, Mattonen SA, El Naqa I. Machine and deep learning methods for radiomics. Med Phys. 2020;47(5):e185–202. https://doi.org/10.1002/mp.13678.
Schmidt-Hansen M, Baldwin DR, Hasler E, Zamora J, Abraira V, Roqué IFM. PET-CT for assessing mediastinal lymph node involvement in patients with suspected resectable non-small cell lung cancer. Cochrane Database Syst Rev. 2014;2014(11): Cd009519. https://doi.org/10.1002/14651858.CD009519.pub2.
Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology. 2004;231(2):305–32. https://doi.org/10.1148/radiol.2312021185.
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, Chirieac LR, Dacic S, Duhig E, Flieder DB, et al. The 2015 World Health Organization Classification of lung tumors impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10(9):1243–60. https://doi.org/10.1097/JTO.0000000000000630.
Detterbeck FC, Nishimura KK, Cilento VJ, Giuliani M, Marino M, Osarogiagbon RU, Rami-Porta R, Rusch VW, Asamura H, Boards A. The International Association for the Study of Lung Cancer Staging Project: methods and guiding principles for the development of the ninth edition TNM classification. J Thorac Oncol. 2022;17(6):806–15. https://doi.org/10.1016/j.jtho.2022.02.008.
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W, Verzijlbergen FJ, Barrington SF, Pike LC, Weber WA, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42(2):328–54. https://doi.org/10.1007/s00259-014-2961-x.
Werner-Wasik M, Nelson AD, Choi W, Arai Y, Faulhaber PF, Kang P, Almeida FD, Xiao Y, Ohri N, Brockway KD, et al. What is the best way to contour lung tumors on PET scans? Multiobserver validation of a gradient-based method using a NSCLC digital PET phantom. Int J Radiat Oncol Biol Phys. 2012;82(3):1164–71. https://doi.org/10.1016/j.ijrobp.2010.12.055.
Sridhar P, Mercier G, Tan J, Truong MT, Daly B, Subramaniam RM. FDG PET metabolic tumor volume segmentation and pathologic volume of primary human solid tumors. AJR Am J Roentgenol. 2014;202(5):1114–9. https://doi.org/10.2214/ajr.13.11456.
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging. 2012;30(9):1323–41. https://doi.org/10.1016/j.mri.2012.05.001.
Zwanenburg A, Vallières M, Abdalah MA, Aerts H, Andrearczyk V, Apte A, Ashrafinia S, Bakas S, Beukinga RJ, Boellaard R, et al. The image biomarker standardization initiative: standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology. 2020;295(2):328–38. https://doi.org/10.1148/radiol.2020191145.
Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, Sanduleanu S, Larue R, Even AJG, Jochems A, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14(12):749–62. https://doi.org/10.1038/nrclinonc.2017.141.
Abdurixiti M, Nijiati M, Shen RF, Ya Q, Abuduxiku N, Nijiati M. Current progress and quality of radiomic studies for predicting EGFR mutation in patients with non-small cell lung cancer using PET/CT images: a systematic review. Br J Radiol. 2021. https://doi.org/10.1259/bjr.20201272.
Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol. 2018;15(2):81–94. https://doi.org/10.1038/nrclinonc.2017.166.
Lv WB, Yuan QY, Wang QS, Ma JH, Feng QJ, Chen WF, Rahmim A, Lu LJ. Radiomics analysis of PET and CT components of PET/CT imaging integrated with clinical parameters: application to prognosis for nasopharyngeal carcinoma. Mol Imaging Biol. 2019;21(5):954–64. https://doi.org/10.1007/s11307-018-01304-3.
Zwanenburg A. Radiomics in nuclear medicine: robustness, reproducibility, standardization, and how to avoid data analysis traps and replication crisis. Eur J Nucl Med Mol Imaging. 2019;46(13):2638–55. https://doi.org/10.1007/s00259-019-04391-8.
Scalco E, Belfatto A, Mastropietro A, Rancati T, Avuzzi B, Messina A, Valdagni R, Rizzo G. T2w-MRI signal normalization affects radiomics features reproducibility. Med Phys. 2020;47(4):1680–91. https://doi.org/10.1002/mp.14038.
Bernatowicz K, Grussu F, Ligero M, Garcia A, Delgado E, Perez-Lopez R. Robust imaging habitat computation using voxel-wise radiomics features. Sci Rep. 2021;11(1):20133. https://doi.org/10.1038/s41598-021-99701-2.
Merisaari H, Taimen P, Shiradkar R, Ettala O, Pesola M, Saunavaara J, Bostrom PJ, Madabhushi A, Aronen HJ, Jambor I. Repeatability of radiomics and machine learning for DWI: Short-term repeatability study of 112 patients with prostate cancer. Magn Reson Med. 2020;83(6):2293–309. https://doi.org/10.1002/mrm.28058.
Chen B, Wang XJ, Yu XN, Xia WJ, Zhao H, Li XF, Liu LX, Liu Y, Hu J, Fu XN, et al. Lymph node metastasis in Chinese patients with clinical T1 non-small cell lung cancer: a multicenter real-world observational study. Thorac Cancer. 2019;10(3):533–42. https://doi.org/10.1111/1759-7714.12970.
Maiga AW, Deppen SA, Mercaldo SF, Blume JD, Montgomery C, Vaszar LT, Williamson C, Isbell JM, Rickman OB, Pinkerman R, et al. Assessment of fluorodeoxyglucose F18-labeled positron emission tomography for diagnosis of high-risk lung nodules. JAMA Surg. 2018;153(4):329–34. https://doi.org/10.1001/jamasurg.2017.4495.
Rezaeijo SM, Hashemi B, Mofid B, Bakhshandeh M, Mahdavi A, Hashemi MS. The feasibility of a dose painting procedure to treat prostate cancer based on mpMR images and hierarchical clustering. Radiat Oncol. 2021;16(1):182. https://doi.org/10.1186/s13014-021-01906-2.
Salmanpour MR, Hosseinzadeh M, Rezaeijo SM, Rahmim A. Fusion-based tensor radiomics using reproducible features: application to survival prediction in head and neck cancer. Comput Methods Programs Biomed. 2023;240: 107714. https://doi.org/10.1016/j.cmpb.2023.107714.
Rogasch JMM, Michaels L, Baumgärtner GL, Frost N, Rückert JC, Neudecker J, Ochsenreither S, Gerhold M, Schmidt B, Schneider P, et al. A machine learning tool to improve prediction of mediastinal lymph node metastases in non-small cell lung cancer using routinely obtainable [(18)F]FDG-PET/CT parameters. Eur J Nucl Med Mol Imaging. 2023;50(7):2140–51. https://doi.org/10.1007/s00259-023-06145-z.
Endoh H, Yamamoto R, Ichikawa A, Shiozawa S, Nishizawa N, Satoh Y, Oriuchi N. Clinicopathologic significance of false-positive lymph node status on FDG-PET in lung cancer. Clin Lung Cancer. 2021;22(3):218–24. https://doi.org/10.1016/j.cllc.2020.05.002.
Heydarheydari S, Birgani MJT, Rezaeijo SM. Auto-segmentation of head and neck tumors in positron emission tomography images using non-local means and morphological frameworks. Pol J Radiol. 2023;88:e365–70. https://doi.org/10.5114/pjr.2023.130815.
Rezaeijo SM, Jafarpoor Nesheli S, Fatan Serj M, Tahmasebi Birgani MJ. Segmentation of the prostate, its zones, anterior fibromuscular stroma, and urethra on the MRIs and multimodality image fusion using U-Net model. Quant Imaging Med Surg. 2022;12(10):4786–804. https://doi.org/10.21037/qims-22-115.
Acknowledgements
All the authors have contributed significantly and have approved the manuscript.
Funding
This work was supported by Shanghai Sailing Program (Grant Number. 21YF1444300) and Natural Science Foundation of Shanghai (Grant Number. 21ZR1481800).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The research was designed by Jingyi Cheng and Yun Sun. Material preparation, data collection and analysis were performed by Caiyue Ren, Fuquan Zhang, and Jiangang Zhang. The first draft of the manuscript was written by Caiyue Ren and reviewed by Shaoli Song. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our Institutional Review Boards (Shanghai Proton and Heavy Ion Center and Fudan University Shanghai Cancer Center Medical Ethics Committees) approved this retrospective study and waived the need for informed consent from patients.
Consent for publication
All authors have read and approved the content and agree to submit for consideration for publication in the journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Specific categories of radiomics features. Table S2. Complete clinicopathologic and metabolic factors of lung cancer patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ren, C., Zhang, F., Zhang, J. et al. Clinico-biological-radiomics (CBR) based machine learning for improving the diagnostic accuracy of FDG-PET false-positive lymph nodes in lung cancer. Eur J Med Res 28, 554 (2023). https://doi.org/10.1186/s40001-023-01497-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01497-6