Abstract
Objectives
To evaluate the effects of two vitamin D repletion therapies (cholecalciferol) on serum levels of 25-hydroxyvitamin D (25(OH)D) and 24-h urine calcium in patients with recurrent calcium kidney stones and vitamin D deficiency (VDD).
Design, setting, participants
A parallel-group randomized controlled clinical trial on patients who referred to Labbafinejad kidney stone prevention clinic, Tehran, Iran. From 88 recurrent calcium stone formers, 62 patients completed the study. The age of participants was 18–70 years who had serum 25(OH)D levels of 10–20 ng/ml.
Intervention
Participants received oral cholecalciferol 2000 IU daily for 12 weeks or 50,000 IU weekly for 8 weeks.
Main outcome measures
Study variables including 24-h urine calcium, supersaturations of calcium oxalate and calcium phosphate, serum 25(OH)D and parathyroid hormone were measured at the beginning of the study and after 12 weeks.
Results
The 24-h urine calcium significantly increased in both groups (β = 69.70, p < 0.001), with no significant difference between treatments. Both groups showed no significant change in the supersaturation levels of calcium oxalate and calcium phosphate. Serum levels of 25(OH)D increased significantly (β = 12.53, p < 0.001), with more increase in the 50,000 IU group (β = 3.46, p = 0.003). Serum parathyroid hormone decreased in both groups (p < 0.001).
Conclusions
Although both treatment protocols increased 24-h urine calcium, they did not increase the supersaturation state of calcium oxalate or calcium phosphate.
Trial registration IRCT20160206026406N4, 13/08/2019.
Similar content being viewed by others
Introduction
Prevalence of vitamin D deficiency (VDD) in kidney stone formers is 18.9 to 59% [1]. In a case–control study by Ticinesi et al. (884 patients with idiopathic calcium stones vs. 967 non-stone-forming controls), the prevalence of VDD (< 20 ng/ml) was 56% in stone formers and 44% in control group (p < 0.001) [2]. In another case–control study on 239 calcium stone formers vs. 127 non-stone-forming controls [3], a VDD was observed in 28% of the patients versus 15.7% in controls (p = 0.009).
However, due to conflicting results of studies regarding association between serum 25(OH)D and hypercalciuria, there has been a concern for VDD treatment in calcium stone formers [4]. Furthermore, few studies evaluated the effect of VDD treatment on hypercalciuria in kidney stone formers [5,6,7,8,9,10]. These studies used different treatment protocols and found conflicting results; therefore, there is a lack of sufficient and robust evidence about the safety of VDD treatment in patients with kidney stones [11]. In the current study, we aimed to investigate the effects of two treatment protocols on serum levels of 25(OH)D and 24-h urine calcium (24-U Ca) in patients with recurrent calcium kidney stones and VDD.
Methods
Study design and participants
This study was a parallel-group randomized controlled clinical trial undertaken in the kidney stone prevention clinic of Shahid Labbafinejad medical center, from April 2018 to May 2020. The patients were recurrent calcium stone formers who had serum 25-hydroxyvitamin D (25(OH)D) level of 10–20 ng/mL, aged 18–70 years, had body mass index (BMI) of less than 30 kg/m2 [12], 24-U Ca below 300 mg [6], normal serum calcium levels who agreed to participate in the study. The recurrent calcium kidney stone was defined as having at least two episodes of radiopaque stones in the past medical history of the patient [13, 14]. The following cases were not included in our study: patients who were pregnant or lactating, using calcium supplements or other forms of vitamin D supplements or any medical drug which may affect serum or urinary calcium, had any history of kidney stone passage or gross hematuria within two months before the study, had known history of primary hyperparathyroidism or diseases that affect vitamin D and calcium metabolism (such as sarcoidosis or some other chronic granulomatous disorders), diabetes mellitus, and any malignancy or malabsorption. Patients who had 24-h urine volume under or over-collection [15] were also excluded from the study.
The study was approved by the ethics committee of the Urology and Nephrology Research Center, Shahid Beheshti University of Medical Sciences (IR. SBMU.UNRC.1395.26), and Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1397.193). The trial was registered in the Iranian Registry of Clinical Trials (IRCT) (IRCT20160206026406N4). All the study protocols were performed in accordance with the 1964 Declaration of Helsinki, and all participants gave written informed consent before the study.
Study interventions and outcomes
Study participants received either a daily dose of 2000 IU oral cholecalciferol for 12 weeks (maintenance dose) or a weekly dose of 50,000 IU oral cholecalciferol for eight weeks (loading dose). The final assessment was performed 12 weeks after the beginning of the study. These doses were selected according to loading treatment and maintenance therapy recommendations for VDD management, published by the endocrine society clinical practice guidelines [16]. In addition, all patients received general nutritional consultation for preventing kidney stone recurrence according to the European Association of Urology guidelines [17] with emphasis on taking adequate calcium from dairy products (800–1200 mg/day), salt intake restriction to less than 5 g/day, and consumption of moderate amounts of animal proteins (0.8–1 g/kg/day) [18,19,20].
Because of the differences in the study protocol, participants and researchers were not blind to the study protocol, and only the statistician was blinded for the statistical analyses.
Study variables included demographic, anthropometric, the duration and episodes of kidney stone disease, serum 25(OH)D, parathyroid hormone (PTH), calcium, and phosphate concentrations, 24-h urine analysis for volume and concentration of urea, creatinine, calcium, sodium, potassium, phosphate, magnesium, citrate, oxalate and uric acid, and also participant`s dietary intake data. Demographic, anthropometric, and kidney stone history data were collected at the beginning of the study. Serum and 24-h urine samples were taken at the beginning and the end of study. All the laboratory measurements were performed as we reported in our previous study [9]. The LithoRisk® software (Biohealth, Italy) was used to calculate relative supersaturations of calcium salts, i.e., calcium oxalate (CaOxSS) and calcium phosphate (CaPSS). Dietary intakes were assessed by two 24-h dietary recalls on non-consecutive days at the beginning, the sixth week of intervention, and the end of study. The recalls were analyzed using Nutritionist 4 software (N-Squared Computing), modified according to Iranian food composition.
Statistical methods
The sample size was calculated using the following equation:
Considering the type one error of 0.05, type 2 error of 0.20, and \(\begin{array}{*{20}c} {effect\begin{array}{*{20}c} {\,} \\ \end{array} \begin{array}{*{20}c} {size = \frac{\mu_1 - \mu_2 }{\sigma }} \\ \end{array} } \\ \end{array}\) of 0.75, the minimum required sample size was 28 in each group. Patients were randomized into study groups with an allocation ratio of 1:1 with a simple randomization method. A random sequence was generated using a computer program to produce the comparable groups and eliminate the source of bias in treatment assignments.
All the statistical analyses were performed using SPSS software version 24.0 (IBM, Chicago, Illinois, USA). Data are shown as mean ± standard deviation or median (IQR) for quantitative variables and frequency (percentage) for qualitative ones. The Kolmogorov–Smirnov test was used to assess the normality of data distribution. According to normality test results, the independent sample T-test or Mann–Whitney test was used to compare the mean outcome quantities between the two study groups. The Chi-Square test or Fisher exact test were also used to compare qualitative factors between the two groups. Serum variables, 24-h urine analysis, and supersaturation changes were compared between groups using a univariate general linear model (GLM) with generalized estimating equations (GEE) approach. Finally, multivariable GEE analysis was performed to assess the 24-h urinary calcium changes by adjusting confounding variables. Regression coefficient (β) were reported along with 95% confidence interval. The β (regression coefficient) signifies how much the mean of a dependent variable (for example the level of serum parathyroid hormone) changes when the participants received loading vitamin D repletion therapy (50,000 IU cholecalciferol/oral/weekly) compared with the maintenance vitamin D repletion protocol (2000 IU cholecalciferol/oral/daily). A p- value < 0.05 was considered statistically significant.
Results
Eighty-eight patients were randomized to study groups, with participation rate of 44%. Of them, 34 patients in the 50,000 IU group and 28 patients in the 2000 IU group completed the study (Fig. 1).
Baseline characteristics for 62 participants who completed the study are shown in Table 1. Duration of kidney stone history was significantly different between patients (p = 0.027). Other parameters had similar distribution between two groups (p > 0.05). The average amount of dietary intake showed no significant difference between groups in terms of energy, macronutrients and micronutrients including vitamin D and calcium (p > 0.05).
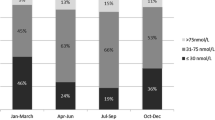
Table 2 represents the serum variables of both groups at the start and the end of the study. Both treatment protocols significantly increased serum 25(OH)D levels (p < 0.001). Comparing the changes in groups, increase in 50,000 IU group was more than 2000 IU group (β: 3.46, 95% CI 1.21, 5.70, p = 0.003). Considering normalization of serum vitamin D, serum 25(OH)D reached normal level (≥ 30 ng/mL [16]) in 55.9% of participants in 50,000 IU group and 25% of participants in 2000 IU group. Regarding other serum variables, PTH decreased (p < 0.001), and phosphate increased (p = 0.025) in both groups, with no significant difference between the two treatment protocols (p = 0.675, p = 0.345, respectively). In addition, we assessed the correlation between 24-U Ca alterations with serum 25(OH)D and PTH changes. There was no significant correlation between 24-U Ca and serum 25(OH)D level differences (r = 0.28, p = 0.15; r = 0.10, p = 0.56 in 2000 IU/daily and 50,000 IU/weekly, respectively). It is interesting that the correlation was higher in groups which received 2000 IU vitamin D per day. In addition, the correlation between 24-U Ca and serum PTH differences was not significant in both groups (r = − 0.14, p = 0.48; r = − 0.13, p = 0.47 in 2000 IU/daily and 50,000 IU/weekly, respectively).
The results of 24-U analysis and calculated supersaturations of participants are shown in Table 3. The 24-U Ca significantly increased in both groups during the time (β = 69.70, 95% CI 52.34, 87.06, p < 0.001), but we found no significant difference between two groups (p = 0.602). Three patients in the 2000 IU group (10.7%) and six patients in the 50,000 IU group (17.6%) had 24-U Ca more than 300 at the end of the study, which was not significantly different (p = 0.494). None of the study groups showed a significant change in CaOx SS and CaP SS (p > 0.05).
In addition to univariate analyses, a multivariate GEE model was used to adjust the effect of potential confounders in evaluation of the treatment protocols on urinary calcium (Table 4). Similar to univariate results, after adjusting confounding variables, the amount of 24-U Ca increased during the time in both groups (β = 44.01 95% CI 16.49, 71.54, p = 0.002), with no significant difference between two groups (p = 0.664).
Discussion
Although some guidelines, such as the Canadian Urology Association, recommend repletion therapy for kidney stone forming patients with VDD [21], there are still concerns about the best treatment protocol in these patients [7]. With this aim in view, our study evaluated the effects of two treatment protocols, i.e., loading and maintenance vitamin D repletion therapy, on 24-U Ca. The loading protocol in the current study was weekly dose of 50,000 IU oral cholecalciferol for 8 weeks, which is a standard therapy protocol for VDD. The maintenance protocol was daily dose of oral cholecalciferol 2000 IU for 12 weeks, recommended for people at higher risk for VDD. Since the groups did not have equivalent cumulative dosage (400,000 IU vs. 168000 IU), we did not expect similar serum 25(OH)D increase in study groups. Our results showed that serum 25(OH)D levels increased in both groups, with a higher increase in 50,000 IU group.
Vitamin D is crucial to improve the efficiency of calcium absorption in the gut. When VDD exists, calcium absorption declines. Consequently, the level of serum PTH increases (called secondary hyperparathyroidism) to maintain serum calcium through increasing renal tubular calcium reabsorption and bone resorption [16, 22]. The treatment of VDD leads to normalization of serum 25(OH)D and PTH. Consequently, an increase in intestinal calcium absorption and decrease in renal tubular calcium reabsorption occur. Therefore, an increase in urinary calcium is speculated after VDD treatment and PTH normalization [7]. The main concern about vitamin D repletion is the change in urinary calcium as a promoter of kidney stone formation.
The results of studies evaluating the effects of vitamin D supplementation on urinary calcium in urolithiasis patients are controversial (Table 5) [5,6,7,8,9,10]. Most of these studies had limitations, including non-controlled design of trials [6,7,8,9], retrospective design [9, 10], and small sample size [5]. Therefore, randomized controlled clinical trials with higher sample sizes are needed to clarify this conflict.
Our study results showed that both treatment protocols increased 24-U Ca by about 44 mg/24 h, with no difference between the two groups. Comparing with previous studies (Table 5), our finding is consistent with the results of Vitale et al. [7], Taheri et al. [9], and Hesswani et al. [10]. Conversely, it is against the result of Ganji et al. [8], Ferroni et al. [5], and Leaf et al. [6]. The reasons mentioned in these studies as the cause for increased urinary calcium include simultaneous calcium supplementation [10], the effect of confounding factors such as urinary sodium [9], and a significant decrease of PTH [6, 7]. Another reason may be the baseline 24-U Ca. As shown in Table 5, significant 24-U Ca levels are found in studies with a lower baseline 24-U Ca. This hypothesis needs further investigation.
The noteworthy finding of our study was similar urinary calcium increase for both repletion protocols, despite more serum 25(OH)D increase in the 50,000 IU group. Both univariate and multivariate analyses showed the same results. In the multivariate analysis, we tried to adjust most of the variables that could affect urinary calcium, including the increase in serum 25(OH)D levels. None of the confounding variables affected 24-U Ca. These results suggest that VDD treatment per se could increase urinary calcium, irrespective of amount of serum 25(OH)D increase. However, this finding should be investigated for treatment protocols that could increase serum 25(OH)D levels more than our study, which is usually in case of patients with severe VDD.
Another noteworthy finding of our study was a similar PTH decrease by both interventions, despite greater serum 25(OH)D increase in the 50,000 IU group. Different studies reveal the inverse correlation between serum 25(OH)D and PTH. Some studies showed that this correlation exists until serum 25(OH)D reaches the level of about 30 ng/mL, and after that, PTH levels begin to plateau [23, 24], however, other studies do not confirm the PTH plateaus at high 25(OH)D concentrations [25].
Studies show that in addition to altering urinary metabolites alone, another way to monitor the treatment of patients with renal stones is to assess the status of 24-h urine supersaturation. Supersaturation is shown to be an acceptable scale for measuring the risk of stone formation [26]. Despite 24-U Ca increase, our findings revealed no significant change in CaOx SS (B = 0.74, p = 0.052) and CaP SS (B = 0.26, p = 0.110). This finding is most likely due to significant increases in 24-h urine volume, magnesium, and citrate as a result of fluid and dietary consultation of patients. In contrary to our result, Vitale et al. [7] showed an increase in CaP SS state. Since 24-h urine volume, magnesium, and citrate are highly affected by dietary intake, controlling the dietary intake of patients could prevent a rise in the supersaturation and stone formation risk.
We evaluated the dietary intakes of our participants to consider their effect on urinary calcium. There was no significant difference in the average intake of micronutrients and macronutrients between the two groups. A noticeable finding was lower than normal calcium and dairy products intake in both groups, although we recommended patients to have a normal calcium intake. Dietary calcium intake could impact serum PTH, 25(OH)D [27] and 24-hour urine calcium. Furthermore, studies to evaluate the impact of different calcium intakes on urinary calcium changes after vitamin D repletion is warranted.
The current study is one of the few clinical trials that evaluated the effects of vitamin D repletion (cholecalciferol) in patients with calcium kidney stones. Another strength of our study was controlling variables that affect urinary calcium and response to vitamin D treatment, such as participants' dietary intake. The main limitation of the current study was lack of a placebo-controlled group which was because of ethical issues. Another limitation was inability of generalizing the results to other conditions, such as severe vitamin D deficiency and severe hypercalciuria, because of study inclusion criteria.
Conclusions
Although VDD treatment protocols increased 24-U calcium, they did not increase the risk of calcium stone formation assessed by supersaturation state of CaOx and CaP stone formation. Controlling the dietary intake of patients including adequate calcium from dairy products (800–1200 mg/day), salt intake restriction to less than 5 g/day, and consumption of a moderate amounts of animal proteins (0.8–1 g/kg/day) could prevent an increase in supersaturation after 24-U calcium rise due to VDD treatment. Further studies are needed to evaluate the effects of severe VDD treatment on 24-U calcium.
Availability of data and materials
The dataset supporting the conclusions of this article is available in the http://dregistry.sbmu.ac.ir.
Abbreviations
- 25(OH)D:
-
25-Hydroxyvitamin D
- VDD:
-
Vitamin D deficiency
- BMI:
-
Body Mass Index
- PTH:
-
Parathyroid hormone
- 24-U:
-
24-Hour urine
- CaOx SS:
-
Calcium oxalate supersaturation
- CaP SS:
-
Calcium phosphate supersaturation
References
Tavasoli S, Taheri F, Bagheri Amiri F, Borumandnia N, Basiri A, Parvin M, et al. The prevalence of vitamin D deficiency, its predisposing factors and association with 24-hour urine metabolites among iranian kidney stone formers. Iran J Kidney Dis. 2021;15:263–9.
Ticinesi A, Nouvenne A, Ferraro PM, Folesani G, Lauretani F, Allegri F, et al. Idiopathic calcium nephrolithiasis and hypovitaminosis D: a case-control study. Urology. 2016;87:40–5.
Girón-Prieto MS, Del Carmen C-G, Arrabal-Polo M, Poyatos-Andujar A, Quesada-Charneco M, de Haro-Muñoz T, et al. Analysis of vitamin D deficiency in calcium stone-forming patients. Int Urol Nephrol. 2016;48:1243–6.
Tang J, Chonchol MB. Vitamin D and kidney stone disease. Curr Opin Nephrol Hypertens. 2013;22:383–9.
Ferroni MC, Rycyna KJ, Averch TD, Semins MJ. Vitamin D repletion in kidney stone formers: a randomized controlled trial. J Urol. 2017;197:1079–83.
Leaf DE, Korets R, Taylor EN, Tang J, Asplin JR, Goldfarb DS, et al. Effect of vitamin D repletion on urinary calcium excretion among kidney stone formers. Clin J Am Soc Nephrol. 2012;7:829–34.
Vitale C, Marangella M, Bermond F, Fabbrini L, Tricerri A. Metabolic effects of cholecalciferol supplementation in patients with calcium nephrolithiasis and vitamin D deficiency. World J Urol. 2021;39:597–603.
Ganji MR, Shafii Z, Hakemi MS. Vitamin D supplementation and risk of hypercalciuria in stone formers. Iran J Kidney Dis. 2019;13:27–31.
Taheri M, Tavasoli S, Shokrzadeh F, Amiri FB, Basiri A. Effect of vitamin D supplementation on 24-hour urine calcium in patients with calcium Urolithiasis and vitamin D deficiency. Int Braz J Urol. 2019;45:340–6.
Hesswani C, Noureldin YA, Elkoushy MA, Andonian S. Combined vitamin D and calcium supplementation in vitamin D inadequate patients with urolithiasis: impact on hypercalciuria and de novo stone formation. Can Urol Assoc J. 2015;9:403–8.
Singh GV, Hampson G, Thomas K, Bultitude M, Willis S. Vitamin D and kidney stones—is there an association? BJU Int. 2019;123:751–2.
Sadat-Ali M, AlTabash KW, Al-Turki HA, AlMousa SA, AlSayed HN. Time out: should vitamin D dosing be based on patient’s body mass index (BMI): a prospective controlled study. J Nutr Sci. 2021;10:e106.
Goldfarb DS, MacDonald PA, Gunawardhana L, Chefo S, McLean L. Randomized controlled trial of febuxostat versus allopurinol or placebo in individuals with higher urinary uric acid excretion and calcium stones. Clin J Am Soc Nephrol. 2013;8:1960–7.
D’Costa MR, Pais VM, Rule AD. Leave no stone unturned: defining recurrence in kidney stone formers. Curr Opin Nephrol Hypertens. 2019;28:148–53.
Inker LA, Perrone RD. Assessment of kidney function. In: Post TW, editor. UpToDate. Waltham, MA: UpToDate; 2021;Number of.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30.
Türk C, Skolarikos A, Neisius A, Petrik A, Seitz C, Thomas K. EAU Guidelines on Urolithiasis: European Association of Urology; 2019 [cited 2019]. http://uroweb.org/guideline/urolithiasis/.
Borghi L, Schianchi T, Meschi T, Guerra A, Allegri F, Maggiore U, et al. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N Engl J Med. 2002;346:77–84.
Rotily M, Léonetti F, Iovanna C, Berthezene P, Dupuy P, Vazi A, et al. Effects of low animal protein or high-fiber diets on urine composition in calcium nephrolithiasis. Kidney Int. 2000;57:1115–23.
Martini LA, Cuppari L, Cunha MA, Schor N, Heilberg IP. Potassium and sodium intake and excretion in calcium stone forming patients. J Ren Nutr. 1998;8:127–31.
Dion M, Ankawi G, Chew B, Paterson R, Sultan N, Hoddinott P, et al. CUA guideline on the evaluation and medical management of the kidney stone patient—2016 update. Can Urol Assoc J. 2016;10:E347–58.
Inker LA, Perrone RD. Assessment of kidney function. UpToDate, Waltham, MA Accessed 2014;9.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81.
Holick MF. The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18:153–65.
Valcour A, Blocki F, Hawkins DM, Rao SD. Effects of age and serum 25-OH-vitamin D on serum parathyroid hormone levels. J Clin Endocrinol Metab. 2012;97:3989–95.
Prochaska M, Taylor E, Ferraro PM, Curhan G. Relative supersaturation of 24-hour urine and likelihood of kidney stones. J Urol. 2018;199:1262–6.
Mazahery H, von Hurst PR. Factors affecting 25-hydroxyvitamin D concentration in response to vitamin D supplementation. Nutrients. 2015;7:5111–42.
Acknowledgements
This article is taken from disease registry, titled “To evaluate and revision of registration system for recording stone formation risk factors in referring patients to Labbafinejad kidney stone prevention clinic” and project with code number IR.SBMU.UNRC.REC.1399.023 from ethic committee, that was supported by research and technology in Shahid Beheshti University of Medical Sciences (http://dregistry.sbmu.ac.ir).
Funding
This research received no funding.
Author information
Authors and Affiliations
Contributions
ST, MT contributed to the study conception and design. Data collection and writing the first draft of the manuscript was done by LSM. Conducting the trial and investigation process with main revision of the manuscript were performed by ST, MT. Application of statistical and mathematical or other formal techniques to analyze the study data was done by NB. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Urology and Nephrology Research Center, Shahid Beheshti University of Medical Sciences (IR. SBMU.UNRC.1395.26), and Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1397.193). The trial was registered in the Iranian Registry of Clinical Trials (IRCT) (IRCT20160206026406N4). All the study protocols were performed in accordance with the 1964 Declaration of Helsinki, and all participants gave written informed consent before the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sardari Masihi, L., Borumandnia, N., Taheri, M. et al. Effect of two vitamin D repletion protocols on 24-h urine calcium in patients with recurrent calcium kidney stones and vitamin D deficiency: a randomized clinical trial. Eur J Med Res 28, 246 (2023). https://doi.org/10.1186/s40001-023-01226-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01226-z