Abstract
Objectives
To compare the clinical and angiographic characteristics of high-risk and low-risk spontaneous coronary artery dissection (SCAD) patients to determine the optimal treatment strategy.
Background
SCAD is a rare and emerging cause of acute coronary syndrome and sudden cardiac death, especially in young female patients. However, the indication of percutaneous coronary intervention (PCI) in patients with SCAD remains elusive.
Methods
We evaluated the clinical and angiographic characteristics of all SCAD patients admitted to our center from 2012 to 2020. The outcomes of the high-risk and low-risk SCAD patients according to the location of the lesion segment with dissection or intramural hematoma were compared. Further analyses were performed to evaluate the vessel healing or residual dissection in the patients receiving the follow-up angiography.
Results
A total of 81 SCAD patients were enrolled in the present study, in which 38 patients were categorized as high-risk group, defined as involvement of the left main artery or proximal segment of any main coronary artery. PCI was the more common treatment approach in the high-risk group (68.4%), while conservative treatment was more common in the low-risk group (62.8%). The incidence of major adverse cardiac events, defined as cardiac death, myocardial infarction, unstable angina pectoris, severe arrhythmias, or heat failure, within 1 year follow-up was similar between the two groups. 57 patients (70.4%) received the follow-up angiography after 1 year. The high- and low-risk groups had a similar rate of vessel healing among the PCI treatment patients. However, more patients achieved spontaneous healing in the low-risk group than the high-risk group among the conservative treatment patients (86.4% vs. 33.3%, p < 0.05).
Conclusions
Conservative management remains the recommended treatment strategy for the low-risk SCAD patients. PCI could be considered in high-risk SCAD patients with favorable clinical outcomes and vessel healing. Characterization of lesion anatomy may be an important indicator for treatment decision.
Similar content being viewed by others
Introduction
Spontaneous coronary artery dissection (SCAD) has emerged as an important etiology of acute coronary syndrome (ACS) and sudden cardiac death, especially in the younger patient population, with female predominance [1]. Due to the rarity of the disease, SCAD is often underdiagnosed or misdiagnosed. The accurate definition of SCAD is an epicardial coronary artery dissection, with exclusion of atherosclerotic, iatrogenic, or traumatic causes. The main mechanism of SCAD is coronary artery obstruction caused by formation of an intramural hematoma (IMH) or intimal disruption rather than atherosclerotic plaque rupture or intraluminal thrombosis [2, 3]. However, the true etiology of SCAD may be multifactorial, including gender, hormone secretion, genetic predisposition, environmental, emotional triggers, or underlying vascular pathology, such as fibromuscular dysplasia [4, 5].
In view of the low diagnostic rate, the true prevalence of SCAD remains unclear. Unseasoned clinicians may be unfamiliar with the coronary angiographic (CAG) presentation of SCAD and can often be misdiagnosed as atherosclerosis-related dissection in patients with ACS. Aside from iatrogenic, traumatic and atherosclerotic dissection, about 1–4% of ACS are caused by SCAD [6, 7]. Recent studies have shown that the left anterior descending (LAD) artery is the most commonly affected coronary artery in SCAD, in which the middle and distal segments are the most common lesion site [8, 9].
In contrast to atherosclerotic ACS, the indication of percutaneous coronary intervention (PCI) in patients with SCAD remains elusive. Previous studies have shown that PCI in SCAD is associated with a higher risk of procedural complications, including iatrogenic dissection, acute vascular occlusion, hematoma extension or unplanned stents implantation. Therefore, the American Heart Association (AHA) and European Society of Cardiology (ESC) Statements on SCAD both recommend conservative management over PCI in most SCAD cases [10, 11]. However, in SCAD patients presenting with high-risk coronary anatomy or compelling clinical scenario, the revascularization strategy, including coronary artery bypass grafting (CABG) or PCI should be considered [11]. However, the definition of high-risk anatomical characteristics and the relevant treatment strategy remain debatable.
The present study retrospectively analyzed the clinical and angiographic data of SCAD patients to investigate whether specific high-risk anatomical clusters can be identified, which may help the individually tailored treatment strategies in patients who experienced SCAD.
Methods
Patient population
Patients with SCAD were recruited between 2012 and 2020 from the electronic medical database of Zhongshan Hospital. The patients diagnosed with coronary artery dissection through CAG were initially screened for eligibility. Patients with atherosclerotic, traumatic or iatrogenic dissection were collectively excluded. Angiographic and intravascular imaging data were reviewed by two independent, experienced interventional cardiologists to identify the anatomical characteristics of the affected vessel and segment. Any dispute or disagreements were settled with an open discussion. Eligible participants were contacted via e-mail or telephone and were asked to provide digital informed consent to examine their hospital records.
Angiographic findings
The culprit lesion was classified based on the Saw angiographic SCAD classification. Type 1 refers to classical appearance of multiple radiolucent lumens or arterial wall contrast staining, Type 2 refers to the presence of diffuse stenosis that can vary in severity and length, Type 3 presents as focal or tubular stenosis, that mimics atherosclerosis. Intracoronary imaging is helpful in confirming a true or false lumen and intramural hematoma, aiding with assessment of vessel dimensions [11]. The high- or low-risk SCAD were categorized by the location of the lesion segment with dissection or intramural hematoma. Involvement of the left main artery or proximal segment of any main coronary artery were considered as high-risk SCAD. Involvement of the side branch or the middle and distal segments of the main coronary artery were defined as low-risk SCAD. Other coronary imaging details, including initial thrombolysis in myocardial infarction (TIMI) flow grade, lesion length, percent of stenosis, and presence of atherosclerosis or thrombus, were also collected.
Treatment methods
The method and device for PCI, including stent implantation and/or balloon angioplasty, were recorded. The medical records of the patients received conservative treatment or CABG were also analyzed. All other evidence-based therapies recommended by the guidelines, including statin, beta-blockers, and antiplatelet therapy, were recorded during index hospitalization and follow-up.
Endpoints
Major adverse cardiac events (MACE) were defined as cardiac death, myocardial infarction, unstable angina pectoris, severe arrhythmias, or heat failure documented within 1 year follow-up. Further analyses were performed on patients who received follow-up CAG to evaluate vessel healing or residual dissection. The residual dissection in the patients receiving the stenting is defined as stent malposition, in-stent restenosis, stent thrombosis, persistent or extension intramural hematoma, or unplanned target vessel revascularization.
Statistical analysis
All statistical analyses were performed with SPSS 23 (IBM Corporation, USA). Categorical variables were presented as frequency (%), while continuous variables as mean ± standard deviation. Categorical variables were compared with Pearson’s correlation or the Chi-square test, while continuous variables were compared using the independent Student’s t test. A Kaplan–Meier analysis and log-rank test were used to display the incidence of MACE during 1 year follow-up. All statistical analyses were two-sided with a given p value of < 0.05 considered as statistically significant.
Results
Patient characteristics
A total of 531 coronary artery dissection patients were screened for inclusion, and 450 patients were subsequently excluded after careful review of the medical history and coronary angiographic or intravascular imaging data. A total of 81 patients diagnosed with SCAD were included in the present study (Fig. 1). Over half of the patients (67.9%) were female, with an average age of 56.8y. Few of the patients have traditional coronary risk factors. However, 95.1% of the patients presented as ACS upon admission, in which ST-elevation myocardial infarction (STEMI) was 23.5%. Only 4.9% of the patients presented as stable angina (SA). Detailed baseline characteristics are summarized in Table 1.
Angiographic and procedural characteristics
According to the Saw angiographic SCAD classification, the percentage of type 1, 2 and 3 were 58.0%, 37.1% and 4.9%, respectively. Majority of SCAD were found in right coronary artery (RCA, 55.6%), followed by LAD (32.1%), left circumflex (LCX, 9.9%) and left main (LM, 2.5%) artery. Affected segment was determined via CAG examination and divided into proximal (46.9%), middle (37.0%) and distal (16.1%). Involvement of the LM or proximal segment of any main coronary artery were found in approximately half of the patients (46.9%), which was classified as high-risk SCAD group. Most of patients (81.5%) had the initial TIMI grade 3 flow. About half of the patients (49.4%) patients received PCI and 44.4% of the patients were managed conservatively. The incidence of MACE after 1 year follow-up was 12.3%. Figure 2 shows the representative cases of SCAD receiving PCI or conservative management.
Coronary angiography in patients with SCAD. A SCAD patients presenting with high-risk coronary anatomy (proximal RCA). B Implantation of drug-eluting stent. C Repeat angiography after initial PCI. D SCAD patients presenting with low-risk coronary anatomy (middle-distal RCA). E Repeat angiography 12 month after conservative treatment. F OCT images visualized the true lumen and the false lumen of SCAD. The white arrows indicate SCAD in RCA. SCAD spontaneous coronary artery dissection, RCA right coronary artery, PCI percutaneous coronary intervention, OCT optical coherence tomography
The high-risk and low-risk SCAD
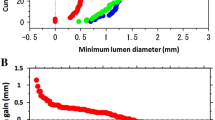
No significant differences were observed between the baseline clinical characteristics of the high-risk and low-risk SCAD groups (Table 1). High-risk group had a higher rate of RCA involvement than the low-risk group (68.4% vs. 44.2%, p < 0.05), while the culprit vessel in the low-risk group was more frequently located in LAD and LCX (39.5% vs. 23.7% and 16.3% vs. 2.6%) (p < 0.05). The length of the dissection was shorter in the high-risk group than the low-risk group (34.1 vs. 45.5 mm, p < 0.05). More patients in the high-risk group received PCI (68.4% vs. 32.5%, p < 0.01), while most patients in the low-risk SCAD group received conservative management (62.8% vs. 23.7%, p < 0.01) (Table 1). However, the incidence of MACE after 1 year follow-up was comparable between the two groups (Fig. 3).
Incidence of MACE for patients with high-risk SCAD (green line) versus low-risk SCAD (blue line). Abbreviations as in Fig. 2
Among 40 patients who received PCI, 26 patients were categorized as high-risk group (Table 2). Cardiac troponin T (cTnT) level was higher and more stents were placed in the low-risk group (0.38 vs. 0.03 ng/ml, 2.55 vs. 1.58, p < 0.05, Table 2). Among 36 patients with conservative management, 9 patients were categorized as high-risk group (Table 3). The levels of cTnT and creatine kinase MB isoenzyme (CK-MB) were higher in the high-risk group (0.52 vs. 0.12 ng/ml, 33 vs. 16 U/L, p < 0.05, Table 3). Involvement of the LAD was more common in the low-risk group (51.9% vs. 22.2%, p < 0.05), while involvement of RCA was more common in the high-risk group (77.7% vs. 29.6%, p < 0.05, Table 3).
Vessel healing analysis
Repeat CAG were performed in 57 patients (70.4%), in which 29 patients received PCI and 28 patients received conservative treatment (Table 4). Among the PCI treatment patients, the high- and low-risk groups had a similar rate of vessel healing. However, more patients achieved spontaneous vessel healing in the low-risk group than the high-risk group among the conservative treatment patients (86.4% vs. 33.3%, p < 0.05). It means that a higher rate of residual dissection was observed in the high-risk group than the low-risk group among the conservative treatment patients (66.7% vs. 13.6%, p < 0.01, Table 4).
Discussion
The present study is the first to compare the clinical characteristics and treatment efficacy of high-risk and low-risk SCAD based on lesion anatomy. High-risk SCAD is defined as dissection involving the LM and the proximal segment of any main coronary artery with a slight modification from previous definition [11]. Conservative management remains the recommended treatment strategy for the low-risk SCAD patients with a high rate of spontaneous vessel healing. PCI in the high-risk SCAD patients could achieve the favorable clinical outcomes and relatively similar vessel healing with the conservative treatment.
Although SCAD belongs to the broad spectrum of coronary heart disease, its treatment strategy is different from traditional CAD [2, 3]. Based on current recommendations, most of the clinically stable patients should consider the conservative management. Only those with ongoing ischemia or hemodynamic instability should consider urgent PCI or CABG [11]. However, emergency CABG is only feasible in certain medical facilities, while emergency PCI has a more widespread coverage. About 5–10% of patients who receive conservative treatment experience early recurrence of MI, which is often related to extension of dissection within the first 7 days after an acute ACS episode [12]. Previous study [13] showed that most SCAD patients undergoing PCI were high risk at presentation, including STEMI, cardiac arrest, TIMI 0/1 flow or proximal dissections. Conservative management in these patients may not be appropriate and can incur greater risks. Several studies have proven the value of PCI in SCAD, especially in high-risk coronary lesions, with promising outcome. Patients with STEMI–SCAD had more favorable prognoses in revascularization management modalities than those who with atherosclerosis-related STEMI [13,14,15,16]. In the present study, the high-risk and low-risk patients had the similar clinical characteristics, including ACS presentation and female predominance. The incidence of 1 year MACE was comparable between the two groups. Due to the retrospective nature of the present study, the appropriate treatment method was determined by the operator. Interestingly, PCI was employed in majority of the high-risk cases, while most of the low-risk cases received conservative management. High-risk patients in the present study underwent PCI treatment for SCAD with low complication rates and similar outcome with the low-risk patients. Several important technical factors, including careful manipulation of guiding catheter and wire, direct stenting without balloon predilation, long stents to cover the proximal and distal ends of the hematoma by 5–10 mm, and guidance with intravascular ultrasound (IVUS), could limit the hematoma propagation-related complications during PCI management of SCAD.
A small portion of the low-risk SCAD patients received PCI in the present study. In SCAD patients who received PCI, cTnT (ng/ml) values were higher in the low-risk group than the high-risk group, which was associated with a higher rate of baseline TIMI 0/1 flow and urgent decision of PCI. This may be associated with a more severe clinical feature, which prompted the clinical decision of PCI. In comparison with the conservative treatment group, cTnT (ng/ml) and CK-MB (U/L) values were higher in the high-risk group (n = 9). Regardless, all 9 patients had a TIMI 3 flow and, therefore, received conservative management and close follow-up. Previous studies have indicated angiographic “healing” of SCAD lesions is plausible in majority of patients after a conservatively managed index episode [8, 9]. According to the follow-up CAG results in our study, majority of the patients in the high-risk group receiving PCI achieved vessel healing. Conservative management was also associated with a significantly higher rate of spontaneous vessel healing in low-risk patients. Therefore, we propose that conservative management is the acceptable treatment approach but should be carefully selected for patients with low-risk SCAD anatomy and stable clinical features. In patients presenting with high-risk SCAD anatomy or compelling clinical scenario, emergency revascularization can be achieved with PCI.
Compared with low-risk lesions, patients with proximal lesions cover a larger myocardial blood supply area. Recent study suggested SCAD involving the proximal coronary arteries was associated with a reduction in post-infarct ejection fraction [17]. This may be associated with a more severe clinical feature, which prompted the clinical decision of PCI. In the present study, no significant difference in Saw classification was noted between high-risk and low-risk groups. Although Saw classification has a high diagnostic value, it cannot provide the reference for treatment decisions in patients with SCAD [18,19,20,21].
There are several limitations in the present study. First, this present study summarizes the experience of a single center, with a rather small sample size. Second, the retrospective nature of the study may incur selection bias especially in treatment methods. Third, this study lacks long-term follow-up data for SCAD patients with different interventions. Future prospective randomized control trial including multi-center data is warranted to validate the present study results.
The present study proposed a new classification method based on lesion segment and anatomical characteristics of SCAD, providing a simple and convenient alternative for interventional cardiologists to quickly formulate a suitable treatment strategy for patients in emergency situations. PCI may be chosen in patients with SCAD involvement of the LM or proximal segment of any main coronary artery. While conservative treatment should be reserved for low-risk SCAD patients with the involvement of the side branch or the middle and distal segments of the main coronary artery.
Conclusion
This study provides insight to the treatment strategy of SCAD patient based on lesion anatomy and affected segment. Conservative management remains the recommended treatment strategy for the low-risk SCAD patients. PCI could be considered in high-risk SCAD patients with favorable clinical outcomes and vessel healing.
Availability of data and materials
Original data could be made available by formal acquisition to the corresponding author.
Abbreviations
- SCAD:
-
Spontaneous coronary artery dissection
- PCI:
-
Percutaneous coronary intervention
- MACE:
-
Major adverse cardiac events
- ACS:
-
Acute coronary syndrome
- IMH:
-
Intramural hematoma
- CAG:
-
Coronary angiography
- TIMI:
-
Initial thrombolysis in myocardial infarction
- LAD:
-
Left anterior descending artery
- LCX:
-
Left circumflex artery
- RCA:
-
Right coronary artery
- LM:
-
Left main artery
- CABG:
-
Coronary artery bypass grafting
- STEMI:
-
ST segment elevation myocardial infarction
- IVUS:
-
Intravascular ultrasound
- cTnT:
-
Cardiac troponin T
- CK-MB:
-
Creatine kinase MB isoenzyme
References
Saw J, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7(5):645–55.
Hayes SN, et al. Spontaneous coronary artery dissection: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76(8):961–84.
Kim ESH. Spontaneous coronary-artery dissection. N Engl J Med. 2020;383(24):2358–70.
Kok SN, et al. Prevalence and clinical factors of migraine in patients with spontaneous coronary artery dissection. J Am Heart Assoc. 2018;7(24):e010140.
Saw J, et al. Canadian spontaneous coronary artery dissection cohort study: in-hospital and 30 day outcomes. Eur Heart J. 2019;40(15):1188–97.
Nishiguchi T, et al. Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care. 2016;5(3):263–70.
Tweet MS, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126(5):579–88.
Rashid HN, et al. Incidence and characterisation of spontaneous coronary artery dissection as a cause of acute coronary syndrome–a single-centre Australian experience. Int J Cardiol. 2016;202:336–8.
Rogowski S, et al. Spontaneous coronary artery dissection: angiographic follow-up and long-term clinical outcome in a predominantly medically treated population. Catheter Cardiovasc Interv. 2017;89(1):59–68.
Adlam D, et al. European society of cardiology, acute cardiovascular care association, SCAD study group: a position paper on spontaneous coronary artery dissection. Eur Heart J. 2018;39(36):3353–68.
Hayes SN, et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American heart association. Circulation. 2018;137(19):e523–57.
Tweet MS, et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7(6):777–86.
Lobo AS, et al. Revascularization in patients with spontaneous coronary artery dissection and ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2019;74(10):1290–300.
Almasi A, et al. Clinical features and prognoses of middle-aged women with ST-elevation myocardial infarction with a focus on spontaneous coronary artery dissection. Crit Pathw Cardiol. 2022;21(1):18–23.
Kotecha D, et al. Risks and benefits of percutaneous coronary intervention in spontaneous coronary artery dissection. Heart. 2021;107(17):1398–406.
Liu X, et al. Clinical characteristics and long-term prognosis of spontaneous coronary artery dissection: a single-center Chinese experience. Pak J Med Sci. 2019;35(1):106–12.
Faden MS, et al. A nationwide evaluation of spontaneous coronary artery dissection in pregnancy and the puerperium. Heart. 2016;102(24):1974–9.
Jackson R, et al. Spontaneous coronary artery dissection: pathophysiological insights from optical coherence tomography. JACC Cardiovasc Imaging. 2019;12(12):2475–88.
Mahmood MM, Austin D. IVUS and OCT guided primary percutaneous coronary intervention for spontaneous coronary artery dissection with bioresorbable vascular scaffolds. Cardiovasc Revasc Med. 2017;18(1):53–7.
Motreff P, et al. How and when to suspect spontaneous coronary artery dissection: novel insights from a single-centre series on prevalence and angiographic appearance. EuroIntervention. 2017;12(18):e2236–43.
Paulo M, et al. Combined use of OCT and IVUS in spontaneous coronary artery dissection. JACC Cardiovasc Imaging. 2013;6(7):830–2.
Acknowledgements
The authors thank all the non-author operators of the cardiology department and the members of the cardiac interventional center.
Funding
This project was supported by the Natural Science Foundation of Shanghai, Grant 21ZR1412700 and The Shanghai Clinical Research Center for Interventional Medicine, Grant 19MC1910300.
Author information
Authors and Affiliations
Contributions
Ma Y, Zhong X and Yin J conducted all statistical analyses and contributed to conception, writing sections of the manuscript. Lu H and Pan C contributed to design figures and tables. Huang D and Ge J contributed to design and final approval of the manuscript submitted. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Zhongshan Hospital’s medical ethics committee (No. B2022-246). Eligible participants were contacted via e-mail or telephone and were asked to provide digital informed consent to examine their hospital records.
Consent for publication
All authors have reviewed the manuscript and approved for publication.
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, Y., Zhong, X., Yin, J. et al. Treatment strategy for spontaneous coronary artery dissection based on anatomical characteristics. Eur J Med Res 28, 29 (2023). https://doi.org/10.1186/s40001-023-00986-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-00986-y