Abstract
Background
Patients with coronavirus disease 2019 (COVID-19) who undergo surgery have impaired postoperative outcomes and increased mortality. Consequently, elective and semi-urgent operations on the increasing number of patients severely affected by COVID-19 have been indefinitely postponed.in many countries with unclear implications on disease progression and overall survival. The purpose of this study was to evaluate whether the establishment of a standardized screening program for acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is sufficient to ensure high-quality medical and surgical treatment of COVID-19 and non-COVID-19 patients while minimizing in-hospital SARS-CoV-2 transmission.
Methods
The screening program comprised polymerase chain reaction (PCR) testing of nasopharyngeal swabs and a standardized questionnaire about potential symptoms for SARS-CoV-2 infection. All elective and emergency patients admitted to the surgical department of a tertiary-care hospital center in Lower Franconia, Germany, between March and May 2020 were included and their characteristics were recorded.
Results
Out of the study population (n = 657), 509 patients (77.5%) had at least one risk factor for a potentially severe course of COVID-19 and 164 patients (25%) were active smokers. The average 7-day incidence in Lower Franconia was 24.0/100,000 during the observation period. Preoperative PCR testing revealed four asymptomatic positive patients out of the 657 tested patients. No postoperative SARS-CoV-2 infection or transmission could be detected.
Conclusion
The implementation of a standardized preoperative screening program to both COVID-19 and non-COVID-19 patients can ensure high-quality surgical care while minimizing infection risk for healthcare workers and potential in-hospital transmission.
Similar content being viewed by others
Introduction
In response to the COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), many surgical departments have had to indefinitely postpone semi-urgent and elective operations to accommodate the rising number of severely affected patients [1, 2]. This has in turn heightened the risk of in-house SARS-CoV-2 transmission between patients and surgical staff [3,4,5,6,7]. Further, patients with perioperative SARS-CoV-2 infection have increased mortality [8,9,10]. Since the middle- to long-term consequences of postponing surgery in non-COVID-19 patients are presently unclear, specific containment and testing strategies are mandatory to ensure universally high-quality medical and surgical treatment while minimizing the risk of in-hospital-acquired infections [1, 11].
Presented with this problem, we introduced a number of precautionary measures including standardized preoperative SARS-CoV-2 testing, establishment of COVID-19 and non-COVID-19 areas (intensive care units, non-intensive care units, emergency rooms and operation rooms) and prioritization of operational interventions based on medical urgency and logistical resources (intensive care unit capacity for COVID-19 and non-COVID-19 patients, personnel and material capacities) [1]. The aim of this study was to show that by implementing these precautionary measures, emergency and elective surgeries are both feasible at a tertiary-care hospital center (university hospital) during the COVID-19 pandemic without increasing the risk for nosocomial transmission of SARS-CoV-2.
Methods
Study population
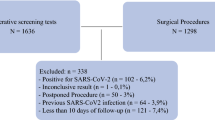
Patients admitted to the Department of Surgery I at the University Hospital Wuerzburg between March 26th and May 24th, 2020, had to answer a standardized COVID-19 questionnaire and were tested for SARS-CoV-2 infection by real-time reverse transcriptase polymerase chain reaction (RT-PCR) [12]. The standardized questionnaire enquired about clinical symptoms that are characteristic of symptomatic SARS-CoV-2 infection including coughing, shortness of breath, rhinorrhea, loss of smell and taste, sore throat, fever or diarrhea [13] as well as any potential contact the patient had with suspected or confirmed COVID-19 patients (Fig. 1). A nasopharyngeal swab for RT-PCR testing [14] was performed at our outpatient clinic by specially trained nursing staff within 48 h of elective surgery. In case of emergency, the questionnaire and PCR testing were conducted immediately prior to the operation. In such cases, anesthesia was performed by using personal protection equipment as generally recommended [1, 15]. Based on the outcome of the questionnaire, operations were performed in COVID-19 or non-COVID-19 operation areas.
Demographic variables included age, sex, body mass index (BMI), immunosuppression, and cardio-pulmonary risk factors. Operative variables included urgency of surgery, diagnosis, and surgical procedure. In parallel, the incidence of COVID-19 patients in the district of Lower Franconia was registered on a daily basis [16].
Statistical analysis
Descriptive data are presented as median with range, mean with standard deviation (SD) or total numbers with percentage. Statistical analysis was performed using SPSS statistics (Version 25, IBM, Armonk, NY, USA).
Results
During the observation period, 657 patients were admitted to our department with an average age of 59.93 ± 17.92 years and BMI of 26.82 ± 5.39 kg/m2, of whom 101 patients underwent emergency surgery and 61 patients received urgent non-surgical treatment. One hundred and sixty-six patients were treated due to a cancer-related problem (Table 1). Almost 12% of patients (n = 78) had a medical history of pulmonary disease including bronchial asthma and chronic obstructive pulmonary disease (COPD), 25% (n = 164) were active smokers and more than three-quarters (77.5%, n = 509) had at least one risk factor for a potentially severe course of COVID-19 [17]. Operative procedures are listed in detail in Table 2, and were performed either using an open, laparoscopic or robotic-assisted approach. Vascular surgery included open and endovascular procedures.
The average 7-day incidence in Lower Franconia (1,317,000 residents) was 24.0/100,000 during the observation period [16]. Standardized RT-PCR testing of admitted patients revealed 4 SARS-CoV-2 positive cases—all of whom were asymptomatic. Treatment was delayed in one of these four patients. The other three patients were isolated and treated in dedicated COVID-19 areas (Fig. 2).
During the observation period, an average of 22 patients were hospitalized due to SARS-CoV-2 infection with a maximum of 22 patients in an ICU ward and 16 patients in a non-ICU ward on April 17th. Postoperative viral transmission and SARS-CoV-2 infection, respectively, were not detected and, thus, no COVID-19-related mortality occurred.
Discussion
Recently published studies showing higher mortality rates after surgery in COVID-19 patients have concluded that the threshold for surgery during the COVID-19 pandemic should be higher [8,9,10]. This has had the implication that surgical procedures should be postponed and that non-operative therapies are promoted instead [8,9,10]. However, closer inspection of the data reveals that only 280 of the 1128 patients included in the study by D. Nepogodiev et al. [8] had an elective operation, of whom 250 had postoperative SARS-CoV-2 infection. Thus, in-hospital transmission of SARS-CoV-2 might be possible, since these data were collected during the beginning of the pandemic when health care systems were overwhelmed and there was a lack of sufficient personal protective equipment and test capacities. Given that asymptomatic undetected SARS-CoV-2-positive patients are a potential source of nosocomial transmission, effective screening and containment measures are mandatory to minimize the risk of in-hospital transmission of SARS-CoV-2. Our data show that under COVID-19 pandemic conditions, use of a standardized questionnaire and systematic RT-PCR testing are highly effective tools to identify preoperatively asymptomatic SARS-CoV-2 patients, and thus safely enable elective surgery. While our findings are supported by other studies [18,19,20], an international survey has shown that standardized screening programs are not yet established in surgical practice [21]. In our test strategy, we excluded the routine computed tomography (CT) of the chest, since its value has been questioned [20, 22], and may thus introduce unnecessary exposure to radiation.
It is well known that cardiovascular comorbidities and cancer are risk factors for a severe disease course of COVID-19 [17]. However, as shown by our analysis and other studies, the introduction of standardized screening programs and the establishment of dedicated COVID-19-free surgical pathways enable elective surgery in these high-risk patients during the COVID-19 pandemic without increasing the risk of postoperative SARS-CoV-2 infection and mortality [23,24,25].
Our study has some limitations including its retrospective character and the single-center design. However, as a tertiary-care hospital center we were faced with the challenge of rapidly providing medical and surgical services to COVID-19 and non-COVID-19 patients at the same time. Thus, our data offer an important example of “real life” experiences in a rural area (Lower Franconia).
During the COVID-19 pandemic, a cost–benefit analysis for performing elective surgery is necessary to provide sufficient medical, personal and material resources for COVID-19 patients. While it is clear that elective operations in SARS-CoV-2-positive patients should be cancelled or postponed, their delay in non-COVID-19 patients suffering from cancer and other serious conditions can lead to disease progression and impact overall survival. Therefore, instead of recommending unconditional postponement of all “elective” operations, the establishment of COVID-19-free surgical pathways and standardized preoperative SARS-CoV-2 testing can ensure that universally high-quality medical and surgical treatment while minimizing the risk of in-hospital-acquired infections.
Conclusion
Despite initial studies recommending the postponement of elective surgeries during the COVID-19 pandemic and that non-surgical treatments should be considered for emergency cases, we show that the implementation of a standardized preoperative screening program ensures high-quality surgery for both COVID-19 and non-COVID-19 patients while minimizing infection risk for healthcare workers and potential in-hospital transmission.
Availability of data and materials
Institutional database. Therefore, restrictions to availability apply due to data protection regulations. Anonymized data are, however, available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- COVID-19:
-
Coronavirus disease 2019
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computer tomography
- ICU:
-
Intensive care unit
- PCR:
-
Polymerase chain reaction
- RT-PCR:
-
Real-time reverse transcriptase polymerase chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SD:
-
Standard deviation
References
Flemming S, et al. Surgery in times of COVID-19-recommendations for hospital and patient management. Langenbecks Arch Surg. 2020;405(3):359–64.
Collaborative, C.O. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020. https://doi.org/10.1002/bjs.11646.
Hu LQ, et al. COVID-19 and improved prevention of hospital-acquired infection. Br J Anaesth. 2020. https://doi.org/10.1016/j.bja.2020.05.037.
Rickman HM, et al. Nosocomial transmission of COVID-19: a retrospective study of 66 hospital-acquired cases in a London teaching hospital. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa816.
Heinzerling A, et al. Transmission of COVID-19 to health care personnel during exposures to a hospitalized patient—Solano County, California, February 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):472–6.
Wang D, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. https://doi.org/10.1001/jama.2020.1585.
Lai X, et al. Coronavirus disease 2019 (COVID-2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Netw Open. 2020;3(5): e209666.
Collaborative CO. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38.
Lei S, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21: 100331.
Doglietto F, et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy. JAMA Surg. 2020. https://doi.org/10.1001/jamasurg.2020.2713.
Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368–71.
Corman VM, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020. https://doi.org/10.2807/1560-7917.ES.2020.25.3.2000045.
Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Kruger S, et al. Performance and feasibility of universal PCR admission screening for SARS-CoV-2 in a German tertiary care hospital. J Med Virol. 2021;93(5):2890–8.
Anaesthesiology ESo. Airway management in patients suffering from COVID-19. 2020. https://www.esahq.org/esa-news/covid-19-airway-management/.
Robert-Koch-Institut. COVID-19 dashboard. https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4.
Sanyaolu A, et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med. 2020. https://doi.org/10.1007/s42399-020-00363-4.
Kane AD, et al. Peri-operative COVID-19 infection in urgent elective surgery during a pandemic surge period: a retrospective observational cohort study. Anaesthesia. 2020;75(12):1596–604.
Tilmans G, et al. Surgical outcomes after systematic preoperative severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) screening. Surgery. 2020;168(2):209–11.
Huybens EM, et al. What is the preferred screening tool for COVID-19 in asymptomatic patients undergoing a surgical or diagnostic procedure? World J Surg. 2020;44(10):3199–206.
Bellato V, et al. Screening policies, preventive measures and in-hospital infection of COVID-19 in global surgical practices. J Glob Health. 2020;10(2): 020507.
Puylaert CAJ, et al. Yield of screening for COVID-19 in asymptomatic patients before elective or emergency surgery using chest CT and RT-PCR (SCOUT): multicenter study. Ann Surg. 2020;272(6):919–24.
Nekkanti SS, et al. Mandatory preoperative COVID-19 testing for cancer patients-Is it justified? J Surg Oncol. 2020;122(7):1288–92.
Ji C, et al. Is elective cancer surgery safe during the COVID-19 pandemic? World J Surg. 2020;44(10):3207–11.
Glasbey JC, et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter comparative cohort study. J Clin Oncol. 2021;39(1):66–78.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This publication was supported by the Open Access Publication Fund of the University of Wuerzburg. This research received no external funding.
Author information
Authors and Affiliations
Contributions
SF and AW designed and supervised the study. SK, MK and SF collected data. FA performed statistical analysis of the dataset. FA, MKH and SK prepared tables. SF and MKH wrote the manuscript. CTG, AW, and MK revised and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical review and approval were waived for this study (ethical committee of University of Wuerzburg, Germany), since this research study was conducted retrospectively from data obtained for clinical purposes with all the procedures being performed were part of the routine care. The informed consent was waived by the ethics committee of the University of Wuerzburg, Germany, since patients cannot be identified by anonymized data used for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Flemming, S., Hankir, M.K., Kusan, S. et al. Safety of elective abdominal and vascular surgery during the COVID-19 pandemic: a retrospective single-center study. Eur J Med Res 26, 112 (2021). https://doi.org/10.1186/s40001-021-00583-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-021-00583-x