Abstract
Right ventricle (RV) dysfunction is a key outcome determinant and a leading cause of death for patients with chronic thromboembolic pulmonary hypertension (CTEPH). In this report, we followed the 5-year clinical journey of a patient with CTEPH. The tricuspid pressure gradient was significantly increased in the early phase of CTEPH and “normalized” at the late phase of this patient’s clinical journey, but this “normalized” gradient is not a positive treatment response but rather an ominous sign of advancing right heart failure owing to an exhaustion of RV contractile function. Thus, appropriate interpretation of the tricuspid pressure gradient change is of importance for assessing RV dysfunction and treatment outcome during follow-up in patients with CTEPH. Besides systolic pulmonary artery pressure (SPAP), other RV functional parameters such as tricuspid annular plane systolic excursion, RV fractional area change, and RV longitudinal strain, together with clinical markers, may provide additional guidance regarding functional improvement or progression in patients with CTEPH.
Similar content being viewed by others
Background
Pulmonary thromboembolism serves as a common cause of pulmonary hypertension (PH), termed chronic thromboembolic pulmonary hypertension (CTEPH; WHO Group IV) [1,2]. Fibrous organization of persistent pulmonary emboli leads to increased pulmonary vascular resistance and promotes adverse pulmonary vascular remodeling, thus contributing to further rises of pulmonary artery pressure. This vicious cycle governs the clinical course of human CTEPH including right ventricular (RV) hypertrophy and, ultimately, progressive right heart failure. It is known that RV dysfunction is a key determinant of patient outcome and the leading cause of death for patients with CTEPH [3-5]. A thorough clinical work-up is required to establish the diagnosis of CTEPH and guide patients through either surgical and/or medical treatment. Echocardiography is widely used to screen individuals for suspected PH and routinely applied during clinical follow-up settings. Here, we report the 5-year clinical journey of a patient with CTEPH.
Case presentation
A woman aged 68 years was admitted to our hospital due to progressive dyspnea in March 2008. She presented mild bilateral leg edema at physical examination. The ECG showed acute right ventricular strain (SI/QIII) and sinus tachycardia (heart rate = 120 beats/min). Blood tests evidenced elevated serum D-dimer (2.59 mg/L, that is, fivefold increase). Computed tomography (CT) revealed extensive bilateral thrombi in proximal and peripheral pulmonary arteries plus RV dilation and hypertrophy (Figure 1A,B,C). Pulmonary function tests indicated GOLD II chronic obstructive pulmonary disease (COPD). Arterial blood gas analysis suggested hypocapnia and hypoxemia (pCO2 30 mmHg; PO2 64 mmHg; O2 saturation 94%). Initial transthoracic echocardiography (TTE; Table 1) showed a significantly dilated RV with D-shaped left ventricle (LV) and a dilated right atrium (RA). LV and left atrium dimensions as well as LV ejection fraction were normal. Doppler-derived maximal systolic pulmonary artery pressure (SPAP) was 69 mmHg (maximum trans-tricuspid pressure gradient of 59 mmHg + estimated RA pressure of 10 mmHg). Diagnosis of CTEPH was established by above examinations and right heart catheterization examination. Other causes of PH were excluded. Initial therapy consisted of sildenafil (3 × 20 mg/day), oral anticoagulation, and diuretics. Therapy was sequentially escalated towards triple therapy including inhaled iloprost (6 × 2.5 μg/day) and endothelin receptor blockade with ambrisentan (1 × 10 mg/day). The patient repeatedly refused evaluation for pulmonary endarterectomy (PEA) and remained clinically stable on WHO level III for 4 years. The N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) levels also remained stable initially, but increased during long-term follow-up (from 2,400 to 14,300 pg/mL; Figure 2). The patient presented with decompensated right heart failure in October 2012 and was evaluated for PEA and heart/lung transplantation; however, the evaluation results were negative. After a stable period of several months under standard medication, the patient presented again with decompensated right heart failure in August 2013 and died in hospital due to cardiogenic shock.
Computed tomography scans at first clinical presentation and 3 months later. (A) Coronal contrast-enhanced CT scan at first clinical presentation shows a flattened eccentric thrombus in the main right pulmonary artery (black arrows). (A’) Repeat CT scan after 3 months of treatment shows the shrunken thrombus formation (black arrow). (B, B’) Coronal contrast-enhanced CT scans at the time of first diagnosis and 3 months later show multiple filling defects both at the bifurcation and in the left pulmonary arteries (white arrows). (C, C’) Axial contrast-enhanced CT scans show dilatation of the right ventricle (RV), dilatation of the right atrium, and thickening of the RV free wall both at initial presentation and 3 months later. LPA: left pulmonary artery; LV: left ventricle; RA: right atrium; RPA: right pulmonary artery; RV: right ventricle.
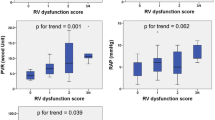
Serial TTE (Figure 3) revealed a constant elevation of Doppler-derived SPAP with the highest value of 86 mmHg between March 2008 and April 2012. Right heart catheterization showed correspondingly high mean pulmonary arterial pressure of 38 to 45 mmHg at this period (Table 1). Of note, Doppler-derived SPAP gradually decreased over the last two examinations. Reduced tricuspid annular plane systolic excursion (TAPSE; Figure 4, left) and RV fractional area (FAC) were additionally seen throughout the follow-up. Two-dimensional speckle tracking imaging (STI) revealed severely impaired RV longitudinal function (global longitudinal strain = −11%) with predominantly compromised function at the apex (Figure 3, right). Additionally, tricuspid regurgitation (TR) continuous-wave Doppler demonstrated a nominally “normal” peak pressure gradient (19 mmHg) with a late peaking velocity spectrum at the final examination. Interestingly, a normal tricuspid pressure gradient with a normal early peaking velocity spectrum was shown by Doppler echocardiography performed in 2007 before the clinical event of pulmonary thromboembolism (Figure 3).
Serial echocardiographic observations of tricuspid regurgitant jet (continuous-wave Doppler recording). Note the pseudo-normal trans-tricuspid pressure gradient (19 mmHg) with the pathological late-peaking velocity spectrum at the final examination (August 2013), clearly distinct from the normal pressure gradient exhibiting an early-peaking velocity spectrum at the examination in 2007, that is, prior to the clinical event of pulmonary thromboembolism.
Measurements of tricuspid annular plane systolic excursion (TAPSE; left) and right ventricular longitudinal systolic strain (LSsys; right) derived from two-dimensional speckle tracking imaging at the final examination (August 2013). Solid-colored lines indicate corresponding segmental strain curves and white dashed line indicates global strain curve on the right panel. Note the considerably reduced measurement values for TAPSE (normal range: >20 mm) and right ventricular global LSsys (−11%). Lat: RV lateral wall; RA: right atrium; RV: right ventricle; Sept: interventricular septum.
NT-proBNP levels, 6-min walk distance (6MWD), and invasive hemodynamic monitoring suggested that severe PH existed during the whole disease journey. Extremely enlarged RV and RA, dilated main PA diameter, and decreased cardiac output, as well as increased pulmonary vascular resistance also provided circumstantial evidence on progressive worsening in both RV volume and pressure overload in this patient. However, significantly elevated tricuspid pressure gradient in the early phase of CTEPH normalized at the late phase of this patient’s clinical journey. The potential reasons for pseudo-normalization of SPAP during development in this patient remain an issue of speculation. This decline of the pressure gradient is not due to improvement of tricuspid regurgitation but rather a feature of progressive right ventricular dysfunction, as indicated by a sustained reduction in TAPSE, RV FAC, and correspondingly reduced RV longitudinal strain in STI (Figure 3). Previous experimental study on chronic RV pressure overload model proved that RV systolic function is preserved, but diastolic function is impaired. To compensate, RA contractility increases to maintain filling stiffened ventricle, and the atrium acts as a reservoir than a conduit [6]. As time passes, RA pressure comes to be further increased due to the exhaustion of RA contractility. When the increased degree in the RA pressure is more than in the RV pressure, the pressure difference between RV and RA (tricuspid pressure gradient) will be reduced. Thus, we speculate that pseudo-normalization of the pressure gradient should not be interpreted as a positive treatment response but rather as an ominous sign of advancing right heart failure owing to an exhaustion of RV and RA contractile function. The shape of the velocity spectrum is another important sign in this context as the late-peaking velocity trace might be related to RV contractile dysfunction.
Additionally, we observed the discrepancy between echocardiographic-derived SPAP (reduced) and right heart catheterization measured pulmonary artery systolic pressure (increased) during the late course of PH in this patient. The underlying reason might be that echocardiographic-derived SPAP reflects the pressure gradient between RV and RA, which is low due to increased RA pressure in this patient at late disease phase. While invasive right heart catheterization-measured SPAP presents the real increased pressure situation at pulmonary artery.
In comparison with tricuspid pressure gradient, some clinical indices and other echocardiographic parameters might be additionally useful for predicting the outcome in this case. When retrospectively reviewing the full journey of this patient, sustained elevated NT-proBNP levels and a significantly low 6MWD were observed. Previous studies showed that BNP and NT-proBNP correlated well with RV function and prognosis in several forms of pulmonary hypertension [7-9]. The 6MWD has been widely used for measuring the response to therapeutic interventions for pulmonary and cardiac disease [8]. Our observation also demonstrated the value of monitoring 6MWD for evaluating PH disease progression. Therefore, monitoring these clinical indices during follow-up might be helpful for predicting the adverse outcome in patients with CTEPH besides standard echocardiographic parameters including SPAP, TAPSE, RV FAC, and STI.
Conclusions
In conclusion, “normalized” echocardiography-derived SPAP with the progression of the disease is a feature of progressive right heart dysfunction in patients with CTEPH. Besides SPAP, other RV functional parameters such as TAPSE, RV FAC, and RV longitudinal strain, together with clinical markers, may provide additionally useful guidance regarding functional improvement or progression in patients with CTEPH.
Consent
The study was approved by Local Ethics Committee at the University of Würzburg and conducted in accordance to the Declaration of Helsinki.
Written informed consent was obtained from the patient’s guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Simonneau G, Galie N, Rubin LJ, Langleben D, Seeger W, Domenighetti G, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2004;43(12 Suppl S):5S–12.
Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34–41.
Lewczuk J, Piszko P, Jagas J, Porada A, Wojciak S, Sobkowicz B, et al. Prognostic factors in medically treated patients with chronic pulmonary embolism. Chest. 2001;119(3):818–23.
Riedel M, Stanek V, Widimsky J, Prerovsky I. Longterm follow-up of patients with pulmonary thromboembolism. Late prognosis and evolution of hemodynamic and respiratory data. Chest. 1982;81(2):151–8.
Voelkel NF, Quaife RA, Leinwand LA, Barst RJ, McGoon MD, Meldrum DR, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114(17):1883–91.
Gaynor SL, Maniar HS, Bloch JB, Steendijk P, Moon MR. Right atrial and ventricular adaptation to chronic right ventricular pressure overload. Circulation. 2005;112(9 Suppl):I212–8.
Leuchte HH, Holzapfel M, Baumgartner RA, Ding I, Neurohr C, Vogeser M, et al. Clinical significance of brain natriuretic peptide in primary pulmonary hypertension. J Am Coll Cardiol. 2004;43(5):764–70.
Leuchte HH, Holzapfel M, Baumgartner RA, Neurohr C, Vogeser M, Behr J. Characterization of brain natriuretic peptide in long-term follow-up of pulmonary arterial hypertension. Chest. 2005;128(4):2368–74.
Suntharalingam J, Goldsmith K, Toshner M, Doughty N, Sheares KK, Hughes R, et al. Role of NT-proBNP and 6MWD in chronic thromboembolic pulmonary hypertension. Respir Med. 2007;101(11):2254–62.
Acknowledgements
This work was supported by grants from the Bundesministerium für Bildung und Forschung (BMBF01 EO1004).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DL, KH, and HP participated in the design of the study, and DL performed the statistical analysis. DL drafted the manuscript. FW, SS, and HP conceived of the study and participated in its design and coordination, and FW, KH, HP, and SS modified the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Liu, D., Hu, K., Pelzer, HT. et al. Journey of a patient with chronic thromboembolic pulmonary hypertension. Eur J Med Res 20, 20 (2015). https://doi.org/10.1186/s40001-015-0112-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-015-0112-x