Abstract
Microglia are the macrophages that reside in the brain. Activated microglia induces further activation of astrocytes and neuronal cells for mounting an immune response. However, activated microglia release neurotoxic mediators causing neuroinflammation, which is associated with chronic etiology of neurodegenerative diseases. We investigated the effect of ethanol extract of Physalis alkekengi L. var. francheti fruit (PAFE) on neuronal cell death mediated by activated microglia. PAFE decreased NO production and IL-6 secretion in LPS-stimulated BV-2 and primary microglial cells without reducing cell viability. Consistently, treatment with PAFE decreased iNOS and COX-2 expression and ERK phosphorylation in LPS-stimulated BV-2 cells. Finally, apoptosis of N2a cells grown in conditioned media prepared from LPS-stimulated BV-2 cells containing PAFE was inhibited via downregulation of the Bax/Bcl-2 ratio. Taken together, PAFE alleviates neuronal cell death by reducing neurotoxic mediators such as NO and IL-6 from activated microglia. Therefore, it could be a potential candidate to treat neurodegenerative diseases caused by chronic neuroinflammation.
Similar content being viewed by others
Introduction
Microglia are neurological macrophage that reside in the central nervous system and share tissue-specific primary immune functions linked to adaptive immune function [1, 2]. Microglia are activated by external cues including lipopolysaccharide (LPS), β-amyloid, and interferon-γ, which are accompanied by an inflammatory response following the release of a group of mediators including nitric oxide (NO), IL-6, IL-1β, prostaglandin E2, and TNF-α [3,4,5,6]. This secreted inflammatory mediators activate astrocytes, leading to further activation of microglia, forming amoeboid morphology with increased cell size for a protective role against threats [7,8,9]. However, uncontrolled activation of microglia derives chronic inflammation with accumulation of pro-inflammatory mediators, leading to chronic neuritis and neuronal cell death, which is associated with chronic progress of neurodegenerative diseases [10].
Physalis alkekengi L. var. francheti is an edible and medicinal plant that belongs to the Solanaceae family according to taxonomical classification and widely distributed from Southern Europe to South Asia as well as Northeast Asia [11]. Physalis alkekengi L. var. francheti fruit (PAF) is used as a raw material for health food and herbal medicine to treat various diseases such as chills, rheumatism, fungal infections, fever, sore throat, inflammation, and toothache in Korea and China [12]. It was known that various steroidal constituents containing physalins are abundant in PAF [13, 14]. Many studies support the idea that these steroidal constituents may contribute to obtaining benefits of PAF on human health, such as an anti-tumor activity [15] and anti-inflammatory activity [14]. In this study, we explored a neuroprotective role of PAF mediated by inhibiting inflammatory response of microglia. We investigated the effect of PAF on the release of inflammatory mediators from LPS-stimulated microglia and its influence on neuroblastoma cell death.
Materials and methods
Preparation of ethanol extract of Physalis alkekengi L. var. francheti fruit (PAFE)
Dried PAFE (voucher number: RPG-PAFE-001) was purchased at an herbal medicine store in Gyeongdong Market, Seoul, South Korea. The skin was crushed and dried for 64 h at 40 °C in a dryer. 60 g of dried PAFE was soaked in 1.5 L of 70% ethanol and extracted once for 2 h using ultrasonic waves. After then, impurities were removed using membrane filters and soluble fraction was concentrated using decompression concentrators to obtain about 6.3 g of dried solid extract, where the yield was 10.5%. The extract was obtained and stored at − 20 °C.
Cell culture
Murine microglia BV-2, primary microglia and neuroblastoma N2a cells were cultured in the DMEM (Hyclone, UT, USA) in the incubator (5% CO2, 37 °C). This media contains 10% of the FBS (RDTech, IL, USA) and Penicillin and streptomycin (100 U/mL each) (Welgene, GyeonBuk, KR) as an antibiotics. For the cell stimulation experiment, 100 ng/mL of LPS (Lipopolysaccharides from Salmonella enterica serotype typhimurium, L6143-1MG, Sigma-Aldrich, MO, USA) was used. All experiments using cultured cells were performed in this condition.
Measurement of NO production and cell viability
To measure NO production, microglial cells in 96-well plate (3 × 104 cells per well) were incubated for 24 h and then various concentration of PAFEs (0, 1, 10, 50, 100 μg/mL) were added. After 30 min, these cells were stimulated by treating LPS. Then, the Griess reagent was used to quantify amount of nitrite in the cultured medium. Briefly, 50 μL of the supernatant was collected and then mixed with 50 μL of Griess reagent containing 0.1% N-1-naphthylenediamine dihydrochloride and 1% sulfanilamide in 5% phosphoric acid. This mixture was measured at 570 nm using a spectrophotometer (BKMPR-1096A, BioKonvision, Gwacheon-Si, KR).
Viability of microglia cells were measured using the MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl-tetrazolium bromide). Cells were seed on a 96 well plate (2 × 104 cells per well) and incubated for 24 h. Then, PAFE (0, 1, 10, 50, or 100 μg/mL) was treated to the media and, after 30 min, LPS was treated for 24 h. After adding MTT reagent (Tokyo chemical industry, TOKYO, JP), they were measured at 595 nm using a spectrophotometer.
ELISA
BV-2 cells were seed on a 24-well plate (3 × 105 cells per well). After 24 h, various concentration of PAFEs (0, 1, 10, 50, 100 μg/mL) were treated for 30 min and then LPS was treated for 24 h. Supernatant from the cultured media was collected to measure amount of secreted IL-6 by using the immunoassay kit (R&D system, MN, USA).
Western blot analysis
Whole cell lysates were prepared and subject to western blot analysis. Antibodies used in western blot: ERK (Cell Signaling, #9102), iNOS (Cell Signaling, #13,120), COX-2 (Santa Cruz, sc-376861), p-ERK (Cell Signaling, #9101), Bcl-2 (Abcam, AB196495), and Bax (Abcam, AB53154). The band density in western blot was analyzed using NEO image for CheBI, ver 3.0 (Neosience, Seoul, KR).
Preparation of the conditioned media and apoptosis analysis of N2a cells
BV-2 cells were incubated for 24 h. After then, these cells were incubated with PAFE (0, 1, 10, 50, or 100 μg/mL) for 30 min, followed by incubation with LPS for 24 h. Then, this medium was centrifuged to collect supernatant as the conditioned medium [16]. This conditioned medium was supplied to N2a cells for 24 h incubation. After then, these N2a cells were subject to apoptosis and cell viability analysis using Annexin V/PI kit (Abcam, Cambridge, UK) and MTT assay kit, respectively. The apoptosis analysis was carried out by FACS (Aria III; BD Biosciences, NJ, USA) and data analysis by BD CellQuest pro software (BD Biosciences, CA, USA).
Statistical analysis
SAS software (PRISM) was used for all data analysis. All data present as mean ± standard deviation (S.D.). One-way ANOVA with Tukey's multiple comparison post-test was performed for statistical comparisons between different treatments.
Results
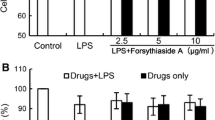
PAFE reduces NO generation in the BV-2 cells activated by treating LPS
Activated BV-2 microglia release NO as an inflammatory response. BV-2 cells were treated with PAFE (0, 1, 10, 50, or 100 μg/mL), and then stimulated with LPS. We observed that the production of nitrite, a soluble form of NO oxidation, decreased as the concentration of the PAFE increased beyond 1 μg/mL, suggesting that the PAFE inhibited NO generation in the BV-2 cells activated by LPS stimulation (Fig. 1a).
Effect of PAFE on NO production and cell viability in LPS-treated BV-2s. BV-2s were treated for 24 h with LPS after 30 min of processing various concentrations of PAFE. After then a production of nitrite and b cell viability were measured. BV-2s grown without treating PAFE and LPS-stimulation were considered control. c Expression of iNOS, COX-2, ERK, and p-ERK in BV-2s treated with PAFEs and treated with LPS. d Effect of PAFE on IL-6 secretion of BV-2s treated by LPS. PAFE of various concentrations was treated in BV-2s and treated by LPS for 24 h, and the secretion of IL-6 was then measured using ELISA. All data were presented together with ± S.D. as the average of the three independent experimental results. *p < 0.05 and **p < 0.01
Next, the viability of these BV-2 cells was analyzed using the MTT assay. There was almost no change in viability of all tested BV-2 cells. Since the cell viability was close to 100%, the concentrations of PAFE used in this experiment were not harmful and did not reduce the number of BV-2 cells (Fig. 1b). Taken together, the PAFE prevented LPS-induced NO production without reducing cell viability.
PAFE inhibits downstream signaling pathway of TLR4 in BV-2 cells stimulated with LPS
To understand the inhibitory effect of PAFE at the molecular level, expression of COX-2, iNOS, ERK, and p-ERK were analyzed in the BV-2 cells activated by treating LPS after incubation with PAFE (0, 10, 50, or 100 μg/mL) using western blotting (Fig. 1c). Expression of COX-2 and iNOS decreased in cells according to increase of PAFE concentration. Moreover, phosphorylated ERK decreased in response to treatment with all tested concentrations of PAFEs, whereas ERK expression did not change. Taken together, these results demonstrate that PAFE suppresses the ERK signaling cascade downstream of TLR4, thereby decreasing the expression of COX-2 and iNOS, and reduced NO production.
PAFE decreases secretion of IL-6 in the BV-2 cells activated by treating LPS
IL-6 secretion was quantitatively measured in the BV-2 cells activated by treating LPS after incubation with PAFE (0, 1, 10, 50, or 100 μg/mL) using ELISA (Fig. 1d). IL-6 secretion was suppressed when cells were incubated with PAFE at concentrations of 10, 50, and 100 μg/mL, but not 1 μg/mL. Notably, this inhibitory effect of the PAFE was concentration-dependent as in the case of NO production, and COX-2 and iNOS expression. This suggests that reduction of iNOS expression and inhibition of NO production by PAFE may prevent inflammatory responses by downregulating IL-6 secretion.
PAFE reduces NO generation in the primary microglia cells activated by treating LPS
PAFE effect on NO generation was examined in primary microglia cells (Fig. 2a). Nitrite production decreased in the primary microglia cells activated by treating LPS when treated with PAFE at concentrations of 50 and 100 μg/mL but not with 1 and 10 μg/mL. Although a relatively low concentration of PAFE had no effect on inhibiting NO generation in primary microglia cells stimulated with LPS, treatment with 50 and 100 μg/mL of PAFE resulted in significant reduction of NO production. Subsequently, the viability of the primary microglia cells used in this experiment was measured (Fig. 2b) and no difference in viability was observed, especially at the concentrations of 50 and 100 μg/mL. Thus, it was confirmed that PAFE inhibits NO generation in primary microglia cells stimulated with LPS without affecting cell viability, as shown in the case of BV-2 cells.
Effect of PAFE on NO production and cell viability of primary microglial cells treated by LPS. Primary microglial cells were treated for 24 h with LPS after 30 min of processing various concentrations of PAFE. Various concentration of PAFEs were treated in primary microglial cells and then treated with LPS for 24 h. After then a production of nitrite and b cell viability were measured. Primary microglial cells grown without treating PAFE and LPS-stimulation were considered control. All data were presented together with ± S.D. as the average of the three independent experimental results. *p < 0.05 and **p < 0.01
PAFE protects N2a cells from toxic mediators released from the BV-2 cells activated by treating LPS
PAFE relieved inflammatory response through the decreased release of neurotoxic mediators, which cause neuroinflammation and can impair neurons. We collected medium from the cultured LPS-stimulated BV-2 cells treated with PAFE (0, 1, 10, 50, or 100 μg/mL), or non-stimulated BV-2 cells cultured without treatment with the PAFE. We termed this CM-PAF (or control for the non-stimulated BV-2 cells). Next, these CM-PAFs were examined for their neurotoxic effects on other neuronal cells and the viability of N2a cells incubated with or without CM-PAFs was measured (Fig. 3). Viability of the N2a cells grown in the CM-PAF decreased significantly (p < 0.01), when compared with the control; however, the viability of N2a cells grown in the two CM-PAFs (50 and 100 μg/mL) increased by ~ 10–20% compared with other CM-PAFs (0, 1, and 10 μg/mL). In conclusion, this result suggested that PAFE may inhibit the release of neurotoxic mediators from BV-2 cells stimulated with LPS, and thus, protect neuronal cells from these toxic products.
Viability of neuronal cells grown on the CM-PAFE. CM-PAFE was prepared from the cultured media where LPS-treated BV-2s were grown after treating various concentration of PAFE. Control means the cultured media where non-treated BV-2s were grown. Viability of N2as grown on the CM-PAFEs or control were measured. All data were presented together with ± S.D. as the average of the three independent experimental results. *p < 0.05 and **p < 0.01
CM-PAF prevents apoptosis of N2a cells via decreasing Bax/Bcl-2 ratio
Neurotoxic mediators released from activated microglia induce apoptotic cell death. We investigated whether CM-PAF could inhibit the apoptosis caused by toxic molecules released from BV-2 cells stimulated with LPS (Fig. 4a–e). N2a cells were treated with control or CM-PAF (0, 1, 10, 50, or 100 μg/mL of PAFE) and apoptosis and necrosis of these cells were analyzed by FACS. Interestingly, apoptosis of N2a cells decreased as the concentration of PAFE used for the CM increased. In particular, early apoptosis decreased significantly under these conditions. This demonstrated that treatment with CM from cells treated with PAFE prevents apoptosis of neuronal cells.
Apoptosis of neuronal cells grown on the CM-PAF. CM-PAF was prepared from the cultured media where LPS-treated BV-2s were grown after treating various concentration of PAF. Control means the cultured media where non-treated BV-2s were grown. Apoptosis and necrosis of N2as were analyzed in the N2as grown on a control, b CM-PAF (0 μg/mL), c CM-PAF (10 μg/mL), d CM-PAF (50 μg/mL), e CM-PAF (100 μg/mL). Expression of Bcl-2 and Bax in neuronal cells grown on CM-PAFs. CM-PAF was prepared from the cultured media where LPS-treated BV-2s were grown after treating various concentration of PAFE. Control means the cultured media where non-treated BV-2s were grown. N2as were grown on control or CM-PAFs and then f expression of Bcl-2, Bax, and β-actin in those cells were shown by western blot. g The Bax/Bcl-2 ratio was calculated based on the relative density shown in the western blot by using the ImageJ software
Next, the expression of Bax and Bcl-2 in these N2a cells was analyzed by western blotting (Fig. 4f). In N2a cells treated with CM-PAFs (0 and 10 μg/mL), expression of Bcl-2 and Bax significantly decreased and increased, respectively, compared with the control. However, expression of Bcl-2 and Bax increased and decreased, respectively, in N2a cells treated with CM-PAFs (50 and 100 μg/mL). Subsequently, the ratio of Bax/Bcl-2 was calculated based on the western blotting data (Fig. 4g). Although the ratio of N2a cells treated with CM-PAFs (0 and 10 μg/mL) significantly increased compared with the control, this ratio decreased gradually in N2a cells treated with CM-PAFs at higher concentrations (50 and 100 μg/mL).Since the increased ratio of Bax/Bcl-2 indicates the progress of apoptosis, these results indicate that downregulation of the Bax/Bcl-2 ratio contributes to the inhibition of apoptosis in N2a cells treated with CM containing high dose of PAFE.
Discussion
Activated microglial induces the secretion of various inflammatory mediators. i. e. NO, IL-6, TNF-α, IL-1β, etc. These changes are known to trigger the progression of neurodegenerative diseases by generating an inflammatory niche [17]. IL-6 is mainly secreted by glial cells, inducing inflammatory cells aggregation and increasing reactive oxygen species as well as cooperating with TNF-α, which causes calcium overload and cellular apoptosis as an inflammatory response [18]. Histopathological features of AD are characterized by extracellular deposit of senile plaques comprising amyloid-beta (Aβ) peptides in its fibrillary form as well as neurofibrillary tangles [19]. Aβ aggregates in AD patients promote the reactivity of glial cells, thus resulting in the consequently increased NO release [20]. Unregulated NO production is considered to cause neuronal cell death via apoptosis; it induces aberrant mitochondrial membrane potential, causing cytochrome c to leak into cytosol. This cytochrome c form a complex with Apaf-1 and caspase-9, which cleaves caspase-3 to initiate the apoptosis [21]. Thus, this strongly supports the notion that the inhibition of IL-6 and NO production can alleviate neurodegenerative disorders by preventing the apoptotic neuronal cell death induced by inflammatory mediators.
PAF, the fruit of a perennial herb widely used in East Asia, has been reported to possess anti-tumor, anti-bacterial, and anti-inflammatory activities [22]. It contains various physalin steroidal constituents, including physalin A and physalin B, which are considered a major contributor to these beneficial effects. For example, the growth of A549 cells was inhibited by physalin A through cell cycle arrest in the G2/M phase [23]. The expression of detoxifying enzymes was also increased by physalin A by upregulating the Nrf2 pathway in HepG2 cells [24]. The growth of breast and lung cancer cells was inhibited by Physalin B through cell cycle arrest [25,26,27,28]. In addition, physalin B exerts therapeutic effects on ulcerative colitis by inhibiting inflammation [16]. However, its role in neuroinflammation remains unclear. Here we demonstrated that PAFE alleviated the neurotoxic effect of activated microglia; it reduced the release of IL-6 and NO by suppressing the downstream signaling pathway of TLR4, resulting in the protection of neuronal cells from apoptosis. Consequently, this study provides novel insights into the role of PAFE in neuroprotection. Nevertheless, the role of physalin constituents in neuroprotection against neuroinflammation needs to be explored further.
In neurodegenerative diseases, numerous studies have focused on neuroinflammation as the cause of chronic neurological disorders. When neuroinflammation is induced, resident macrophages, such as microglial cells, release various neurotoxic mediators, which are often associated with neuronal damage. In this context, our findings support the idea that PAFE could serve as a potential agent to treat the progression of neurodegenerative diseases, such as AD, by inhibiting neuroinflammation.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Moisse K, Strong MJ (2006) Innate immunity in amyotrophic lateral sclerosis. Biochem Biophys Acta 1762:1083–1093
Rivest S (2009) Regulation of innate immune responses in the brain. Nat Rev Immunol 9:429–439
Moreillon P, Majcherczyk PA (2003) Proinflammatory activity of cell-wall constituents from gram-positive bacteria. Scand J Infect Dis 35:632–641
Block ML, Zecca L, Hong JS (2007) Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci 8:57–69
Sugama S (2009) Stress-induced microglial activation may facilitate the progression of neurodegenerative disorders. Med Hypotheses 73:1031–1034
Pangestuti R, Bak SS, Kim SK (2011) Attenuation of pro-inflammatory mediators in LPS-stimulated BV2 microglia by chitooligosaccharides via the MAPK signaling pathway. Int J Biol Macromol 49:599–606
Minghetti L (2004) Cyclooxygenase-2 (COX-2) in inflammatory and degenerative brain diseases. J Neuropathol Exp Neurol 63:901–910
Griffiths MR, Gasque P, Neal JW (2009) The multiple roles of the innate immune system in the regulation of apoptosis and inflammation in the brain. J Neuropathol Exp Neurol 68:217–226
Amor S, Puentes F, Baker D, van der Valk P (2010) Inflammation in neurodegenerative diseases. Immunology 129:154–169
Rojo LE, Fernandez JA, Maccioni AA, Jimenez JM, Maccioni RB (2008) Neuroinflammation: implications for the pathogenesis and molecular diagnosis of Alzheimer’s disease. Arch Med Res 39:1–16
Yang H, Han S, Zhao D, Wang G (2014) Adjuvant effect of polysaccharide from fruits of Physalis alkekengi L. in DNA vaccine against systemic candidiasis. Carbohydr Polym 109:77–84
Tong H, Liang Z, Wang G (2008) Structural characterization and hypoglycemic activity of a polysaccharide isolated from the fruit of Physalis alkekengi L. Carbohydr Polym 71:316–323
Li K, Diao YP, Wang MD, Yang SS, Zhang HL, Huang SS, Yang H (2010) Chemical constituents of the fruits of Physalis alkekengi L. var. franchetii (Mast.) Makino. Chin J Org Chem 30:128–131
Ji L, Yuan Y, Luo L, Chen Z, Ma X, Ma Z, Cheng L (2012) Physalins with anti-inflammatory activity are present in Physalis alkekengi var. franchetii and can function as Michael reaction acceptors. Steroids 77:441–447
Magalhaes HI, Veras ML, Torres MR, Alves AP, Pessoa OD, Silveira ER, Costa-Lotufo LV, de Moraes MO, Pessoa C (2006) In-vitro and in-vivo antitumour activity of physalins B and D from Physalis angulata. J Pharm Pharmacol 58:235–241
Zhang Q, Xu N, Hu X, Zheng Y (2020) Anti-colitic effects of Physalin B on dextran sodium sulfate-induced BALB/c mice by suppressing multiple inflammatory signaling pathways. J Ethnopharmacol 259:112956
Thompson KK, Tsirka SE (2017) The diverse roles of microglia in the neurodegenerative aspects of central nervous system (CNS) autoimmunity. Int J Mol Sci 18(3):504
Li SJ, Liu W, Wang JL, Zhang Y, Zhao DJ, Wang TJ, Li YY (2014) The role of TNF-alpha, IL-6, IL-10, and GDNF in neuronal apoptosis in neonatal rat with hypoxic-ischemic encephalopathy. Eur Rev Med Pharmacol Sci 18:905–909
Maccioni RB, Munoz JP, Barbeito L (2001) The molecular bases of Alzheimer’s disease and other neurodegenerative disorders. Arch Med Res 32:367–381
Saez TE, Pehar M, Vargas M, Barbeito L, Maccioni RB (2004) Astrocytic nitric oxide triggers tau hyperphosphorylation in hippocampal neurons. In Vivo 18:275–280
Nomura Y (2004) Neuronal apoptosis and protection: effects of nitric oxide and endoplasmic reticulum-related proteins. Biol Pharm Bull 27:961–963
Kang H, Kwon SR, Choi HY (2011) Inhibitory effect of Physalis alkekengi L. var. franchetii extract and its chloroform fraction on LPS or LPS/IFN-gamma-stimulated inflammatory response in peritoneal macrophages. J Ethnopharmacol 135:95–101
Kang N, Jian JF, Cao SJ, Zhang Q, Mao YW, Huang YY, Peng YF, Qiu F, Gao XM (2016) Physalin A induces G2/M phase cell cycle arrest in human non-small cell lung cancer cells: involvement of the p38 MAPK/ROS pathway. Mol Cell Biochem 415:145–155
Shin JM, Lee KM, Lee HJ, Yun JH, Nho CW (2019) Physalin A regulates the Nrf2 pathway through ERK and p38 for induction of detoxifying enzymes. BMC Complement Altern Med 19:101
Cao C, Zhu L, Chen Y, Wang CH, ShenTu JZ, Zheng YL (2019) Physalin B induces G2/M cell cycle arrest and apoptosis in A549 human non-small-cell lung cancer cells by altering mitochondrial function. Anticancer Drugs 30:128–137
Wang A, Wang S, Zhou F, Li P, Wang Y, Gan L, Lin L (2018) Physalin B induces cell cycle arrest and triggers apoptosis in breast cancer cells through modulating p53-dependent apoptotic pathway. Biomed Pharmacother 101:334–341
Jia J, Kang XG, Liu YF, Zhang JW (2020) Inhibition of human liver cancer cell growth by evodiamine involves apoptosis and deactivation of PI3K/AKT pathway. Appl Biol Chem 63(1):1–8
Dinku W, Isaksson J, Rylandsholm FG, Bour P, Brichtova E, Choi SU, Lee SH, Jung YS, No ZS, Svendsen JSM, Aasen AJ, Dekebo A (2020) Anti-proliferative activity of a novel tricyclic triterpenoid acid from Commiphora africana resin against four human cancer cell lines. Appl Biol Chem 63(1):1–11
Acknowledgements
Not applicable.
Funding
This work was supported by National Research Foundation of Korea (NRF) Grant (2018M3A9F3055925) funded by the Korean government (Ministry of Science, ICT & Future Planning) to B.C.L.
Author information
Authors and Affiliations
Contributions
BHP and BCL contributed to the writing of the manuscript and performed the majority of data analysis. OWK and ISK performed experiments and prepared raw materials. HML, YJR, MK, YJ, HC, JKP, and ZZ contributed to the discussion of experimental results and data. BCL and BHP planned and led this research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests. The authors have filed a patent application relating to the technology.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, B.H., Kwon, O.W., Kim, I.S. et al. Physalis alkekengi L. var. francheti alleviates neuronal cell death caused by activated microglia in vitro. Appl Biol Chem 64, 23 (2021). https://doi.org/10.1186/s13765-021-00594-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13765-021-00594-6