Abstract
Background
Cockroaches can pose a significant health risk in hospital environments because they may serve as reservoirs and vectors for nosocomial pathogens. Cockroaches harbor epidemiologically significant extended spectrum and metalo beta lactamase producing Gram negative bacterial pathogens, which complicate nosocomial infections.
Objectives
The main aim of this study is to determine aetiology and phenotypic extended spectrum and metalo beta lactamase producing Gram negative bacteria pathogens from cockroaches collected in hospitals.
Methods
A cross-sectional study was employed from February to May 2022 to determine the antibiotic resistance producing bacterial isolates from cockroaches by giving special emphasis to metalo beta lactamase and extended spectrum beta lactamase production from different wards of WSUCSH. Cockroaches were collected with hands wearing sterile gloves. External homogenate was prepared and incubated microbiologically by using different culture media and differentiated biochemically. Antimicrobial susceptibility testing was performed by disk diffusion method. ESBL production was conducted using double disc synergy method and double disk method was used to detect MBL enzyme detection. Descriptive statistics was used to determine prevalence and percentage.
Result
Out of 245 cockroaches, 108 Gram negative bacteria were isolated. K. pneumoniae 29(26.9%) was the most predominant bacteria and Enetrobacter spp. 8(7.4%), was the least. All, K. pneumoniae, P. mirabilis, and Enterobacter isolates were pan-resistant to Ampicillin. P.aeruginosa and P.mirabilis antibiotics showed ≥ 80% resistant for amoxicillin/clavulanic acid antibiotics. Cefotaxime, ceftazidime, ceftriaxone and imipenem showed relative efficacy compared with other antibiotics. Out of 78 amoxicillin-clavulanic acid resistant isolates, 42(34.7%) were ESBL producers. ESBL production is more depicted by P. aeruginosa, A. baumannii, K. pneumoniae and E. coli. The overall prevalence of MBL production is 29(23.1%). K. pneumoniae P. aeruginosa, E.coli, A. baumannii, Enterobacter spp and K.oxytoca revealed MBL production.
Conclusion
The overall prevalence of ESBL and MBL producing nosocomial agents from hospital cockroaches was 34.7% and 23.1% respectively. P.aeruginosa, A.baumannii, K.pneumoniae and E.coli showed pronounced ESBL production. All bacterial isolates except P. mirabilis and C. freundii showed MBL production. The needed to evaluate our antibiotic stewardship program and antibiotic resistance detection for treatment is mandatory. The impact of cockroach as a source of AMR should be sought.
Similar content being viewed by others
Introduction
Antimicrobial resistance (AMR) is a serious global health threat that makes infections harder to treat and increases the risk of disease spread, severe illness and death. AMR is driven by the misuse and overuse of antimicrobials in humans, animals and plants. AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths. AMR also has significant economic costs and could result in US$ 1 trillion additional healthcare costs by 2050 [1].
Cockroaches are known to carry and transmit various bacterial species, including those that cause gastroenteritis in humans. They can contaminate food and food-handling surfaces through their droppings or by mechanical transfer from their bodies [2].
Cockroaches can pose a significant health risk in hospital environments because they may serve as reservoirs and vectors for nosocomial pathogens [3]. Cockroaches have long been regarded as possible vectors of human entero-pathogens owing to their unsanitary lifestyle and their indiscriminate feeding on sanitary wastes and human meals.
In hospitals, cockroaches can act as potential vectors in the epidemiology of nosocomial infections, especially the transmission of drug-resistant Escherichia coli, Pseudomonas aeruginosa, Klebsiella spp., and several other potential pathogens [3]. Studies have shown that 25 different species of medically important bacteria have been isolated from cockroaches in public hospitals in Ethiopia [5].
Cockroaches also harbor epidemiologically significant antibiotic-resistant organisms, such as carbapenem-resistant Enterobacteriaceae, which complicate nosocomial infections [3]. Studies in Ghana and Algeria showed that household and hospital cockroaches could serve as reservoirs of the CTX-M-15, OXA-48, and NDM-1 genes that share beta-lactam resistance determinants with humans [6, 7]. The cockroach brain has antimicrobial properties, and this is thought to be an important factor that accounts for the carriage of antibiotic-resistant organisms among cockroaches [8].
In hospitals, cockroaches that carry antibiotic-resistant bacteria could easily disseminate these organisms on hospital equipment and, therefore, facilitate their transmission to patients. This implies that cockroaches could play a significant role in outbreaks of nosocomial pathogens in hospitals, though little attention has been given to this.
As a preliminary assessment, the hospital infection prevention team takes a visit to the hospital with our research team in 2021. Cockroach infestation was observed everywhere including patients’ meals provided by the hospital. Even though these pests are commonly available, no specific study was conducted on the insects as well no correlational intervention was also done on patients by assumption of how filthy these pests are. So this research team decided to conduct this study and reveal the findings to the hospital.
Materials and methods
Settings and population
A cross-sectional study was employed from February to May 2022 to determine the antibiotic resistance producing bacterial isolates by giving special emphasis to MBL and ESBL producing bacteria from wards of Intensive Care Unit (ICU), operation room (OR), Obstetrics (OBS), Out-patient department (OPD), Surgical (S) and Pediatric (P) wards where much cockroach infestation was observed in WSUCSH (Wolaita Sodo university comprehensive specialized teaching hospital). Wards were selected based on the patient flow, risk, longer hospital stay and availability of vulnerable patients who are at risk of hospital acquired infection.
Only adult cockroaches having whole body parts were included in the study and those cockroaches which were dead or showing missing body parts, nymphs, and eggs of cockroaches were excluded from further sample processing.
Arthropod collection and sample preparation
A total of 245 cockroaches were randomly collected twice a day for 45 consecutive working days. The cockroaches were collected with hands wearing sterile gloves and placed in a sterile screw-capped 250 ml jar. Pests were transported to the WSUCSH microbiology laboratory for bacteriological analysis within five minutes of collection.
The collected cockroaches were immobilized by frigidity at 0°C for 5 min. The external body surface of immobilized cockroaches was washed by shaking in 5 ml of 0.85% sterile normal saline for two minutes and the wash was taken as an external homogenate sample and checked for bacterial growth [9, 10].
Isolation and identification of bacterial pathogens
One ml of the external homogenates was suspended separately into 9 ml of sterile dilution test tubes containing buffered peptone water (BPW) and incubated at 37°C for 18–24 h. Each one of the growth from BPW was inoculated on the following primary media such as MacConkey agar, and sheep blood Agar for 18–48 h to grow. After 24 and 48 h pure colony of bacterial isolate was preliminary characterized by colony morphology, Gram-staining procedure, and API-20E Biomeriux France, for the isolation of Eneterobacterciaeae [10].
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was performed for bacterial isolates by disk diffusion method on Mueller-Hinton agar (Oxoid). Bacterial inoculums were prepared by suspending the freshly grown bacteria in 4-5 ml sterile nutrient broth and the turbidity was adjusted to that of a 0.5 McFarland standard. The antimicrobial susceptibility testing was performed against the following discs, Amikacin (AMK, 30 µg); Ciprofloxacin (CIP, 5 µg); Gentamicin (GEN, 10 µg); Cefepime, CFP, 30 µg); Ampicillin (AMP, 10 µg); Amoxicillin/clavulanic acid (AMC 20 µg/10 µg; Ceftazidime (CAZ) 30 µg); Ceftriaxone (CRO, 30 µg) and Imipenem (IPM 10 µg). [11].
Detection of ESBL production
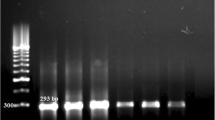
ESBL production was conducted by using double disc method. Cefotaxime and ceftazidime resistant isolates under Kirby-Bauer disk diffusion test were selected and checked for ESBL. The bacterial suspension was prepared while taking 2–3 fresh colonies and adjusted to 0.5 McFarland standards. Lawn culture was done on the Mueller-Hinton Agar (MHA) plate. Cefotaxime (30 µg) and ceftazidime (30 µg) disks were placed onto the inoculated MHA plate and incubated overnight at 37°C. Isolates that revealed ≤ 22 mm inhibition zone size for ceftazidime and/or ≤ 27 mm for cefotaxime were considered as potential ESBL producers. The ceftazidime and ceftazidime/clavulanic acid discs and cefotaxime/ cefotaxime-clavuanic acid were placed at 20 mm apart on the agar surface and incubated overnight at 37°C. After overnight incubation a ≥ 5 mm increase in zone diameter for either cefotaxime or ceftazidime tested in combination with clavulanic acid, were taken as indicative for ESBL production [11].
Detection of MBL production
Imipenem-resistant isolates were screened for producing MBL. The double disk method was used to detect this enzyme. A disc of Imipenem alone (10 µg) and Imipenem (10 µg) in combination with EDTA (750 µg/disc) was placed at the distance of 20 mm (center to center). After overnight incubation at 35 °C, a ≥ 7 mm increase in the inhibition zone of diameter around Imipenem-EDTA discs, as compared to imipenem discs alone, interpreted as indicative of MBL production [12].
Quality control measures
The reliability of the study findings was guaranteed by implementing quality control measures throughout the whole process of laboratory work. Staining reagents, culture media, and antimicrobial discs were checked for their normal shelf life before use. Culture media were prepared based on the manufacturer’s instruction then its sterility was checked by incubating 5% of the batch at 35–37°C overnight and observing bacterial growth. The quality of culture media and antimicrobial susceptibility test was checked by using reference strains of E. coli (ATCC 25922) and P. aeruginosa (ATCC 6538). E. coli ATCC 25,922 and K. pneumoniae ATCC700603 (ESBL-positive isolate) were used as the negative and positive controls, respectively.
Data processing and analysis
Data was edited and entered into SPSS for Windows version 20. Descriptive statistics was used to determine prevalence and percentage. The processed data were presented using a table and figure.
Results
Magnitude of cockroach infestation
Out of a total of 245 cockroaches, the highest infestations of cockroaches were seen in the obstetrics ward followed by the Pediatric ward, and OPD, Surgery, and OR ward followed by the prevalence of cockroaches respectively. However, the least infestation was recorded in the ICU room (Fig. 1).
Bacteria isolated from Hospital cockroaches
Out of 245 cockroaches collected in different wards of the hospital, 108 Gram negative bacterial isolates were isolated. K. peumoniae 29(26.9%) was the most predominant bacteria and Enetrobacter 8(7.4%), was the least (Fig. 2).
Antimicrobial susceptibility pattern
The susceptibility pattern of bacterial isolates (n = 121) identified from cockroaches was tested for nine different antibiotics (Table 1). Accordingly, all K. pneumoniae, P. mirabilis, and Enterobacter isolates were pan-resistant to ampicillin. P. aeruginosa and P. mirabilis antibiotics showed ≥ 80% resistant for amoxicillin/clavulanic acid antibiotics. Cefotaxime, ceftazidime, ceftriaxone and imipenem showed relative efficacy compared with other antibiotics. P. aeruginosa depicted resistance rate of 66.7% for cefotaxime. P.mirabilis showed 66.7% resistance. Ceftazidime on the other hand showed > 60% resistance for E. coli and Enterobacter spp. K. oxytoca and P. aeruginosa both became resistant, 70% for imipenem. A. baumannii showed very high resistance for ciprofloxacin, and gentamicin (Table 1).
ESBL production
Out of 121 bacterial isolates, 42(34.7%) were ESBL producers. ESBL production is more depicted by A.baumannii 7(53.8%), P.aeruginosa 8(53.3%), and K.pneumoniae 15(51.7%)(Table 2).
MBL production rate
The overall prevalence of MBL production is 28(23.1%). Half of the P.aeruginosa produces MBL and 6(46%) A.baumannii isolates were the second. On the other hand a single Enterobacter spp. revealed MBL enzyme production (Fig. 3).
Discussion
Cockroaches as a reservoir for hospital acquired pathogens pose a serious concern in the hospital environment. Bacterial isolates of A.baumannii, C. freundii, E. coli, Entrobacter, K.oxytoca, K. pneumoniae, P. mirabilis, and P.aeruginosa were identified from cuticle of cockroaches in this study. Similarly, these bacteria were also isolated from external surface of cockroaches collected from health care settings according to different studies done previously [5, 13,14,15,16,17,18,19,20,21].
K. pneumoniae is the predominant isolate followed by E.coli and C. freundii. This finding is similar with a study conducted in the country and elsewhere [17, 22,23,24,25]. This isolates are responsible for diverse types of nosocomial and community acquired infections, notably pneumonia, urinary tract infection, respiratory tract infection, skin infections, septicemia, and gastroenteritis.
A.baumannii was first detected in the same setting from the hospital environment in the operation theatre and intensive care unit [26]. The detection of A.baumannii from cockroaches in different wards in this study is the first one compared with previous studies in the country. Previous studies detect Acinetobacter species but only to the genus level [5, 17]. On the other hand, previous studies elsewhere detected this bacterium from surface and gut of cockroaches in different environments. This may indicate that enough attention has not been given for this bacterium even though the World Health Organization (WHO) listed carbapenem-resistant A. baumannii as a critical priority, for which, new antibiotics are urgently needed [1].
Hospital cockroaches have been reported to carry highly antibiotic-resistant bacteria and they could easily disseminate on hospital equipment and facilitate their transmission to patients [3]. In the current study, very high rate of antibiotic resistance (≥ 80%) is evidenced by P.aeruginosa (AMX/CLA, CN, and AK), A. baumannii (AK, CN) Enterobacter spp. (AMP) and P.mirabilis(AMX/CLA). This finding corroborates with studies in the country and elsewhere [5, 7, 9, 16, 18, and 23]. Resistance rate which is in harmony with this study was also reported in the same setting from Hospital surfaces and inpatients where P.aeruginosa, E.coli and Proteus isolates become pan resistant for ampicillin [24, 25].
Most of the bacterial pathogens revealed high rate of cephalosporin (cefotaxime, ceftazidime and ceftriaxone) resistance in the current study. E. coli resistance to ceftazidime, and ceftriaxone was 80.5%, and 78.2%, respectively. Higher percentages of the isolates were also exhibited resistance to amoxicillin-clavulanic acid (74.1%), and cefoxitin (67.2%) in the previous study conducted from this pests [26] A cause for concern is the high resistance displayed to the cephalosporins, which are frontline antipseudomonal drugs for treating P. aeruginosa infections, increased resistance to this class of antibiotics will not be favorable and will result in limited treatment options [27].
A.baumannii showed high rate of resistance for ciprofloxacin, and gentamicin. Imipenem resistance for A.baumannii and P.aeruginosa was also observed from Hospital environment of operation and ICU of the same settings [28]. This antibiotics is one of the diagnostic indicator of MBL producers where > 70% resistance was also detected in different studies from cockroaches in the country and elsewhere. Resistance to carbapenem,70% to imipenem is quite unexpected, given the fact that carbapenems represent one of the most effective and among the best option for treating Gram-negative infections particularly MDR infections [29].
Vector potential of cockroaches for ESBL and MBL producing bacteria is a grave and worrisome concern. The overall prevalence of ESBL resistance is 34.7% in this study. Different prevalence of ESBL production was detected ranging from 15.6 to 91.7% across literature in the world. The discrepancy in different settings could be attributed to difference in bacterial isolates, study settings, antimicrobial stewardship program availability and number of isolate where percentages were formulated for MBL production [6, 7, 30,31,32,33,34].
In this study, all the isolated Gram negative bacterial isolates showed ESBL production. In the same manner, ESBL production among bacteria from cockroaches were also noted from previous findings elsewhere [6, 7, 30,31,32,33,34,35,36,37]. ≥50% ESBL production rate was revealed for P.aeruginosa, A.baumannii, K. pneumoniae and E.coli isolates. ESBL percentage of 55.8% and 62.5% was also isolated from A. baumannii and P. aeruginosa in the current settings from hospital environments [28].
The overall MBL production in this study is 23%. Studies corroborated with this finding, 19% were also evidenced from studies in Iraq [34]. Relatively comparable MBL production was detected from P.aeruginosa and A.baumannii isolates from environmental samples of the current study settings [28]. On the other hand, lower findings from ours, 13.8% [32] and 3% [6] were also recorded from Nigeria and Ghana respectively.
Five different bacterial isolates, P.aeruginosa, A.baumannii, K.pneumoniae, E.coli and Enterobacter species depicted MBL production in the current study. MBL producing bacterial isolates, A.baumannii and P.aeruginosa were also identified from cockroaches in Iran. In addition to that VIM-2 Metallo-β-Lactamase producing Pseudomonas putida was also detected from cockroaches in an Algerian Hospital for the first time. E.coli and K.pneumoniae MBL production from such pests were also detected from previous studies elsewhere [6, 7, 32–34,38]. Enterobacter species showing MBL production is the first of its own in the country though a study conducted in Algeria showed this finding [7].
Conclusion
Extended spectrum beta lactamase and metalo beta lactamase production rate were 53.8% and 23.1% respectively. All identified bacterial isolates showed ESBL production. More than half of P. aeruginosa A. baumannii K. pneumoniae, isolates evidenced ESBL production. A.baumannii, K.pneumoniae, E.coli and Enterobacter and K.oxytoca isolates depicted MBL production with from 13 to 50%. Half of P.aeruginosa and 46% of A.baumannii depicted MBL enzyme production. Due attention is needed for non-clinical sources like cockroaches as a source for ESBL and MBL production. Antibiotic stewardship programs in the hospital needs to widen their target and take notice of vector capacity of cockroaches for AMR.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AMR:
-
Antimicrobial resistance
- ATCC:
-
American type culture collection
- BPW:
-
Buffered Peptone Water
- CLSI:
-
Clinical and Laboratory Standards Institute
- ESBL:
-
Extended spectrum beta lactamase
- ICU:
-
Intensive Care Unit
- MBL:
-
Metalo beta lactamase
- OPD:
-
Out-patient department
- OR:
-
Operation room
- OBS:
-
Obstetrics
- P:
-
Pediatric
- SPP:
-
Species
- SPSS:
-
Statistical Package for Social Science
- S:
-
Surgical
- WHO:
-
World health organization
- WSUCSH:
-
Wolaita Sodo University comprehensive specialized Hospital
References
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):P629–655. https://doi.org/10.1016/S0140-6736(21)02724-0.
Cloarec A, Rivault C, Fontaine F, Guyader AL. Cockroaches as carriers of bacteria in multi-family dwellings. Epidemiol Infect. 1992;109(3):483–90. https://doi.org/10.1017/S0950268800050470.
Donkor ES, Nosocomial Pathogens. An In-Depth analysis of the Vectorial potential of cockroaches. Trop Med Infect Dis. 2019;4:14.
Fakoorziba MR, Eghbal F, Hassanzadel J. Cockroaches are a potential vector of pathogenic bacteria found in nosocomial infectious. Ann Trop Parasitol. 2010;104(6):521–8.
Tilahun B, Worku B, Tachbele E. High load of multi-drug resistant nosocomial neonatal pathogens carried by cockroaches in a neonatal intensive care unit at Tikuranbesa specialized hospital, Addis Ababa, Ethiopia. Antimicrob Resist Control. 2012;1:1–12.
Obeng-Nkrumah N, Labi A, Blankson H, Awuah-Mensah G, Oduro-Mensah D, Anum J, Teye J, Kwashie S, Bako E, Ayeh-Kumi PF et al. Household cockroaches carry CTX-M-15, OXA-48 and NDM-1, and share beta-lactam resistance determinants with humans. bioRxiv. 2018.
Loucif L, Gacemi-Kirane D, Cherak Z, Chamlal N, Grainat N, Rolain JM. First Report of German cockroaches (Blattella germanica) as reservoirs of CTX-M-15 extended-Spectrum-β-Lactamase- and OXA-48 carbapenemase-producing Enterobacteriaceae in Batna University Hospital. Algeria Antimicrob Agents Chemother. 2016;60:6377–80.
Lee S, Atkins H, Duce I, Khan NA. Cockroach and Locust: physicians’ answer to infectious diseases. Int J Antimicrob Agents. 2011;37:279–80.
Vazirianzadeh B, Mehdinejad M. Identification of bacteria which possible transmitted by polyphaga aegyptica (Blattodea: Blattidae) in the region of Ahvaz, Southwest Iran. Jundishapur J Microbiol. 2009;2:36–40.
Cheesbrough M. District Laboratory Practice in Tropical Countries. New York, NY, USA: Cambridge University Press; 2006. [Google Scholar].
2018. CLSI. Performance standards for antimicrobial susceptibility testing. CLSI supplement M100. 28th ed. Clinical and Laboratory Standards Institute: Wayne, PA, Fotedar R, Nayar E, Samantray JC, Shriniwas Banerjee U, Dogra V, Kumar A. Cockroaches as vectors of pathogenic bacteria. J. Commun. Dis. 1989, 21, 318–322.
Yong D, Lee K, Yum J, Shin H, Rossolini G, Chong Y. Imipenem-EDTA disk method for differentiation of metallo-betalactamase- producing clinical isolates of pseudomonas spp. and Acinetobacter Spp. J ClinMicrobiol. 2002;40:3798–801. Return to ref 18 in article.
Oothuman P, Jeffery J, Aziz AH, Abu Bakar E, Jegathesan M. Bacterial pathogens isolated from cockroaches trapped from paediatric wards in peninsular Malaysia. Trans R Soc Trop Med Hyg. 1989;83:133–5.
Le Guyader A, Rivault C, Chaperon J. Microbial organisms carried by brown banded cockroaches in relation to their spatial distribution in a hospital. Epidemiol Infect. 1989;102:485–92.
Fotedar R, Shriniwas UB, Verma A. Cockroaches (Blattella germanica) as carriers of microorganisms of medical importance in hospitals. Epidemiol Infect. 1991;107:181–7.
Moges F, Eshetie S, Endris M, Huruy K, Muluye D, Feleke T, Silassie G, Ayalew F, Nagappan G. R. Cockroaches as a Source of High Bacterial Pathogens with Multidrug resistant strains in Gondar Town, Ethiopia. Biomed Res Int 2016, 2825056.
Salehzadeh A, Tavacol P, Mahjub H. Bacterial, fungal and parasitic contamination of cockroaches in public hospitals of Hamadan. Iran J Vector Borne Dis. 2007;44:105–10.
Naher A, Afroz S, Hamid S. Cockroach associated foodborne pathogens: distribution and antibiogram. Bangladesh Med Res Counc Bull. 2018;44:30–8.
Menasria T, Moussa F, El-Hamza S, Tine S, Megri R, Chenchouni H. Bacterial load of German cockroach (Blattella germanica) found in hospital environment. Pathog Glob Health. 2014;108:141–7.
Tetteh-Quarcoo PB, Donkor ES, Attah SK, Duedu KO, Afutu E, Boamah I, Olu-Taiwo M, Anim-Baidoo I, Ayeh-Kumi PF. Microbial carriage of cockroaches at a tertiary care hospital in Ghana. Environ Health Insights. 2013;7:59–66.
Mpuchane S, Matsheka I, Gashe B, Allotey J, Murindamombe G, Mrema N. Microbiological studies of cockroaches from three localities in Gaborone, Botswana. Afr J Food Agric Nutr Dev. 2006;6(2):1–17. https://doi.org/10.4314/ajfand.v6i2.71739.
Prado MA, Gir E, Pereira MS, Reis C, Pimenta FC. Profile of antimicrobial resistance of bacteria isolated from cockroaches (Periplaneta americana) in a Brazilian health care institution. Brazilian J Infect Dis. 2006;10(1):26–32.
Madebo C, Haile A, Eticha T, Solomon F. Hospital-Based Air-Borne and Surface-Borne bacterial pathogens and their antimicrobial profiles in Wolaita Sodo, Southern Ethiopia. Int J Microbiol. 2022;2022:5718341. https://doi.org/10.1155/2022/5718341.
Ageru TA, Seid H, Abiso TL, Kumalo A, Sidamo T, Balcha T. Burden of Antibiotic Resistance at Wolaita Sodo University Comprehensive Specialized Hospital. BioMed Research International 2022 | https://doi.org/10.1155/2022/7272024
Anjulo T, Seid H, Sidamo T, Balcha T, Abiso TL. Antimicrobial Resistance Profile of clinically isolated Bacteria at Wolaita Sodo University Teaching Referral Hospital. Research Square; 2021. https://doi.org/10.21203/rs.3.rs-645376/v1.
Hosu MC, Vasaikar S, Okuthe GE, Apalata T. Molecular detection of antibiotic-resistant genes in Pseudomonas aeruginosa from Nonclinical Environment: Public Health implications in Mthatha, Eastern Cape Province, South Africa. International Journal of Microbiology; Volume 2021.
Isaac C, Orue PO, Iyamu MI, Ehiaghe JI, Isaac O. Comparative analysis of pathogenic organisms in cockroaches from different community settings in Edo State, Nigeria. Korean J Parasitol. 2014;52(2):177–81.
Solomon FB, Wadilo F, Tufa EG, et al. Extended spectrum and metalo beta-lactamase producing airborne Pseudomonas aeruginosa and Acinetobacter baumanii in restricted settings of a referral hospital: a neglected condition. Antimicrob Resist Infect Control. 2017;6:106. https://doi.org/10.1186/s13756-017-0266-0.
Elshamy AA, Aboshanab KM. A review on bacterial resistance to carbapenems: epidemiology, detection and treatment options. Future Sci OA. 2020;6(3):FSO438. https://doi.org/10.2144/fsoa-2019-0098.
Puspita A, Arizandy RY, Wasito EB, Kuntaman K. The Carrier Rate of Extended Spectrum Beta lactamase (ESBL) producing Bacteria in cockroaches (Periplaneta americana) in hospital and community. Folia Med Indonesiana. 2021;57(4):283.
Adewale Elijah AdejumoAdewale Elijah AdejumoSamuel AlabiSamuel AlabiO.E, Adeleke AOE. Adeleke Adeleke. Antibiotic Resistance Profile and phenotypic detection of Beta- lactamase-producers among Gram-negative Bacteria isolated from the gut of Household cockroaches in and around University of Ibadan. Ig. J Pharm Res. 2016;12(2):117–26.
Ikechuk O, Ifeanyichukwu IR, Igwe DO, Eze UA, Ogbu O. Antibiotic resistance and Beta-lactamase genes detection among extended spectrum Beta-lactamase (ESBL)-Producing Escherichia coli and Salmonella species isolated from cockroaches (Periplaneta americana) in Abakaliki, South-East Nigeria. 2017World J Med Sci 14(4) https://doi.org/10.5829/idosi.wjms.2017.113.120
Mohammed F, AL-Marjani RA, Abdulrazaq ZA, Khadam, Reyam I, Daham, Khiaria J, Tothli. Cockroaches (Periplaneta americana): reservoirs of Metallo Β Lactamase and Extended Spectrum Β-Lactamase producing Bacteria in Medical City Hospital in Baghdad, Iraq. Pakistan J Biotechnol, 201714(3), 317–21.
Seyfi B, Hossainpour H, Kooti S, Azizi Jalilian F. Identification of Carbapenem Resistance Genes in Escherichia coli isolated from Blattella germanica by dot blot assay in Hamadan Hospitals, Iran – 2018. Iran J Med Microbiol. 2022;16(4):357–62.
Ghasemi-dehkordi P, Doosti A, Doosti E, Noshadi E. Arshi. Antimicrobial susceptibility patterns of Escherichia coli isolates from cockroaches in Southwestern Iran. Bulgarian J Veterinary Med. 2016;19(1):63–71.
Landolsi S, Selmi R, Hadjadj L, Yahia AB, Romdhane KB, Messadi L, Rolain JM. March. First Report of Extended-Spectrum β-Lactamase (blaCTX-M1) and Colistin Resistance Gene mcr-1 in E. coli of Lineage ST648 from Cockroaches in Tunisia. Public Health.1 2022.
Loucif L, Cherak Z, Chamlal N et al. First detection of VIM-2 Metallo-β-Lactamase-producing Pseudomonas putida in Blattella germanica cockroaches in an Algerian Hospital. Antimicrob Agents Chemother 2017 61(8).
Acknowledgements
We would like to thank Wolaita Sodo University for their providing lab materials and reagent. Our gratitude also go to the hospital management who cooperated to collect cockroaches. We would also like colleagues and staff who involved in laboratory analysis and write up.
Funding
There was no funding received for the fulfillment of this study.
Author information
Authors and Affiliations
Contributions
1. “FSB’ Conceived the study, study design, execution, and acquisition of data, analysis and interpretation. 2” FSB, HA, FW, KSA, FW, EGT Contributed to the design, drafted or written, or substantially revised or critically reviewed the article. 3. “FSB, HA, FW, KSA, FW, EGT Agreed on the journal to which the article will be submitted. 4. “FSB, HA, FW, KSA, FW, EGT Reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. 5. “All authors agree to take responsibility and be accountable for the contents of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study ethical approval was obtained from Wolaita Sodo University Ethical Review Board.
Competing interests
The authors declare that they have no competing interest.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bisetegn, F.S., Azene, H., Ahmed, K.S. et al. Extended spectrum and metalo beta lactamase producing gram negative bacterial pathogens from cockroaches collected at hospital, Southern Ethiopia. Antimicrob Resist Infect Control 13, 87 (2024). https://doi.org/10.1186/s13756-024-01442-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-024-01442-0