Abstract
Background
Inappropriate or overuse of antibiotic prescribing in primary care highlights an opportunity for antimicrobial stewardship (AMS) programs aimed at reducing unnecessary use of antimicrobials through education, policies and practice audits that optimize antibiotic prescribing. Evidence from the early part of the pandemic indicates a high rate of prescribing of antibiotics for patients with COVID-19. It is crucial to surveil antibiotic prescribing by primary care providers from the start of the pandemic and into its endemic stage to understand the effects of the pandemic and better target effective AMS programs.
Methods
This was a matched pair population-based cohort study that used electronic medical record (EMR) data from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN). Participants included all patients that visited their primary care provider and met the inclusion criteria for COVID-19, respiratory tract infection (RTI), or non-respiratory or influenza-like-illness (negative). Four outcomes were evaluated (a) receipt of an antibiotic prescription; (b) receipt of a non-antibiotic prescription; (c) a subsequent primary care visit (for any reason); and (d) a subsequent primary care visit with a bacterial infection diagnosis. Conditional logistic regression was used to evaluate the association between COVID-19 and each of the four outcomes. Each model was adjusted for location (rural or urban), material and social deprivation, smoking status, alcohol use, obesity, pregnancy, HIV, cancer and number of chronic conditions.
Results
The odds of a COVID-19 patient receiving an antibiotic within 30 days of their visit is much lower than for patients visiting for RTI or for a non-respiratory or influenza-like-illnesses (AOR = 0.08, 95% CI[0.07, 0.09] compared to RTI, and AOR = 0.43, 95% CI[0.38, 0.48] compared to negatives). It was found that a patient visit for COVID-19 was much less likely to have a subsequent visit for a bacterial infection at all time points.
Conclusions
Encouragingly, COVID-19 patients were much less likely to receive an antibiotic prescription than patients with an RTI. However, this highlights an opportunity to leverage the education and attitude change brought about by the public health messaging during the COVID-19 pandemic (that antibiotics cannot treat a viral infection), to reduce the prescribing of antibiotics for other viral RTIs and improve antibiotic stewardship.
Similar content being viewed by others
Background
The value of antimicrobial therapies is threatened by the growth and spread of antibiotic resistant bacteria, in part, due to the inappropriate/overuse of antibiotics [1]. In Canada, and throughout most developed countries, the majority of antibiotics are prescribed in the community. As such, it is essential to understand antibiotic prescribing practices in the primary care setting [2,3,4].
Several Canadian studies have shown that there is significant opportunity to reduce potentially inappropriate antibiotic prescribing in primary care [4,5,6,7,8]. A 2019 study using Canadian electronic medical record (EMR) data found significant variation in the proportion of acute respiratory tract infections (RTI) treated with antibiotics, with the top quartile of prescribers treating the common cold with an antibiotic more than half the time [5].
Inappropriate or overuse of antibiotic prescribing in primary care highlights an opportunity for antimicrobial stewardship (AMS) programs aimed at reducing unnecessary use of antimicrobials through education, policies and practice audits that optimize antibiotic prescribing [9, 10]. Prior to the onset of the COVID-19 pandemic, antibiotic prescribing rates in the community were stable. A report from the Public Health Agency of Canada described that between 2014 and 2018 antibiotic prescribing by family physicians and general practitioners only dropped by 3%, from 428.3 to 416.2 prescriptions per 1000 inhabitants [4]. However, the spread of the COVID-19 virus in early 2020 led to unprecedented changes in not only the delivery of healthcare but also in the transmission of communicable pathogens [11, 12]. Antibiotic prescribing in primary care during the pandemic significantly decreased, most notably for respiratory tract infections [12,13,14,15,16,17].
With the emergence of a novel virus, it is hypothesized that this inappropriate prescribing would also be seen amongst patients with COVID-19. Evidence from the early part of the pandemic indicates a high rate of prescribing of antibiotics for patients with COVID-19 [18]. However, it is unclear if this inappropriate prescribing was sustained. As such, it is crucial to surveil antibiotic prescribing by primary care practitioners from the start of the pandemic and into its endemic stage to understand the effects of the pandemic and better target effective AMS programs.
The objective of this study was to compare antibiotic prescribing and healthcare utilization between COVID-19 positive patients to those with a) respiratory tract infection (RTI); and b) COVID-19 negative patients.
Methods
Data source and study design
This was a matched pair population-based cohort study that used electronic medical record (EMR) data from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN). CPCSSN is a federated network of fourteen practice-based research and learning networks (PBRLN) across Canada. Primary care providers, known as sentinels, share clinical data on their patients with CPCSSN to form a national data repository of patient clinical records. The CPCSSN repository has data on over 1.8 million patients, contributed by over 1,500 primary care providers from British Columbia, Alberta, Manitoba, Ontario, Quebec, Nova Scotia and Newfoundland. While patients represented within this pan-Canadian data repository are older and have more females than the overall Canadian population, the data repository is representative of Canadians who visit primary care [19].
This study excluded clinical data from Manitoba and Quebec as we were unable to classify COVID-19 cases in the data from these two PBLRNs. In these two provinces the lab results confirming a COVID-19 infection were recorded almost exclusively as PDF documents, which are not available (at this time) within the CPCSSN database.
Participants
Participants included all patients that visited their primary care provider and met the inclusion criteria for COVID-19, RTI, or negative (see Additional file 1 for case definitions). To be included a patient had to have a documented birthyear and sex.
COVID-19 encounter
A patient’s visit was included as a COVID-19 primary care visit if there was a diagnosis and/or lab-confirmation of the COVID-19 virus during a primary care visit between April 2020 and December 2021. A patient could only be included as a COVID-19 visit once (incident case = index event).
RTI encounter
A patient’s visit was included as an RTI primary care visit if they had a diagnosis of RTI during a primary care visit between April 2020 and December 2021. Encounters were only included if there was no mention of COVID-19 in any record associated with the encounter date.
Negative encounter
A patient’s visit was included as a ‘negative’ primary care visit if they had a visit with no diagnostic or lab data corresponding to a condition with respiratory symptoms (see Additional file 1 for list of exclusion criteria). Encounters were only included if there was no mention of COVID-19 in any record associated with the encounter date.
Each group was mutually exclusive. Other than the COVID-19 visit group, a patient visit was eligible to be included once every six months. A patient visit (for RTI or negative) within six months of a previous visit (for RTI or negative, respectively) were not eligible for inclusion as the outcome was evaluated up to 180 days after the index event.
We also calculated the proportion of visits that had COVID-19 documentation within the EMR out of all visits during the study time period.
Outcome
Four outcomes were evaluated at four follow up intervals (30 days, 60 days, 90 days, and 180 days): (a) receipt of an antibiotic prescription; (b) receipt of a non-antibiotic prescription; (c) a subsequent primary care visit (for any reason); and (d) a subsequent primary care visit with a bacterial infection diagnosis (see Additional file 2 for a full description of how each outcome was defined).
Matching
In order to compare the COVID-19 visits with each of the comparison groups the COVID-19 subjects were matched (1:1) to an RTI visit and a negative visit on the following covariates: index month (month of diagnosis), age group (0–18, 19–39, 40–64, 65 +), sex (male, female), and province (British Columbia, Alberta, Ontario, Nova Scotia, and Newfoundland).
Covariates
Patient age was determined at time of the index visit. Rural or urban patient locations were determined based on the second digit of the postal code, which indicates whether the patient lives in an urban (1–9) or rural area (0), as defined by Canada Post delivery areas. If a patient was missing a postal code their rural urban status was classified using the postal code of the clinic.
A material and social deprivation index (Pampolon), derived from a linkage between postal code and census data, was used as a proxy for socioeconomic status [20]. Measures of material and social deprivation were derived from the postal code using the Statistics Canada Postal Code Conversion File, along with the material and social deprivation index [20]. This index uses socioeconomic indicators from the census, including education, employment, and income (the material component), as well as marital status and family structure (the social component), to assign scores to dissemination areas (DA) in the form of population quintiles. Mean imputation was used to compute a material or social deprivation score for patients that were missing this covariate.
CPCSSN validated case definitions were used to classify a patient’s comorbidity status, specifically for the following conditions: chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), dementia, depression, diabetes, epilepsy, hypertension, osteoarthritis, Parkinson’s disease, dyslipidemia, and asthma [21,22,23,24]. A patient was classified as obese if there was a recorded BMI observation ≥ 30 kg/m2.
A patient was classified as a smoker, non-smoker, past smoker or unknown based on smoking risk factor records. Similarly, alcohol use was classified as yes, no, or unknown based on alcohol risk factor records.
A patient was classified as pregnant, HIV positive, or has cancer if they had an associated ICD-9 code during the study period (March 2020 to December 2022). The ICD-9 codes used to classify patients for each of these covariates are described in Additional file 2.
Analysis
Conditional logistic regression, a specialized type of regression appropriate for individually matched case–control data, was used to evaluate the association between COVID-19 and each of the four outcomes. Each model was adjusted for location (rural or urban), material and social deprivation, smoking status, alcohol use, obesity, pregnancy, HIV, cancer and number of chronic conditions. As this was an exploratory analysis and there were no a priori hypotheses, all covariates were kept in the fully adjusted model.
The data analyses were completed using SAS© 9.4.
Results
Between April 1st, 2020, and December 31st, 2021, there were 855,434 patients that had at least one visit with a participating primary care provider. Of these patients, there were 19,890 that visited their primary care provider for a COVID-19 infection during the study period. 1.57% of all patient visits had documentation of COVID-19. In comparison to patients visiting primary care for other reasons, COVID-19 patients were significantly more likely to be younger (34.7% of COVID-19 patients were young adults 19–39 years, compared to 23.3% of all other patients), more urban (90.5% compared to 82.5%) and have less comorbidities (56.8% have ≥ 1 comorbidity compared to 64.2%) (Table 1). Of the 19,890 COVID-19 visits 19,020 were matched to an RTI visit, and all 19,890 were matched to a negative visit. 17.5% of patients were missing a social and material index and were assigned a value using mean imputation. Table 2 compares the demographic and clinical characteristics of the COVID-19 group to each matched control group.
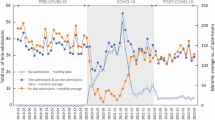
The unadjusted and adjusted odds ratios for each outcome are displayed in Table 3. Figure 1 exhibits the results of the conditional logistic regression analysis for receipt of an antibiotic prescription within 30 days, 60 days, 90 days, and 180 days of the index event. The adjusted odds of a COVID-19 patient receiving an antibiotic within 30 days of their visit is much lower than for patients visiting for RTI or for a non-respiratory or influenza-like-illnesses (AOR = 0.09, 95% CI[0.07,0.09] compared to RTI, and AOR = 0.43, 95% CI[0.38, 0.48] compared to negatives). This remained true across all time periods (Fig. 1).
The conditional logistic regression analysis for receipt of a non-antibiotic prescription in the days following a visit revealed that a patient encounter with a COVID-19 code was much less likely to receive a prescription than a patient visit for RTI or a patient visit unrelated to respiratory or influenza-like illness (negative) (Fig. 2).
The third outcome evaluated using conditional logistic regression was a subsequent primary care visit and it was found that a patient presenting with COVID-19 was much more likely to have a subsequent visit within 30 days compared to a patient visiting for RTI (AOR = 1.61, 95% CI[1.53, 1.68], or a non-respiratory or non-influenza like-illness (AOR = 1.52, 95% CI[1.45, 1.58]) (Fig. 3). This increased likelihood remained true at 60 days (AOR = 1.33, 95% CI[1.27, 1.40] compared to RTI, and AOR = 1.35, 95% CI[1.29, 1.40] compared to negative), but by 180 days after the index visit patients with COVID-19 were as likely to have a subsequent visit as patients with RTI (90 day AOR = 1.17, 95% CI[1.14, 1.23], 180 day AOR = 0.96, 95% CI[0.91, 1.01]) or negative (90 day AOR = 1.23, 95% CI[1.18, 1.29], 180 day AOR = 0.99, 95% CI[0.94, 1.04].
Lastly, we evaluated the likelihood of a subsequent visit for a bacterial infection (Fig. 4). It was found that a patient visit for COVID-19 was much less likely to have a subsequent visit for a bacterial infection at all time points, in comparison to patients visiting for RTI (30 day AOR = 0.07, 95% CI[0.06, 0.07], 60 day AOR = 0.08, 95% CI[0.07,0.09], 90 day AOR = 0.09, 95% CI[0.08, 0.10], 180 day AOR = 0.11, 95% CI[0.10, 0.11]).
Discussion
Overall, in the first year and a half of the pandemic, there were a low number of primary care visits where COVID-19 was documented (1.57%). This low number of COVID-19 visits suggests that most patients with COVID-19 infections were either not seeking healthcare (mild cases) or potentially seeking healthcare at alternate settings such as COVID-19 assessment centres or emergency rooms (severe cases).
Similar to past work, we found patients that did visit primary care with a COVID-19 infection were much less likely to receive an antibiotic prescription. Two studies using Canadian pharmacy data also found that there has been an overall significant reduction in total outpatient antibiotic prescriptions issued during the COVID-19 pandemic [12, 24]. Integrating the results from the pharmacy data with the results from this study suggests that the reduction may be due to a change in the amount of circulating respiratory tract viruses, rather than a change in the propensity to prescribe for a respiratory virus. In addition, research shows that public messaging and social media has a significant influence on patient behaviour, such as medication seeking [25]. It is possible that the reduction in overall antibiotic prescribing was also due to effective public health awareness campaigns that antibiotics are not useful to treat viral infections like COVID-19. Nonetheless, these findings emphasize that there is room for improvement in reducing potentially inappropriate antibiotic prescribing for non-COVID-19 RTIs.
The observation that COVID-19 patients are more likely to have a subsequent visit within 60 days of their index event compared to RTI or negative patients may be due to the uncertainty and fear around the outcomes of a COVID-19 infection during the first 18 months of the pandemic, or that patients presenting to primary care with COVID-19 represent more severe or lingering cases that require a higher level of primary care compared to those that do not seek medical attention.
The finding that a patient with a COVID-19 visit is less likely to receive a non-antibiotic prescription than patient encounters for RTI or negative may reflect how the use of primary care visits changed due to the pandemic, with patients combining multiple needs into one visit because of public health measures and reduced access to primary care. A recent study evaluating reasons for primary care visits during the pandemic found that there was an increase in visits for anxiety but a decrease in visits for preventive care and chronic disease [26]. Patient encounters for RTI or non-respiratory illness (negative) during the COVID-19 pandemic may be more likely to be combining multiple health concerns into one appointment than encounters for COVID-19.
Reassuringly, this study reveals that patients presenting with COVID-19 are much less likely to have record of a subsequent bacterial infection in the 180 days following their COVID-19 visit, compared to RTI patients. In contrast, COVID-19 patients were as likely to have record of a bacterial infection within 30 days of their index event compared to patients visiting for a non-respiratory illness or health concern, and more likely to have record of a bacterial infection between 60 to 180 days following their COVID-19 visit compared to patients visiting for a non-respiratory illness or health concern. These findings suggest that in comparison to other respiratory viruses the COVID-19 virus does not increase a patient’s vulnerability to a bacterial infection, and COVID-19 patients are like other primary care patients seeking care for non-respiratory illness concerns.
Limitations
There are several limitations to this study. First, the EMR data used in this study were collected for clinical and administrative purposes and may result in incomplete capture of information. Second, the clinical context for some of the diagnoses and outcomes evaluated in this study can be difficult to infer from secondary use of EMR data. Third, there is likely some misclassification as the ability to identify patients with COVID-19 during the first 18 months of the pandemic is dictated by testing procedures in each jurisdiction.
It is likely that some patients within the matched groups (RTI and negative) had COVID-19 infections during the study period but it was not indicated in the EMR of that patient. Furthermore, documentation patterns at the onset of the pandemic were variable and could lead to some misclassification. This may be particularly true for RTI encounters as it is uncertain how providers were documenting RTI during the initial years of the COVID-19 pandemic. However, attempts were made to minimize this misclassification by only including RTI encounters if there was no mention of COVID-19 in any records associated with that encounter date. There were also variable treatment protocols over the course of the early stages of the pandemic and this study is not able to account for different regimens at different institutions.
Neighborhood-level indicators of socioeconomic status were used, and this could also contribute to some misclassification.
Conclusion
This study evaluated the primary healthcare services provided to patients with documented COVID-19 in comparison to patients presenting with RTI and non-respiratory conditions. Encouragingly, COVID-19 patients were much less likely to receive an antibiotic prescription than patients with an RTI. However, this highlights an opportunity to leverage the education and attitude change brought about by the public health messaging during the COVID-19 pandemic (that antibiotics cannot treat a viral infection), to reduce the prescribing of antibiotics for other viral RTIs and improve antibiotic stewardship. This has a direct impact on patient outcomes by reducing morbidity and mortality from antimicrobial resistant infections [9, 27].
Availability of data and materials
The data used in this work was from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN). It can be accessed via their website www.cpcssn.org.
Abbreviations
- AMS:
-
Antimicrobial Stewardship
- ATC:
-
Anatomical Therapeutic Classification
- CKD:
-
Chronic Kidney Disease
- COPD:
-
Chronic Obstructive Pulmonary Disease
- CPCSSN:
-
Canadian Primary Care Sentinel Surveillance Network
- DA:
-
Dissemination Area
- EMR:
-
Electronic Medical Record
- ICD-9:
-
International Classification of Diseases – 9th version
- AOR:
-
Adjusted Odds Ratio
- PBLRN:
-
Practice Based Research and Learning Network
- RTI:
-
Respiratory Tract Infection
References
Cecchini M, Langer J, Slawomirski L. Antimicrobial Resistance in G7 Countries and Beyond: Economic issues, Policies and Options for Action. Germany: OECD; 2015.
Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128(6):1053–61.
Leis JA, Born KB, Ostrow O, Moser A, Grill A. Prescriber-led practice changes that can bolster antimicrobial stewardship in community health care settings. Can Commun Dis Resp. 2020;46(1):1–5.
Public Health Agency of Canada. Canadian Antimicrobial Resistance Surveillance System Report Update 2020. 2020. https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2020-report.html. Accessed 12 Sept 2023.
Wong S, Rajapakshe S, Barber D, Patey A, Levinson W, Morkem R, Hurwitz G, Wintermute K, Leis JA. Antibiotic prescribing for respiratory tract infection across a national primary care network in 2019. Can Commun Dis Resp. 2022;48(4):157.
Kitano T, Langford BJ, Brown KA, Pang A, Chen B, Garber G, Daneman N, et al. The association between high and unnecessary antibiotic prescribing: a cohort study using family physician electronic medical records. Clin Infect Dis. 2021;72(9):345-e351.
Silverman M, Povitz M, Sontrop JM, Li L, Richard L, Cejic S, Shariff SZ. Antibiotic prescribing for nonbacterial acute upper respiratory infections in elderly persons. Ann Intern Med. 2017;66(11):765–74.
Schwartz KL, Langford BJ, Daneman N, Chen B, Brown KA, McIsaac W, et al. Unecessary antibiotic prescribing in a Canadian primary care setting: a descriptive analysis using routinely colleted electronic medical record data. CMAJ Open. 2020;8:E360–9.
Brown KA, Khanafer N, Daneman N, Fisman DN. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother. 2013;57:2326e32.
Feazel LM, Malhotra A, Perencevich EN, Kaboli P, Diekema DJ, Schweizer ML. Effect of antibiotic stewardship programmes on Clostridium difficile incidence: a systematic review and meta-analysis. J Antimicrob Chemother. 2014;69(7):1748–54. https://doi.org/10.1093/jac/dku046.
Glass RJ, Glass LM, Beyeler WE, Min HJ. Targeted social distancing design for pandemic influenza. Emerg Infect Dis. 2006;12:1671–81.
Knight BD, Shurgold J, Smith G, MacFadden DR, Schwartz KL, Daneman N, Gravel Topper D, Brooks J. Impact of COVID-19 on community antibiotic use in Canada: an ecological study. Clin Microbiol Infect. 2022;28:426–32.
Weill A, Drouin J, Desplas D, Cuenot F, Spira RD, Zureik M. Outpatient use of drugs in France during the COVID-19 epidemic—patients and providers characteristics and impact of the COVID-19 pandemic. Antibiotics (Basel). 2022;11(5):643.
Sluggett JK, Dinh YH, Wesselingh SL, Inacio MC, Caughey GE. National changes in outpatient systemic antibiotic use during the coronavirus disease 2019 pandemic in Australia. Clin Infect Dis. 2021;73:2150–2.
Hussain AZ, Paudyal V, Hadi MA. Impact of the COVID-19 pandemic on the prescribing patterns of first-line antibiotics in english primary care: a longitudinal analysis of national prescribing dataset. Antibiotics. 2021;10:591.
King LM, Lovegrove MC, Shehab N, Tsay S, Budnitz DS, Geller AI, et al. Trends in U.S. outpatient antibiotic prescriptions during the COVID-19 pandemic. Clin Infect Dis. 2021;73:e652e60.
Zhu N, Aylin P, Rawson T, Gilchrist M, Majeed A, Holmes A. Investigating the impact of COVID-19 on primary care antibiotic prescribing in North West London across two epidemic waves. Clin Microbiol Infect. 2021;27:762e8.
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, Soucy JPR, Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26(10):1622–9.
Queenan J, Williamson T, Khan S, Drummond N, Garies S, Morkem R, Birtwhistle R. Representativeness of patients and providers in the Canadian Primary Care Sentinel Surveillance Network: a cross-sectional study. CMAJ Open. 2016;4(1):E28–32.
Gamache P., Hamel D., Blaser C. Material and social deprivation index: a summary –INSPQ. 2020. www.inspq.qc.ca/en/publications/2639.
Williamson T, Green ME, Birtwhistle R, et al. Validating the 8 CPCSSN case definitions for chronic disease surveillance in a primary care database of electronic health records. Ann Fam Med. 2014;12(4):367–72.
Vijh R, Wong S, Grandy M, Peterson S, Ezzat A, Gibb AG, Hawkins NM. Identifying health failure in patients with chronic obstructive lung disease through the Canadian Primary Care Sentinel Surveillance Network in British Columbia: a case derivation study. CMAJ Open. 2021;9(2):E376–83.
Cave AJ, Davey C, Ahmadi E, Drummond N, Fuentes S, Kazemi-Bajestani SMR, Sharpe H, Tayler M. Development of a validated algorithm for the diagnosis of paediatric asthma in electronic medical records. NPJ Prim Care Respir. 2016;26:16085.
Kitano T, Brown KA, Daneman N, MacFadden DR, Langford BJ, Leung V, So M, Leung E, Burrows L, Manuel D, Bowdish DME, Maxwell CJ, Bronskill SE, Brooks JI, Schwartz KL. The impact of COVID-19 on outpatient antibiotic prescriptions in Ontario, Canada; an interrupted time series analysis. Open Forum Infect Dis. 2021;8(11):ofab533. https://doi.org/10.1093/ofid/ofab533. PMID: 34805442; PMCID: PMC8601042.
Schellack N, Strydom M, Pepper MS, Herd CL, Hendricks CL, Bronkhorst E, Meyer JC, et al. Social media and COVID-19 – perceptions and public deceptions of ivermectin, colchicine and hydroxychloroquine: lessons for future pandemics. Antibiotics (Basel). 2022;11(4):445.
Stephenson E, Butt DA, Gronsbell J, Ji C, O’Neill B, Crampton N, Tu K. Changes in the top 25 reasons for primary care visits during the COVID-19 pandemic in a high-COVID region of Canada. PLoS One. 2021;16(8):e0255992.
MacFadden DR, Fisman DN, Hanage WP, Lipsitch M. The relative impact of community and hospital antibiotic use on the selection of extended spectrum beta-lactamase-producing Escherichia coli. Clin Infect Dis. 2019;69:182e8.
Acknowledgements
Not applicable.
Funding
This study was funded by the Public Health Agency of Canada (PHAC).
Author information
Authors and Affiliations
Contributions
GS and BK conceived of the study. GS, BK and RM developed the methods. DB and STW supervised and oversaw the work. RM conducted the analysis and wrote the first draft of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has received approval from the Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (FMED-6785–21) and adheres to all relevant guidelines and regulations for research involving de-identified health data (Tri-Council Policy Statements on the Ethical Conduct for Research Involving Humans [TCPS2]).
Any data included in the CPCSSN database was obtained under ethics approval, including waivers of individual patient informed consent for their de-identified data to be used for surveillance and research purposes, from each Practice Based Research and Learning Network’s local Research Ethics Board (University of British Columbia, University of Alberta, University of Calgary, University of Manitoba, University of Western Ontario, University of Toronto, Queen’s University, University of Ottawa, Bruyère Research Institute, and Memorial University of Newfoundland).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Morkem, R., Smith, G., Knight, B. et al. Understanding the impact of COVID-19 on antibiotic use in Canadian primary care: a matched-cohort study using EMR data. Antimicrob Resist Infect Control 13, 76 (2024). https://doi.org/10.1186/s13756-024-01434-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-024-01434-0