Abstract
Background
Carbapenem-resistant Pseudomonas aeruginosa (CRPA) are a serious cause of healthcare-associated infections. Part of the infection prevention and control measures are outbreak investigations (OI) of patients, healthcare workers (HCW), and the environment after identifying a CRPA in order to identify carriers and environmental reservoirs, so that targeted actions can be taken to prevent further transmission. However, little is known on when and how to perform such OI. Therefore, this systematic review aims to summarize OI performed after detection of CRPA in the endemic and epidemic hospital setting.
Main text
Articles related to our research question were identified through a literature research in multiple databases (Embase, Medline Ovid, Cochrane, Scopus, Cinahl, Web of Science, and Google Scholar) until January 12, 2022 (Prospero registration number CRD42020194165). Hundred-twenty-six studies were included. In both the endemic and the epidemic setting, a median number of two out of seven predefined components of OI were identified. In the endemic setting, the most frequent component of OI was screening of the environment (28 studies, 62.2%). In the epidemic setting, screening of the environment (72 studies, 88.9%), and screening of patients during hospitalization (30 studies, 37%) were most frequently performed. Only 19 out of 126 studies (15.1%) reported screening of contact patients, and 37 studies reported screening of healthcare workers (HCW, 29.4%).
Conclusion
Due to probable underreporting of OI in the literature, the available evidence for the usefulness of the individual components of OI is scarce. This could lead to inhomogeneous performance of OI after detection of CRPA in the healthcare setting, and with this, potential under- or overscreening. While we could show evidence for the usefulness for environmental screening in order to identify the mode of transmission, evidence for HCW screening is scarce and might not lead to the identification of modes of transmission. Further studies are needed to better understand CI in different settings and, finally, develop guidance on when and how to best perform OI.
Similar content being viewed by others
Background
Pseudomonas aeruginosa is a well-known microorganism causing healthcare-associated infections (HAI), especially in immunocompromised patients or patients admitted to the intensive care unit (ICU) [1, 2]. The prevalence of multidrug-resistant (MDR) strains of P. aeruginosa was reported to be approximately 15% in the Unites States of America [3] and 17.2% in the European Union [4], but varies widely across and within countries and continents [5]. P. aeruginosa infections increased over the last two decades [5, 6], including bacteraemia and pneumonia, leading to high morbidity and mortality [7], and infections with MDR P. aeruginosa were no exception [8]. Carbapenem-resistant P. aeruginosa (CRPA) infections are of particular concern, since antimicrobial treatment of these bacteria is difficult [9], and mortality rates for bacteraemia are high (i.e. estimates between 30 and 70%) [7, 8, 10].
When a patient is unexpectedly identified with CRPA, infection prevention and control (IPC) measures should be taken. Especially in cases where contact precautions were not applied, an outbreak investigation (OI) as part of the IPC measures is a common approach to identify carriers and environmental reservoirs to stop further transmission. A OI may comprise several components, but usually contains the identification and screening of contact patients, as well as screening of the environment to identify environmental niches. Sometimes, screening of healthcare workers (HCW) is performed as well. OI are not well defined in the literature, except for tuberculosis [11], and more recently for COVID-19 [12]. In the review by Tomczyz et al. [13], the impact of practices to prevent and control CRPA were assessed, but not the impact of OI. Additionally, in 2014, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) released guidelines containing IPC measures meant to reduce transmission of MDR Gram-negative bacteria in hospitalized patients [14]. However, the guidelines do not give any recommendation regarding OI in either endemic or epidemic situations (Additional file 1: Table S1) but instead, specifically mention that there is no consensus on the role of screening to identify carriers. However, various screening strategies are used for carbapenem-resistant Gram-negatives, mostly in outbreak settings, as recently presented by Verdugo-Paiva et al. [15]. In addition, the guidelines recommend environmental cleaning and disinfection, nevertheless, no recommendation is made regarding screening of the environment to identify potential sources.
The routes of transmission of P. aeruginosa in the hospital setting often remain unknown [16], but several modes of transmission have been described in the literature, including hands of HCW [17], contaminated medical devices and supplies [18], and water-related devices [19]. These modes of transmission have been identified with rigorous OI using clinical, microbiological, and genotyping data. Nevertheless, there is little information available on if, when, and how a OI of patients, the environment, and HCW should be performed. Therefore, the aim of this systematic review is to give an overview of the strategies used for OI described in the literature, and their contribution to identify a source and/or contain the outbreak after detection of CRPA.
Methods
This systematic review followed the guidelines presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [20]. The PRISMA 2020 checklist is available in Additional file 1: document 1. Additionally, the protocol of the study is registered in the PROSPERO international prospective register of systematic reviews (CRD42020194165, Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020194165).
Study selection
Articles related to our research question were identified through a literature research in Embase, Medline Ovid, Cochrane, Scopus, Cinahl, Web of Science, and Google Scholar (initial search until 10 June 2020, updated search performed on 12 January 2022). The search was not limited by language, date of publication, country of publication, or study design (Additional file 1: document 2).
Studies were included based on title and abstract if conducted in a hospital setting or long-term care facility (LTCF), and (1) reporting hospital or LTCF outbreaks involving CRPA, or (2) published case reports about CRPA. The specific inclusion criteria for the full-text selection was that the article should report on OI regarding CRPA. We excluded studies related to non-human infections, reviews, conference abstracts [21], and studies with missing information about OI after contacting the corresponding author. First, titles and abstracts of all retrieved citations were screened independently by ACB and SNS. After this screening, ACB and SNS performed a second screening based on the full-text. Disagreements were resolved by discussion with a third researcher (AFV) if necessary. We excluded duplicate publications. If several studies were published from the same author/institution during overlapping periods, we contacted the author/institution to avoid including duplicates. Reference lists of relevant reviews, which were identified during the literature research, were screened to identify additional studies that had been missed by our search strategy.
Definitions and data extraction
Seven components of OI were predefined: (1) identification of contact patients (i.e. the exact definition of them), (2) screening of contact patients (i.e. the actually screened patients), (3) screening on admission, (4) screening during hospitalization, (5) screening of HCW, (6) screening of the environment (wet/dry), and (7) others.
A data extraction file was created, and the following data were extracted by ACB and SNS: first author, journal, year of publication, study site and location, type of hospital/healthcare setting, start and end date of the study, characteristics of the study, population (age, sex), number of patients with confirmed CRPA infection or colonization, number of patients selected for screening, criteria on which their selection was based, number of patients eventually screened and the results, number of HCW screened including screening sites and results, details of environment screening (e.g. number, location), number of performed components within a strategy, quality of the OI, and identification of the source and containment of the outbreak. In addition, we also extracted clinical outcomes, culture methods, and all molecular data if available. The data extraction file was sent to the corresponding authors of the included studies to verify the extracted data, and a request to provide missing data if applicable. In case we did not receive any response after the given deadline (i.e. 2 weeks), a reminder was sent. If no response was received and crucial information was missing, the study was excluded.
Data analysis
Characteristics of the studies were collected in Excel. We conducted a qualitative synthesis of the OI components after detection of a CRPA. We stratified data by endemic/epidemic (as described by the authors of the included articles) setting, hospital type, and high/low prevalence of CRPA for studies conducted in Europe. Low and high prevalence was based on the EARS-Net data of CRPA from 2020, with low prevalence defined as < 10%, and high prevalence as ≥ 10% [22]. Continuous variables were analysed by median with range, or mean with standard deviation; categorical variables were analysed using percentages, or a median with range if applicable. P values were calculated using the chi-square or the independent sample median test. P values were only calculated if there was an expected count of more than five. All analyses were performed with IBM SPSS Statistics (Version 28.0.1.0).
Study quality
Pre-specified quality assessment checklists according to the type of study were used to assess the risk of bias of the individual studies. ACB performed the quality assessments. The methodological quality was assessed for all included studies using the strengthening reporting of observational studies in epidemiology (STROBE) guideline [23], the guidelines for transparent reporting of outbreak reports and intervention studies of nosocomial infection (ORION) [24], or the consensus-based clinical case reporting (CARE) guideline [25] depending on the study design. The study quality was defined using the following threshold scores: STROBE (high 23–33 points, medium 12–22 points, and low 0–11 points), ORION (high 25–52 points, medium 18–34 points, and low 0–17 points), CARE (high 21–30 points, medium 11–20 points, and low 0–10 points). The classification was based on the achieved points of the maximum score possible, divided in thirds.
Results
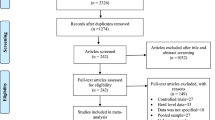
The literature search was performed on 12 January 2022 (Fig. 1). The search identified 3599 non-duplicate articles, and 111 additional articles were identified after searching the references list of reviews of interest. After the abstract selection, 712 articles were potentially relevant for this study. Full texts of these 712 articles were screened (56 full texts not retrieved), which resulted in 130 studies included of which data were extracted and forms sent to the authors (Fig. 1). The corresponding authors of 47 studies (36.2%) responded to our request to provide feedback on the extracted data. After review by the authors, four studies had to be excluded additionally, resulting in a total of 126 studies included (Fig. 1).
Study characteristics
The included 126 studies were published between 1989 and 2021 (Additional file 1: Figure 1). Fifty-nine studies (46.8%) were conducted in Europe. The three most common countries of origin were France (n = 15, 11.9%), Germany (n = 11, 8.7%), and the Unites States (n = 10, 7.9%). Ninety-three of the studies were conducted at a tertiary care centre (73.8%), and two at a primary care centre, a secondary care centre, and in LTCF (1.6%). One study was from a rehabilitation centre. The precise setting was not described in 26 studies (20.6%), but all of them were performed in the hospital setting. Data on the number of beds was available for 75 studies (59.5%), resulting in a median of 925 beds per hospital (range 26–2974). Sixty-five outbreak descriptions (51.6%), 48 cohort studies (38.1%), six case–control studies (4.8%), three cross-sectional studies (2.4%), three case reports (2.4%), and one before-after study (0.8%) were included. Eighty-one studies were conducted in an epidemic setting (64.3%), while 47 were conducted in an endemic setting (37.3%) for CRPA as defined by the authors of the respective study. Four of the studies conducted in the endemic setting provided information about outbreaks during the study period and were therefore analysed in the epidemic group [26,27,28,29]. For one study, the setting was not described [30]. The median study size was 36 patients, ranging from 1 to 7071 patients. One study did not provide information on the study size [31]. Information about patients’ characteristics was fully available in 123 studies (97.6%): 114 studies provided information about adult patients (90.5%) and 24 studies about paediatric patients (19.0%, paediatric patients only: N = 9, 7.1%). ICU patients were included in 77 studies (61.1%), burn unit patients in 13 studies (10.3%, burn unit patients only: N = 5, 4.0%), cystic fibrosis (CF) patients in six studies (4.8%), paediatric ICU (PICU) patients in 10 studies (7.9%), and neonatal ICU (NICU) patients in seven studies (5.6%). The study duration was available for 117 (92.9%) of the studies providing a median of 17 months (SD ± 29.6 months). The characteristics of the included studies are available in Additional file 1: Table S2.
Outbreak investigation components performed after identifying CRPA
In both the endemic and the epidemic setting, a median number of two out of seven predefined components of OI were identified (range 1–5, Table 1). The most common components in the endemic setting were screening of the environment in 62.2%, and screening of patients on admission and during the hospitalization in 46.7% and 46.7%, respectively. Identification and screening of contact patients was only described in less than 10% of the studies. In contrast, in the epidemic setting screening of the environment was more common (88.9%) as well as identifying (22.2%) and screening (19.8%) of contact patients than in the endemic setting. Nevertheless, patients’ screening on admission or during hospitalization was lower with 16.0% and 37.0%, respectively.
Screening of contact patients
Nineteen out of 126 studies reported screening of contact patients. In these 19 studies, screening was performed for the following patients: patients who had contact with the patient identified with CRPA (n = 2), roommates of the CRPA positive patient (n = 3), patients admitted to the same ward at the same time as the CRPA positive patient (n = 9), patients hospitalized in the same clinic as the CRPA positive patient (n = 1), all hospitalized patients at a certain time point (n = 1), concomitantly admitted patients (n = 1), or patients undergoing the same procedure (n = 1). In one study, screening of relatives of the CRPA-positive patient was performed in addition [32]. The information was not available for two studies (10.5%). Only four out of 19 studies reported the outcome of the screening of contact patients: one found additional cases in 17.4% (15 out of 86 contact patients) [33], and the others found no additional cases [34,35,36] while screening 11 contact patients, 111 swabs of 52 contact patients, and 55 contact patients, respectively. Approaching contact patients after discharge was not described in any of the studies.
Screening of HCW
Screening of HCW was performed in 37 (29.4%) of the studies, describing the screening of a median of 28.5 HCW per OI (range 5–120). In the majority of the studies (32; 86.5%), hands were cultured. No positive CRPA screenings were reported in 22 out of 37 studies (59.5%). Seven studies (18.9%) reported positive CRPA screenings of HCW with a range of one to 34 HCW per OI. In eight studies (21.6%), no results of the performed screening was reported. In 23 studies (62.2%) it was described that the isolates identified in HCW was non-identical to the isolate of the index patient, and eight studies (21.6%) reported identical isolates with a range of one to 27 identical isolates per OI. However, often it was not described how many HCW were screened and how many were identified with CRPA. In six studies (16.2%), no comparison of isolates was reported. Details of the HCW screening can be found in Additional file 1: Table S4.
Screening of the environment
Overall, the environment was screened in 100 studies (79.4%); 53 (42.1%) screened the dry environment (e.g. surfaces, floors, equipment), and 93 (73.8%) screened the wet environment (e.g. water, sinks, showers, endoscopes, liquids). The quality of the reported results of the environmental screenings did not allow further analysis.
Contribution of outbreak investigations to identify a source and contain the outbreak
In the epidemic setting, we analysed additional measures contributing to the containment of the outbreaks (Table 2). The most common measure was the construction of an epidemiological timeline in 64.2% of the studies, and a retrospective laboratory review to identify additional cases in 42.0%. In 61.7% of the studies, the source of the outbreak was identified, and in 81.5% the outbreak was contained. In all but three studies [35, 37, 38], contaminated environment was described as the primary source. The availability of an outbreak protocol was not described in any of the studies.
Comparison of European studies by prevalence of the countries
Fifty-two (41.3%) out of the 126 reports were from Europe, and of these, 44 (84.6%) were from countries considered as low prevalence country, while 8 (15.4%) were classified as high prevalence. The median number of applied components of OI was similar in high prevalence countries compared to low prevalence countries (Table 1). However, the identification (25% vs. 20.5%) and screening (25% vs. 18.2%) of contact patients was performed more frequently, but not the screening on admission (12.5% vs. 34.1%). On the other hand, OI of the environment were performed more frequently in high prevalence countries (87.5% vs. 75%), especially of the wet environment (87.5% vs. 70.5%).
Study quality assessment
In the endemic setting, the quality assessment of the 45 studies was performed with STROBE (n = 43) and ORION (n = 2). In the epidemic setting, STROBE was used for 12 studies, ORION for 66 studies, and CARE for 3 studies. Overall, study quality assessed with STROBE was high in 9.1%, moderate in 63.6%, and low in 27.3% of the studies. For ORION, high quality was 0%, moderate quality 44.1%, and low quality 55.9%. With CARE, all studies had moderate quality (100%) (Additional file 1: Table S5). In the endemic setting, the median STROBE score was 13 (range 6–25) and the median ORION score was 22 (range 22–22), in the epidemic setting the median STROBE score was 15.5 (range 10–24), the median ORION score was 17 [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29], and the median CARE score was 16 (range 15–19), respectively.
Discussion
Summary of evidence
In this systematic review, analysing 126 studies, we found that a median of two OI components were performed in the endemic as well as in the epidemic setting. The most common OI components in the endemic settings were screening of the environment as well as general screening of patients on admission and during hospitalization. Identifying an environmental source might guide designated IPC measures to prevent further spread. Measures to combat spread of CRPA were previously described by a systematic review by Tomczyk et al. [13], where the most frequent IPC measures were contact precautions, active surveillance cultures (from all patients, high risk patients, and also contact patients of indexes), monitoring, audit and feedback of preventive measures, and patient cohorting. However, this review did not describe all possible components of OI, even though environmental cleaning was mentioned in 40% of the studies, which implies previous environmental screening might have been performed. Environmental screening is a labour-intensive measure, but to the best of our knowledge, no cost-effectiveness analysis is available in the literature. It is a balance in which it takes an effort to identify an environmental source, but the identification will possibly prevent a potential (ongoing) outbreak. The same applies for screening of patients at admission or during hospitalization. Depending on the prevalence of CRPA in the specific healthcare setting, the costs might exceed the benefits and index-case driven screening might be more appropriate. Recent studies show a benefit of overall screening in the detection of carbapenem-resistant Enterobacterales [39, 40], but it remains unknown if this is also applicable for P. aeruginosa.
In the epidemic setting, screening of the environment as well as identification and screening of contact patients were the most commonly performed components. However, identification and screening of contact patients was only reported in one fifth of the studies. As the epidemic studies report successful containment of the outbreaks in four out of five outbreaks, it remains unknown whether these components were not reported or actually not performed. Our results are in addition to a recently published systematic review by Verdugo-Paiva et al. [15], which reported mostly screening of high-risk patients for carbapenem-resistant Gram-negatives in the endemic as well as the epidemic setting, whereas screening of contact patients was only described in less than half of the studies. In addition, the definition of contact patients was often vague in these studies, ranging from roommates to ward mates and to hospitalized at the same time in the whole hospital or admitted at the same time. These inhomogeneous definitions complicate the interpretation of the yield of screening of contact patients, and therefore, also the clinical impact. Interestingly, the identification and screening of contact patients were more often performed in high prevalence European countries compared to low prevalence countries, which might be due to the expected higher yield in countries with a higher prevalence overall or publication bias due to underreporting of OI without any secondary cases. For other carbapenem-resistant Gram-negative microorganisms, such as Enterobacterales, a few studies report the identification and screening of contact patients with a yield of 2.0% in a low endemic setting [41], but this result might not be transferable to P. aeruginosa due to the often water-related environmental niches [42].
Screening of HCW is often discussed as an additional measure to identify the mode of transmission, but guidance on if and when this would be useful, and how this should be performed, is scarce. Less than a third of the studies reported screening of HCW, often without mentioning the screening site(s) or the result of the screening. If screening sites were reported, it was mainly performed on the hands of HCW. However, detection of CRPA on the hands of HCW is difficult to interpret, as it could be a transient colonization while working with patients colonized with CRPA or an actual, more persistent, source of transmission from a colonized HCW to a patient or the environment. Only two studies reported screening of HCW by rectal swabs or stool cultures [43, 44], interestingly without any detection of CRPA (Additional file 1: Table S3). Nevertheless, screening of HCW is often performed as part of a bundle to increase awareness for hand hygiene.
Implications for clinical practice and research
Due to the probable underreporting of OI in the literature, the available evidence for the individual components is scarce. This leads to an inhomogeneous performance of OI after detection of CRPA in the healthcare setting, and with this, potential under- or overscreening. The current ESCMID guidelines on management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients recommends the enforcement of hand hygiene, and contact precautions in the case of multidrug-resistant P. aeruginosa in the endemic setting [14]. In the epidemic setting, emphasizing hand hygiene, introducing contact precautions for colonized patients, and implementing active screening at hospital admission are recommended (Additional file 1: Table S1) [14]. Guidance for how to perform OI, especially identification and screening of contact patients, but also measures for source identification, is urgently needed to standardize and optimize the yield of OI. In addition, the definition of contact patients is inhomogeneous, making it challenging to compare the different studies. For this, prospective studies focusing on how to conduct OI are needed and an implementation of OI in the ORION statement would be beneficious [24].
Strengths and limitations
Our systematic review gives a detailed overview over OI performed after detection of CRPA with focus on individual components of OI. This is an underreported and underappreciated topic in the current literature, even though it influences daily practice of IPC teams worldwide. It has some limitations. First, in the included studies, the patients’ characteristics are poorly described. Often not even basic demographic information such as age and gender are available. This might make it more difficult to apply the generated knowledge to specific patient populations. Second, the response rate of the authors to review the extracted data was only one-third, partly caused by the gaps between publication date and performance of the search, but probably also due to the pandemic with SARS-CoV-2. This might have caused a lack of information and data in our review. Third, as it is an overall view, there is a mix of high and low prevalence settings, which might have influenced the OI performed. Therefore, we analysed the data by prevalence of CRPA in the respective country, but this data was only available for European countries. Fourth, we looked at OI from the IPC perspective for the healthcare facility only, and not from the perspective of the individual patient.
Conclusions
In conclusion, OI are poorly described in the literature and further studies are needed to better define and evaluate OI after identifying CRPA in the endemic as well as the epidemic setting. While we could show evidence for the usefulness for environmental screening in order to identify the mode of transmission, evidence for HCW screening is scarce and might not lead to the identification of modes of transmission. Even though the yield of screening of CP is poorly described in the literature, it might still be key to contain an outbreak. International guidelines should be further improved and include recommendations for OI as well as guidance to report the OI performed in future studies.
Availability of data and materials
All data generated or analysed during this study are included in the article and its additional files. The data extraction file is available on request.
Abbreviations
- CARE guidelines:
-
Case reports guidelines
- CF:
-
Cystic fibrosis
- CRPA:
-
Carbapenem-resistant Pseudomonas aeruginosa
- ESCMID:
-
European Society for Clinical Microbiology and Infectious Diseases
- HAI:
-
Healthcare-associated infections
- HCW:
-
Healthcare workers
- ICU:
-
Intensive care unit
- IPC:
-
Infection prevention and control
- LTCF:
-
Long term care facility
- MDR:
-
Multidrug-resistant
- NICU:
-
Neonatal intensive care unit
- ORION statement:
-
Guidelines for transparent reporting of outbreak reports and intervention studies of nosocomial infection
- OI:
-
Outbreak investigations
- PICU:
-
Paediatric intensive care unit
- PRISMA statement:
-
Preferred reporting items for systematic reviews and meta-analysis statement
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus type 2
- STROBE:
-
The strengthening the reporting of observational studies in epidemiology
References
Al-Hasan MN, Wilson JW, Lahr BD, Eckel-Passow JE, Baddour LM. Incidence of Pseudomonas aeruginosa bacteremia: a population-based study. Am J Med. 2008;121(8):702–8.
Sadikot RT, Blackwell TS, Christman JW, Prince AS. Pathogen-host interactions in Pseudomonas aeruginosa pneumonia. Am J Respir Crit Care Med. 2005;171(11):1209–23.
Weiner-Lastinger LMAS, Edwards JR, Kallen AJ, Karlsson M, Magill SS, Pollock D, See I, Soe MM, Walters MS, Dudeck MA. Antimicrobial-resistant pathogens associated with adult healthcare-associated infections: summary of data reported to the National Healthcare Safety Network, 2015–2017. Infect Control Hosp Epidemiol. 2020;41:1–18.
European Centre for Disease Prevention and Control (ECDC). Surveillance of antimicrobial resistance in Europe 2018. 2019.
World Health Organization (WHO) and the European Centre for Disease Prevention and Control (ECDC). Antimicrobial resistance surveillance in Europe 2022 – 2020 data. 2022.
Wieland K, Chhatwal P, Vonberg RP. Nosocomial outbreaks caused by Acinetobacter baumannii and Pseudomonas aeruginosa: Results of a systematic review. Am J Infect Control. 2018;46(6):643–8.
Persoon MC, Voor in't holt AF, Wielders CCH, Gommers D, Vos MC, Severin JA. Mortality associated with carbapenem-susceptible and Verona Integron-encodes Metallo-β-lactamase-positive Pseudomonas aeruginosa bacteremia. Antimicrob Resist Infect Control. 2020;9(25).
Karakonstantis S, Kritsotakis EI, Gikas A. Pandrug-resistant Gram-negative bacteria: a systematic review of current epidemiology, prognosis and treatment options. J Antimicrob Chemother. 2020;75(2):271–82.
Gomila M. Emergence of carbapenemases in Pseudomonas aeruginosa: a worldwide problem. Expert Rev Anti Infect Ther. 2014;12(1):9–11.
Ciofi degli Atti M, Bernaschi P, Carletti M, Luzzi I, Garcia-Fernandez A, Bertaina A, Sisto A, Locatelli F, Raponi M. An outbreak of extremely drug-resistant Pseudomonas aeruginosa in a tertiary care pediatric hospital in Italy. BMC Infect Dis. 2014;14:494.
World Health Organization. Recommendations for investigating contacts of persons with infectious tuberculosis in low- and middle-income countries. 2012.
Rainisch G, Jeon S, Pappas D, Spencer KD, Fischer LS, Adhikari BB, et al. Estimated COVID-19 cases and hospitalizations averted by case investigation and contact tracing in the US. JAMA Netw Open. 2022;5(3): e224042.
Tomczyk S, Zanichelli V, Grayson ML, Twyman A, Abbas M, Pires D, et al. Control of Carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii, and Pseudomonas aeruginosa in healthcare facilities: a systematic review and reanalysis of Quasi-experimental studies. Clin Infect Dis. 2019;68(5):873–84.
Tacconelli ECMA, Dancer SJ, De Angelis G, Falcone M, Frank U, Kahlmeter G, Pan A, Petrosillo N, Rodriguez-Bano J, Singh N, Venditti M, Yokoe DS, Cookson B. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect. 2014;20(Suppl. I):1–55.
Verdugo-Paiva F, Otaiza F, Roson-Rodríguez P, Rojas-Gomez AM, Galas M, El Omeiri N, Fuentes Y, Rada G, Ramón-Pardo P. Effects of screening strategies to detect carbapenem-resistant gram-negative bacteria: a systematic review. Am J Infect Control. 2022;50(12):1381–8. https://doi.org/10.1016/j.ajic.2022.02.018.
Maltezou HCPO, Nikolopoulos G, Ftika L, Maragos A, Kaitsa H, Protonotariou E, Diya E, Georgiadis N, Vatopoulos A, Nicolaidis P. Post-cataract surgery endophthalmitis outbreak caused by multidrug-resistant Pseudomonas aeruginosa. Am J Infect Control. 2012;40:75–7.
Kohlenberg A, Weitzel-Kage D, van der Linden P, Sohr D, Voegeler S, Kola A, et al. Outbreak of carbapenem-resistant Pseudomonas aeruginosa infection in a surgical intensive care unit. J Hosp Infect. 2010;75:350–7.
Weng MK, Brooks RB, Glowicz J, Keckler MS, Christensen BE, Tsai V, et al. Outbreak investigation of Pseudomonas aeruginosa infections in a neonatal intensive care unit. Am J Infect Control. 2019;47:1148–50.
Tran-Dinh A, Neulier C, Amara M, Nebot N, Troché G, Breton N, et al. Impact of intensive care unit relocation and role of tap water on an outbreak of Pseudomonas aeruginosa expressing OprD-mediated resistance to imipenem. J Hosp Infect. 2018;100(3):e105–14.
Moher DLA, Tetzlaff J, Altman DG, The PRISMA group. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. Plos Med. 2009;6(7):97.
Scherer RW, Saldanha IJ. How should systematic reviewers handle conference abstracts? A view from the trenches. Syst Rev. 2019;8(1):264.
EARS-Net. Data from the ECDC Surveillance Atlas - Antimicrobial resistance: European Centre for Disease Prevention and Control (ECDC); 2022 [Available from: https://www.ecdc.europa.eu/en/antimicrobial-resistance/surveillance-and-disease-data/data-ecdc.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, for the STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8.
Stone SP, Cooper BS, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al. The ORION statement: guidelines for transparent reporting of outbreak reports and intervention studies of nosocomial infection. Lancet Infect Dis. 2007;7:282–8.
Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218–35.
Adachi JA, Perego C, Graviss L, Dvorak T, Hachem R, Chemaly RF, et al. The role of interventional molecular epidemiology in controlling clonal clusters of multidrug resistant Pseudomonas aeruginosa in critically ill cancer patients. Am J Infect Control. 2009;37(6):442–6.
Cholley P, Gbaguidi-Haore H, Bertrand X, Thouverez M, Plésiat P, Hocquet D, et al. Molecular epidemiology of multidrug-resistant Pseudomonas aeruginosa in a French university hospital. J Hosp Infect. 2010;76(4):316–9.
Gomes MZR, Machado CR, De da Souza Conceição M, Ortega JA, Neves SMFM, Da Silva Lourenço MC, et al. Outbreaks, persistence, and high mortality rates of multiresistant Pseudomonas aeruginosa infections in a hospital with AIDS-predominant admissions. Braz J Infect Dis. 2011;15(4):312–22.
Mammina C, Di Carlo P, Cipolla D, Casuccio A, Tantillo M, Plano MRA, et al. Nosocomial colonization due to imipenem-resistant Pseudomonas aeruginosa epidemiologically linked to breast milk feeding in a neonatal intensive care unit. Acta Pharmacol Sin. 2008;29(12):1486–92.
Mahmoud MF, Fathy FM, Gohar MK, Awad WM, Soliman MH. Genotyping of Pseudomonas aeruginosa strains isolated from surgical site infected patients by RAPD-PCR. Syst Rev Pharm. 2020;11(12):1998–2005.
Geladari A, Karampatakis T, Antachopoulos C, Iosifidis E, Tsiatsiou O, Politi L, et al. Epidemiological surveillance of multidrug-resistant gram-negative bacteria in a solid organ transplantation department. Transplant Infect Dis. 2017. https://doi.org/10.1111/tid.12686.
Carattoli A, Fortini D, Galetti R, Garcia-Fernandez A, Nardi G, Orazi D, Capone A, Majolino I, Proia A, Mariani B, Parisi G. Isolation of NDM-1-producing Pseudomonas aeruginosa sequence type ST235 from a stem cell transplant patient in Italy, May 2013. Eurosurveillance. 2013;18(46):20633.
Cezário RC, De Duarte Morais L, Ferreira JC, Costa-Pinto RM, Da Costa Darini AL, Gontijo-Filho PP. Nosocomial outbreak by imipenem-resistant metallo-β-lactamase- producing Pseudomonas aeruginosa in an adult intensive care unit in a Brazilian teaching hospital. Enferm Infecc Microbiol Clin. 2009;27(5):269–74.
Hopman J, Meijer C, Kenters N, Coolen JPM, Ghamati MR, Mehtar S, et al. Risk assessment after a severe hospital-acquired infection associated with carbapenemase-producing Pseudomonas aeruginosa. JAMA Netw Open. 2019;2(2): e187665.
Flateau C, Janvier F, Delacour H, Males S, Ficko C, Andriamanantena D, Jeannot K, Merens A, Rapp C. Recurrent pyelonephritis due to NDM-1 metallo-beta-lactamase producing Pseudomonas aeruginosa in a patient returning from Serbia, France, 2012. Euro Surveill. 2012;17(45):20311.
Milan O, Debroize L, Bertrand X, Plesiat P, Valentin AS, Quentin R, et al. Difficult-to-detect carbapenem-resistant IMP13-producing P. aeruginosa: experience feedback concerning a cluster of urinary tract infections at a surgical clinic in France. Antimicrob Resist Infect Control. 2013;2(1):1–5.
Dubois V, Arpin C, Melon M, Melon B, Andre C, Frigo C, et al. Nosocomial outbreak due to a multiresistant strain of Pseudomonas aeruginosa P12: efficacy of cefepime-amikacin therapy and analysis of beta-lactam resistance. J Clin Microbiol. 2001;39(6):2072–8.
Freire MP, Camargo CH, Yamada AY, Nagamori FO, Reusing Junior JO, Spadao F, et al. Critical points and potential pitfalls of outbreak of IMP-1-producing carbapenem-resistant Pseudomonas aeruginosa among kidney transplant recipients: a case-control study. J Hosp Infect. 2021;115:83–92.
Otter JA, Mookerjee S, Davies F, Bolt F, Dyakova E, Shersing Y, et al. Detecting carbapenemase-producing Enterobacterales (CPE): an evaluation of an enhanced CPE infection control and screening programme in acute care. J Antimicrob Chemother. 2020;75(9):2670–6.
Foley M, Duffy F, Skally M, McCormack F, Finn C, O’Connor M, et al. Evolving epidemiology of carbapenemase-producing Enterobacterales: one hospital’s infection prevention and control response over nine years. J Hosp Infect. 2021;112:61–8.
Chang E, Chang HE, Shin IS, Oh YR, Kang CK, Choe PG, et al. Investigation on the transmission rate of carbapenemase-producing carbapenem-resistant Enterobacterales among exposed persons in a tertiary hospital using whole-genome sequencing. J Hosp Infect. 2022;124:1–8.
Pham TM, Buchler AC, Voor In ’t Holt AF, Severin JA, Bootsma MCJ, Gommers D, et al. Routes of transmission of VIM-positive Pseudomonas aeruginosa in the adult intensive care unit-analysis of 9 years of surveillance at a university hospital using a mathematical model. Antimicrob Resist Infect Control. 2022;11(1):55.
Saharman YR, Pelegrin AC, Karuniawati A, Sedono R, Aditianingsih D, Goessens WHF, et al. Epidemiology and characterisation of carbapenem-non-susceptible Pseudomonas aeruginosa in a large intensive care unit in Jakarta, Indonesia. Int J Antimicrob Agents. 2019;54(5):655–60.
Mudau M, Jacobson R, Minenza N, Kuonza L, Morris V, Engelbrecht H, et al. Outbreak of multi-drug resistant Pseudomonas aeruginosa bloodstream infection in the haematology unit of a South African Academic Hospital. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0055985.
Acknowledgements
We thank Dr. Wichor M. Bramer for devising and executing our systematic literature search. We thank the corresponding authors of the evaluated studies for providing feedback on our extracted data.
Funding
This work was supported by a personal grant to Andrea C. Büchler by the Forschungsfonds of the University of Basel, Basel, Switzerland. The funding source had no role in the design, analysis or results of the study.
Author information
Authors and Affiliations
Contributions
Conceived and design the study: ACB, SNS, JAS, MCV, and AVF. Data collection: ACB, SNS, AFV. Analysed the data: ACB. Interpretation of the data: ACB and AVF. Wrote the manuscript: ACB and AVF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable for this study.
Consent for publication
Not applicable for this study.
Competing interests
ACB, SNS, JAS, MCV, and AFV declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Table 1. Overview table of the evidence and recommendation for multidrug-resistant Pseudomonas aeruginosa in the healthcare setting, adapted from the ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Table 2. Study characteristics of the included 126 studies. Table 3. Outbreak investigations after detection of CRPA stratified by hospital setting. Table 4. Quality assessments of the included studies by study type. Document 1. PRISMA 2020 Checklist. Document 2. Literature search strategies. Figure 1. Year of publication of the included studies (N=126).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Büchler, A.C., Shahab, S.N., Severin, J.A. et al. Outbreak investigations after identifying carbapenem-resistant Pseudomonas aeruginosa: a systematic review. Antimicrob Resist Infect Control 12, 28 (2023). https://doi.org/10.1186/s13756-023-01223-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-023-01223-1