Abstract
Background
In low- and middle-income countries, the prevalence of antimicrobial resistance (AMR) is increasing. To control AMR, WHO recommends monitoring antibiotic use, in particular Watch antibiotics. These are critically important antibiotics, with restricted use because at risk of becoming ineffective due to increasing AMR. We investigated pre-hospital antibiotic use in rural Burkina Faso.
Methods
During 2016–2017, we collected data from patients aged > 3 months presenting with severe acute fever to the rural hospital of Nanoro Health District, Burkina Faso, including antibiotic use in the two weeks prior to consultation or hospitalization. We analysed reported antibiotic use by applying the WHO Access, Watch, Reserve classification.
Results
Of 920 febrile participants (63.0% ≤ 14 years), pre-hospital antibiotic use was reported by 363 (39.5%). Among these 363, microbiological diagnoses were available for 275 (75.8%) patients, of whom 162 (58.9%) were non-bacterial infections. Use of more than one antibiotic was reported by 58/363 (16.0%) participants. Of 491 self-referred patients who did not previously visit a primary health care center, 131 (26.7%) reported antibiotic use. Of 424 antibiotics reported, 265 (62.5%) were Access and 159 (37.5%) Watch antibiotics. Watch antibiotic use was more frequent among patients > 14 year olds (51.1%) compared to those 0–14 year old (30.7%, p < 0.001) and among referrals from the primary health care centers (42.2%) compared to self-referred patients (28.1%, p = 0.004). Most frequently reported Watch antibiotics were ceftriaxone (114, 71.7%) and ciprofloxacin (32, 20.1%).
Conclusion
The reported frequent use of Watch group antibiotics among febrile patients prior to presentation to the hospital in rural Burkina Faso highlights the need to develop targeted interventions to improve antibiotic use in community settings as part of strengthening antibiotic stewardship in low- and middle-income countries. This should include facilitating referral, access to qualified prescribers and diagnostic tools in rural primary health care centers.
Trial registration ClinicalTrials.gov identifier: NCT02669823. Registration date was February 1, 2016.
Similar content being viewed by others
Introduction
The emergence of antimicrobial resistance (AMR) is driven by appropriate and inappropriate use of antimicrobials. Increasing microorganisms’ exposure to antibiotics results in selection pressure, while suboptimal regimen allows selective survival of resistant microorganisms [1, 2]. Globally, mortality attributable to AMR infections has been estimated to increase from 700,000 annual deaths in 2014 to 10 million in 2050 [3]. The World Health Organization's 2015 Global Action Plan on AMR urges a.o. to strengthen surveillance of AMR and antibiotic use, and to optimize the use of antibiotics [4]. A global surveillance network for monitoring concurrently AMR and antibiotic use, the Global Antimicrobial Resistance Surveillance System (GLASS), has since been set up, reporting country-wide AMR prevalence of key human pathogens and antibiotics [5]. To monitor antibiotic use, WHO proposed a classification of antibiotics for human use in three groups, "Access", "Watch" and "Reserve", according to their clinical importance, specific recommendations for their appropriate use, and resistance potential [6]. Antibiotic sales data during 2000–2015 showed that the human use of so-called Watch antibiotics, critically important antibiotics particularly at risk of AMR emergence, was declining in high-income countries, while importantly increasing in middle income countries for which data were available [7, 8].
In sub-Saharan Africa, self-medication with over-the-counter antibiotics from private pharmacies or informal drug stores, without prior prescription by a qualified health worker, is frequent and facilitates uncontrolled antibiotic use [8,9,10,11]. To optimize antibiotic use, it is crucial to understand the epidemiology of antibiotic use, in the community as well as in the hospital. Furthermore, also in local primary health care centers, antibiotic prescriptions are not always rational [9, 12]. Peripheral health workers’ poor understanding of the correct use of antibiotics and risks of AMR, limited availability and use of diagnostic tools and difficult access to qualified referral healthcare are likely to be fuelling irrational prescribing of antibiotics [13, 14]. National level antibiotic consumption estimated from wholesale data, as in Burkina Faso, is limited to the official healthcare sector and usually aggregates in- and outpatient use [15]. To our knowledge, no studies so far have investigated community-level antibiotic use. The purpose of this study is to understand community-level antibiotic use in febrile patients prior to presentation to the hospital in a rural district of Burkina Faso.
Methods
Study population
From March 23, 2016 to June 30, 2017, the PaluBac study recruited patients aged > 3 months presenting to the Nanoro district hospital with acute fever (tympanic temperature ≥ 38.0 °C) or history of fever in the last 48 h and ≥ 1 symptom(s) of respiratory distress, generalized weakness (prostration), impaired consciousness, seizures (one or more episodes), clinical jaundice, signs of shock, or with suspected severe malaria, invasive bacterial infection, or severe viral infection. A total of 920 patients of whom 344 (37.4%) inpatients and 576 (62.6%) outpatients were included. From March 23 to November 8, 2016, only inpatients were recruited; from November 9, 2016 to June 30, 2017 also outpatients were included. PaluBac evaluated the performance of an automated cell counter to quantify malaria parasitaemia [16]. Our embedded cross-sectional study recorded patients’ pre-hospital antibiotic use.
The study was conducted in the Nanoro Health District in the West-Central region of Burkina Faso, about 90 km from Ouagadougou, the capital city of Burkina Faso. The district has 24 primary health care centers and one district hospital, “Centre Médical avec Antenne Chirurgicale” (CMA). Primary health care centers are meant to be the patients’ first point of contact with the healthcare system, during outpatient consultations. There are no medical doctors attached. More complicated cases are referred from the primary health care centers to the district hospital [17]. The district hospital has hospitalization units, medical doctors and a clinical microbiology laboratory. In the health district, the most frequently reported diagnosis is malaria [18], in children often associated with a community-acquired invasive bacterial co-infection [19, 20]. Malaria is endemic with a high malaria transmission season from July to November. This period overlaps with the rainy season, which extends from June to October. The low malaria transmission season is from December to June.
Antibiotics dispensing in Burkina Faso
In Burkina Faso health districts, antibiotics can be obtained from formal public or private drug stores after prescription by a Medical Doctor or a nurse. Importation and quality of antibiotics (and medicines in general) is under the control of the national pharmaceutical regulatory agency [21]. However, some medicines escape from this control and are available over-the-counter in public places such as markets [22]. Also in formal drug stores, antibiotics can be purchased without prior consultation or prescription. In primary health care centers, the only diagnostic tools available to support febrile diseases management are malaria rapid diagnostic tests (RDT). If such tests show a negative result, this often leads to systematic antibiotic prescription [23].
Data collection
At inclusion, study clinicians completed case report forms with medical history, including the use of antibiotics and antimalarials in the two weeks prior to consultation, which we refer to as pre-hospital antibiotic use, the date of symptom onset, and whether the patient was referred or not from a primary health care center. Referral patients first attended a primary health care center where a nurse decided about the need for higher-level care and referral to the district hospital, based on clinical symptoms. Proper inpatient care is not possible at a primary health care center, the patient can only be observed for a maximum of 48 h. Self-referred patients were those presenting directly at the district hospital without first attending a primary health care center.
Data analysis
Pre-hospital antibiotics were classified (1) according to WHO's Access, Watch, Reserve (AWaRe) classification and (2) according to products name as stated in the WHO essential medicines list [6]. For the latter, we combined ampicillin and amoxicillin use into one category (“ampicillin or amoxicillin”), and zoomed in on the use of the most prevalently prescribed antibiotic in the Watch group in particular. Anti-tuberculosis drugs were excluded from analysis. We report frequencies of antibiotics used by product name and by AWaRe group, of the use of more than one antibiotic, and compared by age (0–14 years vs. > 14 years), by malaria transmission season, by hospitalisation status after arrival to the hospital (in- vs outpatients) and by referral vs self-referred, using chi-square tests. We stratified the frequencies of pre-hospital antibiotic use by malaria transmission season. Data was analysed with Stata version 14.2 (StataCorp LP, Texas, USA).
Results
Characteristics of the study population
Of 1212 screened febrile patients, 920 (75.9%) patients were included in the study and had complete data available about pre-hospital antibiotic use. Of these 920, 344 (37.4%)were hospitalized upon arrival at the hospital and 576 (62.6%) were treated as outpatients. Children aged 0–14 years represented 580 (63.0%) of patients and 533 (57.9%) patients were male. A total of 428 (46.5%) patients were referrals from primary health care centers, the remaining were self-referred (Table 1).
Pre-hospital antibiotic use
Pre-hospital antibiotic use was reported by 363/920 (39.5%) patients, of whom 58 (16.0%) used more than one antibiotic. Proportion of use tended to be more prevalent among 0–14 year olds (240, 41.4%) compared to those > 14 (123, 36.2%) (p = 0.12). Referral patients significantly more frequently reported pre-hospital antibiotic use (231, 54.0%) than self-referred patients (131, 26.7%, p < 0.001). Fewer patients (131, 34.7%) reported antibiotic use during the high malaria transmission season than outside (232, 42.7%, p < 0.001).
Microbiological diagnoses (malaria microscopy, blood culture, PCR of nasopharyngeal swabs) were available for 275/363 (75.8%) patients who reported pre-hospital antibiotic use. Of these, 113 (41.1%) were bacterial infections; the other diagnoses were malaria (70, 25.5%), viral infections excluding HIV (85, 30.9%), and HIV (7, 2.6%) HIV.
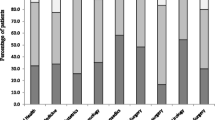
AWaRe distribution of antibiotics
Overall, 424 antibiotics were reported by 363 patients: 265 (62.5%) antibiotics belonged to the Access group, 159 (37.5%) to the Watch group and none to the Reserve group. Watch antibiotics were more frequently reported by > 14 year olds (72, 51.1%) than by 0–14 year olds (87, 30.7%, p < 0.001) and by referrals (117, 42.2%) compared to self-referred patients (41, 28.1%, p = 0.004). There was no difference in the proportion of Watch antibiotics used between the high and low malaria-transmission season (Table 2).
Antibiotics reported
Ampicillin or amoxicillin use (Access) was the most reported antibiotic, accounting for 137/424 (32.3%) of all antibiotics reported. The most frequently reported Watch antibiotics were ceftriaxone (114, 26.9% of all antibiotics reported) and ciprofloxacin (32, 7.5% of all antibiotics reported). Among antibiotics reported by referral patients (n = 277 antibiotics), ceftriaxone was recorded 100 times (36.1%) and ciprofloxacin 12 times (4.3%). Among antibiotics reported by self-referred patients (n = 146), ciprofloxacin was recorded 20 times (13.7%) (Table 3).
Discussion
Nearly 40% of patients presenting with acute fever to a referral hospital in rural Burkina, reported pre-hospital antibiotic use; more than half of patients who were referred by a primary health care centre, and a quarter of self-referred patients. Nearly 60% of febrile patients with pre-hospital antibiotic use for whom a microbiological diagnosis was available did not have a bacterial infection confirmed.
While empirical first- or second-choice (Access) antibiotics were most frequently used, Watch antibiotics were used by 42% of patients referred from a primary health care center. The high use of Watch antibiotics in referred patients is worrisome particular since ceftriaxone (Watch) is not on the Burkina Faso medicine list for use in primary health care centers and is recommended at this level only in case of a meningitis outbreak (which did not occur during our study period) [24]. Moreover, Watch antibiotics accounted for 28% of antibiotics used by self-referred patients, who presumably self-medicated with antibiotics obtained without prescription at private pharmacies or from informal drug sellers. Use of Watch antibiotics was not associated with severity or seasonality as there was no increased risk for patients admitted compared to those treated as outpatients nor during low-malaria transmission season compared to high-malaria transmission season.
High and increasing use of Watch antibiotics has been observed in other low- and middle-income settings [7, 25, 26]. To optimize antibiotic use, it is important to better understand the origins of and reasons why Watch antibiotics are used, both at primary health care center level and without prescription at the community-level. Our study illustrates the need to monitor antibiotic use among official and informal healthcare providers. Nationwide antibiotic use estimated from official sales data found that, in 2015, 75% of antibiotics used in Burkina Faso were Access and 24% Watch group, achieving the WHO target of at least 60% of antibiotics used to be Access antibiotics [15]. This use of Watch antibiotics is lower than the proportion of Watch antibiotics reported in the present study. In comparison, the frequency of pre-hospital antibiotic use by febrile patients admitted to the Nanoro district hospital in 2012–2013 was lower (28.2%), and the proportion of Access antibiotics used was higher (45.9% amoxicillin or ampicillin vs. 32.3% now and 35.1% trimethoprim + sulfamethoxazole vs. 10.6% now) [19], further confirming the need to halt and reverse this high prevalence of Watch antibiotic use.
Despite ampicillin being the treatment of choice for patients with severe infectious diseases at primary health care center level pending referral, it is increasingly ineffective against Enterobacterales. Indeed, most (90.5%) of non-Typhi Salmonella and 87.5% of Escherichia coli were resistant to ampicillin in Nanoro during 2012–2013 [19]. This could explain (systematic) use of ceftriaxone when—in the absence of a microbiological diagnosis—bloodstream infection is suspected. Rapid referral to the district hospital, where laboratory testing should be available as recommended in the WHO model list of essential in vitro diagnostics [27] is then indicated. Because cephalosporin use has been associated to the emergence of beta-lactamase-producing pathogens, particular caution must be taken to optimize its use [28]. Integrating point-of-care CRP or procalcitonin tests at primary health care center level, to differentiate between bacterial and non-bacterial causes of fever, could be explored [29].
Some caution interpreting these findings is needed. First, the inclusion of outpatients during the second half of the study period might have resulted in some changes in the study population and pre-hospital antibiotic use. However, we observed no difference in the prevalence of antibiotic use, when comparing the two populations from both recruitment periods. Further, data about pre-hospital antibiotic use were missing for a quarter of screened patients. Also, antibiotic use was collected via a survey capturing use during the two weeks before consultation at the hospital, potentially underestimating actual use. Whenever possible, reported antibiotic use was verified from referral forms, patient medical files (healthcare booklet), and antibiotic packaging or blisters. Dosage and duration of antibiotic used were not available and the final diagnoses at the district hospital may not correspond to those that had triggered prescription or self-medication within the two preceding weeks.
Conclusion
The frequent use of Watch antibiotics in primary health care centers and at community-level in rural Burkina Faso is concerning in a context of increasingly ineffective first-line antibiotics. It points to the need to set up antibiotic use monitoring and antibiotic stewardship in rural communities in low- and middle-income countries (LMIC. As no alternatives for the currently available Watch antibiotics are available nor affordable in many LMIC settings, it is imperative to act to avoid even more alarming levels of resistance in years to come.
Availability of data and materials
All data generated or analysed during this study are included in this published article and datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMR:
-
Antimicrobial resistance
- AWaRe:
-
Access, watch, reserve
- CMA:
-
Centre Médical avec Antenne Chirurgicale
- CRP:
-
C-reactive protein
- GLASS:
-
Global antimicrobial resistance surveillance system
- HIV:
-
Human immunodeficiency virus
- RDT:
-
Rapid diagnostic test
- WHO:
-
World Health Organization
References
Booton RD, Meeyai A, Alhusein N, Buller H, Feil E, Lambert H, et al. One Health drivers of antibacterial resistance: quantifying the relative impacts of human, animal and environmental use and transmission. One Heal. 2021;12:100220.
Montero MM, Domene-Ochoa S, López-Causapé C, Luque S, Sorlí L, Campillo N, et al. Impact of ceftolozane/tazobactam concentrations in continuous infusion against extensively drug-resistant Pseudomonas aeruginosa isolates in a hollow-fiber infection model. Sci Rep. 2021;11(1):1–8. https://doi.org/10.1038/s41598-021-01784-4.
O’Neill J. Antimicrobial resistance: tackling a crisis for the health and wealth of nations. Rev Antimicrob Resist. 2014.
WHO. Global action plan on antimicrobial resistance. 2015. p. 1–28
World Health Organization. Global antimicrobial resistance surveillance system (GLASS) report. Early implementation. 2017–2018. 2018. https://www.who.int/glass/resources/publications/early-implementation-report/en/.
World Health Organization (WHO). World Health Organization Model List of Essential Medicines 2021. 2021. https://www.who.int/leishmaniasis/burden/Leishmaniasis_India/en/.
Klein EY, Van Boeckel TP, Martinez EM, Pant S, Gandra S, Levin SA, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci U S A. 2018;115(15):E3463–70.
Klein EY, Milkowska-Shibata M, Tseng KK, Sharland M, Gandra S, Pulcini C, et al. Assessment of WHO antibiotic consumption and access targets in 76 countries, 2000–15: an analysis of pharmaceutical sales data. Lancet Infect Dis. 2020;21:107–15.
Yeika EV, Ingelbeen B, Kemah BL, Wirsiy FS, Fomengia JN, van der Sande MAB. Comparative assessment of the prevalence, practices and factors associated with self-medication with antibiotics in Africa. Trop Med Int Heal. 2021;26(8):862–81.
Hughes R, Chandler CR, Mangham-Jefferies LJ, Mbacham W. Medicine sellers’ perspectives on their role in providing health care in North-West Cameroon: a qualitative study. Health Policy Plan. 2013;28(6):636–46.
Noordam AC, Carvajal-Velez L, Sharkey AB, Young M, Cals JWL. Care seeking behaviour for children with suspected pneumonia in countries in sub-Saharan Africa with high pneumonia mortality. PLoS ONE. 2015;10(2):1–14.
Chem ED, Anong DN, Akoachere JFKT. Prescribing patterns and associated factors of antibiotic prescription in primary health care facilities of Kumbo East and Kumbo West Health Districts, North West Cameroon. PLoS ONE. 2018;13(3):1–18.
Bessat C, Zonon NA, D’Acremont V. Large-scale implementation of electronic Integrated Management of Childhood Illness (eIMCI) at the primary care level in Burkina Faso: a qualitative study on health worker perception of its medical content, usability and impact on antibiotic prescription. BMC Public Health. 2019;19(1):1–12.
Ahiabu MA, Tersbøl BP, Biritwum R, Bygbjerg IC, Magnussen P. A retrospective audit of antibiotic prescriptions in primary health-care facilities in Eastern Region. Ghana Health Policy Plan. 2016;31(2):250–8.
WHO. WHO report on surveillance of antibiotic consumption. 2018. https://apps.who.int/iris/bitstream/handle/10665/277359/9789241514880-eng.pdf.
Post A, Kaboré B, Reuling IJ, Bognini J, Van Der Heijden W, Diallo S, et al. The XN-30 hematology analyzer for rapid sensitive detection of malaria: a diagnostic accuracy study. BMC Med. 2019;17(1):1–12.
OMS, Ministère de la santé du Burkina Faso. Profil sanitaire du Burkina Faso. 2017. p. 1–64.
Ministère de la santé/Burkina Faso. PLAN D ’ ACTON 2018 du District Sanitaire de Nanoro. 2018.
Maltha J, Guiraud I, Kaboré B, Lompo P, Ley B, Bottieau E, et al. Frequency of severe malaria and invasive bacterial infections among children admitted to a rural hospital in Burkina Faso. PLoS ONE. 2014;9(2):1–8.
Guiraud I, Post A, Diallo SN, Lompo P, Maltha J, Thriemer K, et al. Population-based incidence, seasonality and serotype distribution of invasive salmonellosis among children in Nanoro, rural Burkina Faso. PLoS ONE. 2017;12:e0178577.
Ministère de la santé Burkina Faso. Plan stratégique pharmaceutique 2019–2023. 2019.
Ministère de la Santé du Burkina Faso. Plan d’action national multisectoriel de lutte contre la resistance aux antimicrobiens. 2017. p. 85
Bonko MDA, Kiemde F, Tahita MC, Lompo P, Some AM, Tinto H, et al. The effect of malaria rapid diagnostic tests results on antimicrobial prescription practices of health care workers in Burkina Faso. Ann Clin Microbiol Antimicrob. 2019;18(1):1–9. https://doi.org/10.1186/s12941-019-0304-2.
Ministère de la Santé du Burkina Faso. Liste national des médicaments essentiels et autres produits de santé. 2016. p. 81.
Sulis G, Adam P, Nafade V, Gore G, Daniels B, Daftary A, et al. Antibiotic prescription practices in primary care in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2020;17(6):e1003139. https://doi.org/10.1371/journal.pmed.1003139.
Ingelbeen B, Koirala KD, Verdonck K, Barbé B, Mukendi D, Thong P, et al. Antibiotic use prior to seeking medical care in patients with persistent fever: a cross-sectional study in four low- and middle-income countries. Clin Microbiol Infect. 2020. https://doi.org/10.1016/j.cmi.2020.11.003.
World Health Organization. Second WHO model list of essential in vitro diagnostics. Who/Mvp/Emp/2019.05. 2019. https://www.ghdonline.org/uploads/EDL_ExecutiveSummary_15may.pdf.
Hu YJ, Ogyu A, Cowling BJ, Fukudaa K, Panga H. Available evidence of antibiotic resistance from extended-spectrum ß-lactamase-producing enterobacteriaceae in paediatric patients in 20 countries: a systematic review and meta-analysis. Bull World Health Organ. 2019;97(7):486-501B.
Keitel K, Kagoro F, Samaka J, Masimba J, Said Z, Temba H, et al. A novel electronic algorithm using host biomarker point-of-care tests for the management of febrile illnesses in Tanzanian children (e-POCT): a randomized, controlled non-inferiority trial. PLoS Med. 2017;14(10):1–29.
Acknowledgements
We acknowledge all the Palubac study team and all study participants for their willingness to participate in this study. We are also thankful to the Palubac study staff, mainly the clinicians and nurses who participated in data collection. We thank all the Clinical Research Unit of Nanoro staff as well as the Nanoro district hospital staff for being part in some ways of the success of this study.
Funding
The study was partly funded by the Belgian Directorate of Development Cooperation through the corresponding author’s Master in Sciences of public health funding and through the collaboration between the Institute of Tropical Medicine, Antwerp Belgium and the Clinical Research Unit Nanoro, Burkina Faso. The study was also partly funded by the Conseil de l’Action International de l’ Université Catholique de Louvain, through the corresponding author’s Ph.D. funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: DV, BI, MABvdS, JJ. Data curation: DV. Formal analysis: DV. Investigation: BK, IK, MP, PL, AP, JC. Methodology: DV, BI, MABvdS, JJ. Software: DV. Supervision: HT, MABvdS, JJ. Validation: HT, MABvdS, JJ. Writing—Original Draft Preparation: DV. Writing—Review & Editing: BI, BK, MP, PL, EV, AP, JC, QdM, AR, MABvdS, HRV, AvdV, HT, JJ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The PaluBac study protocol and an amendment to include pre-hospital antibiotic use were approved by the Ethics Committee for Health Research of Burkina Faso (ref 1029/15 and 2017-01-001). Written informed consent was obtained from all included patients or their caretakers.
Consent for publication
All the patients included in the study or their caretakers gave their consents for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Valia, D., Ingelbeen, B., Kaboré, B. et al. Use of WATCH antibiotics prior to presentation to the hospital in rural Burkina Faso. Antimicrob Resist Infect Control 11, 59 (2022). https://doi.org/10.1186/s13756-022-01098-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-022-01098-8