Abstract
Background
Disinfectant products are used frequently on environmental surfaces (e.g. medical equipment, countertops, patient beds) and patient care equipment within healthcare facilities. The purpose of this study was to assess the risk of cross-contamination of Staphylococcus aureus and Pseudomonas aeruginosa during and after disinfection of predetermined surface areas with ready-to-use (RTU) pre-wetted disinfectant towelettes.
Methods
This study tested six disinfectant towelette products against S. aureus ATCC CRM-6538 and P. aeruginosa strain ATCC-15442 on Formica surfaces. Each disinfectant was evaluated on a hard nonporous surface and efficacy was measured every 0.5 m2 using a modified version of EPA MLB SOP-MB-33 to study the risk of cross-contamination.
Results
We found that all of the wipes used in this study transferred S. aureus and P. aeruginosa from an inoculated surface to previously uncontaminated surfaces. Disinfectant towelettes with certain chemistries also retained a high level of viable bacteria after disinfection of the surface area. The cross-contamination risk also varied by product chemistry and bacterial strain.
Conclusion
Disinfectant wipes can cross-contaminate hard nonporous surfaces and retain viable bacterial cells post-disinfection, especially over larger surface areas. This highlights a need to further investigate the risk disinfectant wipes pose during and post-disinfection and guidance on maximum surface areas treated with a single towelette.
Similar content being viewed by others
Background
Healthcare Acquired Infections (HAIs) are prevalent in healthcare settings and are becoming harder to treat especially as levels of multidrug resistant infections are on the rise [1]. According to the Center for Disease Control and Prevention (CDC), approximately one in 31 United States (US) patients will contract at least one HAI within 4 days of health care facility admission [2]. Although this is an improvement from 2011 statistics with daily HAI incidence rates of at least one in 25 patients, in 2015, an estimated 633,300 US patients suffered from 687,200 HAI [3]. The most prevalent infection rates occur in acute care hospitals (ACHs), predominantly due to opportunistic pathogens occurring in healthcare settings [4], and the HAI tracking and reporting requirements for acute care facilities to the National Healthcare Safety Network of the CDC. The risk of a HAI occurring is highest among immunocompromised individuals [5]; with mortality rates of approximately 11% among hospitalized patients suffering from HAIs [3].
Staphylococcus aureus and P. aeruginosa are among the most prevalent etiological agents of HAIs [6]. S. aureus is typically harmless to a healthy individual, but can cause deadly infections, such as septicemia, endocarditis, osteoarticular infections, and pleuropulmonary infections [7]. P. aeruginosa can also cause infections such as cystic fibrosis [8] septicemia and pneumonia that can be fatal for immunocompromised individuals [9].
Hard nonporous environmental surfaces in healthcare facilities harbor pathogens that cause HAIs [10]. S. aureus and P. aeruginosa have been detected from bedside cupboards, bed rails, floors and other hospital equipment [11]. S. aureus and P. aeruginosa persist on these surfaces [12, 13], increasing transmission risk resulting in HAIs [14]. Overall, pathogen persistence could be due to sub-lethal concentrations of disinfectants [15, 16], low efficacy levels for some classes of disinfectant wipes [17, 18], amount of surface area wiped [18], and the label-use recommendations not being followed [19].
Healthcare personnel rely on disinfectant wipes for environmental surface disinfection [20, 21]. Previous studies have focused mainly on the bactericidal efficacy of disinfectants under label and off-label use conditions [20, 22]. However, despite widespread use of disinfectants, limited studies [23,24,25] have evaluated the risk of disinfectant towelettes cross-contaminating previously uncontaminated surfaces during the wiping process from an inoculum source. The objectives of this study were to (i) evaluate the risk of disinfectant towelettes transferring S. aureus or P. aeruginosa from an inoculated zone to otherwise not contaminated surfaces and (ii) detect levels of S. aureus or P. aeruginosa on disinfectant towelettes after the wiping process. We hypothesized that during the wiping process, disinfectant towelettes are capable of transferring pathogens to otherwise low-risk areas of an environmental surface. We also hypothesized that post-disinfection, and following label-defined contact times, towelettes may remain contaminated with viable S. aureus or P. aeruginosa.
Methods
Bacteria, disinfectant towelettes, and surface type used for testing
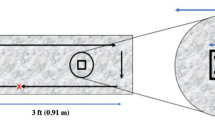
This study tested six disinfectant towelettes (Table 1) that are commonly used in healthcare facilities for equipment and environmental surface disinfection. The experiment proceeded with Formica (laminate) imitation-granite surface, which was two square meters in length as previously described by Nkemngong et al., 2020 (submitted). Briefly, the Formica board was partitioned into five testing zones: the inoculation zone (i-zone) and one-half (0.5 m2), one (1.0 m2), one and a half (1.5 m2), and two square meters (2.0 m2) from the i-zone (Fig. 1). The zones for testing (swabbing) were 10 × 10 cm (0.01 m2) in size. The disinfectant towelette itself was also analyzed after the wiping procedure was complete.
Schematic diagram of the Formica surface used for wipe testing. Two meters of Formica were delineated into 0.5 m2 sections. Approximately 2.5 × 107 log10 CFU of S. aureus or P. aeruginosa were spotted onto the i-zone (red dots). The surface was wiped in an up and down pattern as indicated by black outlined arrows from left to right. Light grey squares 10 cm × 10 cm (100 cm2) were sampled to recover potentially cross-contaminated S. aureus or P. aeruginosa
Surface preparation, wiping method, and sample collection
The Formica was cleaned and disinfected between trials as previously described by Nkemngong et al., 2020. Briefly, the surface was wetted with a 10% bleach solution, followed by rinsing with sterile deionized water. It was then followed by a standard house-hold neutral agent, containing 0.05% Thymol, to reduce chemical residue on the prepared surface. The neutralizing agent was allowed to sit for its recommended contact time (two minutes) before following with a second rinse with sterile deionized water. Lastly, before surface inoculation, 70% ethanol was applied to the Formica sheet and allowed to air dry.
A total of 50 μL of approximately 5.0 × 108 log10 CFU/ml in 10 μL aliquots (2.5 × 107 CFU) were dispensed unto the i-zone, and the wiping procedure followed a modified version of the EPA SOP MB-33-00 for S. aureus and P. aeruginosa [26]. Once inoculated, the culture was allowed to air-dry before using the towelette to wipe the surface from the i-zone to the 2.0 m2 mark (Fig. 1). From each RTU disinfectant product, the first two towelettes were discarded and the third towelette was used for testing, to ensure it was fully loaded with disinfectant liquid. The wiping process began at the bottom left corner of the Formica board (below where the board was inoculated) and was wiped evenly in an up-down pattern with consistent speed and pressure from the i-zone to the 2.0 m2 mark. Once the wiping procedure was complete, the disinfectant was left undisturbed for its label-defined contact time (Table 1). At the end of the contact time, the towelette itself was placed in a sterile stomacher bag with 50 mL of 0.52% neutralizing buffer (BD Difco, Becton, Dickinson and Company, MD, USA). Swab samples were also collected from standard 10 cm × 10 cm (100 cm2) sampling areas within each partitioned zone (i-zone, 0.5m2, 1.0 m2, 1.5m2 and 2.0m2). Samples for S. aureus or P. aeruginosa detection were collected using PUR-Blue Swabs (World BioProducts, Libertyville, IL; with 10 mL sterile HiCap neutralizing buffer).
Pathogen detection and enumeration
After the wiping procedure and sample collection, each swab sampler was vortexed for 30s to release bacteria cells from the sponge of the swab sampler into 10 mL sterile neutralizing buffer (World BioProducts, Libertyville, IL). Used towelettes in 50 mL of 0.52% neutralizing buffer (BD Difco, Becton, Dickinson and Company, MD, USA) were stomached at 200 rpm for 5 min to release bacteria cells trapped on the towelettes into the neutralizing buffer. Ten mL aliquots from swab samplers and wipe samples were vacuum-filtered onto sterile filter membranes (0.2 μm pore; Pall Corporation, Port Washington, NY) and plated on tryptic soy agar (TSA; BD Biosciences, San Jose, CA) for S. aureus and Reasoner’s 2A agar (R2a; Becton, Dickinson and Company Sparks, MD) for P. aeruginosa. Plates were incubated at 37 °C for 24 ± 2 h prior to counting colony forming units (CFU).
Statistical analyses
S. aureus and P. aeruginosa were recovered after wiping five separate test zones of a two-meter square Formica sheet and recovered CFU were log10 -transformed. The disinfectant towelette was also tested for viable S. aureus and P. aeruginosa CFU post-disinfection of the two-meter square surface area. Average log10 CFU loads were calculated for towelettes and sampled surface areas, which were used to test for statistically significant differences among six disinfectant products. The least squares method of the Proc Glimmix test was used to fit linear models (n = 36, α = 0.05) and interactions amongst disinfectant products, sampled surfaces, and log10 densities on towelettes. Treating both the product type and surface area as continuous variables throughout the data analysis, Tukey adjustments were used to analyze statistically significant differences between mean log10 CFU/100 cm2 counts recovered post-disinfection on surface areas treated. The same procedure was used to test for significant differences among average log10 CFU on used disinfectant towelettes. All statistical tests were conducted using SAS version 9.4 (SAS institute, Cary, NC).
Results
S. aureus detected on previously uncontaminated surfaces post-disinfection with towelettes
Irrespective of disinfectant product, ready-to-use disinfectant towelettes transferred S. aureus to previously uncontaminated surfaces from the i-zone (Figs. 2 & 3). Overall, the towelettes transferred on average, 0.19 ± 0.18 and 0.21 ± 0.21 log10 CFU/100 cm2 to the 0.5 m2 and 1.0 m2 surface areas, respectively. Disinfectant towelettes also transferred a mean of 0.20 ± 0.19 and 0.27 ± 0.34 log10 CFU/100 cm2 from the i-zone to the 1.5 m2 and 2.0 m2 surface areas regardless of the product being tested.
Regardless of the sampling zone, there were no statistically significant differences among the log10 CFU/100 cm2 detected from previously uncontaminated surfaces when wipes were challenged with S. aureus (P > 0.3499; Figs. 2 & 3). The product type was also not statistically relevant overall (P > 0.0756). Specifically, none of the products transferred statistically significant different log10 CFU/100 cm2 to the 0.5 m2, 1.0 m2, 1.5 m2 and 2.0 m2 compared to the log10 CFU/100 cm2 recovered from the i- zone post-disinfection (P > 0.05; Figs. 2 & 3).
Varying levels of P. aeruginosa were transferred by disinfectant wipes to uncontaminated surfaces
P. aeruginosa was transferred from the i-zone to previously uncontaminated low-risk surfaces by ready-to-use disinfectant towelettes (Figs. 4 & 5). When transfer levels for all wipes were averaged, a mean of 0.37 ± 0.33 log10 CFU/100 cm2 and 0.27 ± 0.23 log10 CFU/100 cm2 were transferred from the i-zone to the 0.5 m2 and 1.0 m2 surface areas respectively. From the i-zone to the 1.5 m2 and 2.0 m2 surface areas, each towelette transferred an average of 0.31 ± 0.26 and 0.35 ± 0.27 log10 CFU/100 cm2, respectively, onto hard nonporous low risk surfaces regardless of the product type.
Regardless of the sampling zone, the surface area wiped was statistically significant, and there were relevant differences between the i-zone and uncontaminated surfaces (P < 0.0001; Figs. 4 & 5 . Irrespective of product type, the average log10 CFU/100 cm2 transferred to the 0.5 m2, 1.0 m2, 1.5 m2 and 2.0 m2 surface areas were significantly lower than the log10 CFU/100 cm2 recovered from the i- zone after surface disinfection (P < 0.05). There were no statistically significant differences in the mean log10 CFU/100 cm2 between the 0.5 m2, 1.0 m2, 1.5 m2 and 2.0 m2 uncontaminated surface areas (P ≥ 0.05; Figs. 4 & 5).
Product type was statistically relevant (P < 0.0001; Figs. 3 & 4). Within the i-zone, QA1 and QA3 had a significantly lower log10 reduction than QA2 (P < 0.05; Fig. 5). Specifically, QA2 transferred significantly higher log10 CFU/100 cm2 from the i-zone to the uncontaminated surface areas (0.5 m2, 1.0 m2, 1.5 m2, and 2.0 m2) than QA1 or QA3 (P < 0.05; Fig. 5). Within the i-zone, HP2 and HP3 were not statistically significantly different ((P ≥ 0.05; Fig. 4). However, HP3 had a significantly higher log10 reduction (lower log10 CFU/100 cm2) compared to HP1 within the i-zone (P < 0.05; Fig. 4). HP2 and HP3 were also significantly lower when compared to disinfectant wipe QA2 (P < 0.05; Figs. 4 & 5). There was, however, no statistically significant difference between QA2 and HP1 (P ≥ 0.05; Figs. 4 & 5). There were also no statistically significant differences in the mean log10 CFU/100 cm2 among HP1, HP2, HP3, QA1, and QA3 (P ≥ 0.05; Figs. 4 & 5).
The cross-contamination risk presented by disinfectant towelettes varies between S. aureus and P. aeruginosa
The surface area wiped and strain type were statistically significant (P < 0.0001). Overall, disinfectant towelettes transferred significantly higher log10 CFU/100 cm2 of P. aeruginosa than S. aureus to previously uncontaminated surfaces (P < 0.05) and there were significant differences among the tested products (P < 0.05). For both S. aureus and P. aeruginosa, surfaces wiped with HP3, QA1, and QA3 had significantly lower log10 CFU/100 cm2 post-disinfection than HP1 and QA2 (P < 0.05). Similarly, for both S. aureus and P. aeruginosa, the log10 CFU/100 cm2 detected from the i-zone for HP1 and HP2 were statistically similar after disinfection (P ≥ 0.05; Figs. 2 & 4).
Viable P. aeruginosa and S. aureus were found on disinfectant towelettes after use
Overall, the bacterial log10 CFU remaining on towelettes after disinfection based on the product type used was statistically significant for S. aureus (P < 0.0053) and P. aeruginosa (P < 0.0001). For S. aureus, log10 CFU/wipe ranged from 1.09 ± 0.41 for HP3 to 2.96 ± 0.54 for HP1. Residual P. aeruginosa ranged from 0.94 ± 0.13 for HP3 to 2.69 ± 0.78 for QA1 (Fig. 6). When comparing S. aureus and P. aeruginosa, strain type was significant (P = 0.0038, Fig. 6). Post-disinfection, all products had a significantly higher mean log10 CFU/ towelette of P. aeruginosa than S. aureus (P < 0.05; Fig. 6). Regardless of strain, HP3 wipes had significantly lower average log10 CFU/towelette than HP1, HP2, QA1 and QA3 after use (P < 0.05; Fig. 6). The mean log10 CFU/wipe for HP3 and QA2 post-disinfection were not significantly different (P > 0.05; Fig. 6) and were not different by strain.
Mean log10 CFU remaining on used towelettes post-disinfection with quaternary ammonium alcohol and hydrogen peroxide disinfectant towelettes for S. aureus and P. aeruginosa. a, ab, b Tukey grouping (mean comparison) for S. aureus; x, xy, y Tukey grouping for P. aeruginosa. Bars with the same letter are not statistical different
Among the wipes used to disinfect surfaces inoculated with S. aureus, there were no statistically significant differences among QA1, QA2, or QA3 (P ≥ 0.05; Fig. 6). For the HP products, HP1 had significantly higher log10 CFU/towelette than HP2 and HP3 (P < 0.05; Fig. 6). Similarly, HP1 had significantly higher log10 CFU/ towelette than QA1, QA2 and QA3 (P < 0.05; Fig. 6). However, there were no statistically significant differences in the log10 CFU/ towelette among HP2, HP3, QA1, QA2, and QA3 after use (P ≥ 0.05; Fig. 6).
Among the wipes used to disinfect P. aeruginosa, there were no significant differences in the mean log10 CFU/ towelette among QA1, QA2 and QA3 (P > 0.05; Fig. 6) after use. However, for the accelerated HP products, HP3 had the lowest log10 CFU/ towelette and was statistically significant in comparison to disinfectant towelettes of HP2 post-disinfection (P < 0.05; Fig. 6). There were, however, no significant differences between the average log10 CFU/wipe between HP1 and HP3 (P > 0.05; Fig. 6). Similarly, there were no statistically relevant differences in the average log10 CFU detected on towelettes of HP1, QA2 and QA3 (P > 0.05; Fig. 5) and between HP2 and QA1 towelettes post-disinfection P > 0.05; Fig. 6).
Discussion
In this study, we evaluated the cross-contamination risk that may be presented by disinfectant towelettes during and after the wiping process. During the wiping procedure, disinfectant towelettes transferred the test pathogens from the i-zone to uncontaminated surfaces (0.5 m2, 1.0 m2, 1.5 m2 and 2.0 m2), with significant differences between the log10 CFU/100 cm2 transferred by the products tested. We also found that post-disinfection, all used towelettes retained some level of S. aureus or P. aeruginosa, with some significant differences among the tested products. Overall, HP3, QA1 and QA3 had higher log10 reductions than the other products tested.
Used disinfectant wipes are potential cross-contamination agents for S. aureus
Overall, the tested disinfectant towelettes transferred S. aureus from the i-zone to previously uncontaminated surfaces. This is similar to findings by Ramm et al. who studied the potential for detergent wipes to transfer S. aureus from a contaminated stainless steel surface onto three other surfaces [27]. Specifically, Ramm et al. found that all seven disinfectant towelettes tested cross-contaminated the sterile stainless steel surfaces [27]. The transfer of pathogens to hard nonporous surfaces as demonstrated by our study is particularly important as pathogens are more easily transferred from hard nonporous surfaces to human hands than from porous surfaces [28].
We found no significant differences among the log10 CFU/100 cm2 remaining on uncontaminated surfaces post-disinfection. In a similar study with methicillin resistant S. aureus (MRSA) inoculated on stainless steel discs, Williams et al. did not find significant differences in the log10 CFU detected post-disinfection with towelettes [29]. While overall there were no significant differences in the log10 CFU/100 cm2 of S. aureus transferred among all six products we tested, QA1 transferred significantly lower log10 CFU/100 cm2 to the 1.5 m2 zone than all the other products. This difference may be accounted for by the high alcohol content (55% alcohol) of QA1 (Table 1).
Quaternary ammonium towelettes transfer more P. aeruginosa than hydrogen peroxide towelettes
Hydrogen peroxide products transferred significantly less log10 CFU/100 cm2 to previously uncontaminated surfaces than QA products. This is similar to previous findings by our group where we demonstrated that hydrogen peroxide disinfectant towelettes were more bactericidal against S. aureus and P. aeruginosa inoculated on 97 mm Formica disc than quaternary alcohol towelettes [18]. This significant difference could be explained by the potential for accelerated HP products to produce hydroxyl free radicals which are generally more bactericidal than quaternary alcohols [20]. Moreover, Edwards et al. reported that the number of bacterial cells transferred from contaminated to uncontaminated surfaces is dependent on the disinfectant active ingredient type loaded unto the towelettes [30]. This further emphasizes the role disinfectant chemistry plays in the cross-contamination levels observed in our study.
Among the QA products, QA1 and QA3 had a significantly higher log10 reduction within the i-zone and also presented a significantly lower cross-contamination risk to uncontaminated surfaces than QA2. Although QA1 and QA3 have differences in their alcohol contents (55% for QA1 and 14.3% for QA3), they had very similar quaternary ammonium contents (0.25% for QA1 and 0.233% for QA3). The similar levels of quaternary ammonium compounds between QA1 and QA3 may have been optimal enough to complement and enhance the bactericidal efficacy of the alcohol levels in these products. This is specifically important as in 2015, Gerba reported that the efficacy of quaternary ammonium compounds is dependent on the product formulation [31].
P. aeruginosa is a higher cross-contamination risk from towelettes than S. aureus
Disinfectant towelettes transferred significantly higher log10 CFU/100 cm2 of P. aeruginosa than S. aureus. The lipopolysaccharides (LPS) in the outer membrane of Gram negative bacteria may serve as a barrier offering reduced permeability to some disinfectants as this has been specifically demonstrated with quaternary ammonium compounds [32]. In a 2002 study that evaluated the transfer rate of Gram positive and Gram negative bacteria from hard nonporous fomites to the hands of workers, it was found that Gram positive bacteria transfer rates were higher [28].
Regardless of strain, the cross-contamination risk presented by disinfectant towelettes was highly product-dependent as HP3, QA1 and QA3 wipes had significantly lower log10 CFU/100 cm2 post-disinfection than HP1 and QA2. The observed differences may be explained by factors as differences in the wipe material type [33], active ingredient class [17], and differences in the amount of liquid released onto the test surfaces [18] during the wiping process. The disinfectant towelette substrate type has been demonstrated to play a major role in the physical removal of pathogens from test surfaces [34]. In a 2013 study that compared the bactericidal efficacy of different towelette substrate types composed of either cellulose, cotton, microfiber and a blend of cotton and cellulose loaded with silver dihydrogen citrate, it was found that substrates with a mix of cellulose and cotton were more bactericidal [33]. This may be the case as substrates with cellulose/cotton blends may absorb more disinfectant liquids than the other substrate types tested. It is also likely that differences in the amount of liquid dispensed from the towelettes account for differences we observed in this study and as previously reported [18].
Used disinfectant wipes are potential reservoirs for recontamination after use
After wiping the Formica sheet, all the disinfectant wipes we tested retained some level of S. aureus or P. aeruginosa. This is similar to findings by Cheng et al. who reported MRSA on disinfectant towelettes after use on bedrails [35]. This suggests that disinfectant towelettes could continue to pose a cross-contamination risk if used on larger surfaces (e.g. two meters square surface used in this study). Moreover, in a 2015 study, Ramm et al. reported that detergent towelettes are designed to efficiently pick up and retain microorganisms but that this did not always occur [27]. This finding is consistent with our study as towelettes retained viable cells after disinfection and while the level of risk varies significantly by product for Pseudomonas, there is some level of risk of cross-contaminate for all the wipes studies. An observational study by Williams et al. reported that environmental staff in healthcare facilities used a single disinfectant towelette on at least five different surfaces during routine cleaning and disinfection [36]. This further emphasizes the risk that some disinfectant towelettes present when they retain high levels of common pathogens causing HAI and are used on multiple surfaces by healthcare personnel. Post-disinfection, wipes were found to have significantly higher mean log10 CFU of P. aeruginosa than S. aureus. The rod shape of P. aeruginosa [37] may have allowed for a better fit into the perforations on the tested towelettes compared to S. aureus cocci [38]. Our study is limited as the impact of the wipe material type was not specifically evaluated. In addition, we did not study the cross-contamination risk towelettes may present in the presence of soil loads.
Conclusion
Overall, disinfectant towelettes transferred viable CFU of S. aureus and P. aeruginosa from the point of inoculation to uncontaminated surfaces, while retaining viable bacterial loads post-disinfection. The results of this study underscore the risk of spreading S. aureus and P. aeruginosa during and after the wiping process by some products. Considering that bacterial biofilms are more prevalent in nature than planktonic bacteria, conducting similar studies against biofilms on environmental surfaces may provide more insights into the possible cross-contamination risk that disinfectant towelettes present. We also recommend conducting similar studies using other Gram negative and Gram positive bacteria relevant in healthcare settings, as well as with mixed cultures to further understand the likely differences in the cross-contamination risk under relevant healthcare scenarios.
Availability of data and materials
All quantitative data generated or analyzed during this study are included in this published article.
Abbreviations
- ACH:
-
Acute Care Hospital
- CFU:
-
Colony Forming Units
- EPA:
-
Environmental Protection Agency
- HAI:
-
Healthcare Associated Infections
- HP:
-
Hydrogen Peroxide
- QA:
-
Quaternary ammonium
- TSA:
-
Tryptic Soy Agar
References
Office of Disease Prevention and Health Promotion. Healthcare-associated infections. Healthy People. ODPHP. 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/healthcare-associated-infections. Accessed 4 Feb 2020.
Center for Disease Control. National and state healthcare-associated infections progress report, vol. 2017: CDC; 2017. https://www.cdc.gov/hai/data/archive/2017-HAI-progress-report.html. Accessed 28 Oct 2019.
Magill SS, O’Leary E, Janelle SJ, Thompson DL, Dumyati G, Nadle J, Wilson LE, Kainer MA, Lynfield R, Greissman S, Ray SM, Beldavs Z, Gross C, Bamberg W, Sievers M, Concannon C, Buhr N, Warnke L, Maloney M, Ocampo C, Brooks J, Oyewumi T, Sharmin S, Richards K, Rainbow J, Samper M, Hancock EB, Leaptrot D, Scalise E, Badrun F, Phelps R, Edwards JR. Changes in prevalence of health-care associated infection in U.S. hospitals. N Engl J Med. 2018;379:1732–44.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32.
Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28:603–61.
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, Kallen A, Limbago B, Fridkin S. National Healthcare Safety Network (NHSN) Team and Participating NHSN Facilities. Antimicrobial-resistant pathogens associated with healthcare-associated infections summary of data reported to the national healthcare safety network at the centers for disease control and prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013;34:1–14.
Ondusko DS, Nolt D. Staphylococcus aureus. Pediatr Rev. 2018;39:287–98.
Bhagirath AY, Yanqi L, Somayajula D, Dadashi M, Badr S, Duan K. Cysitic fibrosis lung environment and Pseudomonas aeruginosa infection. BMC Pulm Med. 2016;16:174.
Driscoll JA, Brody SL, Kollef MH. The epidemiology, pathogenesis and treatment of Pseudomonas aeruginosa infections. Drugs. 2007;67:351–68.
Leas BF, Sullivan N, Han JH, Pegues DA, Kaczmarek JL, Umscheid CA. Environmental cleaning for the prevention of healthcare-associated infections. Rockville: Agency for Healthcare Research and Quality (US); 2015. (Technical Briefs, No. 22) Available from: https://www.ncbi.nlm.nih.gov/books/NBK311016/. Accessed 2 Nov 2019.
Russotto V, Cortegiani A, Maurizio Raineri S, Giarratano A. Bacterial contamination of inanimate surfaces and equipment in the intensive care unit. J Intensive Care. 2015;3:54.
Ohashi Kurashige EJ, Oie S, Furukawa H. Contamination of environmental surfaces by methicillin-resistant Staphylococcus aureus (MRSA) in rooms of inpatients with MRSA-positive body sites. Braz J Microbiol. 2016;47:703–5.
Dancer SJ. Controlling hospital-acquired infection: focus on the role of the environment and new technologies for decontamination. Clin Microbiol Rev. 2014;27:665–90.
Chemaly RF. The role of the healthcare environment in the spread of multidrug-resistant organisms: update on current best practices for containment. Ther Adv Infect Dis. 2014;2:79–90.
Slany M, Oppelt J, Cincarova L. Formation of Staphylococcus aureus biofilm in the presence of sublethal concentrations of disinfectants studied via a transcriptomic analysis using transcriptome sequencing (RNA-seq). Appl Environ Microbiol. 2017. https://doi.org/10.1128/AEM.01643-17.
Bridier A, Briandet R, Thomas V, Dubois-Brisonett F. Resistance of bacterial biofilms to disinfectants: a review. Biofouling. 2011;27:1017–32.
Lineback CB, Nkemngong CA, Wu T, Li X, Teska PJ, Oliver HF. Hydrogen peroxide and sodium hypochlorite disinfectants are more effective against Staphylococcus aureus and Pseudomonas aeruginosa biofilms than quaternary ammonium compounds. Antimicrob Resist Infect Control. 2018; https://doi.org/10.1186/s13756-018-0447-5 -5.
West AM, Nkemngong CA, Voorn MG, Wu T, Li X, Teska PJ, Oliver HF. Surface area wiped, product type, and target strain impact bactericidal efficacy of ready-to-use disinfectant towelettes. Antimicrob Resist Infect Control. 2018. https://doi.org/10.1186/s13756-018-0416-z.
Boyce JM. Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob Resist Infect Control. 2016. https://doi.org/10.1186/s13756-016-0111-x.
Center for Disease Control. Guideline for disinfection and sterilization in healthcare facilities: CDC; 2008. https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf. Accessed 30 Oct 2019.
Han JH, Sullivan N, Leas BF, Pegues DA, Kaczmarek JL, Umscheid CA. Cleaning hospital room surfaces to prevent healthcare-associated infections. Ann Intern Med. 2015;163:598–607.
Ríos-Castillo AG, González-Rivas F, Rodríguez-Jerez JJ. Bactericidal efficacy of hydrogen peroxide-based disinfectants against gram-positive and gram-negative bacteria on stainless steel surfaces. J Food Sci. 2017;82:2351–6.
Sattar AS, Bradley C, Kibbee R, Westgate R, Wilkinson MA, Sharpe T, Maillard JY. Disinfectant wipes are appropriate to control microbial bioburden from surfaces: use of a new ASTM standard test protocol to demonstrate efficacy. J Hosp Infect. 2015;91:319–25.
McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev. 1999;12:147–79.
Song X, Vossebein L, Zille A. Efficacy of disinfectant-impregnated wipes used for surface disinfection in hospitals. Antimicrob Resist Infect Control. 2019. https://doi.org/10.1186/s13756-019-0595-2.
Environmental Protection Agency. Standard operating procedure for quantitative petri plate method (QMP) for determining the effectiveness of antimicrobial towelettes against vegetative bacteria on inanimate, hard, and non-porous surfaces: MB-33-00: EPA; 2014. https://www.epa.gov/sites/production/files/2014-12/documents/mb-33-00.pdf. Accessed 30 Oct 2019.
Ramm L, Siani H, Wesgate R, Maillard JY. Pathogen transfer and high variability in pathogen removal by detergent wipes. Am J Infect Control. 2015;43:724–8.
Rusin P, Maxwell S, Gerba C. Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria, and phage. J Appl Microbiol. 2002;93:585–92.
Williams GJ, Denyer SP, Hosein IK, Hill DW, Maillard JY. The development of a new three-step protocol to determine the efficacy of disinfectant wipes on surfaces contaminated with Staphylococcus aureus. J Hosp Infect. 2007;67:329–35.
Edwards NWM, Best EL, Connell SD, Goswami P, Carr CM, Wilcox MH, Russell SJ. Role of surface energy and nano-roughness in the removal efficiency of bacterial contamination by nonwoven wipes from frequently touched surfaces. Sci Technol Adv Mater. 2017;18:197–209.
Gerba CP. Quaternary ammonium biocides: efficacy in application. J Appl Environ Microbiol. 2014;81:464–9.
Macgregor DR, Elliker PR. A comparison of some properties of strains of Pseudomonas aeruginosa sensitive and resistant to quaternary ammonium compounds. Can J Microbiol. 1958;4:499–503.
Masuka SM, Babu D, Martin EM, Koo OK, O’BRyan CA, Crandall PG, Ricke SC. Cleaning and decontamination efficacy of wiping cloths and silver dihydrogen citrate on food contact surfaces. J Appl Microbiol. 2012;113:89–95.
Gold KM, Hitchins VM. Cleaning assessment of disinfectant cleaning wipes on an external surface of a medical device contaminated with artificial blood or Streptococcus pneumoniae. Am J Infect Control. 2013;41:901–7.
Cheng KL, Boost MV, Chung JW. Study on the effectiveness of disinfection with wipes against methicillin-resistant Staphylococcus aureus and implications for hospital hygiene. Am J Infect Control. 2011;39:577–80.
Williams GJ, Denyer SP, Hosein IK, Hill DW, Maillard JY. Limitations of the efficacy of surface disinfection in the healthcare setting. Infect Control Hosp Epidemiol. 2009;30:570–3.
Elomari M, Coroler L, Verhille S, Izard D, Leclerc H. Pseudomonas monteilii sp. nov., isolated from clinical specimens. Int J Syst Bacteriol. 1997;47:846–52.
Singh N, Paterson DL, Chang FY, Gayowski T, Squier C, Wagener MM, Marino IR. Methicillin-resistant Staphylococcus aureus: the other emerging resistant gram-positive coccus among liver transplant recipients. Clin Infect Dis. 2000;30:322–7.
Acknowledgements
Dr. Oliver is supported by the USDA National Institute of Food and Agriculture Hatch project 2016-67017-24459. The authors thank Gurpreet K. Chaggar for reviewing and editing the manuscript.
Funding
This work was supported by Diversey Inc., Charlotte, NC, USA.
Author information
Authors and Affiliations
Contributions
MGV, SEG and CAN performed trials, collected, analyzed and interpreted the data generated, and wrote the manuscript. XL provided industry experience, designed elements of the experimental protocol, and was a contributor in writing and editing the manuscript. PT also provided industry experience and was a contributor in writing and editing the manuscript. HFO served as the principal investigator for the study and was a contributor in writing and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
HFO, MGV, SEG, and CAN report grants from Diversey, Inc. during the conduct of the study. PT and XL report grants from Diversey, Inc. during the conduct of the study; personal fees from Diversey, Inc., outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Voorn, M.G., Goss, S.E., Nkemngong, C.A. et al. Cross-contamination by disinfectant towelettes varies by product chemistry and strain. Antimicrob Resist Infect Control 9, 141 (2020). https://doi.org/10.1186/s13756-020-00797-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-020-00797-4