Abstract
Background
Intraoperative hypotension (IOH) is well-described in the academic setting but not in community practice. IOH is associated with risk of postoperative morbidity and mortality. This is the first report of IOH in the community setting using the IOH measure definition from the Centers for Medicare and Medicaid Services Merit-based Incentive Payment System program. Objectives: To describe the incidence of IOH in the community setting; assess variation in IOH by patient-, procedure-, and facility-level characteristics; and describe variation in risk-adjusted IOH across clinicians.
Methods
Design
Cross-sectional descriptive analysis of retrospective data from anesthesia records in 2020 and 2021.
Setting
Forty-five facilities affiliated with two large anesthesia providers in the USA.
Participants
Patients aged 18 years or older having non-emergent, non-cardiac surgery under general, neuraxial, or regional anesthesia. Cases were excluded based on criteria for the IOH measure: baseline mean arterial pressure (MAP) below 65 mmHg prior to anesthesia induction; American Society of Anesthesiologists (ASA) physical status classification of I, V, or VI; monitored anesthesia care only; deliberate induced hypotension; obstetric non-operative procedures; liver or lung transplant; cataract surgery; non-invasive gastrointestinal cases.
Main outcomes
IOH, using four definitions. Primary definition: binary assessment of whether the case had MAP < 65 mmHg for 15 min or more. Secondary definitions: total number of minutes of MAP < 65 mmHg, total area under MAP of 65 mmHg, time-weighted average MAP < 65 mmHg.
Results
Among 127,095 non-emergent, non-cardiac cases in community anesthesia settings, 29% had MAP < 65 mmHg for at least 15 min cumulatively, with an overall mean of 12.4 min < 65 mmHg. IOH was slightly more common in patients who were younger, female, and ASA II (versus III or IV); in procedures that were longer and had higher anesthesia base units; and in ambulatory surgery centers. Incidence of IOH varied widely across individual clinicians in both unadjusted and risk-adjusted analyses.
Conclusion
Intraoperative hypotension is common in community anesthesia practice, including among patients and settings typically considered “low risk.” Variation in incidence across clinicians remains after risk-adjustment, suggesting that IOH is a modifiable risk worth pursuing in quality improvement initiatives.
Similar content being viewed by others
Background
Intraoperative hypotension (IOH) is associated with adverse myocardial, renal, and neurological outcomes; increased hospital length of stay; and postoperative mortality (Ahuja et al. 2020; An et al. 2019; Bijker and Gelb 2013; Bijker et al. 2012, 2009; Brady et al. 2020; Futier et al. 2017; Gregory et al. 2021; Gu et al. 2018; Huang et al. 2020; Maheshwari et al. 2020; Mathis et al. 2020; Monk et al. 2016; Radinovic et al. 2019; Salmasi et al. 2017; Sessler et al. 2019; Wesselink et al. 2018; Wijnberge et al. 2021). Associations are well-documented and consistent across observational studies and across multiple blood pressure thresholds (Ahuja et al. 2020; An et al. 2019; Sessler et al. 2019). However, they are generally studied at major academic centers, with limited data on IOH in community anesthesia practice where a significant portion of annual anesthetics are estimated to occur (Almanac 2021).
Anesthesia clinicians routinely monitor intraoperative blood pressure and maintain hemodynamic stability. The American Society of Anesthesiologists (ASA) standard for intraoperative blood pressure monitoring includes a minimum of one reading every 5 min (American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring 2010), and the Perioperative Quality Initiative consensus statement recommends maintaining systolic arterial pressure above 100 mmHg and mean arterial pressure (MAP) above 60–70 mmHg (Sessler et al. 2019). To aid in monitoring and reducing IOH, a risk-adjusted, clinician-level measure was developed to assess intraoperative hemodynamic control during non-emergent non-cardiac surgery (Christensen et al. 2021). This measure—the “IOH measure”—assesses the percent of cases with MAP below 65 mmHg for 15 min or more cumulatively, risk-adjusted for patient age, sex, body-mass-index (BMI), ASA physical status, and surgery length. The IOH measure has been reported in the Centers for Medicare and Medicaid Services (CMS) Merit-based Incentive Payment System (MIPS) as a Qualified Clinical Data Registry measure since 2020. While there are many ways to define IOH (Bijker et al. 2007), the IOH measure is one validated method using blood pressure readings recorded in the anesthesia information management system (AIMS). It is also supported by the ASA and utilized as a federal quality measure.
The aims of this manuscript are to assess the incidence of IOH in community anesthesia practice, to describe variations in the incidence of IOH across subgroups of patients and surgical procedures, and to assess whether incidence of IOH varies among clinicians after controlling for risk factors.
Methods
Study approval
The Health Media Lab Institutional Review Board (IRB) reviewed this study and determined it met criteria for IRB exemption, in accordance with the US Code of Federal Regulations for the Protection of Human Subjects, 45 CFR 46.104. The requirement for written informed consent was waived by the IRB. The study was conducted in accordance with the appropriate Enhancing the QUAlity and Transparency Of health Research (EQUATOR) guidelines.
Data sources
Two anesthesia practices (NorthStar Anesthesia [NSA] and US Anesthesia Partners [USAP]) collaborated on this study. Each practice extracted retrospective data from their AIMS, electronic health records (EHR), and/or billing systems on non-emergent, non-cardiac cases from 2020 and 2021, from a subset of facilities that store the perioperative blood pressure readings in the AIMS. One practice used their qualified clinical data registry vendor to supply data, and the other relied on their quality improvement department. Researchers from outside the practices determined which covariates each practice could provide in structured fields. Data included: blood pressure readings taken approximately every 1–5 min, patient characteristics (age, sex, BMI, ASA physical status classification), procedure characteristics (anesthesia procedure code, surgery length), and facility type (ambulatory surgical center [ASC] or hospital). We did not have access to information on the anesthesia coverage model or anesthesia clinician type (e.g., anesthesiologist, certified registered nurse anesthetist), although the majority of cases were performed in an anesthesia care team model with collaboration between anesthesiologists and anesthetists. We also did not collect data regarding vasoactive medication use or choice of anesthetic agent. The data were reviewed and put into a uniform structure and thorough data quality checks were conducted.
Study sample
Surgical cases were included in the analysis if they met criteria for the IOH measure: patients aged 18 years or older having non-emergency, non-cardiac surgeries (including elective and urgent surgeries) under general, neuraxial, or regional anesthesia care. Cases also must have included one of the 220 anesthesia CPT codes eligible for the IOH measure. Surgical cases were excluded from this analysis if they met exclusion criteria for the IOH measure: baseline MAP below 65 mmHg; ASA physical status classification I, V, or VI; monitored anesthesia care only; induced hypotension (using CPT add on code 99,135); obstetric non-operative procedures; liver or lung transplant; cataract surgery; non-invasive gastrointestinal cases.
Outcomes
We assessed IOH using four definitions. The primary definition aligned with the IOH measure and is a binary assessment of whether the case had MAP < 65 mmHg for at least 15 min, cumulatively. Secondary definitions of IOH included: the total number of minutes of MAP < 65 mmHg, the total area under MAP of 65 mmHg, and the time-weighted average (TWA) MAP < 65 mmHg. Total area under 65 mmHg was calculated as follows: for each blood pressure episode below 65 mmHg, we calculated the area as the units of mmHg below 65 mmHg (depth of hypotension), multiplied by the length (in minutes) between the index blood pressure reading and the next reading (duration of hypotension). The areas were then summed across all hypotensive episodes during the case to arrive at the total area (Maheshwari et al. 2018). TWA MAP < 65 mmHg was calculated as the total area under 65 mmHg divided by the surgery length in minutes. Because blood pressure data can contain artifactual values, we dropped readings documented as an artifact by the clinician, systolic blood pressure (SBP) ≥ 300 mmHg or ≤ 20 mmHg, diastolic blood pressure (DBP) ≤ 5 mmHg or ≥ 225 mmHg, SBP, and DBP within 5 mmHg, MAP ≤ 30 mmHg or ≥ 250 mmHg.
To calculate IOH, each blood pressure reading was attributed to the period from the time the reading was recorded to the time of either the next reading or the anesthesia end time, capped at 5 min maximum.
Statistical analysis
We assessed the incidence of IOH in the full sample using the four definitions described above. To describe the depth and duration of hypotension among cases that met the primary definition, we calculated the secondary definitions, stratified by whether cases met the primary definition. To determine the variation in hypotension across subgroups, we calculated IOH by patient characteristic, procedure characteristic, and facility type. ASA physical status classification was a proxy for patient comorbidities. Anesthesia base units, which are procedure-specific values that partially determine anesthesia payments, were a proxy for procedure complexity. Chi-square tests assessed the statistical significance of the variation. We also calculated IOH for the 10 most common anesthesia procedure codes in the sample.
For analyses of clinician-level variation in IOH, we attributed each case to the clinician(s) included on the anesthesia record. We limited to clinicians with at least 30 cases during the study period to ensure reliable estimates, based on data-driven recommendations from the measure developers (Christensen et al. 2021). For each clinician, we calculated the unadjusted and risk-adjusted versions of the IOH measure and the TWA. The risk-adjusted IOH measure is calculated as an observed to expected ratio (O:E ratio); its development and validation has been described previously (Christensen et al. 2021). It is equal to the count of “observed” or actual cases of IOH during the study period, divided by the number of cases of IOH that were “expected” during the study period based on their case mix. The expected number is determined by a logistic regression model with covariates for patient age, sex, BMI, ASA physical status, and surgery length. To calculate the risk-adjusted measure in a subset of cases with missing BMI, we imputed missing values as the median BMI for the patient’s age and sex combination.
To assess whether clinicians with different rates of hypotension had different case mixes, we categorized clinicians by their risk-adjusted rates of hypotension (O:E ratios of less than 0.8, 0.8 to 1.2, greater than 1.2), then described the patient, procedure, and facility characteristics of the cases in each clinician group.
Data management and statistical analyses were performed using R software. All statistical tests were two-tailed, and P values less than 0.01 were considered significant.
Results
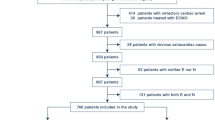
From NSA and USAP, respectively, the sample included 127,095 surgical cases (43% and 57%) from 45 facilities (10 and 35) in the midwest, southeast, and southwest regions of the USA. Cases were conducted by 663 anesthesia clinicians (49% and 51%). Supplemental Figure S1 shows the sample selection flowchart. Sample characteristics are shown in Table 1. Nearly half of cases were among patients aged 40 to 64 years. Forty-seven percent of patients were ASA physical status II; 46% were ASA physical status III. The most common surgical duration was 60–199 min (42%). Eighty-seven percent of surgeries occurred in a hospital setting, and 13% occurred in an ASC.
The incidence of IOH per the primary outcome (MAP < 65 mmHg for at least 15 min, cumulatively) was 29.0% (Table 2). Cases had a mean of 12.4 min of MAP < 65 mmHg. The mean area under MAP of 65 mmHg was 65.4 mmHg*min, and the mean time weighted average below a MAP of 65 mmHg was 0.67 mmHg. Cases that met the IOH measure numerator had an average of 36.2 min < 65 mmHg.
Incidence of IOH (defined as MAP < 65 mmHg for at least 15 cumulative minutes) differed by patient age, sex, ASA physical status, surgery length, anesthetic type, anesthesia base units, and facility type (Table 3; all Chi-square tests < 0.01). Across all four definitions of IOH, younger patients (age 18 to 39) had more IOH than older patients (age 40 to 64 and ≥ 65), and females experienced more IOH than males. Patients with ASA physical status II had the highest incidence of MAP < 65 mmHg for 15 min and had the most minutes of MAP < 65 mmHg; however, patients with ASA physical status IV had the highest area under MAP of 65 mmHg and highest time weighted average MAP below 65 mmHg. Using three definitions of IOH, the incidence increased steadily with increasing surgery length; however, once time-weighted, patients with surgeries between 60 and 119 min long had the greatest time-weighted average MAP < 65 mmHg. Cases with regional anesthesia had more IOH than those with general or neuraxial anesthesia for three of the definitions of IOH. Using three definitions of IOH, the incidence increased with increasing anesthesia complexity (base units); however, once time-weighted, cases with the lowest complexity (base units 0 to 5) had the greatest time-weighted average MAP < 65 mmHg.
IOH was slightly more common in ASCs than hospitals, across three of the four definitions shown in Table 3.
Among the 10 most common anesthesia procedures, incidence of IOH (defined as MAP < 65 mmHg for at least 15 min) varied from 16.9% during anesthesia for hand cases to 36.5% during anesthesia for extensive spine procedures (Table 4). The TWA ranged from 0.44 mmHg in anesthesia for lower abdominal cases including laparoscopy, to 0.96 mmHg in anesthesia for procedures on the skin (Table 4).
Clinician-level analyses
The incidence of IOH varied widely across clinicians for each of the 3 definitions of the outcome we assessed: percent of cases with MAP < 65 mmHg for ≥ 15 min (unadjusted); TWA; and risk-adjusted intraoperative hypotension using the IOH measure (Fig. 1). Clinicians varied from having 3.4 to 74.3% of their cases having MAP < 65 mmHg for at least 15 min, with a median incidence of 29.9% (not shown).
Clinicians who had at least 20% more cases of IOH than expected (O:E ≥ 1.2) had cases that were slightly younger, slightly more female, and slightly lower BMI and ASA physical status than clinicians with O:E ratios less than 0.8. Median surgery length was 2 min longer for clinicians with more hypotension than expected, compared to those with less hypotension than expected. Clinicians with more IOH had a greater proportion of cases in ASCs (19% in ASCs for clinicians with O:E ratios > 1.2; 8% in ASCs for those with O:E ratios 0.8–1.2; 7% in ASCs for those with O:E ratios < 0.8) (Supplemental material Tables S1–S6).
Discussion
In our sample of community anesthesia practice, there was a substantial occurrence of IOH using the previously-defined IOH measure, with 29% of cases having MAP < 65 mmHg for 15 min or longer. IOH has been reported in 5–99% of surgical cases (Bijker and Gelb 2013; Warner and Monk 2007; Weinberg et al. 2022). Limiting to studies that use a similar MAP threshold of 65 mmHg, the incidence of IOH ranges from 19 to 88% for MAP < 65 mmHg for at least 1 min (Bijker and Gelb 2013; Gregory et al. 2021; Shah et al. 2020), 45–49% for at least 5 min (Bijker and Gelb 2013; Shah et al. 2020), and 31% for at least 10 min (Bijker and Gelb 2013; Shah et al. 2020). Most previous studies are from major academic institutions. The incidence we observed was surprising; we presumed our study population in community anesthesia was lower risk compared to previous studies that focused on academic hospitals.
Counter-intuitively, patients under age 40 experienced more IOH than those over 65. This aligns with some (Shah et al. 2020) but not all (Gregory et al. 2021; Dai et al. 2020; Wickham et al. 2022) published reports. Clinicians may be less likely to intervene on younger patients perceived to tolerate lower pressures (Franck et al. 2011). While older patients are more predisposed to hemodynamic disturbances, it is unclear whether this is predictive of adverse outcomes (Gregory et al. 2021; Bonnet et al. 2020). IOH occurred more commonly in females than males, which aligns with published data (Gregory et al. 2021; Kalezic et al. 2013; Wickham et al. 2022). We did not report variation by BMI due to missing data. Patients with ASA physical status II experienced more minutes of IOH and were more likely to have at least 15 min of MAP < 65 mmHg, compared to patients with ASA status III or IV. This aligns with some published reports (Kalezic et al. 2013) but contrasts with others (Wickham et al. 2022). This pattern may reflect sicker patients being managed by more experienced clinicians and in better-equipped settings. Practically, sicker patients are more likely to be monitored more frequently—or more invasively—and hypotensive episodes may be shorter-lived because of earlier or more aggressive intervention (Bijker et al. 2009). However, ASA IV patients had the highest area under MAP < 65 mmHg and highest time weighted average MAP < 65 mmHg, suggesting that this group had more severe drops in blood pressure when they occurred.
Incidence of IOH increased with surgical duration across most definitions, a finding in agreement with some (Bijker et al. 2009; Südfeld et al. 2017; Sun et al. 2015) but not all (Ahuja et al. 2020; Franck et al. 2011; Kalezic et al. 2013) reports. The time-weighted average of IOH was higher among shorter surgeries and highest among surgeries lasting 1–2 h. This may be because anesthetic induction is a period of risk for IOH, and the induction period makes up a larger proportion of shorter surgeries versus longer surgeries.
The majority (96.6%) of analyzed cases qualified as general anesthetics with 28.6% incidence of IOH. Reliable comparisons between different anesthetics cannot be made since anesthetic type was determined by the highest level anesthetic administered. Anesthesia base units were used as a practical surrogate of anesthetic complexity. Most cases were lower complexity (0–5 base units) or intermediate complexity (6–10 base units). High complexity cases (11 or greater base units) were least common but had the highest incidence of MAP < 65 for at least 15 min (33.5%) compared to intermediate (29.1%) and low complexity (28.2%) cases. However, in the time-weighted definition of IOH, the lowest complexity cases (base units 0 to 5) had the highest TWA MAP < 65 mmHg.
Incidence of IOH was higher in ASCs than in hospitals, using three of the four definitions of IOH, including TWA. Our median surgery length was only 21 min shorter in ASCs than in hospitals (65 versus 86 min) (Supplemental material Table S7). This result may reflect trends in management of IOH in ASCs, where patients are presumed to be healthier (less intensively monitored), or sites are less prepared to escalate IOH treatment.
The incidence of IOH varied across clinicians. Counter-intuitively, clinicians with worse scores on the risk-adjusted IOH measure were generally caring for younger patients with lower ASA physical status and were more likely in an ASC. This suggests that variation in IOH at least partially results from differences in clinician behavior or assessment of risk, as opposed to simply being driven by patient risk factors. Hence, IOH—generally attributed to pre-existing conditions and higher-risk procedures (Mathis et al. 2020; Wickham et al. 2022)—may be an appropriate target for quality improvement.
This analysis has limitations. The data represent a convenience sample from two large anesthesia practices. Despite including 45 facilities in multiple U.S. regions, data may not be nationally representative. Our study population is limited to non-emergent non-cardiac surgical procedures and the facilities that contributed data do not use unified hemodynamic monitoring protocols. Considering the inherent limitations of retrospective and descriptive analyses, it is difficult to determine differences in IOH treatment among clinicians. We were unable to adjust the analysis based on combination anesthetics (i.e., general + regional) since the highest anesthetic intervention was allocated to each case.
BP values were either manually entered or automatically captured in the electronic record. It is reasonable to assume that manually recorded vitals would be artificially “smoothened,” but they may also omit obvious artifacts that an electronic system would include (Franck et al. 2011). However, there was not a clinically meaningful difference in IOH incidence across modes of data entry.
The IOH measure used for the clinician-level analysis is only risk-adjusted for five factors. To minimize reporting burden and limit chart reviews, the current model was limited to variables available to the anesthesia registries that calculate the measure: age, gender, BMI, ASA physical status, and surgical duration. Also, while some clinicians recommend using relative drops in blood pressure from a predefined, patient-specific baseline as a means to individualize hemodynamic management (Futier et al. 2017); absolute thresholds have been shown to be similarly predictive of morbidity (Mathis et al. 2020; Salmasi et al. 2017; Mascha et al. 2015). It is plausible that MAP < 65 mmHg is equivalent to a ≥ 20% deviation from baseline for most patients. Based on these different definitions and thresholds, it is difficult to determine which of our four IOH definitions is the best target for intervention.
We did not have outcome data to study acknowledging that IOH is consistently associated with adverse outcomes. Based on published observational analyses, it is likely that the lower the blood pressure, and the longer the episode of hypotension, the greater the risk for adverse outcomes (An et al. 2019; Bijker et al. 2009; Brady et al. 2020; Futier et al. 2017; Gregory et al. 2021; Radinovic et al. 2019; Salmasi et al. 2017; Sessler et al. 2019; Wesselink et al. 2018; Wijnberge et al. 2021; Maheshwari et al. 2018; Wickham et al. 2022). We also did not have access to comorbidity or hospital details for our population, which would have made our results more robust. Community practice sites included in this analysis have limited resources for research, if any, and requesting that granular data was deemed not feasible within the scope of this project.
Despite limitations, this study contributes by describing IOH rates in a community anesthesia setting and suggests that the burden of IOH is not limited to complex cases in academic hospitals. That IOH is more common in “lower risk” patients/settings and that it varies across clinicians, even after risk adjustment, suggests that it is modifiable (not solely determined by the patient and case risk) and a potential target for quality improvement. By instituting educational and systematic quality efforts, IOH could be amenable to mitigation, potentially improving outcomes for many patients. Policy changes may also provide incentives to reduce IOH. A recent government report on adverse events in hospitals found that hypotension was the most common harm event related to surgeries and procedures. The report recommended that CMS update its lists of hospital acquired conditions (HAC) for the HAC Reduction Program and the Deficit Reduction Act HAC list to capture common, preventable, and high-cost harm events, potentially including IOH (Grimm 2018).
Conclusions
Intraoperative hypotension is common in community anesthesia practice, including among patients and settings typically considered “low risk.” Variation in incidence across clinicians remains after risk-adjustment, suggesting that IOH is a modifiable risk worth pursuing in quality improvement initiatives.
Availability of data and materials
The data that support the findings of this study are available from NorthStar Anesthesia and US Anesthesia Partners. Restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of NorthStar Anesthesia and US Anesthesia Partners.
Abbreviations
- AIMS:
-
Anesthesia information management system
- ASA:
-
American Society of Anesthesiologists
- ASA:
-
American Society of Anesthesiologists
- ASC:
-
Ambulatory surgical center
- BMI:
-
Body-mass-index
- CMS:
-
Centers for Medicare and Medicaid Services
- DBP:
-
Diastolic blood pressure
- HAC:
-
Hospital acquired conditions
- HER:
-
Electronic health records
- IOH:
-
Intraoperative hypotension
- IRB:
-
Institutional Review Board
- MAP:
-
Mean arterial pressure
- MAP:
-
Mean arterial pressure
- MIPS:
-
Merit based Incentive Payment System
- NSA:
-
NorthStar Anesthesia
- O:E ratio:
-
Observed to expected ratio
- SBP:
-
Systolic blood pressure
- TWA:
-
Time-weighted average
- USAP:
-
US Anesthesia Partners
References
Ahuja S, Mascha EJ, Yang D, et al. Associations of intraoperative radial arterial systolic, diastolic, mean, and pulse pressures with myocardial and acute kidney injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2020;132(2):291–306. https://doi.org/10.1097/ALN.0000000000003048.
American Society of Anesthesiologists. 2021 Anesthesia Almanac. https://www.asahq.org/research-and-publications/analytics-and-research-services. September 8, 2021. Accessed October 14, 2022.
American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring. https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring. Updated October 20, 2010. Affirmed December 13, 2020. Accessed August 22, 2022.
An R, Pang QY, Liu HL. Association of intra-operative hypotension with acute kidney injury, myocardial injury and mortality in non-cardiac surgery: a meta-analysis. Int J Clin Pract. 2019;73(10):e13394. https://doi.org/10.1111/ijcp.13394
Bijker JB, Gelb AW. Review article: the role of hypotension in perioperative stroke. Can J Anaesth. 2013;60(2):159–67. https://doi.org/10.1007/s12630-012-9857-7.
Bijker JB, van Klei WA, Kappen TH, van Wolfswinkel L, Moons KG, Kalkman CJ. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107(2):213–20. https://doi.org/10.1097/01.anes.0000270724.40897.8e.
Bijker JB, van Klei WA, Vergouwe Y, et al. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology. 2009;111(6):1217–26. https://doi.org/10.1097/ALN.0b013e3181c14930.
Bijker JB, Persoon S, Peelen LM, et al. Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology. 2012;116(3):658–64. https://doi.org/10.1097/ALN.0b013e3182472320.
Bonnet JF, Buggy E, Cusack B, et al. Can routine perioperative haemodynamic parameters predict postoperative morbidity after major surgery? [published correction appears in Perioper Med (Lond). 2020 May 29;9:19]. Perioper Med (Lond). 2020;9:9. Published 2020 Mar 24. doi:https://doi.org/10.1186/s13741-020-0139-6
Brady KM, Hudson A, Hood R, DeCaria B, Lewis C, Hogue CW. Personalizing the definition of hypotension to protect the brain [published correction appears in Anesthesiology. 2020 Jul;133(1):250]. Anesthesiology. 2020;132(1):170–179. https://doi.org/10.1097/ALN.0000000000003005
Christensen AL, Jacobs E, Maheshwari K, et al. Development and evaluation of a risk-adjusted measure of intraoperative hypotension in patients having nonemergent, noncardiac surgery. Anesth Analg. 2021;133(2):445–54.https://doi.org/10.1213/ANE.0000000000005287.
Dai S, Li X, Yang Y, Cao Y, Wang E, Dong Z. A retrospective cohort analysis for the risk factors of intraoperative hypotension. Int J Clin Pract. 2020;74(8):e13521. https://doi.org/10.1111/ijcp.13521
Franck M, Radtke FM, Prahs C, et al. Documented intraoperative hypotension according to the three most common definitions does not match the application of antihypotensive medication. J Int Med Res. 2011;39(3):846–56. https://doi.org/10.1177/147323001103900318.
Futier E, Lefrant JY, Guinot PG, et al. Effect of individualized vs standard blood pressure management strategies on postoperative organ dysfunction among high-risk patients undergoing major surgery: a randomized clinical trial. JAMA. 2017;318(14):1346–57. https://doi.org/10.1001/jama.2017.14172.
Gregory A, Stapelfeldt WH, Khanna AK, et al. Intraoperative hypotension is associated with adverse clinical outcomes after noncardiac surgery. Anesth Analg. 2021;132(6):1654–65. https://doi.org/10.1213/ANE.0000000000005250.
Grimm CA. Adverse Events in Hospitals: A Quarter of Medicare Patients Experienced Harm in October 2018. U.S. Department of Health and Human Services Office of Inspector General. U.S. Department of Health and Human Services Office of Inspector General; 2022. OEI-06–18–00400. Accessed August 23, 2022. https://oig.hhs.gov/oei/reports/OEI-06-18-00400.asp.
Gu WJ, Hou BL, Kwong JSW, et al. Association between intraoperative hypotension and 30-day mortality, major adverse cardiac events, and acute kidney injury after non-cardiac surgery: A meta-analysis of cohort studies. Int J Cardiol. 2018;258:68–73. https://doi.org/10.1016/j.ijcard.2018.01.137.
Huang WW, Zhu WZ, Mu DL, et al. Intraoperative hypotension is associated with shortened overall survival after lung cancer surgery. BMC Anesthesiol. 2020;20(1):160. https://doi.org/10.1186/s12871-020-01062-2. Published 2020 Jun 29.
Kalezic N, Stojanovic M, Ladjevic N, et al. Risk factors for intraoperative hypotension during thyroid surgery. Med Sci Monit. 2013;19:236–41. https://doi.org/10.12659/MSM.883869. Published 2013 Apr 3.
Maheshwari K, Khanna S, Bajracharya GR, et al. A randomized trial of continuous noninvasive blood pressure monitoring during noncardiac surgery. Anesth Analg. 2018;127(2):424–31. https://doi.org/10.1213/ANE.0000000000003482.
Maheshwari K, Ahuja S, Khanna AK, et al. Association between perioperative hypotension and delirium in postoperative critically ill patients: a retrospective cohort analysis. Anesth Analg. 2020;130(3):636–43. https://doi.org/10.1213/ANE.0000000000004517.
Mascha EJ, Yang D, Weiss S, Sessler DI. Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology. 2015;123(1):79–91. https://doi.org/10.1097/ALN.0000000000000686.
Mathis MR, Naik BI, Freundlich RE, et al. Preoperative risk and the association between hypotension and postoperative acute kidney injury. [published correction appears in Anesthesiology. 2020 Jan 6]. Anesthesiology. 2020;132(3):461–75. https://doi.org/10.1097/ALN.0000000000003063.
Monk TG, Bronsert MR, Henderson WG, et al. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. [published correction appears in Anesthesiology. 2016 Mar;124(3):741–2]. Anesthesiology. 2015;123(2):307–19. https://doi.org/10.1097/ALN.0000000000000756.
Radinovic K, Markovic Denic L, Milan Z, Cirkovic A, Baralic M, Bumbasirevic V. Impact of intraoperative blood pressure, blood pressure fluctuation, and pulse pressure on postoperative delirium in elderly patients with hip fracture: a prospective cohort study. Injury. 2019;50(9):1558–64. https://doi.org/10.1016/j.injury.2019.06.026.
Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126(1):47–65. https://doi.org/10.1097/ALN.0000000000001432.
Sessler DI, Bloomstone JA, Aronson S, et al. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019;122(5):563–74. https://doi.org/10.1016/j.bja.2019.01.013.
Shah NJ, Mentz G, Kheterpal S. The incidence of intraoperative hypotension in moderate to high risk patients undergoing non-cardiac surgery: a retrospective multicenter observational analysis. J Clin Anesth. 2020;66:109961. https://doi.org/10.1016/j.jclinane.2020.109961
Südfeld S, Brechnitz S, Wagner JY, et al. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth. 2017;119(1):57–64. https://doi.org/10.1093/bja/aex127.
Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology. 2015;123(3):515–23. https://doi.org/10.1097/ALN.0000000000000765.
Warner MA, Monk TG. The impact of lack of standardized definitions on the specialty. Anesthesiology. 2007;107(2):198–9. https://doi.org/10.1097/01.anes.0000271863.20091.60.
Weinberg L, Li SY, Louis M, et al. Reported definitions of intraoperative hypotension in adults undergoing non-cardiac surgery under general anaesthesia: a review. BMC Anesthesiol. 2022;22(1):69. https://doi.org/10.1186/s12871-022-01605-9. Published 2022 Mar 11.
Wesselink EM, Kappen TH, Torn HM, Slooter AJC, van Klei WA. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121(4):706–21. https://doi.org/10.1016/j.bja.2018.04.036.
Wickham AJ, Highton DT, Clark S, et al. Treatment threshold for intra-operative hypotension in clinical practice-a prospective cohort study in older patients in the UK. Anaesthesia. 2022;77(2):153–63. https://doi.org/10.1111/anae.15535.
Wijnberge M, Schenk J, Bulle E, et al. Association of intraoperative hypotension with postoperative morbidity and mortality: systematic review and meta-analysis. BJS Open. 2021;5(1):zraa018. https://doi.org/10.1093/bjsopen/zraa018.
Acknowledgements
None.
Funding
Drs. Christensen and Xing were supported by a contract with Edwards Lifesciences.
Author information
Authors and Affiliations
Contributions
Saasouh, Christensen: These authors developed the objectives for the manuscript, interpreted results, drafted the manuscript, and reviewed/revised the manuscript. Chappell, Lumbley, Woods, Dutton: These authors developed the objectives for the manuscript, oversaw data collection/extraction, interpreted results, and reviewed/revised the manuscript. Xing: This author analyzed the data, interpreted results, and reviewed/revised the manuscript. Mythen: This author developed the objectives for the manuscript, interpreted results, and reviewed/revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Health Media Lab Institutional Review Board (IRB) reviewed this study and determined it met criteria for IRB exemption, in accordance with the US Code of Federal Regulations for the Protection of Human Subjects, 45 CFR 46.104. The requirement for written informed consent was waived by the IRB.
Consent for publication
Not applicable.
Competing interests
Ms. Chappell is on the speakers’ bureau for Edwards Lifesciences and on the advisory board for ProVation. Dr Mythen is a paid consultant for Edwards Lifesciences. Dr. Saasouh received a one-time compensation for an advisory board consultation to Edwards Lifesciences. This relationship ended in 2022. Drs. Christensen, Dutton, Lumbley, Woods, and Xing: declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Sample selection. Table S1. Patient age distributionby clinician score group. Table S2. Percent female by clinician score group. Table S3. Mean patient BMI by clinician score group. Table S4. Mean ASA physical status by clinician score group. Table S5. Surgery length distributionby clinician score group. Table S6. Facility type by clinician score group. Table S7. Surgery length distributionby facility type.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saasouh, W., Christensen, A.L., Xing, F. et al. Incidence of intraoperative hypotension during non-cardiac surgery in community anesthesia practice: a retrospective observational analysis. Perioper Med 12, 29 (2023). https://doi.org/10.1186/s13741-023-00318-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-023-00318-y