Abstract
Background
Residential treatment is a common approach for treating opioid use disorder (OUD), however, few studies have directly compared it to outpatient treatment. The objective of this study was to compare OUD outcomes among individuals receiving residential and outpatient treatment.
Methods
A retrospective cohort study used linked data from a state Medicaid program, vital statistics, and the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Episodes Dataset (TEDS) to compare OUD-related health outcomes among individuals treated in a residential or outpatient setting between 2014 and 2017. Multivariable Cox proportional hazards and logistic regression models examined the association between treatment setting and outcomes (i.e., opioid overdose, non-overdose opioid-related and all-cause emergency department (ED) visits, hospital admissions, and treatment retention) controlling for patient characteristics, co-morbidities, and use of medications for opioid use disorders (MOUD). Interaction models evaluated how MOUD use modified associations between treatment setting and outcomes.
Results
Of 3293 individuals treated for OUD, 957 (29%) received treatment in a residential facility. MOUD use was higher among those treated as an outpatient (43%) compared to residential (19%). The risk of opioid overdose (aHR 1.39; 95% CI 0.73–2.64) or an opioid-related emergency department encounter or admission (aHR 1.02; 95% CI 0.80–1.29) did not differ between treatment settings. Independent of setting, MOUD use was associated with a significant reduction in overdose risk (aHR 0.45; 95% CI 0.23–0.89). Residential care was associated with greater odds of retention at 6-months (aOR 1.71; 95% CI 1.32–2.21) but not 1-year. Residential treatment was only associated with improved retention for individuals not receiving MOUD (6-month aOR 2.05; 95% CI 1.56–2.71) with no benefit observed in those who received MOUD (aOR 0.75; 95% CI 0.46–1.29; interaction p = 0.001).
Conclusions
Relative to outpatient treatment, residential treatment was not associated with reductions in opioid overdose or opioid-related ED encounters/hospitalizations. Regardless of setting, MOUD use was associated with a significant reduction in opioid overdose risk.
Similar content being viewed by others
Background
Approximately 2.7 million Americans have an opioid use disorder (OUD), yet fewer than 20% report receiving treatment [1, 2]. Initial treatment setting for OUD varies, but may involve medically supervised withdrawal (i.e. detoxification) in an inpatient or residential facility; treatment may also be initiated as an outpatient. The American Society of Addiction Medicine (ASAM) Criteria are widely used guidelines for level of care placement for patients with substance use disorders [3]. Studies suggest that patients who receive an insufficient intensity of treatment have worse outcomes compared to those who are triaged appropriately [4, 5]. While it is firmly established that medications for opioid use disorder (MOUD) such as buprenorphine and methadone are very effective at reducing opioid-related harms (e.g. overdose, death, infectious disease) and improving other addiction outcomes [6, 7], the optimal setting in which to initiate treatment remains unclear [8, 9].
Historically, spending on residential care has been a major cost center for the treatment of substance use disorders, accounting for 26–37% of spending between 2006 and 2015 [10]. While the role of outpatient care has increased, one in four adults continue to receive addiction treatment in a residential treatment facility [11]. Although residential treatment may have some advantages over outpatient care for individuals with OUD such as providing structured environment free from substances and the provision of clinical services like withdrawal support, evidence that it improves outcomes is sparse [12, 13]. Most notably, individuals entering residential or inpatient treatment are less likely to be offered ongoing outpatient care, including MOUD, which is associated with reduced rates of return to use [14, 15]. Models of care that link inpatient or residential withdrawal management induction to outpatient treatment improve outcomes.[16, 17]. Yet, fewer than half of patients who receive medically supervised withdrawal are transitioned to outpatient MOUD treatment, leading to increased risk of overdose [18,19,20].
Three recent studies examined the comparative effectiveness of treatment setting on OUD-related outcomes [20,21,22]. In a cohort of more than 30,000 patients undergoing medically managed inpatient detoxification in Massachusetts, Walley et al. found that subsequent MOUD was associated with a large reduction in opioid-related mortality (adjusted hazard ratio = 0.31), especially when combined with continued use within a residential treatment setting (adjusted hazard ratio = 0.14) compared to no further treatment [20] Yet, studies suggest fewer than a third of residential treatment settings offer opioid agonist therapy (i.e., buprenorphine or methadone) [23, 24].
Growing evidence suggests that outpatient treatment, when coupled with MOUD, may be superior to other treatment settings. Studies among commercial or Medicare Advantage enrolled patients demonstrate that outpatient treatment involving MOUD is associated with fewer overdoses, readmissions, or subsequent inpatient detoxification stays compared to inpatient detoxification or residential treatment [21, 22]. However, these recent studies comparing treatment settings have not focused on individuals with Medicaid, which has a critical role in responding to our nation’s opioid crisis. Collectively, state Medicaid programs cover 38% of individuals with OUD and finance more than half of all treatment in the US [25]. Additionally, those enrolled in Medicaid also have a considerably higher risk of opioid overdose [26]. Using a dataset linking administrative Medicaid claims, Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Episodes Dataset (TEDS), and vital statistics data from the state of Oregon, this analysis compared clinical outcomes for Medicaid beneficiaries with OUD receiving residential or outpatient treatment.
Material and methods
Data sources and study sample
The National Drug Abuse Treatment Clinical Trials Network (UG1DA015815) In and Out study (CTN-0086) was a retrospective cohort study comparing outcomes among individuals with OUD treated in different settings based on a secondary analysis of linked Medicaid, TEDS, and vital statistics data from Oregon. TEDS and Medicaid records were linked on the recipients’ Medicaid ID. TEDS data are collected by states and maintained by SAMHSA to track admissions (TEDS-A) to publicly funded substance use treatment facilities. For each admission, TEDS includes individual-level information describing substances used, routes of administration, frequency of use, and age of first use as well as demographics, and treatment-related characteristics (e.g. level of care). Oregon’s Medicaid data were also linked to the state’s death certificate data to identify opioid-related overdose fatalities. This linked dataset has been described and used in other studies related to opioid overdose [27,28,29,30].
Cohort and independent variable definitions
Individuals were included if they had procedure codes indicating a residential treatment stay or an outpatient treatment encounter (Additional file 1: Table S1) and diagnosis of OUD (Additional file 1: Table S2) between July 2014 to June 2017 [31, 32]. For those with multiple episodes, we selected the first chronologically and designated that as their index treatment encounter. We excluded individuals with fewer than 180 days of Medicaid enrollment prior to their treatment episode to ensure a sufficient period to capture baseline clinical characteristics. We used the 180-days preceding their index admission to assess baseline clinical characteristics using diagnoses described in the Elixhauser comorbidity index [33,34,35]. The Elixhauser comorbidity index contains a standardized set of thirty categories of behavioral (e.g. depression, ‘drug abuse,’ psychoses) and physical health (e.g. congestive heart failure, diabetes, liver disease) conditions based on International Classification of Disease (ICD) diagnosis codes and has been shown to predict in-hospital mortality and readmissions (Additional file 1: Table S3) [36].
We used linked TEDS data to ascertain additional details about their OUD such as opioid type (e.g. heroin, prescription opioids), other substances used (e.g. stimulants, alcohol), and other features of their OUD such as years of misuse, opioid injection, and frequency (e.g. daily, 3–6 times/week, 1–2 times/week, 1–3 times/month, no use in past month), whether they injected opioids, and frequency of use. We included patients if they had a TEDS admission record at any point during the baseline period and up to 7 days following their Medicaid index date. TEDS admission and Medicaid treatment episode index dates were identical for 60% episodes (72% of outpatient episodes and 42% of residential episodes). For individuals with multiple TEDS admissions, we used all admissions to quantify addiction characteristics with respect to substances used, frequency, and route. We excluded individuals whose TEDS admission record did not indicate opioid (heroin, prescription opioid, non-prescription methadone) as a problem substance (5.4% of individuals with linked TEDS data and an outpatient or residential episode).
We defined treatment-related (i.e. baseline) use of MOUD with Medicaid claims occurring during and up to 30 days after their residential index episode. Because an index outpatient treatment episode could persist for a longer period of time, we defined treatment-related MOUD for only those episodes where MOUD was present within the first 30 days of their index outpatient treatment date. MOUD included methadone dispensed through an opioid treatment program, office-based buprenorphine, and extended-release injectable naltrexone (XR-NTX). Buprenorphine was identified using National Drug Codes in outpatient pharmacy prescription claims (Additional file 1: Table S4). MOUD treatment with methadone or XR-NTX was identified using CPT codes in medical claims data (Additional file 1: Table S4).
Outcome definitions
The primary outcome was fatal or non-fatal opioid overdose. Fatal opioid overdoses were identified using Oregon’s vital statistics death data using ICD-10 codes (Additional file 1: Table S5). Potential non-fatal opioid overdoses were identified using Medicaid claims as an emergency department encounter or hospitalization (ED/hospitalization) with ICD diagnostic codes for an opioid poisoning (Additional file 1: Table S5). These codes have been validated in other Medicaid datasets and endorsed by the Centers for Disease Control and Prevention [37, 38].
We also examined three other secondary outcomes: non-overdose opioid-related ED/hospitalizations (e.g. opioid dependence; Additional file 1: Table S5), all cause ED/hospitalizations, and overall treatment retention. We defined retention as number of days from index episode until the day when all treatment across any treatment setting was discontinued. We defined discontinuation as having a 60-day gap without any claims for substance use disorder treatment services including provision of MOUD [32, 39].
Statistical analysis
We used multivariate Cox proportional hazards regression models to estimate the associations between treatment setting and overdose and ED/hospitalization outcomes. Following their index treatment episode, individuals were followed until they were censored by loss of Medicaid enrollment (one-month gap in enrollment) or the end of the study (December 2017). We included all baseline covariates for statistical adjustment. We chose the Elixhauser comorbidity composite score over the individual condition variables to increase the events-per-variable ratio and stabilize model estimates. Included covariates were: all baseline demographics (age, race, sex), Elixhauser comorbidity score, TEDS OUD characteristics (substances used, injection drug use, frequency of use), MOUD use, and medically managed withdrawal immediately preceding their treatment episode (Additional file 1: Table S1). We also adjusted for all-cause and opioid-related ED/hospitalizations occurring in the 180 prior to their index treatment episode.
The follow-up period was from index treatment episode date until an event occurred or the individual was censored by loss of Medicaid enrollment or the end of the study period. The variance inflation factor assessed multicollinearity. Cox proportional hazard models met all necessary assumption except all cause ED/hospitalization model which violated the proportional hazards assumption. To resolve this, we split this analysis into two separate follow-up periods (time 0 to day 13, day 14 until end of study).
For the analysis of treatment retention, we used a subset of individuals with at least one year of Medicaid enrollment after their index treatment date to evaluate the association between treatment setting and retention. Using the same adjustment variables included in the Cox proportional hazard models, we used multivariable logistic regression to evaluate the association between treatment setting and retention at six and twelve months.
Our main hypothesis concerned identifying clinical benefits of residential over outpatient treatment, independent of potential unbalanced confounders (e.g. MOUD use). However, because MOUD is a vital component of OUD treatment, we also examined how its use modified potential associations between treatment setting and all opioid-related outcomes. To do this, we included the interaction between MOUD and treatment setting in our models and report treatment setting associations stratified by MOUD. All analyses used SAS (version 9.4) and considered two-sided p-values < 0.05 to be statistically significant. This study was deemed non-human subjects research by the Oregon Health & Science University Institutional Review Board.
Results
Study sample characteristics
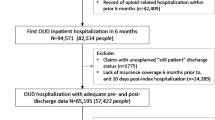
We identified 3293 individuals receiving treatment for OUD that met inclusion criteria (Fig. 1). Table 1 summarizes demographic, co-morbidities, treatment, and addiction-related characteristics. There were 957 individuals with an index episode in a residential facility, and 2336 treated as outpatients. Most individuals were White (74%), male (54%), and between the ages of 18 and 39 (78%). Aside from drug misuse, which was present in all patients, the most common Elixhauser conditions were alcohol misuse (20%), depression (17%), and psychoses (10%). In general, individuals treated in a residential facility had higher rates of comorbidity. Heroin was the most commonly used opioid (71%). About 39% of individuals reported a problem with prescription opioids, 39% with stimulants, and 20% with alcohol. Nearly half of individuals reported injection drug use and 57% reported daily opioid use.
Overall, 17% of patients had inpatient medically managed withdrawal immediately preceding their treatment episode, however this was more than sixfold more likely in those receiving residential treatment (44% vs 7%). About one-third (36%) of individuals received MOUD treatment during their index treatment episode. Receipt of MOUD was higher among those treated as outpatients (43% vs. 19%). The most prevalent type of MOUD was buprenorphine (25%).
Opioid-related and healthcare utilization outcomes
Table 2 summarizes Cox proportional hazard models comparing outcomes across treatment settings. Of the 56 individuals experiencing an opioid overdose, 24 (2.5%) were among those receiving residential treatment and 32 (1.4%) received outpatient treatment; 25 of these events were fatal. The risk of opioid overdose did not differ significantly between individuals who were treated in a residential setting (adjusted hazard ratio [aHR] 1.39; 95% confident interval [CI] 0.73 to 2.64) compared to those treated as outpatients. Receipt of MOUD was associated with a reduction in opioid overdose (aHR 0.45; 95% CI 0.23 to 0.89). Table 3 summarizes the interaction models and adjusted ORs stratified by MOUD use. The interaction between MOUD and setting did not meet the threshold for statistical significance.
There was no association between index treatment setting and opioid-related ED/hospitalization (aHR 1.02; 95% CI 0.08–1.29) overall. However, the interaction with MOUD was significant (p = 0.005) suggesting that among individuals receiving MOUD, patients receiving residential care had a higher risk (aHR 1.59; 95% CI 1.09–2.32) of an opioid-related ED/hospitalization relative to outpatient care.
In both follow-up intervals, the risk for an all-cause ED/hospital admission was elevated for those receiving residential treatment [< 14 days: aHR 2.48 (95% CI 1.98–3.11); 14 + days: aHR 1.25 [95% CI 1.12–1.41)].
Treatment retention
There were 1913 individuals (58% of original sample) with at least one year of Medicaid enrollment. Demographic variables and comorbidities were similar to the overall sample (Additional file 1: Table S6). Retention outcomes for these individuals are summarized in Table 4. Compared to those receiving outpatient treatment, individuals receiving residential treatment were more likely to be retained at 6-months (adjusted odds ratio [aOR] 1.71; 95% CI 1.32–2.21) with no difference at 12-months (aOR 1.12; 95% CI 0.83–1.52). For both retention outcomes, the MOUD interactions were significant, suggesting residential treatment was favored over outpatient treatment only for those without MOUD use.
Discussion
Residential treatment is often considered the highest intensity of treatment for individuals with OUD [40], and may by particularly important for those with unstable housing, co-morbid mental health conditions, or high medical need [41]. However, evidence supporting this assumption is mixed and has primarily focused on treatment completion, retention, and abstinence outcomes [9, 13]. Few studies have directly compared residential treatment with outpatient treatment for clinical outcomes such as overdose [20,21,22]. In this analysis, we used a linked Medicaid dataset to compare outcomes for individuals with OUD who received residential or outpatient treatment. After adjustment for a variety of physical, mental, and addiction-related comorbidities, we found that rates of overdose, opioid-related, and all-cause ED or hospitalizations were not reduced for individuals receiving residential treatment compared to those treated as an outpatient. While residential treatment was associated with higher retention at 6-months, this difference was not significant at 12-months. In stratified analyses, the benefits of residential treatment on retention appeared to be confined to those not receiving MOUD.
Historically, public perception has assumed residential treatment to be the gold standard, a view often endorsed by the addiction treatment community despite its greater cost and limited evidence [8, 13]. Efforts to further refine selection of patients most likely to benefit from residential treatment are likely to be eclipsed by increasing the use of MOUD in, and following, residential treatment. Opioid agonist treatment for OUD improves a variety of addiction-related outcomes and markedly reduces the risk of overdose and all-cause mortality [7, 42]. In our study, MOUD was associated with a 55% reduction in the risk of opioid overdose independent of treatment setting. About one-third of individuals receiving treatment were prescribed MOUD which is comparable to other reports and suggests missed opportunities for improving OUD treatment outcomes [1, 24].
This study adds to a mixed literature demonstrating the potential benefits of residential treatment for individuals with OUD with respect to treatment retention [13, 21, 22, 43]. Studies using SAMHSA TEDS data exclusively have generally shown that individuals entering residential facilities have higher treatment completion rates [43, 44]. Consistent with this literature, we found that residential treatment was associated with enhanced retention. While treatment completion is associated with improved some clinical and social outcomes, it is a surrogate indicator of improved addiction-related health outcomes. Moreover, OUD is now universally recognized as a chronic condition requiring long-term outpatient management. Although residential care was associated with improved retention in our study, it was not associated with improvements in overdose or other opioid-related outcomes. This largely comports with recent claims-based analyses that suggest outpatient treatment may be clinically superior to inpatient or residential treatment, especially when coupled with MOUD [21, 22].
Our subgroup analyses found that among individuals receiving MOUD, outpatient treatment was associated with improved opioid-related ED or hospitalizations compared to residential treatment. Using a similar retrospective cohort design, Morgan et al. found outpatient-based MOUD to be associated with improved rates of opioid overdose and all-cause admissions compared to inpatient treatment initiation [21]. Additional research is required to identify whether other subgroups of patients might benefit from residential treatment in the fentanyl era, such as those with a history of previous unsuccessful attempts at outpatient treatment, housing instability, and adolescents.
This study has several limitations. This was an observational study design, and findings are potentially affected by selection bias and confounding. Although we statistically adjusted for a wide variety of demographic, medical, and addiction-related covariates, our findings may be affected by residual confounding from unmeasured clinical and addiction-related characteristics. Further, the source data for this study was Medicaid administrative claims data, TEDS, and vital statistics data and missing data could affect our findings in uncertain ways. Because most outcomes were constructed using Medicaid data, gaps in Medicaid enrollment may also have introduced biases in how outcomes were measured. Although we measured opioid-related outcomes using ED and hospitalization administrative claims, non-fatal overdoses not treated in these settings could be missed. We were unable to link every treatment episode identified in the Medicaid dataset with a corresponding TEDS admission. This is likely due to under or inconsistent data submission by treatment providers and may further limit external validity [45]. Finally, study data was from one state Medicaid program and may not reflect treatment experiences or outcomes from other states or payers, such as those with commercial insurance. Despite this limitation, our findings are insightful because Oregon has among the highest burden of substance use in the nation, yet ranks last in treatment access [46].
Conclusions
The findings of this study suggest residential treatment was not associated with improved outcomes relative to outpatient treatment. Although overall retention was enhanced for residential treatment in the short-term, this benefit was short-lived and limited to individuals not receiving MOUD. Importantly, MOUD use, independent of setting, was associated with a significant reduction in the risk for opioid overdose, underscoring the importance of MOUD across all treatment settings. In the absence of compelling evidence of benefit associated with residential treatment, expansion of treatment access should focus on broadening outpatient MOUD treatment capacity.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available because of terms of data use agreements.
Abbreviations
- aHR:
-
Adjusted hazard ratios
- ASAM:
-
American Society of Addiction Medicine
- CPT:
-
Current procedural terminology
- ED:
-
Emergency department
- ICD:
-
International Classification of Disease
- MOUD:
-
Medications for opioid use disorder
- OUD:
-
Opioid use disorder
- SAMHSA:
-
Substance Abuse and Mental Health Services Administration
- TEDS:
-
Treatment Episodes Dataset
- XR-NTX:
-
Extended-release naltrexone
References
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. 2017. https://www.samhsa.gov/data/.
Wu L-T, Zhu H, Swartz MS. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016;169:117–27.
Baker SL, Gastfriend DR. Reliability of multidimensional substance abuse treatment matching: implementing the ASAM Patient Placement Criteria. J Addict Dis. 2003;22(Suppl 1):45–60.
Sharon E, Krebs C, Turner W, Desai N, Binus G, Penk W, et al. Predictive validity of the ASAM patient placement criteria for hospital utilization. J Addict Dis. 2004;22(sup1):79–93.
Magura S, Staines G, Kosanke N, Rosenblum A, Foote J, DeLuca A, et al. Predictive validity of the ASAM patient placement criteria for naturalistically matched vs mismatched alcoholism patients. Am J Addict. 2003;12(5):386–97.
Larochelle MR, Stopka TJ, Xuan Z, Liebschutz JM, Walley AY. Medication for opioid use disorder after nonfatal opioid overdose and mortality. Ann Intern Med. 2019;170(6):430–1.
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357: j1550.
McCarty D, Priest KC, Korthuis PT. Treatment and prevention of opioid use disorder: challenges and opportunities. Annu Rev Public Health. 2018;39:525–41.
Blanco C, Volkow ND. Management of opioid use disorder in the USA: present status and future directions. Lancet. 2019;393(10182):1760–72.
Substance Abuse and Mental Health Services Administration. Behavioral Health spending & use accounts 2006–2015. HHS Pub. No. (SMA) 19–5095. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2019.
Substance Abuse and Mental Health Services Administration. Results from the 2020 national survey on drug use and health: detailed tables, sections 5; [Internet]. Rockville (MD): SAMHSA; 2021.
Stewart M, O'Brien P, Shields M, Ma M, Mulvaney D. State residential treatment for behavioral health conditions: regulation and policy environmental scan 2019.
Reif S, George P, Braude L, Dougherty RH, Daniels AS, Ghose SS, et al. Residential treatment for individuals with substance use disorders: assessing the evidence. Psychiatr Serv (Washington, DC). 2014;65(3):301–12.
Ling W, Amass L, Shoptaw S, Annon JJ, Hillhouse M, Babcock D, et al. A multi-center randomized trial of buprenorphine-naloxone versus clonidine for opioid detoxification: findings from the National Institute on Drug Abuse Clinical Trials Network. Addiction (Abingdon, England). 2005;100(8):1090–100.
Amato L, Minozzi S, Davoli M, Vecchi S. Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification. Cochrane Database Syst Rev. 2011;9:Cd005031.
Mark TL, Vandivort-Warren R, Montejano LB. Factors affecting detoxification readmission: analysis of public sector data from three states. J Subst Abuse Treat. 2006;31(4):439–45.
Spear SE. Reducing readmissions to detoxification: an interorganizational network perspective. Drug Alcohol Depend. 2014;137:76–82.
Mojtabai R, Mauro C, Wall MM, Barry CL, Olfson M. Medication treatment for opioid use disorders in substance use treatment facilities. Health Aff. 2019;38(1):14–23.
Stein M, Herman D, Conti M, Anderson B, Bailey G. Initiating buprenorphine treatment for opioid use disorder during short-term in-patient ‘detoxification’: a randomized clinical trial. Addiction (Abingdon, England). 2020;115(1):82–94.
Walley AY, Lodi S, Li Y, Bernson D, Babakhanlou-Chase H, Land T, et al. Association between mortality rates and medication and residential treatment after in-patient medically managed opioid withdrawal: a cohort analysis. Addiction (Abingdon, England). 2020;115(8):1496–508.
Morgan JR, Barocas JA, Murphy SM, Epstein RL, Stein MD, Schackman BR, et al. Comparison of rates of overdose and hospitalization after initiation of medication for opioid use disorder in the inpatient vs outpatient setting. JAMA Netw Open. 2020;3(12): e2029676.
Wakeman SE, Larochelle MR, Ameli O, Chaisson CE, McPheeters JT, Crown WH, et al. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020;3(2): e1920622.
Beetham T, Saloner B, Gaye M, Wakeman SE, Frank RG, Barnett ML. Therapies offered at residential addiction treatment programs in the United States. JAMA. 2020;324(8):804–6.
Huhn AS, Hobelmann JG, Strickland JC, Oyler GA, Bergeria CL, Umbricht A, et al. Differences in availability and use of medications for opioid use disorder in residential treatment settings in the United States. JAMA Netw Open. 2020;3(2):e1920843-e.
Henry J Kaiser Family Foundation. The opioid epidemic and Medicaid’s role in facilitating access to treatment. www.kff.org/medicaid/issue-brief/the-opioid-epidemic-and-medicaids-role-in-facilitating-access-to-treatment. Accessed 4 Feb 2021.
Sharp MJ, Melnik TA. Poisoning deaths involving opioid analgesics—New York State, 2003–2012. MMWR Morb Mortal Wkly Rep. 2015;64(14):377–80.
Hallvik SE, El Ibrahimi S, Johnston K, Geddes J, Leichtling G, Korthuis PT, et al. Patient outcomes after opioid dose reduction among patients with chronic opioid therapy. Pain. 2022;163(1):83–90.
El Ibrahimi S, Hallvik S, Johnston K, Leichtling G, Korthuis PT, Chan B, et al. Characteristics and health care events of patients admitted to treatment for both heroin and methamphetamine compared to patients admitted for heroin only. J Subst Abuse Treat. 2022;132: 108615.
Hartung DM, Geddes J, Johnston KA, Leichtling G, Hallvik S, Hildebran C, et al. Patterns of prescription opioid use prior to self-reported heroin initiation. J Addict Med. 2021;15(2):130–3.
Hartung DM, Johnston KA, Hallvik S, Leichtling G, Geddes J, Hildebran C, et al. Prescription opioid dispensing patterns prior to heroin overdose in a state medicaid program: a case-control study. J Gen Intern Med. 2020;35(11):3188–96.
Harris AHS, Ellerbe L, Phelps TE, Finney JW, Bowe T, Gupta S, et al. Examining the specification validity of the HEDIS quality measures for substance use disorders. J Subst Abuse Treat. 2015;53:16–21.
Hadland SE, Bagley SM, Rodean J, et al. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr. 2018;172(11):1029.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55(7):698–705.
Kalra V, Gulati S, Pandey RM, Menon S. West syndrome and other infantile epileptic encephalopathies–Indian hospital experience. Brain Develop. 2002;24(2):130–9.
Green CA, Perrin NA, Hazlehurst B, Janoff SL, DeVeaugh-Geiss A, Carrell DS, et al. Identifying and classifying opioid-related overdoses: a validation study. Pharmacoepidemiol Drug Saf. 2019;28(8):1127–37.
Clark RE, Baxter JD, Aweh G, O’Connell E, Fisher WH, Barton BA. Risk Factors for relapse and higher costs among medicaid members with opioid dependence or abuse: opioid agonists, comorbidities, and treatment history. J Subst Abuse Treat. 2015;57:75–80.
Mee-Lee D, Shulman H, Fishman MJ, Gastfriend DR. The ASAM criteria: treatment criteria for addictive, substance-related, and co-occurring conditions, 3rd edn. Carson City, NV: The Change Companies; 2013. Copyright 2013 by the American Society of Addiction Medicine.; 2013.
Wenzel SL, Audrey Burnam M, Koegel P, Morton SC, Miu A, Jinnett KJ, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158–69.
Santo T Jr, Clark B, Hickman M, Grebely J, Campbell G, Sordo L, et al. Association of opioid agonist treatment with all-cause mortality and specific causes of death among people with opioid dependence: a systematic review and meta-analysis. JAMA Psychiat. 2021;78(9):979–93.
Stahler GJ, Mennis J, DuCette JP. Residential and outpatient treatment completion for substance use disorders in the U.S.: moderation analysis by demographics and drug of choice. Addict Behav. 2016;58:129–35.
Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Treatment episode data set (TEDS): 2019. admissions to and discharges from publicly funded substance use treatment. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2021.
Analysis of Oregon’s publicly funded substance abuse treatment system: report and findings for senate bill 1041. Oregon Criminal Justice Commission. 2019.
2019-2020 NSDUH State Estimates Of Substance Use And Mental Disorders. December 29, 2021. https://www.samhsa.gov/data/report/2019-2020-nsduh-state-prevalence-estimates.
Acknowledgements
The opinions expressed in this manuscript are solely those of the authors and do not represent the official views of the National Institutes of Health. Udi Ghitza’s role in this study was as NIDA Project Scientist (Scientific Officer), and Dr. Ghitza has not had and will not have any programmatic involvement with non-cooperative agreement grants cited.
Funding
This project was supported through grants from the National Institutes of Health National Institute on Drug Abuse (UG1DA015815, UH3DA044831) and Centers for Disease Control (U01 CE00278).
Author information
Authors and Affiliations
Contributions
DH, TK conceptualized study, oversaw acquisition of data, interpreted results, drafted and provided critical revisions to manuscript. KJ, JG, SM assisted with data acquisition and analysis and provided critical revisions to manuscript. JG, KJ, RB, SM, GL, CH, BC, RRC, DM, UG: interpreted results, drafted and provided critical revisions to manuscript. All authors have approved submitted version of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed by the OHSU IRB and is considered non-human subjects research.
Consent for publication
NA
Competing interests
Authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
. CPT/HCPCS codes used to define initial treatment type. Table S2. Opioid use disorder diagnosis codes. Table S3. Elixhauser Comorbidity Conditions. Table S4. Medication for opioid use disorder codes. Table S5. Opioid-related ICD codes. Table S6. Patient and treatment characteristics of patients with one year of continuous Medicaid enrollment (n=1,913).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hartung, D.M., Markwardt, S., Johnston, K. et al. Association between treatment setting and outcomes among oregon medicaid patients with opioid use disorder: a retrospective cohort study. Addict Sci Clin Pract 17, 45 (2022). https://doi.org/10.1186/s13722-022-00318-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13722-022-00318-1