Abstract
Background
Patients with opioid use disorder (OUD) display an interindividual variability in their response to medications for opioid use disorder (MOUD). A genetic basis may explain the variability in this response. However, no consensus has been reached regarding which genetic variants significantly contribute to MOUD outcomes.
Objectives
This systematic review aims to summarize genome-wide significant findings on MOUD outcomes and critically appraise the quality of the studies involved.
Methods
Databases searched from inception until August 21st, 2020 include: MEDLINE, Web of Science, EMBASE, CINAHL and Pre-CINAHL, GWAS Catalog and GWAS Central. The included studies had to be GWASs that assessed MOUD in an OUD population. All studies were screened in duplicate. The quality of the included studies was scored and assessed using the Q-Genie tool. Quantitative analysis, as planned in the protocol, was not feasible, so the studies were analyzed qualitatively.
Results
Our search identified 7292 studies. Five studies meeting the eligibility criteria were included. However, only three studies reported results that met our significance threshold of p ≤ 1.0 × 10–7. In total, 43 genetic variants were identified. Variants corresponding to CNIH3 were reported to be associated with daily heroin injection in Europeans, OPRM1, TRIB2, and ZNF146 with methadone dose in African Americans, EYS with methadone dose in Europeans, and SPON1 and intergenic regions in chromosomes 9 and 3 with plasma concentrations of S-methadone, R-methadone, and R-EDDP, respectively, in Han Chinese.
Limitations
The limitations of this study include not being able to synthesize the data in a quantitative way and a conservative eligibility and data collection model.
Conclusion
The results from this systematic review will aid in highlighting significant genetic variants that can be replicated in future OUD pharmacogenetics research to ascertain their role in patient-specific MOUD outcomes.
Systematic review registration number CRD42020169121.
Similar content being viewed by others
Background
Rationale
Opioid use has been on the rise over the past decade, causing the United States and Canada, amongst other countries, to declare an opioid crisis and epidemic [1, 2]. In a 2019 report, the United Nations estimated about 53 million past-year users of opioids for 2017 worldwide [3]. That same year, 110,000 deaths were attributed to opioid use [3].
Treatments for opioid use disorder (OUD) have become more available and accessible under the term medication-assisted treatments or medications for opioid use disorder (MOUD). MOUD include the controlled administration of an opioid agonist or antagonist along with behavioural therapy or counselling with the objective of full recovery from opioid use [4]. Pharmacological agents of MOUD include the commonly used methadone, buprenorphine, buprenorphine/naloxone combination, naltrexone, heroin-assisted treatment, and sustained release morphine.
MOUD decreases the risk of overdose and mortality in individuals with OUD [5, 6]. A recent systematic review has reported the pooled overdose crude mortality rates for individuals being treated with MOUD compared to after the cessation of MOUD and during untreated periods being 0.24, 0.68, and 2.43, respectively [5]. Another review summarizing MOUD effectiveness in randomized controlled trials reported that the administration of MOUD at least doubles the rates of opioid abstinence when compared to placebo medications or no medications [6].
MOUD initiation and termination are important stages in determining patient health outcomes. As mentioned earlier, mortality risks tend to spike shortly after MOUD cessation [5]. Additionally, induction of methadone has shown an increased risk of overdose in multiple studies [7, 8]. Methadone dosing can affect electrocardiographic QTc interval prolongation, inducing respiratory depression amongst patients and increasing the risk for overdose mortality [9]. This is indicative that perhaps dosing of MOUD and its metabolism in patients are important factors in determining patient outcomes.
Given the individual basis of the treatment administration, a genetic predisposition to MOUD responses may be involved. OUD is a complex polygenic disorder with not one genetic variant attributing to a large risk or effect. Genetic association studies researching genetic variants or single-nucleotide polymorphisms (SNPs) associated with OUD or its treatment outcomes require large sample sizes to generate enough power to identify such variants [10].
Currently, the most common SNPs associated with MOUD outcomes correspond to OPRM1, OPRD1, ABCB1, and CYP2B6 genes [11, 12]. OPRM1, ABCB1, and CYP2B6 variants have been associated with altered methadone doses [12]. ABCB1 along with CYP2B6 variants have also been linked to variable methadone plasma concentrations. Other studies showed variants in OPRD1 to be associated with opioid-positive urine screens and therapeutic responses in patients administered methadone versus buprenorphine [11, 12].
Though there seem to be numerous studies assessing the pharmacogenetics of MOUD, many of which are candidate gene studies with small samples sizes. To produce replicable results and discover new significantly associated SNPs, robust genome-wide association studies (GWASs) need to be performed and assessed. This systematic review is the first to summarize the current literature, assess the quality of the findings, and report on the areas that need to be addressed within this field.
Objectives
The aims of this systematic review are to highlight any significant GWAS genetic variants that are associated with MOUD outcomes in patients, including illicit opioid use as well as secondary outcomes such as MOUD plasma concentrations and doses [13].
The specific objectives are:
-
1.
Summarize the genome-wide significant SNP outcome associations reported in the literature and highlight novel ones.
-
2.
Critically examine and assess the quality of the findings extracted within the relevant studies using the Q-Genie tool.
-
3.
Identify gaps within the literature that need to be addressed with respect to pharmacogenetic research of MOUD outcomes.
Methods
This systematic review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. A supplementary PRISMA checklist is in Additional File 1. Since the focus of this review is on GWASs, it does not conform with the Human Genome Epidemiology Network (HuGENet) guideline expectations of reporting on candidate gene study findings [15]. However, the HuGENet guideline is used to supplement the PRISMA guidelines, to provide a more informed review, upholding a standard of reporting specific to genetic association studies.
Protocol and registration
This systematic review has been registered with the International Prospective Register of Systematic Reviews (PROSPERO) [16]; registration ID CRD42020169121. A systematic review protocol has been published in Systematic Reviews [13]. The detailed methods of this systematic review are specified and documented in the registration and protocol.
Eligibility criteria and search strategy
The eligibility for inclusion in this systematic review is three-fold. The study design of included studies is limited to GWASs specific to genetic variants of interest reported as SNPs. The included studies have to look at an OUD population. Lastly, included studies have to investigate a MOUD, such as methadone, buprenorphine/naloxone, buprenorphine, naltrexone, or heroin-assisted treatment. Studies are not restricted by language, patient demographics, or MOUD administration setting.
A search strategy was developed with help from a Health Sciences Librarian (SS). Table 1 outlines the databases searched and the search terms used. All databases were searched from inception to August 21st, 2020. Handsearching was used to identify relevant studies that were not detected by the search strategy, such as those assessing sustained-release morphine as a treatment.
Data collection and outcomes
Title and abstract screening, full-text screening, and data extraction of studies were all completed in duplicate via Covidence [17]. The voting of reviewers remained blinded and conflict resolution for the screening stages was performed by a senior reviewer (AH or CC), keeping the process unbiased. Authors of full text articles that were not found or unavailable were contacted regarding the provision of the full text so the study can better assess them for inclusion in this systematic review. The data extraction form was pilot tested in duplicate prior to proceeding with data collection.
Data extracted include study information, baseline participant characteristics, relevant and significant measured outcomes, statistical measures, and reported study limitations and conflicts. For the purposes of this review, the significance threshold of SNP outcome associations extracted is p ≤ 1 × 10–7, as some GWAS results with this significance level have been shown to be replicable within the literature [18].
The outcomes of interest in this review pertain to genetic variants significantly associated with MOUD outcomes observed in OUD patients. The primary MOUD outcome considered is illicit opioid use or abstinence during or following MOUD. The secondary MOUD outcomes include time to relapse, treatment retention, opioid overdose, non-opioid substance use, comorbid psychiatric disorders, drug-related risk-taking behaviours, MOUD and metabolite plasma concentration, MOUD dose, and mortality.
Quality assessment and data analysis
Quality assessment of each included study is done using the Quality of Genetic Association Studies (Q-Genie) tool [Version 1.1], assessing the study validity, reliability, and risk of bias [19]. Quality assessments are completed in duplicate, and conflicts regarding the scoring are resolved by the reviewers.
A heterogeneity test and random effects meta-analysis through pooled odds ratios or calculated mean differences, respective of the measure of association, were planned to quantitatively assess the data, as outlined in the protocol. However, these measures were not appropriate as data extracted from each study was unique and could not be synthesized.
For the aforementioned reasons, subgroup meta-analyses and risk of bias assessments across studies also could not be completed.
Results
Study selection
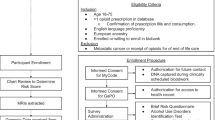
A total of 5 studies were eligible for inclusion in this systematic review [20,21,22,23,24]. The search strategy along with handsearching techniques identified 7292 studies, with 5809 advancing to the title and abstract screening after the removal of duplicates by both the Zotero reference manager and Covidence [17, 25]. Following title and abstract screening, 38 studies were deemed relevant for full-text screening, and 5771 studies were excluded due to not being GWASs, not assessing an OUD population, and/or not assessing a MOUD. Of the 38 full-text studies assessed for eligibility, 5 GWASs (3 prospective, 1 cross-sectional, and 1 case–control) underwent data extraction and qualitative assessment. See flow diagram in Fig. 1.
Study characteristics
Table 2 provides a summary of the included study characteristics. All five studies were published in English. Three were prospective studies, one case–control, and one cross-sectional. The sample size studied varied from a few hundred to thousands of participants, the smallest being 344 and largest 4049. All studies had a majority male study population, varying from 59.72% to 81.6% males. The mean age per studied population varied from 33.03 (5.45) to 45.6 (8.4). Ancestries of the participants included in these GWASs were European, African American, and/or Han Chinese, with Europeans constituting the largest sample. Two of the studies identified used the same sample population of Han Chinese individuals for their analyses, though performed different statistical measures [23, 24]. Three of the studies reported that participants were administered methadone as their MOUD [22,23,24], and two did not specify [20, 21]. The outcomes of interest that were associated with genetic variants were opioid cessation, daily heroin injection while on MOUD, methadone dose, and plasma concentrations of methadone and its metabolite EDDP. No study assessed relapse, treatment retention, opioid overdose, non-opioid substance use, psychiatric disorders, risk-taking behaviours, or mortality as outcomes associated with genetic variation.
Risk of bias within studies
The quality and validity of each study was assessed using the Q-Genie tool on a scale of 1 to 7 [19]. Studies with a control group and with overall scores of greater than or equal to 45, as well as studies with no control group with overall scores of greater than 40 were considered of good quality, per the tool classification guidelines. All but one study were assessed to be of good quality, while Nelson et al. was deemed to be of moderate quality [21]. It should be noted that the primary objectives of Nelson et al.’s study might not have been to assess an MOUD outcome per se, but rather opioid dependence end points amongst opioid-dependent daily injectors (cases) versus nondaily injecting opioid misusers (controls). However, due to satisfying the eligibility criteria and analyzing an outcome of interest to us in only the cases, this study was included. Three of the included studies report insufficient sample sizes that might result in not detecting genome-wide significant SNPs [22,23,24]. The three studies also disclose conflicts of interest that are reported to not be interferent with the research conducted [20,21,22]. See Table 3 for a summary of the reported limitations and conflicts of interest, as well as the quality assessments.
Results of individual studies
Of the five studies included, only three reported outcomes that reached the threshold of significance set for this systematic review (Table 4) [21, 22, 24].
Nelson et al. identified three SNPs associated with opioid dependence end point in the gene CNIH3 (chromosome 1). The participants were daily heroin-injecting patients on methadone or buprenorphine of European ethnicity. The three SNPs reported are in moderate to high linkage disequilibrium, with the odds of the risk alleles being found in the daily heroin injecting group approximately 50% lower than in the control group [21].
Smith et al. identified thirty-seven SNPs associated with methadone dose in varying genes across methadone-treated African American and European American populations. Amongst participants of African American ethnicity, the SNPs correlated to the following genes: OPRM1 (chromosome 6), TRIB2 (chromosome 2), and ZNF146 (chromosome 19). On the other hand, the SNPs identified in European Americans correlated to only one gene, EYS (chromosome 6). The leading SNP nearest to the OPRM1 gene (rs73568641) was reported to be in mid to high linkage disequilibrium with neighbouring SNPs identified. Linkage disequilibrium amongst SNPs of other genes was not reported as they were not genome-wide significant. The presence of the risk alleles in the OPRM1, TRIB2, and ZNF146 genes is observed to be associated with an increase in the usual daily methadone dose in African American patients. In contrast, the presence of the risk alleles in the EYS gene is observed to be associated with a decrease in the usual daily methadone dose in European Americans [22].
Lastly, Yang et al. identified three SNPs associated with methadone and EDDP plasma concentrations. The participants were methadone-administered patients in Taiwan of Han Chinese ancestry. One SNP was associated with plasma concentration of R-methadone, corresponding to an intergenic region (chromosome 9), one with plasma concentration of S-methadone, corresponding to the SPON1 gene (chromosome 11), and the last one associated with plasma concentration of R-EDDP, corresponding to another intergenic region (chromosome 3). The measure and magnitude of association for these SNPs were not reported [24].
Discussion
Summary of evidence
Advances in pharmacogenetic research within OUD populations have been on the rise. Yet, no attempt has been made in quantitatively and qualitatively analyzing the literature and critiquing the quality of evidence reported by GWASs. This systematic review was able to summarize findings from GWASs with borderline genome-wide significance and the potential of being replicable in future studies. We have identified five studies that match our inclusion criteria, with three studies reporting significant results. SNPs associated with outcomes of daily heroin injection, methadone dose, and methadone and EDDP plasma concentration were found to be significant. SNPs corresponding to genetic regions of CNIH3 were reported to be more prevalent in daily heroin injecting patients. SNPs corresponding to or near OPRM1, TRIB2, ZNF146, and EYS were associated with methadone dose levels, depending on ethnicity. SNPs in an intergenic region on chromosome 9, SPON1, and an intergenic region on chromosome 3 were associated with differing plasma concentration of R-methadone, S-methadone, and R-EDDP, respectively. The quality of research and reporting of each study was assessed with the Q-Genie tool and no study was deemed to be of poor quality. Varying sample sizes were however observed, with some being too small for what is considered acceptable for GWAS analysis. With sample sizes of thousands required to produce adequately powered results in GWASs [26], sample sizes from Yang et al. (n = 344) and the African American population of Smith et al. (n = 383) fell short.
One gene related to the SNPs identified has been reported previously within candidate gene studies and has an established biological relevance within the genetics and pharmacogenetics of OUD research. The OPRM1 gene encodes the mu-opioid receptor, which binds endogenous and exogenous opioids [27]. Genetic variability in OPRM1 has been reported to have biological effects on the mu-opioid receptor function contributing to complex disorders. An in-vitro study showed that the OPRM1-G118 variant reduces OPRM1 mRNA and protein levels [28]. When studied in mice models, the equivalent point mutation OPRM1-G112 also resulted in decreased mu-opioid receptor mRNA and protein expression [29]. Findings showed that mice with the G112 allele had reduced morphine-induced antinociceptive responses [29]. Consistently, OPRM1 has been reported to be highly influential in opioid dependency, and, by some findings, OUD treatment outcomes, such as methadone dose and plasma concentrations, in European patients [30]. Therefore, it is not a surprise for SNPs in this gene to be associated with methadone dose at a GWAS significance level. Though, Smith et al.’s results are interesting because they found an OPRM1 association in patients of African American ethnicity but not of European ethnicity, as was expected. This incongruity calls for additional powered research in both ethnic populations to be conducted for a consensus.
Another gene identified has not been previously associated with OUD or MOUD outcomes in the literature but could be involved in biological pathways relevant to opioid use. The CNIH3 gene encodes the protein cornichon homolog 3, which regulates AMPA receptor trafficking [27]. This gene has been identified in schizophrenia studies by NCBI’s Gene database [31]. Therefore, it is possible that CNIH3 could be associated with the regulation of opioid use.
Most of the genes involving an identified SNP summarized in this systematic review do not seem to have been relevant to OUD or MOUD outcomes, nor could a biological relevance be identified for them. These genes include TRIB2, ZNF146, EYS, SPON1, as well as the intergenic regions for the SNPs located on chromosomes 3 and 9. The TRIB2 gene encodes the tribbles homolog 2 protein that regulates MAP kinase proteins’ activation [27]. This gene is evident in many tissues, most prominently in the ovaries, spleen, and nymph node tissues [31]. It has also been reported in the NCBI Gene Database to be identified in studies researching schizophrenia, neuropsychiatric disorders, autism, and aging [31]. ZNF146 encodes the zinc finger protein OZF, the primary function of which is to regulate DNA binding and transcription [27]. As such, it is present in a lot of tissues, including the brain, but is more prominent in the endometrium and thyroid [31]. In humans, EYS encodes the protein eyes shut homolog, which as deduced from the name, is involved in vision, more specifically, in maintaining the morphological integrity of photoreceptor cells through the possible involvement in channel regulations [27]. EYS is most prevalently expressed in fat and testis tissue [31], which shows no direct relation to methadone dose or metabolism as identified in Smith et al. Lastly, SPON1 encodes spondin-1, which is a cell adhesion protein within the nervous system [27]. SPON1 is mostly expressed in the gall bladder tissue [31], which does not provide a clear biological link to its function nor the outcome of methadone plasma concentration reported by Yang et al. [31]. Further research is required to make any conclusive statements concerning the biological relevance of SNPs in these genes to the observed MOUD outcomes.
In general, the results of this systematic review are able to inform future candidate gene studies and GWASs of key SNPs that require further research in larger cohorts as well as replications to solidify their associations to MOUD outcomes in indicated patients. The findings from such studies are able to inform the clinical and pharmacological response to patient doses and drug outcomes for administered MOUD.
Limitations
Though rigorous, this systematic review has some limitations associated with the strict eligibility criteria predetermined in the protocol. It is important to note that in the process of including studies that were primary GWASs, GWAS meta-analyses were excluded. This could have affected the number, quality, and significance of the findings. An example is the exclusion of the GWAS meta-analysis findings from Nelson et al. that replicated original findings in a larger meta-analyzed sample, highlighting new SNPs that achieved significance (rs10799590, rs12130499, and rs298733) and SNPs that fell below our significance threshold in the process (rs1436175) [21]. However, since most GWAS meta-analyses reported associations using the same study populations and sample data, their inclusion would have made any reported findings redundant. Another limitation could be the exclusion of studies that reported genetic variance in the form of haplotypes. Though their inclusion might have made a meta-analysis possible, they did not satisfy the eligibility criteria of a SNP identified by a GWAS and would, therefore, not be very informative within the scope of our systematic review.
As stated previously, a meta-analysis was not feasible with the heterogeneity of the reported findings. This makes consensus more difficult to reach and the findings less generalizable, especially when considering differing ethnicities.
In addition, this systematic review was only able to highlight published GWAS associations. As a result, any findings that were not published due to inability to meet statistical thresholds might not have been included. Though efforts were made to include near genome-wide significant findings, the possible presence of publication bias should still be acknowledged.
Conclusions
Through this systematic review, we were able to summarize GWAS significant findings in the field of OUD pharmacogenetics. We were able to inform the availability of data by highlighting what has been done within this research field, and what gap exists and needs to be addressed. Recommendations of further powered research are made, with close attention to the ethnicities of participating cohorts to test whether SNP outcome associations within one ethnicity hold competing levels of validity in another.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- OUD:
-
Opioid use disorder
- MOUD:
-
Medications for opioid use disorder
- SNP:
-
Single nucleotide polymorphism
- GWAS:
-
Genome-wide association study
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- HuGENet:
-
Human Genome Epidemiology Network
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- Q-Genie:
-
Quality of Genetic Association Studies
References
Government of Canada. Federal action on opioids—Canada.ca. 2020. https://www.canada.ca/en/health-canada/services/substance-use/problematic-prescription-drug-use/opioids/federal-actions.html. Accessed 6 Feb 2020.
HHS. HHS Acting Secretary Declares Public Health Emergency to Address National Opioid Crisis | HHS.gov. 2017. https://www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html. Accessed 6 Feb 2020.
United Nations Office on Drug and Crimes. World drug report 2019. 2019.
SAMHSA. Medication and counseling treatment. https://www.samhsa.gov/. Accessed 2 Jun 2020.
Ma J, Bao Y-P, Wang R-J, Su M-F, Liu M-X, Li J-Q, et al. Effects of medication-assisted treatment on mortality among opioids users: a systematic review and meta-analysis. Mol Psychiatry. 2019;24(12):1868–83.
Connery HS. Medication-assisted treatment of opioid use disorder: review of the evidence and future directions. Harv Rev Psychiatry. 2015;23(2):63–75.
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017. p. 357. http://www.bmj.com/content/357/bmj.j1550. Accessed 2 Jun 2020.
Buster MCA, van Brussel GHA, van den Brink W. An increase in overdose mortality during the first 2 weeks after entering or re-entering methadone treatment in Amsterdam. Addiction. 2020. https://doi.org/10.1046/j.1360-0443.2002.00179.x.
Chou R, Cruciani RA, Fiellin DA, Compton P, Farrar JT, Haigney MC, et al. Methadone safety: a clinical practice guideline from the American pain society and college on problems of drug dependence, in collaboration with the heart rhythm society. J Pain. 2014;15(4):321–37.
Hong EP, Park JW. Sample size and statistical power calculation in genetic association studies. Genomics Inform. 2012;10(2):117–22.
Berrettini W. A brief review of the genetics and pharmacogenetics of opioid use disorders. Dialogues Clin Neurosci. 2017;19(3):229–36.
Fonseca F, Torrens M. Pharmacogenetics of methadone response. Mol Diagn Ther. 2018;22(1):57–78.
Chawar C, Hillmer A, Sanger S, D’Elia A, Panesar B, Guan L, et al. GWAS-identified genetic variants associated with medication-assisted treatment outcomes in patients with opioid use disorder: a systematic review and meta-analysis protocol. Syst Rev. 2020;9(1):200.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Little J, Higgins J (eds). The HuGENetTM HuGE Review Handbook, version 1.0. Atlanta, GA; Centers for Disease Control and Prevention; 2006.
PROSPERO: International prospective register of systematic reviews. CRD42020169121; 2020. https://www.crd.york.ac.uk/PROSPERO/. Accessed 2 June 2020.
Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia. www.covidence.org. Accessed 1 Oct 2020.
Panagiotou OA, Ioannidis JPA. What should the genome-wide significance threshold be? Empirical replication of borderline genetic associations. Int J Epidemiol. 2012;41(1):273–86.
Sohani ZN, Meyre D, de Souza RJ, Joseph PG, Gandhi M, Dennis BB, et al. Assessing the quality of published genetic association studies in meta-analyses: the quality of genetic studies (Q-Genie) tool. BMC Genet. 2015. https://doi.org/10.1186/s12863-015-0211-2.
Cox JW, Sherva RM, Lunetta KL, Johnson EC, Martin NG, Degenhardt L, et al. Genome-wide association study of opioid cessation. J Clin Med. 2020;9(1):180.
Nelson EC, Agrawal A, Heath AC, Bogdan R, Sherva R, Zhang B, et al. Evidence of CNIH3 involvement in opioid dependence. Mol Psychiatry. 2016;21(5):608–14.
Smith AH, Jensen KP, Li J, Nunez Y, Farrer LA, Hakonarson H, et al. Genome-wide association study of therapeutic opioid dosing identifies a novel locus upstream of OPRM1. Mol Psychiatry. 2017;22(3):346–52.
Wang S-C, Chung R-H, Kuo H-W, Liu T-H, Fang C-P, Liu SC, et al. GRK5 is associated with the regulation of methadone dosage in heroin dependence. Int J Neuropsychopharmacol. 2018;21(10):910–7.
Yang H-C, Chu S-K, Huang C-L, Kuo H-W, Wang S-C, Liu S-W, et al. Genome-wide pharmacogenomic study on methadone maintenance treatment identifies SNP rs17180299 and multiple haplotypes on CYP2B6, SPON1, and GSG1L associated with plasma concentrations of methadone R- and S-enantiomers in heroin-dependent patients. PLOS Genet. 2016;12(3):e1005910.
Center for History New Media, George Mason University. Zotero: The Next-Generation Research; 2009. http://www.zotero.org/. Accessed 20 Nov 2021.
Ziyatdinov A, Kim J, Prokopenko D, Privé F, Laporte F, Loh P-R, et al. Estimating the effective sample size in association studies of quantitative traits. bioRxiv. 2019.12.15.877217.
UniProt Consortium. UniProt: a worldwide hub of protein knowledge. Nucleic Acids Res. 2019;47(D1):D506-15.
Zhang Y, Wang D, Johnson AD, Papp AC, Sadée W. Allelic expression imbalance of human mu opioid receptor (OPRM1) caused by variant A118G*. J Biol Chem. 2005;280(38):32618–24.
Mague SD, Blendy JA. OPRM1 SNP (A118G): Involvement in disease development, treatment response, and animal models. Drug Alcohol Depend. 2010;108(3):172–82.
Crist RC, Clarke T-K, Berrettini WH. Pharmacogenetics of opioid use disorder treatment. CNS Drugs. 2018;32(4):305–20.
National Library of Medicine (US), National Center for Biotechnology Information. Gene - NCBI. https://www-ncbi-nlm-nih-gov.libaccess.lib.mcmaster.ca/gene/. Accessed 5 Jun 2020.
Acknowledgements
Not applicable.
Funding
This systematic review was partially funded by CIHR (grant number PJT-156306). The funding agency had no role in the study design, interpretation of data, or dissemination of results.
Author information
Authors and Affiliations
Contributions
ZS is the guarantor. CC and ZS conceptualized the systematic review. CC implemented the design of the review and search strategy with the aid of AH and SS. CC, AH, AD, BP, LG, DX, NB, and AA screened studies, extracted data, and assessed the quality of the studies. CC prepared the first draft. AH, SS, AD, BP, LG, DX, NB, AA, FK, GP, LT, and ZS reviewed and revised the protocol draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
PRISMA 2009 Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chawar, C., Hillmer, A., Sanger, S. et al. A systematic review of GWAS identified SNPs associated with outcomes of medications for opioid use disorder. Addict Sci Clin Pract 16, 70 (2021). https://doi.org/10.1186/s13722-021-00278-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13722-021-00278-y