Abstract
Background
Self-rated physical health (SRPH) is known as an important predictor of mortality. Previous studies mostly used baseline values of self-rated health to predict long-term mortality. The effect of change in self-rated physical health on mortality during the course of aging has rarely been researched. The present study aimed to determine SRPH over time in women and men of an aging population, assess whether and how change in SRPH affects mortality while adjusting for known determinants of mortality, and test effect modification by sex on the relation between course of SRPH and mortality.
Methods
Data of N = 12,423 respondents of the 5-year follow-up of the Gutenberg Health Study (GHS) with participation at the baseline assessment were analysed. All-cause mortality from 5-year follow-up onwards was defined as the primary outcome. SRPH was assessed by a single item. Cox proportional hazards models with adjustment for age, sex, socio-economic status and physical diseases were fitted to assess the predictive power of baseline score and course of SRPH. Additionally, effect modification by sex was assessed.
Results
During a median follow-up period of 7.3 years (quartiles 6.0-8.5 years), 618 (5%) participants died. Overall, 70.9% of the participants indicated good or very good SRPH at baseline (T1) and follow-up (T2), 6.9% rated their SRPH as not so good at T1 and T2, and 0.6% reported bad SRPH at T1 and T2. An improvement of SRPH was indicated by 9.6% and 12.0% indicated deterioration of their SRPH. Change in SRPH added substantial predictive information to the Cox proportional hazards models, when adjusting for relevant covariates. In men, deterioration and constantly bad SRPH were associated with the strongest increase in risk of mortality by 87%, resp. 228%. While improvements increased mortality risk in men (67%), women with an improved SRPH had a lower risk (57%).
Conclusion
A sizeable subgroup of aging participants reported deterioration of SRPH over five years. The association between change of SRPH and mortality is modified by sex. Deterioration of SRPH predicts mortality over baseline-assessment even when adjusted for relevant covariates. SRPH should be assessed regularly as part of an older individual’s health evaluation. Deterioration, constantly bad and improved SRPH should be taken seriously as unfavorable prognostic indicators, the latter only in men.
Similar content being viewed by others
Taxt box 1. Contributions to the literature |
|---|
- There is limited evidence on the association of change in self-rated physical health and mortality risk, especially in Germany. Furthermore, the role of sex on the association has been neglected. |
- Change in self-rated physical health is associated with increased mortality in the long run among German adults. |
- In men, an improvement of self-rated physical health should be taken seriously as unfavourable prognostic indicator. |
- Self-rated physical health is an important additional health indicator beyond clinical assessment and should be checked in medical consultations routinely. |
Introduction
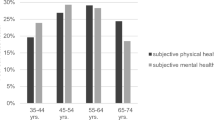
To date, self-rated health has been recognized as an important predictor of quality of life, adverse health outcomes (e.g. diabetes, cardiovascular diseases, functional decline, depression) and mortality in adulthood [1,2,3,4,5,6,7,8,9]. Hence, within in an aging population, self-rated health has become a commonly used indicator of successful aging [10, 11]. It describes individuals’ subjective assessment of their health including physical, mental, cultural and social aspects of health [12,13,14,15]. Self-rated health is mostly assessed by single item questions, e.g. “In general, how would you rate your health today?” with response options such as very good or good, moderate, poor or very poor [16]. Its validity has been proven extensively [17] and shown to be stable among different age-groups and sex [18, 19]. A multitude of socio-economic and individual factors influence self-rated health. Poor self-rated health was more often reported by older adults and women compared to younger age groups and men [15, 20, 21]. Further, low education and income [22], unemployment [23], multimorbidity [24], health behavior [25], as well as mental health burdens were associated with poor self-rated health [20, 26]. However, the influence of these factors on self-rated health varies among individuals of different age cohorts in Europe. While age showed the strongest effect within adults born before 1945, education and employment were found to be strongest determinants in the age cohort of 1945 to 1964 and smoking was negatively associated among the younger generations born after 1965 [25].
Poor self-rated health has been consistently linked to higher all-cause mortality [27,28,29] and cardiovascular as well as cancer mortality [27, 30]. Compared to excellent self-rated health, poor self-ratings of health were associated with a two-fold higher mortality risk [31]. When relevant clinical correlates of mortality (e.g., co-morbidity, depression, subclinical illness or functional status) were taken into account, the association of self-rated health and mortality remained, even though its predictivity decreased [1, 32]. Analyzing cross-classification between self-rated health and objective health status for potential risk stratification, Mutz and Lewis [2] showed that, individuals with excellent self-rated health and favourable health status had lower mortality risk compared to individuals with poor self-rated health and unfavourable health status. The relation between self-rated health and mortality varied among individuals of different populations. For instance, poor self-rated health is more predictive of mortality in men than in women [12, 33, 34]. Further, authors of a French cohort study comparing the predictive value of self-rated health for mortality between different socio-economic groups over a mean period of 17.2 years, found weaker predictive ability within higher occupation, income and education groups [35].
Self-rated health may capture health aspects relevant to mortality which are not covered by clinical assessment [15]. However, most studies have not distinguished between the dimensions of self-rated physical and mental health when predicting mortality. Hence, using data of the Gutenberg Health Study (GHS), a large, prospective community cohort study in mid-Germany, we have already analysed the predictive value of the two self-rated health dimensions separately and showed that only self-rated physical, but not mental health is predictive of mortality, after controlling for relevant covariates [34]. Also, results of the Rotterdam Study suggested, that self-rated mental health is not predictive of mortality when sociodemographic, major chronic physical diseases, functional status, and mental health indicators were taken into account [36].
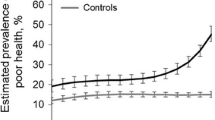
Research mainly used baseline measures of self-rated health to predict long-term mortality and treated self-rated health as a time constant variable, even when multiple assessments were available [12, 37]. However, self-rated health can be expected to change over the course of aging. Using data from the European Social Survey, Bauknecht and Merkel [38] examined the development of self-rated health of older persons in 17 countries between 2002 and 2018. Overall, an improvement of self-rated health was found in older subjects from different cohorts. Furthermore, in a recent Swedish study, which investigated change in self-rated health among older adults over a 20-year study period, 42.6% reported stable self-rated health, 40.6% deterioration, and 16.8% indicated an improvement [39]. Sperlich and Tetzlaff [40] analyzed age- and sex-specific longitudinal changes in self-rated health in Germany over 20 years based on 29,251 women and 26,967 men in the German Socio-Economic Panel. The authors found increasing self-rated health over time among women aged 41–50 to 71–80 years, while men reported improvements at the ages 61–70 and 71–80 years. No improvements were shown in the youngest (31–40 years) and oldest age group (81–90 years) in both sexes. To date, a multitude of studies tried to explain these changes by taking further socio-economic characteristics into account. For instance, a cohort study from the US determined changes in self-rated health in a sample of older adults (50–84 years) between 1972 and 2018 and showed that self-rated health has steadily improved over the 46-year study period, especially among participants with 13 years of education or more [41]. Also, Lamidi [42] highlighted the role of marital status and education in changes in self-rated health. While a recent systematic review concluded that the predictive impact of self-rated health on mortality is persistent in the medium and long-term perspective [43], other studies noted that the long-term predictive value of self-rated health on mortality was poorer than the short-term prediction [29, 37, 44]. Thus, independent effects of change in self-rated health on the association of self-rated health and mortality risk might have been disregarded.
To date, only a few studies analysed the association of change in self-rated health and mortality risk. For instance, Vogelsang [45] analysed the relationship between self-rated health change and mortality in a nationally representative sample of U.S. oldest-old adults and found that, adults indicating a decline in self-rated health had the greatest mortality risk. Interestingly, adults reporting an improvement in their self-rated health died more often than those who indicated no change. The author suspected that improvements may have been associated with surviving and recovering from a major health event (e.g. diagnoses of cancer, stroke, lung disease) or with normalizing pre-existing conditions [46, 47]. Thus, it can be assumed that sources of change may have independent associations with mortality [48]. Further, these initially slightly confusing findings underscore the fact that self-rated health improvements imply worse prior health ratings [49], that may still increase the risk of mortality compared to an unchanged or good health status. Additionally, Vogelsang [45] found no statistically significant differences between participants with an improved and participants with an unchanged self-rated health in respect to number of chronic physical health conditions, limited mobility or activities of daily living suggesting that improvements are more influenced by other factors. Especially with increasing age, individuals tend to change their subjective health norms and evaluation standards [50]. Thus, an improvement may be rather driven by a cut-point shift or psychological adaptation [51] reflecting the multitude of aspects that influence one’s subjective evaluation of their health. Han and Phillips [52] compared the predictive value of change in self-rated health with assessments of baseline self-rated health and ratings of self-rated health prior to death in community-dwelling disabled women aged 65 or older. A decline in self-rated health was significantly associated with increased mortality, while baseline self-rated health and self-rated health prior to death were not related controlling for relevant covariates. Also, in a cohort of Danes, a decline in self-rated health was associated with an increased mortality risk compared to unchanged good self-rated health. Notably, unchanged poor and improved self-rated health were also related to an increase mortality risk. The authors noted that poor self-rated health at any one measurement point was associated with an increased risk [49]. Change in self-rated health, specifically deterioration, were mainly predicted by low socio-economic status, poor quality of life, low trust in people and behavioural factors (e.g., moderate level of physical activity) or polypharmacy [53, 54].
However, to the best of our knowledge, the few prior studies analysing the association of change in self-rated health and mortality risk have not used data from Germany. Accordingly, there is a need for further research into the association between change in self-rated health and mortality risk among German older adults. The role of sex as a potential effect modifier of the relation of self-rated health and mortality has been neglected (e.g., 46). For instance, in our previous analysis we found that men rate their physical health better than women; the association of poor self-rated physical health to mortality was also stronger in men compared to women [34].
Thus, we aimed to extend prior findings by analysing levels of and change in self-rated health and their association with mortality over time in a German cohort and to determine the role of sex. Since previous research has shown, that self-rated physical health was most strongly associated with mortality [34, 36], we focused on self-rated physical health (SRPH).
Specifically, we:
-
(1)
Determined levels and change of SRPH in women and men of a large, aging community cohort.
-
(2)
Assessed whether and how change in SRPH affect mortality over baseline assessment while adjusting for major correlates of mortality (age, sex, socio-economic status, chronic physical diseases).
-
(3)
Test effect modification by sex on the relation between course of SRPH and mortality.
Materials and methods
Study design and participants
The present study used data of the Gutenberg Health Study (GHS), an ongoing population-based, prospective, observational single-center cohort study in the Rhine-Main region located in western Mid-Germany [55]. Primary endpoints are myocardial infarction and cardiovascular death. Overall mortality and diseases of the eye, the immune system, cancer, and mental health were defined as additional endpoints. The ethics committee of the Medical Chamber of Rhineland-Palatinate and the local and federal data safety commissioners approved the study protocol. The sample of the GHS was drawn randomly from the local registries of the city of Mainz and the district of Mainz-Bingen and stratified 1:1 for sex and residence and in equal strata across age decades. Further inclusion criteria were age 35 to 74, sufficient knowledge of the German language, and physical or mental ability to visit the study center for study investigations. Before inclusion in the study, written informed consent was obtained from each participant, according to the tenets of the Declaration of Helsinki. Inclusion criterion for the current investigation was participation at follow-up including filling out SRPH at baseline (T1, 2007–2012) and at 5-years follow-up (T2, 2012–2017) leading to a final analysis sample of N = 12,423 participants.
Measures
To be able to analyze the effect of change in SRPH between T1 and T2 on mortality, all-cause mortality from T2 assessment onwards was defined as primary outcome. Updates of vital status were performed by quarterly queries to the registry offices and the mortality registry Rhineland-Palatinate. Reviews and death certificates with the exact date of death were acquired. For this analysis, mortality follow-up was complete as of December, 13, 2021, which results in a complete mortality follow-up for at least 5 five years in participants of T2 assessment with a median follow-up of 7.3 years due to administrative censoring only.
Self-rated physical was measured with the single-item “How would you rate your current physical health?” Response options ranged from very good to bad (1 = very good and 2 = good, 3 = not so good and 4 = bad). In line with widely used and valid single item questions assessing self-rated health [16, 17], the present single-item was previously formulated for the use in the GHS. Its validity has been demonstrated by relations to sociodemographic factors, chronic physical diseases and mortality in a current study. For instance, better SRPH was found among men and married participants. Moreover, while a positive association with SES was observed, negative associations with depression and anxiety symptoms as well as number of chronic physical diseases were determined [34]. We classified change of SRPH combining baseline and follow-up as one category by five classes: unchanged good/ very good, improved, unchanged not so good, deteriorated, and unchanged bad.
Chronic physical diseases were assessed in a computer-assisted personal interview at baseline and 5-year follow-up, cancer also after 7,5 years. Participants were asked whether they had ever (T1) received a definite diagnosis or whether they had received a definite diagnosis within the last five years (T2) of myocardial infarction, coronary artery disease, stroke, peripheral artery disease, atrial fibrillation, heart failure, cancer or chronic obstructive pulmonary disease by a physician. For the present analyses, numbers of chronic physical diseases reported at baseline and at follow-up were summarized to a sum score. Thirty participants were excluded from analysis due to incomplete SRPH. Disease information was incomplete in one item in 460 cases and on more than one item in 40 cases. For statistical analysis, the respective number of reported diseases we used as explanatory variable, irrespective of whether single items were incomplete. As the level of incompleteness was low, we did not apply more advanced imputation methods.
Sociodemographic characteristics were assessed as self-report and included age in years, sex as male and female, married [no/yes]. Combining data of education, profession and income, we defined socio-economic status (SES) according to Lampert, Kroll [56] ranging from 3 (lowest) to 21 (highest) SES.
Statistical analysis
Descriptive characteristics were reported as absolute numbers and percentages for categorical variables and as means with standard deviations for continuous variables. Mortality was reported as proportions of deaths from T2 onwards. We fitted Cox proportional hazards models for assessing the predictive power of course of SRPH while adjusting for age, sex, SES and number of chronic physical diseases at T1 and T2. We further tested the interaction between sex and SRPH (ref. men with unchanged very good/good SRPH). The adequacy of entering age, SES and number of diseases as linear terms was checked by the method of fractional polynomials.
P-values were assumed to be significant with p < 001. Confidence intervals are reported at confidence level 95% without any adjustment for simultaneous error control. Statistical analyses were performed using SAS (2013) Statistical Analysis Software. Users’ Guide Statistics Version 9.4.
Results
Participants
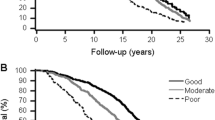
A total of 12,423 participants filled out self-rated physical health at baseline and at follow-up. Their mean age was 54.5 years, and 49.8% were female. At T2, a total of 79.4% rated their physical health as very good/ good, while 2.5% reported bad SRPH. In women 76.8% indicated very good/good and 2.8% bad SRPH. 81.9% of men showed very good/good and 2.3% bad SRPH. During a median follow-up period of 7.3 (quartiles 6.0-8.5) years, 618 (5%) participants died.
Detailed information about participants’ sociodemographic and health characteristics, stratified according to mortality and sex, are shown in Table 1.
Change in SRPH
Overall, 70.9% of the participants indicated very good/good SRPH at T1 and T2, 6.9% reported not so good SRPH at T1 and T2, and 0.6% rated their SRPH as bad at both measurement points. 9.6% reported improvement and 12.0% deterioration of their SRPH. Among women, 67.7% reported unchanged very good/good SRPH, 10.5% indicated unchanged not so good SRPH, and 0.8 rated their SRPH as unchanged bad. An improvement of SRPH was reported by 13.1% of women, while 8.0% indicated a deterioration of their SRPH. 74.1% of men reported unchanged very good/good SRPH, 8.8% rated their SRPH at both measurements as not so good, and 0.4% indicated unchanged bad SRPH. An improvement of SRPH was found in 10.9% of men and deteriorated SRPH in 5.9%.
Change in SRPH and mortality
In the total sample, among participants, who died, 55.1% had indicated an unchanged very good/ good SRPH, 10.0% reported not so good SRPH at both measurement points, and 1.7% indicated no change in their bad SRPH. While 10.0% of the participants reported an improvement of their SRPH, 23.2% of the participants, who died, indicated a deteriorated SRPH. In women, of those who died, 57.3% reported an unchanged very good/good SRPH, 6.0% indicated an unchanged not so good SRPH and in 2.7% was an unchanged bad SRPH found. While 21.6% the women, who died showed an improvement in their SRPH, 12.4% indicated a deterioration in SRPH. Among men, who died, 54.2% rated their SRPH at T1 and T2 as very good/good, 11.7% showed an unchanged not so good SRPH, and 1.4% reported bad SRPH at both measurements. While an improvement of SRPH was observed in 23.8% of men, who died, deteriorated SRPH was found in 8.9%.
Results of Cox proportional hazards models, showed that the course of SRPH was predictive for mortality risk after adjusting for age, sex, SES, and known physical diseases (Table 2). SRPH at T1 showed predictive only without including SRPH at T2 (p = 0.006). As judged by likelihood ratio testing, adding baseline SRPH did not improve model fit when added to the SRPH at T2 (p = .029). There was a significant interaction between sex and SRPH (Likelihood ratio chi square p = 0.022 comparing the model with vs. without interaction). Overall, hazard ratios of men were mostly in the same direction but higher compared to women. The highest hazard ratio for mortality were found for unchanged bad (men: HR: 2.28; 95% CI: 1.00 to 5.19%; women: HR: 2.01; 95% CI: 0.82–4.95); deterioration (men: HR: 1.87; 95% CI: 1.47 to 2.38; women: HR: 1.37; 95% CI: 0.95 to 1.98), followed by unchanged not so good (men: HR: 1.47; 95% CI: 1.04 to 2.08; women: HR:1.33; 95% CI: 0.84 to 2.09). For improvement we found divergent effects: in men, improvements were associated with a 1.67-fold increase in mortality (HR: 1.67; 95% CI: 1.22 to 2.27), while women, who reported an improved SRPH, had a lower mortality risk (HR: 0.57%; 95% CI: 0.31 to 1.06) compared to unchanged very good/good SRPH in men and women, respectively. For detailed information see Table 2. Note, that further differentiating between very good and good SRPH did not improve model fit as judged by likelihood ratio test.
Discussion
Since the 1950s, self-rated health has been recognized as an important global health indicator in predicting future health-related events and use of medical care, especially the dimension of self-rated physical health [15, 34, 36]. However, most findings relied on baseline measures of self-rated health. The role of sex in this association has hardly been explored. Thus, the mid- and long-term predictive power of self-rated health and its change over time is still unclear. The present work aimed to assess the course of SRPH in an aging population over time and associate it with mortality in men and in women. While the number of chronic physical diseases increases when getting older, we found a remarkable average stability of very good/good self-rated physical health over five years in the great majority of 70.9% of participants. Nevertheless, 0.6% reported bad SRPH at both measurement points and a sizeable subgroup of 12.0% indicated a deteriorated SRPH. Sex-stratified analyses mirrored similar patterns: Most women and men rated their SRPH at both measurements as very good/good (67.7%; 74.0%). While 0.8% of women and 0.4% of men reported unchanged bad SRPH, deterioration was showed by 8.0% of women and 5.9% of men. Notably, in the total sample, participants with an unchanged bad SRPH or a deterioration of SRPH were at highest risk of mortality compared to participants indicating very good/good SRPH at both measurement points, even after taking relevant confounders into account. Moreover, additional analyses demonstrated, that SRPH at T1 was predictive only without including SRPH at T2. Further, adding SRPH at T1 to SRPH at T2. Similar patterns were found in the sex-stratified analyses. As in a previous, cross-sectional paper, associations were stronger for men than for women. However, specifying previous findings on the effect modification by sex [45, 49], results of interactions in a Cox proportional hazards models showed that, an improvement in SRPH increased the risk compared to an unchanged very good/ good SRPH, but only in men. In women we found the reverse association, declined mortality in the case of improved SRPH. These findings indicate that men and women may rate their health differently. As we had previously shown [34], men rated their physical health better, but suffered from a higher mortality than women. Possibly, unlike women, they also may overrate their physical health after having endured and mastered a significant health crisis [46]. Further, findings may also reflect a stronger response shift in males [50]. Higher age, male sex, lower socio-economic status and chronic physical disease at T2 were predictive of mortality. Overall, our findings are in line with previous findings showing that poor self-rated health ratings were associated with higher mortality compared to participants with good self-rated health, even when controlling for relevant confounders (e.g., 27, 28, 29, 34). Further, results of the present work supported the assumption of [15], that self-rated health capture health aspects relevant to mortality which are not covered by clinical assessment. Consistent with findings on change of self-rated health, we found an improved prediction of mortality when repeated assessments of SRPH were taken into account. Comparable to Beth et al. (2005), our findings suggested that, a decline in SRPH was significantly associated with increased mortality risk, even when controlling for relevant confounders.
Strength and limitations
Strengths of the present study referring to its longitudinal study design with repeated measurements from a large-scale cohort study. Further, the use of one specific component of self-rated health enabled us to analyse the specific predictive value of the physical aspect. Thus, findings may target preventive health policies as well as to clarify understanding of the overall construct of self-rated health. However, the findings must be interpreted considering the study’s limitations. About one third of the regional population were willing to participate which resulted in some selection toward higher social status, less migrant background and possibly with respect to health status at study entry. As in other large cohorts no selection with respect to outcomes was effective and a bias in exposure risk relations would be plausible only in presence of strong interaction effects. Neither sex nor SES showed such behaviour. As data of the present study were gathered within the German general population, the generalizability to other countries is still unclear. Results may also change when different operationalization were used to capture change in SRPH. For instance, instead of using computed change, change can also be operationalized as retrospectively reported change by asking participants if they feel that their health has improved, declined, or stayed constant between two measurement points [46]. We used all-cause mortality as outcome, therefore we were not able to assume prediction on cause-specific mortality. Further, our results suggested that even an improvement in SRPH increased the risk compared to an unchanged very good/ good SRPH. However, we have to concede that we did not take differences of distinct courses of improvement into account. For instance, an improvement from bad to not so good may had different effects on mortality compared to an improvement from not so good to very good/good. To aim at a better understanding of underlying mechanisms, future research should integrate cause-specific mortality data into the analysis and differentiate courses of improvements. Nevertheless, improvements should be interpreted critically taking further evaluating aspects into account. It should be kept in mind, that mortality risk is higher even if precious health conditions may normalize. Further, we concede that older adults who lived in, or moved to nursing homes, respectively, and those who were house-bound were presumably underrepresented as study participation required on-site visits. Also, our set of correlates may not be sufficient. For instance, some researchers pointed to a difference of self-rated health among rural and urban residents [57, 58]. The present study did not take this into account. Our study was based on a proposal that contained a statistical analysis plan, including a limited list of covariables to be considered. Physical disease, sex and SES were considered the most relevant variables. We had learned from similar investigations on the health status and SRPH at baseline, that the number of serious chronic conditions as documented in the GHS captures essential prognostic information. Thus, we performed a number of sensitivity analyses to make sure that no variation of disease variable coding provided more information. We did so by comparing refined models with a basic model via likelihood ratio testing. Further, the interplay between physical and mental health with anxiety and depression could be considered in future studies.
Conclusion
Finding of the present work pointed to potential adjustment to chronic physical diseases. Indeed, maintaining self-rated physical health in the face of diseases may indicate healthy ageing. However, a sizeable subgroup reported deterioration of SRPH. Data of the present work extend previous findings showing that low levels of SRPH, especially a deterioration, is associated with increased mortality in the long run. Thus, it can be assumed, that previous well-established associations between SRPH and mortality might have been underestimated mortality risk for individuals with recent change in SRPH. They endorse the view that SRPH is an important additional health indicator beyond clinical assessment which should be checked in medical consultations, particularly in elderly patients routinely. It can be included as a simple question in doctor visits or surveys. Further, change in SRPH can be easily created with longitudinal data.
Data availability
Written informed consent from GHS study participants does not allow publicaccess to the data. Access to the data in the local database is possible at anytime upon request according to the ethics vote. This concept was developed withthe local data protection officer and the ethics committee (local ethicscommittee of the Rhineland-Palatinate Medical Association, Germany).Interested scientists can make their requests to the Gutenberg Health StudySteering Committee (e-mail: info@ghs-mainz.de).
Abbreviations
- SRPH:
-
Self-rated physical health
- GHS:
-
Gutenberg Health Study
- SES:
-
Socio-economic status
References
Murata C, Kondo T, Tamakoshi K, Yatsuya H, Toyoshima H. Determinants of self-rated health: could health status explain the association between self-rated health and mortality? Arch Gerontol Geriatr. 2006;43(3):369–80.
Mutz J, Lewis CM. Cross-classification between self-rated health and health status: longitudinal analyses of all-cause mortality and leading causes of death in the UK. Sci Rep. 2022;12(1):459.
Puts M, Monette J, Girre V, Sourial N, Wolfson C, Monette M, et al. The relationship of self-rated health with functional status, toxicity and mortality: results of a prospective pilot study of older patients with newly-diagnosed cancer. J Geriatr Oncol. 2013;4(4):319–26.
Jones JW, Ledermann T, Fauth EB. Self-rated health and depressive symptoms in older adults: a growth mixture modeling approach. Arch Gerontol Geriatr. 2018;79:137–44.
de Oliveira LFS, Wanderley RL, de Medeiros MMD, de Figueredo OMC, Pinheiro MA, Garcia RCMR, et al. Health-related quality of life of institutionalized older adults: influence of physical, nutritional and self-perceived health status. Arch Gerontol Geriatr. 2021;92:104278.
Nylund O, Johansson L, Lind MM, Johansson M. The association between self-rated health, health-related quality of life, and risk of venous thromboembolism. Prev Med Rep. 2023;36:102434.
Noh JW, Chang Y, Park M, Kwon YD, Ryu S. Self-rated health and the risk of incident type 2 diabetes mellitus: a cohort study. Sci Rep. 2019;9(1):3697.
Fong JH, Kok ZC. Does subjective health matter? Predicting overall and specific ADL disability incidence. Arch Gerontol Geriatr. 2020;90:104169.
Whyne EZ, Woo J, Jeon-Slaughter H. The effects of subjective wellbeing and self-rated health on Lifetime Risk of Cardiovascular conditions in Women. Int J Environ Res Public Health. 2023;20(14):6380.
Whitley E, Popham F, Benzeval M. Comparison of the Rowe–Kahn model of successful aging with self-rated health and life satisfaction: the West of Scotland Twenty-07 prospective cohort study. Gerontologist. 2016;56(6):1082–92.
Lee WJ, Peng LN, Lin MH, Loh CH, Chen LK. Determinants and indicators of successful ageing associated with mortality: a 4-year population-based study. Aging. 2020;12(3):2670–9.
Idler EL, Benyamin Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;21–37.
Viljanen A, Salminen M, Irjala K, Heikkila E, Isoaho R, Kivela SL, et al. Subjective and objective health predicting mortality and institutionalization: an 18-year population-based follow-up study among community-dwelling Finnish older adults. BMC Geriatr. 2021;21(1):358.
Ou JY, Peters JL, Levy JI, Bongiovanni R, Rossini A, Scammell MK. Self-rated health and its association with perceived environmental hazards, the social environment, and cultural stressors in an environmental justice population. BMC Public Health. 2018;18(1):970.
Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69(3):307–16.
WHO. Statistics Netherlands. Health interview surveys: towards international harmonization of methods and instruments. Volume 58. European: WHO Regional; 1996.
Ganna A, Ingelsson E. 5 year mortality predictors in 498,103 UK Biobank participants: a prospective population-based study. Lancet. 2015;386(9993):533–40.
Jylhä M, Guralnik JM, Ferrucci L, Jokela J, Heikkinen E. Is self-rated health comparable across cultures and genders? Journals Gerontol Ser B: Psychol Sci Social Sci. 1998;53(3):144–52.
Vingilis ER, Wade TJ, Seeley JS. Predictors of adolescent self-rated health: analysis of the National Population Health Survey. Can J Public Health Rev Can Santé Publique. 2002;93:193–7.
Zhang L, Bi X, Ding Z. Health lifestyles and Chinese oldest-old’s subjective well-being-evidence from a latent class analysis. BMC Geriatr. 2021;21(1):206.
Cui S, Yu Y, Dong W, Xu T, Huang Y, Zhang X, et al. Are there gender differences in the trajectories of self-rated health among Chinese older adults? An analysis of the Chinese longitudinal healthy longevity survey (CLHLS). BMC Geriatr. 2021;21(1):563.
Byun M, Kim E, Ahn H. Factors Contributing to Poor Self-Rated Health in older adults with Lower Income. Healthc (Basel). 2021;9(11).
Johansson E, Böckerman P, Lundqvist A. Self-reported health versus biomarkers: does unemployment lead to worse health? Public Health. 2020;179:127–34.
Mavaddat N, Valderas JM, Van Der Linde R, Khaw KT, Kinmonth AL. Association of self-rated health with multimorbidity, chronic disease and psychosocial factors in a large middle-aged and older cohort from general practice: a cross-sectional study. BMC Fam Pract. 2014;15:1–11.
Aguilar-Palacio I, Gil-Lacruz AI, Sánchez-Recio R, Rabanaque MJ. Self-rated health in Europe and its determinants: does generation matter? Int J Public Health. 2018;63(2):223–32.
Liu S, Qiao Y, Wu Y, Shen Y, Ke C. The longitudinal relation between depressive symptoms and change in self-rated health: a nationwide cohort study. J Psychiatr Res. 2021;136:217–23.
Bamia C, Orfanso P, Juerges H, Schöttker B, Brenner H, Lorbeer R, et al. Self-rated health and all-cause and cause-specific mortality of older adults. Individual data meta-analysis of prospective cohort studies participating in the CHANCES Consortium. Maturitas. 2017;103:37–44.
Heistaro S, Jousilahti P, Lahelma E, Vartiainen E, Puska P. Self rated health and mortality: a long term prospective study in eastern Finland. J Epidemiol Community Health. 2001;55(4):227–32.
Wuorela M, Lavonius S, Salminen M, Vahlberg T, Viitanen M, Viikari L. Self-rated health and objective health status as predictors of all-cause mortality among older people: a prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. 2020;20(1):120.
Mavaddat N, Parker RA, Sanderson S, Mant J, Kinmonth AL. Relationship of self-rated health with fatal and non-fatal outcomes in cardiovascular disease: a systematic review and meta-analysis. PLoS ONE. 2014;9(7):e103509.
DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21(3):267–75.
Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1989;279:585–92.
Idler EL, Discussion. Gender diferences in self-rated health, in mortality, and in the relationship between the two. Gerontologist. 2003;43:372.
Reinwarth AC, Wicke FS, Hettich N, Ernst M, Otten D, Brahler E, et al. Self-rated physical health predicts mortality in aging persons beyond objective health risks. Sci Rep. 2023;13(1):19531.
Singh-Manoux A, Dugravot A, Shipley MJ, Ferrie JE, Martikainen P, Goldberg M, et al. The association between self-rated health and mortality in different socioeconomic groups in the GAZEL cohort study. Int J Epidemiol. 2007;36(6):1222–8.
Sajjad A, Freak-Poli RL, Hofman A, Roza SJ, Ikram MA, Tiemeier H. Subjective measures of health and all-cause mortality–the Rotterdam Study. Psychol Med. 2017;47(11):1971–80.
Lyyra TM, Leskinen E, Jylhä M, Heikkinen E. Self-rated health and mortality in older men and women: a time-dependent covariate analysis. Arch Gerontol Geriatr. 2009;48:14–8.
Bauknecht J, Merkel S. Differences in self-reported health between low- and high-income groups in pre-retirement age and retirement age. A cohort study based on the European Social Survey. Health Policy Open. 2022;3:100070.
Almevall A, Almevall AD, Ohlin J, Gustafson Y, Zingmark K, Niklasson J, et al. Self-rated health in old age, related factors and survival: a 20-Year longitudinal study within the Silver-MONICA cohort. Arch Gerontol Geriatr. 2024;122:105392.
Sperlich S, Tetzlaff J, Geyer S. Trends in good self-rated health in Germany between 1995 and 2014: do age and gender matter? Int J Public Health. 2019;64(6):921–33.
Schellekens J, Ziv A. The role of education in explaining trends in self-rated health in the United States, 1972–2018. Demographic Res. 2020;42:383–98.
Lamidi EO. Trends in self-rated health by union status and education, 2000–2018. SSM - Popul Health. 2020;11:100616.
Drame M, Cantegrit E, Godaert L. Self-rated health as a predictor of mortality in older adults: a systematic review. Int J Environ Res Public Health. 2023;20(5).
Benyamini Y, Blumstein T, Lusky A, Modan B. Gender differences in the self-rated health–mortality association: is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist. 2003;43(3):396–405.
Vogelsang EM. Self-rated health changes and oldest-old mortality. J Gerontol B Psychol Sci Soc Sci. 2014;69(4):612–21.
Vogelsang EM. Feeling better at this age? Investigating three explanations for Self-Rated Health Improvements among the Oldest-Old. Gerontologist. 2017;58(5):825–34.
Diehr P, Williamson J, Patrick DL, Bild DE, Burke GL. Patterns of self-rated health in older adults before and after sentinel health events. J Am Geriatr Soc. 2001;49(1):36–44.
Benítez-Silva H, Ni H. Health status and health dynamics in an empirical model of expected longevity. J Health Econ. 2008;27(3):564–84.
Nielsen ABS, Siersma V, Kreiner S, Hiort LC, Drivsholm T, Eplov LF, et al. The impact of changes in self-rated general health on 28-year mortality among middle-aged Danes. Scand J Prim Health Care. 2009;27(3):160–6.
Wu Q, Zhang P. Longitudinal validity of self-rated health: the presence and impact of response shift. Psychol Health. 2023;38(7):905–26.
Wells Y, de Vaus D, Kendig H, Quine S. Health and wellbeing through work and retirement transitions in mature age: understanding pre-post and retrospective measures of change. Int J Aging Hum Dev. 2009;69(4):287–310.
Han B, Phillips C, Ferrucci L, Bandeen-Roche K, Jylha M, Kasper J, et al. Change in Self-Rated Health and Mortality among Community-Dwelling Disabled Older Women. Gerontologist. 2005;45(2):216–21.
Barghouth MH, Schaeffner E, Ebert N, Bothe T, Schneider A, Mielke N. Polypharmacy and the Change of Self-Rated Health in Community-Dwelling older adults. Int J Environ Res Public Health. 2023;20(5):4159.
Tur-Sinai A, Soskolne V. Socioeconomic status and health behaviors as predictors of changes in self‐rated health among older persons in Israel. Health Soc Care Commun. 2021;29(5):1461–72.
Wild PS, Zeller T, Beutel M, Blettner M, Dugi KA, Lackner KJ, et al. Gutenberg Health Study Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55(6–7):824–9.
Lampert T, Kroll L, Muters S, Stolzenberg H. Measurement of socioeconomic status in the German Health Interview and examination survey for adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5–6):631–6.
Monnat SM, Beeler Pickett C. Rural/urban differences in self-rated health: examining the roles of county size and metropolitan adjacency. Health Place. 2011;17:311–9.
Bethea TN, Lopez RP, Cozier YC, White LF, McClean MD. The relationship between rural status, individual characteristics, and self-rated health in the behavioral risk factor Surveillance System. J Rural Health. 2012;28:327–38.
Acknowledgements
Not applicable.
Funding
This work was supported by the government of Rhineland-Palatinate (‘Stiftung Rheinland Pfalz für Innovation’, contract No. AZ 961-386261/733), the research program ‘Wissen schafft Zukunft’ and ‘Schwerpunkt Vaskuläre Prävention’ of the Johannes Gutenberg-University of Mainz, and its contract with Boehringer Ingelheim and Philips Medical Systems including an unrestricted grant for the Gutenberg Health Study as well as through the grants from the Initiative Health Economy Rhineland-Palatinate by the Ministry of Health and the Ministry of Economics, Rhineland-Palatinate, Germany (AZ.623-1) and the Federal Ministry of Education and Research, Germany (BMBF, 01EO1003 and BMBF 01EO1503). P.S.W. and T.M. are PI’s of the DZHK (German Center for Cardiovascular Research), Partner Site Rhine-Main, Mainz, Germany.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
A.C.R. conceived and designed the analysis, communication and visualization of results, scientific project administration (management and coordination responsibility), drafted manuscript, approved final version to be published, agreed to be accountable for all aspects of the work. F.S.W. reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. K.K.R. reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. J.M.S. acquired funding for the study, conceived and designed the study, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. O.T. acquired funding for the study, conceived and designed the study, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. P.S.W. acquired funding for the study, conceived and designed the study, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. T.M. acquired funding for the study, conceived and designed the study, supervision and leadership, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. J.K. performed the analysis, visualization of results, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. K.J.L.: Acquired funding for the study, conceived and designed the study, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. N.P. acquired funding for the study, conceived and designed the study, reviewed manuscript for important intellectual content, approved final version to be published, agreed to be accountable for all aspects of the work. M.E.B. acquired funding for the study, conceived and designed the study, supervision and leadership, drafted manuscript, approved final version to be published, agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol and documents of the study were approved by the local data safety commissioner and by the ethics committee of the Medical Chamber of Rhineland-Palatinate (reference no. 2018–13720; original vote: December 12, 2017, latest update: September 27, 2021). Study investigations were all conducted in line with the Declaration of Helsinki and principles outlined in recommendations for Good Clinical Practice and Good Epidemiological Practice. Written informed consent was obtained from each participant before their inclusion in the study.
Consent for publication
Not applicable.
Competing interests
J.M.S. declares consulting honoraria from Akero, 89Bio, Boehringer Ingelheim, Ipsen, Inventiva Pharma, Madrigal, Northsea Therapeutics, Novo Nordisk, Roche, Siemens Healthineers, research Funding from Boehringer Ingelheim and speaker Honoraria from Novo Nordisk, Madrigal, MedPublico GmbH. The others authors declare none.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Reinwarth, A.C., Wicke, F.S., Rückert, K.K. et al. Change of self-rated physical health predicts mortality in aging individuals: results of a population-based cohort study. Arch Public Health 82, 130 (2024). https://doi.org/10.1186/s13690-024-01363-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-024-01363-9