Abstract
Background
In recent years, Saudi Arabia has witnessed staggering rates of hypertension and dyslipidemia-related cardiovascular (CV) deaths, overburdening the healthcare ecosystem of the country. Appropriate public health interventions can be devised through quantitative mapping of evidence. Identification of potential data gaps can prioritize future research needs and develop a ‘best-fit’ framework for patient-centric management of hypertension and dyslipidemia.
Methods
This review quantified data gaps in the prevalence and key epidemiological touchpoints of the patient journey including awareness, screening, diagnosis, treatment, adherence, and control in patients with hypertension and dyslipidemia in Saudi Arabia. Studies published in English between January 2010 and December 2021 were identified through a structured search on MEDLINE, Embase, BIOSIS, and PubMed databases. An unstructured search on public and government websites, including Saudi Ministry of Health, without date limits was carried out to fill data gaps. After exclusion of studies based on predefined criteria, a total of 14 studies on hypertension and 12 studies and one anecdotal evidence for dyslipidemia were included in the final analyses.
Results
The prevalence of hypertension was reported to be 14.0%–41.8% while that for dyslipidemia was 12.5%–62.0%. The screening rate for hypertension was 100.0% as revealed by the nationwide surveys. Among hypertensive patients, only 27.6%–61.1% patients were aware of their condition, 42.2% patients underwent diagnosis, 27.9%–78.9% patients received antihypertensive treatment, 22.5% patients adhered to treatment medication, while blood pressure (BP) control was achieved in 27.0%–45.0% patients. Likewise, among patients with dyslipidemia, 10.5%–47.3% patients were aware of their condition, 34.6% patients were screened, and 17.8% underwent diagnosis. Although high treatment rates ranging from 40.0%–94.0% were reported, medication adherence recorded was 45.0%–77.4% among the treated patients. The overall low control rates ranged from 28.0%–41.5%.
Conclusions
The study findings highlight evidence gaps along key touchpoints of patient journey. Reinforcing the efforts for high-quality evidence-based research at a national level may pave a path for better resource utilization and provide guidance to practice and amend health policies for patients, healthcare practitioners (HCPs), and healthcare policy makers for better patient outcomes in Saudi Arabia.
Similar content being viewed by others
Background
The burden of noncommunicable diseases (NCDs) has been a growing challenge faced by the global community. The mortality due to NCDs has undergone a huge transition particularly across Western countries and extending to countries in the Middle East North Africa (MENA) region and Asia [1, 2]. Saudi Arabia has been at the cusp of this shift with a reported 73.0% of all deaths attributed to NCDs [2]. The ever-increasing population of Saudi Arabia along with major lifestyle changes, rapid economic and technological growth has exposed the country to a myriad of lifestyle-related NCDs including hypertension, dyslipidemia, diabetes mellitus (DM), obesity, and coronary artery diseases (CAD) [3]. Likewise, the exponential increase in life expectancy (45.6–74.9 years) by nearly 30.0 years over the past six decades has also led to a corresponding rise in NCDs [4]. Although the mean age of overall population remains low compared with Western countries, recent estimates suggest incremental increase in the aging population from 5.6% in 2017 to 22.9% in 2050 [5]. Cardiovascular diseases (CVDs) remain a major cause of deaths (37.0%) in Saudi Arabia [6]. Although hypertension, smoking, DM, and dyslipidemia are the major modifiable risk factors for CVDs, emerging robust data suggest hypertension to be an independent risk factor strongly linked with various CVD complications [7, 8]. Likewise, dyslipidemia is associated with a two-fold higher risk of CVD causation [9].
Huge financial investments have been made by the Saudi government in the healthcare sector along with the provision of accessible healthcare services. Despite this, a high prevalence of hypertension (15.2%, hypertension; 40.6%, prehypertension) and dyslipidemia (43.0%) has been reported by two recent nationwide surveys [10, 11]. Understandably, there are certain barriers for patients and healthcare practitioners (HCPs) that can hinder adequate utilization of healthcare facilities. From the patients’ perspective, undermining the importance of blood pressure (BP) screening, inconsistent follow-up with the primary healthcare clinics (PHCCs) due to limited technical knowledge to avail online consultations, variations in the distribution of PHCCs across urban and rural regions, lower number of HCPs in PHCCs (lower by 40% vs. hospitals), are some of the hindrances in the patient journey [12,13,14]. As for the HCPs, there is a notably low adherence to treatment guidelines and an absence of validated risk assessment tools designed for the local population. This leads to missed screening opportunities in appropriate individuals that can constitute a significant barrier for timely diagnosis and treatment and may lead to poor CVD prognosis [15]. Additionally, socioeconomic factors associated with CVDs, gender-based inequalities, regional differences, and diverse cultural norms across different regions of Saudi Arabia may constitute another hurdle in primary prevention efforts [1, 12].
Frequent nationwide and regional screening campaigns, constant and unbiased medical communication between patients and HCPs, and patient engagement programs in the community settings can lead to better healthcare facilities utilization, thereby reducing the burden of hypertension and dyslipidemia in Saudi Arabia [12]. A longitudinal patient journey map can reflect on the critical needs of managing these NCDs from the patients’ perspective and that can help strategizing the treatment goals, improving the patient-HCP communication, and eventually patient care [16]. This can be achieved by mapping patients’ disease journey through six broad touchpoints, namely awareness, screening, diagnosis, treatment, adherence, and control.
Previously, a national survey that mapped patient journeys in the Saudi population in 2005 reported > 1200 participants to be hypertensive with less than half of them being aware, receiving treatment, and having their BP controlled [17]. However, the studies reporting patient journeys in the following years were region-specific individual studies done at different times [18]. This may not provide an accurate estimate across all the journey touchpoints within the Saudi population who already have varied cultural norms and behavior towards CVD management [19]. Under such circumstances, a literature review with quantitative mapping and data visualization including the patient journey touchpoints can identify patients at-risk by providing a holistic perspective on risk factors stratified by age, gender, and dwelling place (urban or rural). Moreover, no Saudi studies could map the CVD care continuum through the lens of diverse settings, i.e., community or multilevel healthcare. Such data mapping can reflect upon the missed opportunities along the care continuum within both the settings—community healthcare: for risk factor identification and modification; and diagnosis and healthcare: for targeted treatments (first line and advanced) and palliative care [20]. Through this review, the overall evidence gap map thus generated can interest the researchers and clinicians to implement necessary steps towards closing the gap and provide nuanced care towards CVDs while ensuring smooth transition through each level of patient journey.
Traditionally, high-quality research outcomes focus on a few select developed countries, wherein the data across global population is extrapolated to locally design country-specific or region-specific guidelines. This results in inaccurate patient journey mapping due to lack of real-world local data [21]. Localized data mapping can aid global policy makers design priority framework from the viewpoint of recommending nutrition and lifestyle along with estimating the overall economic burden resulting from CVDs. From the standpoint of Saudi Arabia, such evidence mapping studies help the international agencies guide Saudi Arabia towards an optimal utilization and distribution of resources, maintenance of inventories, and development of policies and strategies to help shape up practical approaches towards CVD management in the country [21, 22]. The evidence mapping can also ensure preparedness of policy makers and practitioners in prioritizing at-risk patient pool and budget infrastructure in an event of unprecedented health crisis, e.g., coronavirus disease 2019 (COVID-19) [23]. Furthermore, implementation of health programs and policies along with elaboration of comprehensive reforms and recommendations and devising prioritization matrices for future epidemiological research efforts within the Saudi population can maneuver the policies and improve overall health status of the country. Table 1 highlights a few of the many roles of evidence mapping studies in shaping healthcare policies on a local and global level.
The objective of this review is to present the data across various patient journey touchpoints (prevalence, awareness, screening, diagnosis, treatment, adherence, and control) of hypertension and dyslipidemia in Saudi Arabia to further strengthen the healthcare system and overall quality of care by providing direction. To achieve this objective, the following research questions were designed: How much is the evidence gap along each journey touchpoint specifically in the Saudi population barring the expatriates since last 10 years? What is the reason that led to those gaps?
Methods
Review design
An extensive literature review was conducted using structured and unstructured search strategies to identify studies dealing with patient journey touchpoints (awareness, screening, diagnosis, treatment, adherence, and control) for hypertension and dyslipidemia in Saudi Arabia. Hypertension was defined as an average systolic blood pressure (SBP) ≥ 140 mmHg and/or average diastolic blood pressure (DBP) ≥ 90 mmHg. Dyslipidemia was defined as total cholesterol (TC) of ≥ 5.0 mmol/L or ≥ 200.0 mg/dL [21]. Definitions of each patient journey touchpoint are provided in Additional file 1. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used in this review, with minor modifications to fit within the scope of this study. The evidence was mapped using MAPS (Mapping the Patient Journey Towards Actionable Beyond the Pill Solutions) methodological approach [18, 21]. The mapping strategy was divided into six steps: (1) developing a comprehensive search strategy; (2) establishing the inclusion and exclusion criteria; (3) screening and shortlisting; (4) supplementing with additional and/or local data; (5) data extraction and synthesis; and (6) evidence mapping.
Search strategy
An electronic structured search was conducted to identify studies published from 01 January 2010 to 31 December 2021 through Medline and Embase databases using the keywords related to hypertension and dyslipidemia and different touchpoints of patient management. The comprehensive search was designed to ensure the inclusion of all studies conducted in Saudi Arabia on hypertension and dyslipidemia. The complete search strategy is provided in Additional file 2.
To address data gaps in the structured search, an additional unstructured search was conducted through the Incidence and Prevalence Database (IPD), World Health Organization (WHO), Country’s Ministry of Health (MOH), and Google Scholar websites. No date limits were applied to the unstructured search. Data gaps were further supplemented with anecdotal data from clinical experts in Saudi Arabia.
Eligibility criteria
Eligible publications were based on: (a) studies on the human adult population (aged ≥ 18 years) with hypertension and dyslipidemia that focused on the prevalence and epidemiological data from different patient journey touchpoints (awareness, screening, diagnosis, treatment, adherence, and control or remission); (b) peer–reviewed published systematic review and/or meta-analysis, narrative reviews, observational studies; (c) studies representing patient population from Saudi Arabia.
Studies with special populations such as pregnant women; patients with comorbidities, non-English language studies, thesis abstracts; letters to the editor, and editorials; studies including specific patient subgroups; duplicate records and studies without full text were excluded from the analysis.
Screening of studies
The first independent reviewer retrieved the studies using both structured and unstructured search strategies. Studies were screened and selected based on their title and abstract. The second independent reviewer assessed the selected studies considering predetermined inclusion/exclusion criteria and reviewed the full text. Any disagreements between the first and the second reviewer were resolved to arrive at a mutual consensus. A comprehensive review through manual screening of all the selected studies was carried out again, prior to data extraction and synthesis. Furthermore, any identified data gaps were supplemented with anecdotal data from clinical experts in Saudi Arabia.
Data extraction and synthesis
Following a thorough manual screening of all the selected studies, relevant studies were shortlisted and exported to the data extraction grid in Microsoft Excel. Quantitative data pertaining to the various patient journey touchpoints (awareness, screening, diagnosis, treatment, adherence, and control) were captured in the grid. The data extraction grid was rechecked and verified by the reviewers for consistency and accuracy. The grid was further synthesized to highlight the evidence gap map for both hypertension and dyslipidemia.
Results
Screening of studies for hypertension
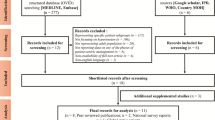
A total of 524 studies were retrieved from the structured and unstructured searches on the prevalence and the patient journey touchpoints of hypertension. Of these, 512 studies were obtained through structured search and 12 studies from unstructured search. Most of the excluded studies represented specific patient subgroups (pregnant women, patients with other comorbidities, n = 234) and diseases other than hypertension (n = 135). Other reasons for exclusion of studies were nonavailability of data on patient journey touchpoints (n = 48), < 18 years of age (n = 34), lack of nationally representative population (n = 18), data not from Saudi Arabia (n = 5), nonavailability of full text (n = 5), duplicate studies (n = 4), case studies (n = 2), studies published before 2010 (n = 1). Twenty-eight studies from the structured and 10 studies from the unstructured searches were selected for detailed review. Twenty-four studies from the structured search were excluded as they did not match the MAPS criteria definition for patient journey touchpoints. Finally, four studies from the structured searches [10, 17, 24, 25] and 10 studies from the unstructured searches [11, 26,27,28,29,30,31,32,33,34] were included in the final analyses. The literature search and study selection process are presented in Fig. 1.
Flowchart describing the inclusion of hypertension-related studies in the final analysis. Abbreviations: IPD, Incidence and Prevalence Database; MAPS, Mapping the Patient Journey Towards Actionable Beyond the Pill Solutions; MOH, Ministry of Health; n, number of studies; WHO, World Health Organization
Description of included studies for hypertension
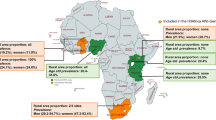
The included studies were conducted both in community-based and hospital-based settings. The overall prevalence of hypertension in community-based settings ranged from 14.0%–36.0% [10, 11, 17, 25, 26, 29, 34], while the prevalence in hospital-based settings ranged from 14.8%–41.8% [24, 30, 31]. The prevalence data as reported in two studies, i.e., Global Status report on NCDs and the Kingdom of Saudi Arabia World Health Survey (KSA WHS), both in collaboration with WHO, ranged from 14.0%–21.8% [11, 26]. A nationwide multistage random sampling carried out in 20 health regions of Saudi Arabia reported a hypertension prevalence of 25.5%; 44.7% patients were aware of their condition, 71.8% patients received treatment for their condition, and 37.0% patients achieved hypertension control [17]. A subgroup analysis of the Africa Middle East Cardiovascular Epidemiological (ACE) study revealed a prevalence of 41.8% among young Saudi patients and expatriates [17].
A nationwide multistage survey carried out by El Bcheraoui et al. reported an overall prevalence of hypertension of 15.2%; further, 42.2% patients were diagnosed with hypertension [10]. About 78.9% of the previously diagnosed hypertensive patients were receiving treatment for hypertension management and 45.0% of the treated patients had achieved control [10]. Two studies involving Saudi national subgroup analysis of the Prospective Urban Rural Epidemiology (PURE) study reported data that were both standardized and non-standardized by age. The first subgroup analysis reported hypertension prevalence to be 36.0%; 56.0% patients were aware of their condition, 53.0% patients were receiving treatment, and 27.0% patients were having controlled BP [25]. Similarly, the second subgroup analysis reported hypertension prevalence (non-standardized by age) to be 30.3%; further, 61.1% patients were aware of their condition, 58.9% patients received treatment, and 30.7% reported hypertension control [29].
A nationwide screening campaign as a part of the global screening initiative, May Measurement Month, reported 100.0% screening of hypertension [26]. The campaign reported that 29.2% patients were hypertensive, 60.8% patients were aware of their condition and were receiving treatment, and 39.3% patients had their BP controlled [30]. One university-based study revealed that hypertension was prevalent among 31.0% patients [34], while one study reported 27.6% of patients to be aware of their condition [32]. The screening rates among the patients was reported to be 100.0% from three studies [30, 32, 34]. As per the data obtained from two cross-sectional studies, the average prevalence of hypertension was found to be 14.8% [29], whereas the awareness, stratified by the patients’ knowledge of SBP and DBP was reported to be 48.7% and 47.3%, respectively [33]. The detailed study characteristics are presented in Table 2.
Screening of studies for dyslipidemia
A total of 373 studies were retrieved from the structured and unstructured searches on the prevalence and the patient journey stages of dyslipidemia. Of these, 362 studies were found through structured search and 11 studies through unstructured search. Most of the excluded studies represented specific patient subgroups (pregnant women, patients with other comorbidities, n = 168) and did not have dyslipidemia (n = 56). Other reasons for exclusion of studies were non-availability of data on stages of patient journey touchpoints (n = 82), < 18 years of age (n = 22), lack of nationally representative population (n = 11), data not from Saudi Arabia (n = 2), non-availability of full text (n = 10), duplicate records (n = 2), and editorials (n = 1). Finally, two studies from the structured searches [35, 36] and 10 studies from the unstructured searches [11, 29, 33, 37,38,39,40,41,42,43] were included. To fill the data gap, one anecdotal evidence was included in the final analyses. The literature search and study selection process are presented in Fig. 2.
Flowchart describing the inclusion of dyslipidemia-related studies in the final analysis. Abbreviations: IPD, Incidence and Prevalence Database; MAPS, Mapping the Patient Journey Towards Actionable Beyond the Pill Solutions; MOH, Ministry of Health; n, number of studies; WHO, World Health Organization
Description of included studies for dyslipidemia
The studies from community-based settings reported a prevalence ranging from 12.5%–43.0% [11, 29, 43], while the prevalence in hospital-based settings was 62.0% [41]. As per the data reported by KSA WHS, dyslipidemia was prevalent in 43.0% of the Saudi population [11].
The Saudi national subgroup analysis of the PURE study reported the prevalence to be 32.1% [29]. Two cross-sectional survey studies reported the dyslipidemia prevalence to be 12.5% and 62.0%, respectively [41, 43]. A Saudi national subgroup analysis of the SHIS (Saudi Health Interview Survey) study revealed that 17.8% participants who self-rated their health to be poor/fair were diagnosed with dyslipidemia [35]. Lipid profile screening rate was reported in only one cross-sectional survey study (34.6%) [38]. A multinational survey study, which included Saudi Arabia, reported a very high proportion of patients (94.0%) undergoing treatment, particularly with statins [36]. Likewise, the Saudi national subgroup analysis of PURE study indicated that 40.6% of the patients were undergoing lipid-lowering treatment as secondary prevention of CVD [39]. Similarly, in a prospective cohort study, although 40.0% reported as being prescribed the lipid-lowering drugs, only 15.0% received appropriate dosing [42].
The Morisky Medication Adherence Scale (MMAS) assessing medication adherence rate reported that 26.0% patients adhered to the therapy which increased to 62.0% over nine months [42]. A retrospective cross-sectional study that captured data from electronic health records (EHRs) of patients with type 2 diabetes (T2D) and dyslipidemia showed 77.4% adherence to lipid-lowering treatment, while 41.5% of the patients displayed control [40]. According to the anecdotal data provided by Dr. Ashraf Amir, 45.0% patients were found to be adherent to the treatment. The study details are summarized in Table 3.
Discussion
This review presents the data across the patient journey touchpoints (awareness, screening, diagnosis, treatment, adherence, and control) for hypertension and dyslipidemia. However, there are inconsistencies across the number of studies included for each touchpoint leading to evidence gaps for both hypertension and dyslipidemia. By highlighting the gaps, the HCPs and healthcare policymakers of Saudi Arabia can be encouraged to design more research programs and develop more publications, which in turn will aid in evidence-based informed decision-making in routine clinical practice.
Hypertension: Gaps along patient journey touchpoints
The overall prevalence estimates of hypertension were represented in a wide range, which could be attributed to the heterogeneity of patients’ baseline characteristics, differences in the study settings (community-based or hospital-based), and difference in the severity of the disease. The prevalence reported from community-based settings were lower (14.0%–36.0%) [10, 11, 17, 25, 26, 29, 34, 35] than in hospital-based settings (14.6%–41.8%) [24, 30, 31], which is indicative that a majority of patients visiting the PHCC were with underlying cardiovascular (CV) risk factors, hypertension being one of them. This was in agreement with the results from previous studies that also showed higher prevalence of hypertension (30.0%–92.0%) [44, 45] in hospital settings compared with community-based studies (13.6%–26.1%) [46, 47]. Additionally, other reasons may include differences in the study duration between the two settings and its corresponding effect on disease severity and differences in diagnostic practices across different locations [24].
Majority of the studies revealed hypertension awareness to be strikingly low in male patients, rural population, and younger patients [25, 29, 30, 32]. On the contrary, increased awareness was observed among female patients, urban dwellers, geriatric patients, and those with chronic comorbidities [25, 29]. These findings were consistent with previous reports wherein heightened awareness was observed among females vs. males [48], urban population, and in patients with DM and CVD. [25] Although Saudi Arabia displays heightened hypertension awareness when compared with other Middle East countries, the hypertension awareness rates were still lower in comparison to other high-income countries (HICs) such as Germany and South Korea (40.0%–80.0%) [25, 49, 50]. Except for two screening campaigns held nationwide and in Eastern province, respectively, the review findings suggested a paucity in screening studies across Saudi Arabia [31, 32, 34]. The reason for high screening rates found in these studies (100.0%) is simply because all the patients underwent screening as part of the survey protocol which did not include targeted screening. However, previously reported community-based screening campaigns taking place in Eastern Province reported lower participant turnout (ranging from 21.0%-33.0%) [49, 50] for screening owing to refusal of undergoing long tedious screening procedures or lack of incentive schemes for participation [51]. Overall, the screening rates remained low in Saudi Arabia which was also similar to that observed in other Middle Eastern countries including United Arab Emirates (UAE), Iran, and Occupied Palestinian Territory (OPT) [25].
Low diagnosis rates (47.1%) trace back to lower rates of awareness and screening campaigns in Saudi Arabia. Although rates of diagnosis have improved over the last decade (from 11.5% to 47.1%), they still remain low when compared to HICs such as South Korea, Canada, and Iceland, where almost 70% of the hypertensive patients were accurately diagnosed [50, 52]. A wide variability was observed in the proportion of patients undergoing treatment (27.9%–78.9%) [10, 17, 25, 27, 29, 30]. Similar to the observations made on awareness, the participants who received treatment mainly belonged to geriatric, female, those with comorbidities and educated cohorts [10, 24, 25]. Although treatment rates in Saudi Arabia are higher, compared with UAE and Iran (45% and 43%, respectively), the treatment rates in HICs were reported to be > 70% [25, 52]. Further, proportion of patients adhering to antihypertensive medications was reported to be low in Saudi Arabia (22.5%) [28], which was similar to the findings from other Middle Eastern countries like OPT (16.9%) [53], but was lower than UAE (42.0%) [54]. Consistent with these findings, previously published studies have reported higher treatment (74.0%) and lower adherence rates (6.2%) within Saudi Arabia [52, 55]. Likewise, a huge variation was observed in the proportion of patients achieving BP control (27.0%–45.0%) [10, 17, 25, 29, 30], while HICs including Canada and Germany reported higher BP control (50.0%–69.0%) [52].
Overall, when compared with other Middle Eastern countries, the prevalence of hypertension reported within community-settings in Saudi Arabia (14.0%–36.0%) was found to be comparable with countries like Iran, Turkey, and Oman (19.2%–33.7%) [56]. The awareness in UAE, Iran and OPT ranged from 45.0%–57.0%, which was higher compared with Saudi Arabia (27.6%–61.1%). Treatment (27.9%–78.9%) and control rates (27.0%–45.0%) within Saudi Arabia were comparatively higher than that in Iran (treatment; 43.0% and control; 16.0%) and UAE (treatment; 45.0% and control; 14.0%), respectively [25]. The overall increasing trends in hypertension seen across all the patient journey touchpoints pose a major challenge to the healthcare system in Saudi Arabia. The gender differences observed in hypertension prevalence has a physiological basis as suggested by few gender-based analytical studies [57, 57,58,59]. The experimental models of hypertension show a higher level of angiotensin II receptors (type 1; AT1), which are mainly responsible for vasoconstriction, sodium reabsorption, and eventual rise in BP, in males vs. females [59]. Additionally, other challenges include disparity across various sections of the community with regards to the knowledge and attitude towards preventive healthcare, unhealthy lifestyle behavior, and lack of motivation among Saudi people to self-manage hypertension [10, 17]. Moreover, low numbers of evidence pertaining to each critical patient journey touchpoint can impede adequate implementation of health interventions among hypertensive patients (Fig. 3).
Dyslipidemia: gaps along patient journey touchpoints
The prevalence of dyslipidemia has increased steeply over the last many years from 12.5% to 43.0% [11, 29, 41, 43]. This increase could be attributed to lifestyle changes owing to rapid urbanization, poor diet, and low physical activity [35]. Dyslipidemia (with increased low-density lipoprotein cholesterol [LDL–C]) was the leading CV risk factor (32.1%–68.6%) among other risk factors, including hypertension, diabetes, smoking, obesity (body mass index [BMI] ≥ 30 kg/m2), or abdominal obesity [24, 40, 41]. These findings were comparable to HICs in Western Europe (40.0%–60.0%) and North America (40.0%–45.0%) [60]. Elevated LDL-C over a prolonged period can increase the risk of atherosclerotic cardiovascular diseases (ASCVDs) events by almost five times, which reiterates the importance of maintaining an optimum lipid profile [61]. Dyslipidemia was also positively associated (62.0%) in patients with increased body mass index (BMI) and waist circumference (WC) along with faulty lifestyle and dietary habits such as inadequate sleep, caffeine intake, and consumption of sugary carbonated beverages [41].
A wide variability in dyslipidemia awareness level (10.5%–47.3%) was observed in geriatric patients, uneducated individuals, and rural dwellers in Saudi Arabia [33, 37]. The awareness rates pertaining to CVD risk factors including dyslipidemia in the urban educated population in Saudi Arabia were also within this range (47.1%) [62]. A small proportion of patients (34.6%) visiting the PHC underwent lipid screening in Saudi Arabia. This could be because of lack of awareness pertaining to the importance of regular screenings, especially among younger individuals (> 20 years), gender disparity, and unemployment [38]. On the other hand, UAE reported higher screening rates (49.3%) in > 8000 patients [63].
As reported by CEPHEUS study, a high proportion of patients (94.0%) with high and very high ASCVD risk underwent statin therapy. This reinstates the importance of dyslipidemia management in the primary prevention of CVD events, especially in individuals with multiple CVD risk factors [36]. However, a lower proportion of patients (40.6%) were receiving lipid-lowering treatment for secondary prevention of CVDs. This was due to the inequality in wealth distribution persistent in Saudi Arabia that led to inequality in accessing adequate treatment and poor prognosis of CVDs. These observations agree with previous Saudi studies that reported underwhelming use of high-intensity statins for secondary prevention in patients with ASCVD or sub-optimal adherence to prevention guidelines in secondary prevention of coronary events [64, 65]. Conversely, this trend was not observed in other HICs such as UAE, Canada, and Sweden, where more than half of the population received lipid-lowering treatment for secondary prevention [39]. Furthermore, a higher adherence rate (62.0%–77.4%) was observed in patients with type 2 DM and dyslipidemia which was the result of extensive dyslipidemia education programs that were undertaken at the beginning of the study [42]. The anecdotal evidence for adherence (45.0%) further calls for urgent implementation of such education programs across various communities in Saudi Arabia. Notably, the control rates were found to be lower (23.0%–41.5%) among the patients, which could be due to non-indulgence in physical activity or not having a controlled diet which reemphasizes the important role of non-pharmacological therapy along with drug therapy [36, 40]. Moreover, drug intolerance, inadequate PHC follow-up and using medications that are not evidence-based, especially in females, can hamper optimal lipid control [36].
While, the prevalence of dyslipidemia in Northern Emirates was reported to be slightly higher (72.5%) [66] compared to Saudi Arabia (12.5%–62.0%), the Gulf Registry of Acute Coronary Events (Gulf RACE) encompassing countries such as Bahrain, Kuwait, Qatar, Oman, UAE, and Yemen had a lower prevalence (32.7%) [67]. Egypt reported lower screening rate (8.6%) compared to Saudi Arabia (34.6%). In other middle-eastern countries like Jordan, Lebanon, UAE, Kuwait, and Oman, higher treatment (55.9%) and control rates (52.4%) were observed, compared to that in Saudi Arabia (treatment rate: 40.0% and control rate: 28.0%–41.5%, respectively) [36, 38, 42].
Overall, a huge scarcity in data for dyslipidemia along each patient journey touchpoint has been observed in Saudi Arabia that deters targeted management strategies (Fig. 4).
Scope of recommendations for enhanced patient care and health outcomes
The Saudi Arabia healthcare system has rapidly evolved over the last 20 years and is home to world-class hospitals and efficient healthcare facilities. The Saudi Healthcare National Transformation Program (NTP) has been a driving force for Saudi Vision 2030 to bring about a transformation in the healthcare sector by prioritizing NCD prevention [29, 68]. However, despite the availability of adequate resources and implementation of multiple initiatives, numerous evidence gaps along each patient journey touchpoint in hypertension and dyslipidemia still persist. This may be partly due to less NCD research output from Saudi Arabia compared with other Middle Eastern countries and a smaller number of national awareness programs and multi–faceted healthcare policies [29, 68]. Furthermore, the current COVID-19 pandemic has adversely impacted the overall management of hypertension and dyslipidemia owing to partial and complete lockdowns and cancellation of in–person visits to PHCCs [69].
As the future steps to reduce CVD burden within the Saudi population, active collaborations are needed between patients, HCPs, community/hospital pharmacists, and healthcare policy makers to enhance coordination between primary care and health services delivery systems, backed by adequate funding and leadership for uniform implementation [70]. Such collaborations can also help identify barriers along the patient journey and plan future research to address them. This could be accomplished by emphasizing national-level epidemiological studies over region-based data, with bias-free study designs and protocols for hypothesis testing. Further, dissemination of study results adhering to standardized reporting guidelines such as STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) can ensure study ethics and methodological robustness [71].
Table 4 represents recommendations for enhanced patient care and health outcomes across all patient journey touchpoints, designed by all authors through mutual consensus.
Limitations
This review had several limitations. Firstly, we excluded studies conducted in specific patient subgroups (pregnant women, patients with co-morbidities). However, the reason for this exclusion was solely based on the objective to understand and highlight the evidence gaps in the patient journey of hypertension and dyslipidemia, respectively. Furthermore, adding data from patients with comorbidities would have increased literature volume diluting the objectives of this study or skew the overall effect size resulting from additional treatment/patient arms. As a result, the gaps in hypertension and dyslipidemia patients’ journey may not be extrapolated from participants with comorbidities [80]. Nevertheless, this could have led to the underestimation of the overall data and can be a perspective for future research by designing appropriate study methodology. Secondly, we chose to exclude non-English language studies to overcome the reduced traceability of studies that are published in local language and the associated translation costs, although attempts were made to include local language studies with data validated by local experts [81]. Thirdly, we excluded specific study types (i.e., thesis abstracts; letters to the editor, and editorials) to ensure that studies of high quality and strong recommendations (systematic reviews followed by observational studies and narrative reviews) be considered to enable the readers make evidence-informed decisions [76]. Furthermore, we did not include publication bias analysis for the selected studies, and we did not calculate the pooled estimates for each touchpoint owing to the wide variability in data. We considered only TC while including studies for dyslipidemia without considering additional variables such as LDL-C, triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C). Finally, we could not include information on the efficacy of specific treatment intervention(s). This was again attributed to our underlying objective for this study which was to only highlight the evidence gaps in the patient journey.
Conclusion
This review presented detailed insights across various patient journey touchpoints during the management of hypertension and dyslipidemia in Saudi Arabia. A comprehensive search strategy was applied, and major data gaps were identified. Addressing these data gaps can aid the healthcare stakeholders to strategize a goal-oriented approach for achieving positive CV outcomes among patients and further strengthen the Saudi Arabia healthcare system. Multi-faceted healthcare policies including well-defined protocols for NCD prevention along with collective effort from the triad of patients, HCPs, and the healthcare policy makers can amplify the quality of care and better utilization of healthcare resources. Furthermore, this review emphasizes the need for more epidemiological research, national-level surveillance data highlighting the changing patterns of CVD risk factors, and mortality among key subpopulations including high-risk individuals, women, and children.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files). Anecdotal data as personal communication from the local expert in the context of dyslipidemia that has been used in this study will be available on request from the corresponding author.
Abbreviations
- ACE study:
-
Africa Middle East Cardiovascular Epidemiological study
- ASCVD:
-
Atherosclerotic cardiovascular diseases
- AT1:
-
Angiotensin II receptor type 1
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CAD:
-
Coronary artery diseases
- CEPHEUS study:
-
Centralized Pan-Middle East Survey on the under-treatment of hypercholesterolemia (CEPHEUS) study
- COVID-19:
-
Coronavirus disease
- CV:
-
Cardiovascular
- CVDs:
-
Cardiovascular diseases
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- HCPs:
-
Healthcare practitioners
- HDL-C:
-
High-density lipoprotein cholesterol
- HIC:
-
High income countries
- IPD:
-
Incidence and Prevalence Database
- KSA WHS:
-
Kingdom of Saudi Arabia World Health Survey
- LDL–C:
-
Low-density lipoprotein cholesterol
- MAPS:
-
Mapping the Patient Journey Towards Actionable Beyond the Pill Solutions
- MENA:
-
Middle East, North Africa
- MMAS:
-
Morisky Medication Adherence Scale
- NCDs:
-
Non communicable diseases
- NTP:
-
National Transformation Program
- OPT:
-
Occupied Palestinian Territory
- PHC:
-
Primary healthcare
- PHCCs:
-
Primary healthcare clinics
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PURE study:
-
Prospective Urban Rural Epidemiology study
- SBP:
-
Systolic blood pressure
- SHIS:
-
Saudi Health Interview Survey
- T2D:
-
Type 2 diabetes
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- UAE:
-
United Arab Emirates
- WC:
-
Waist circumference
- WHO:
-
World Health Organization
References
Al-Hanawi MK. Socioeconomic determinants and inequalities in the prevalence of non-communicable diseases in Saudi Arabia. Int J Equity Health. 2021;20(1):174.
GBD 2017 Saudi Arabia Collaborators. The burden of disease in Saudi Arabia 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Planet Health. 2020;4(5):e195–208. https://doi.org/10.1016/S2542-5196(20)30075-9.
Al-Hazzaa HM, Albawardi NM. Obesity, lifestyle behaviors, and dietary habits of Saudi adolescents living in Riyadh (ATLS-2 Project): revisited after a ten-year period. Life (Basel). 2021;11(10):1078. https://doi.org/10.3390/life11101078.
Young Y, Alharthy A, Hosler AS. Transformation of Saudi Arabia’s health system and its impact on population health: what can the USA learn? Saudi J Health Syst Res. 2021;1:93–102.
Alqahtani BA, Alenazi AM, Alshehri MM, Osailan AM, Alsubaie SF, Alqahtani MA. Prevalence of frailty and associated factors among Saudi community-dwelling older adults: a cross-sectional study. BMC Geriatr. 2021;21:185.
Alghnam S, Alessy SA, Bosaad M, Alzahrani S, Al Alwan II, Alqarni A, et al. The Association between obesity and chronic conditions: results from a large electronic health records system in Saudi Arabia. Int J Environ Res Public Health. 2021;18:12361.
Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285–92.
Kannel WB. Risk stratification in hypertension: new insights from the Framingham Study. Am J Hypertens. 2000;13(Suppl 1):3–10. https://doi.org/10.1016/s0895-7061(99)00252-6.
Gebreegziabiher G, Belachew T, Mehari K, Tamiru D. Prevalence of dyslipidemia and associated risk factors among adult residents of Mekelle City Northern Ethiopia. PLoS One. 2021;16: e0243103.
El Bcheraoui C, Memish ZA, Tuffaha M, Daoud F, Robinson M, Jaber S, et al. Hypertension and its associated risk factors in the kingdom of Saudi Arabia, 2013: a national survey. Int J Hypertens. 2014;2014: 564679. https://doi.org/10.1155/2014/564679.
Biological Risk Factors. World Health Survey Saudi Arabia (SAUDI ARABIAWHS). 2021. https://www.moh.gov.sa/en/Ministry/Statistics/Indicator/Documents/Report-Biological-Risk-Factors.pdf. Accessed 19 Jan 2022.
Alharbi A, Alzuwaed J, Qasem H. Evaluation of e-health (Seha) application: a cross-sectional study in Saudi Arabia. BMC Med Inform Decis Mak. 2021;21:103.
Akl C, Akik C, Ghattas H, Obermeyer CM. The cascade of care in managing hypertension in the Arab world: a systematic assessment of the evidence on awareness, treatment and control. BMC Public Health. 2020;20:835.
Al Saffer Q, Al-Ghaith T, Alshehri A, Al-Mohammed R, Al Homidi S, Hamza MM, et al. The capacity of primary health care facilities in Saudi Arabia: infrastructure, services, drug availability, and human resources. BMC Health Serv Res. 2021;21:365.
Gosadi IM. Utilization of evidence-based guidelines for prevention of obesity and hypercholesterolemia among primary healthcare physicians in southwest of Saudi Arabia. Medicine (Baltimore). 2021;100: e28152.
Meyer MA. Mapping the patient journey across the continuum: lessons learned from one patient’s experience. J Patient Exp. 2019;6:103–7.
Saeed AA, Al-Hamdan NA, Bahnassy AA, Abdalla AM, Abbas MA, Abuzaid LZ. Prevalence, awareness, treatment, and control of hypertension among Saudi adult population: a national survey. Int J Hypertens. 2011;2011: 174135.
Faria-Neto JR, Yarleque C, Vieira LF, Sakane EN, Santos RD. Challenges faced by patients with dyslipidemia and systemic arterial hypertension in Brazil: a design of the patient journey. BMC Cardiovasc Disord. 2022;22:237.
Al-Baghli NA, Al-Ghamdi AJ, Al-Turki KA, El-Zubaier AG, Al-Mostafa BA, Al-Baghli FA, et al. Awareness of cardiovascular disease in eastern Saudi Arabia. J Family Community Med. 2010;17:15–21.
McClellan M, Brown N, Califf RM, Warner JJ. Call to action: urgent challenges in cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2019;139:e44–54.
Bharatan T, Devi R, Huang PH, Javed A, Jeffers B, Lansberg P, et al. A methodology for mapping the patient journey for noncommunicable diseases in low- and middle-income countries. J Healthc Leadersh. 2021;13:35–46.
Alqunaibet, A, Herbst CH, El Saharty S, Algwaizini, A. Noncommunicable diseases in Saudi Arabia : toward effective interventions for prevention. Int Dev Focus. 2021. https://openknowledge.worldbank.org/handle/10986/36546.
Downey A, Brown L, Calonge N. Improving and expanding the evidence base for public health emergency preparedness and response. National Academies Press (US); 2020. https://www.ncbi.nlm.nih.gov/books/NBK564000/.
Ahmed AM, Hersi A, Mashhoud W, Arafah MR, Abreu PC, Al Rowaily MA, et al. Cardiovascular risk factors burden in Saudi Arabia: The Africa Middle East Cardiovascular Epidemiological (ACE) study. J Saudi Heart Assoc. 2017;29:235–43.
Yusufali AM, Khatib R, Islam S, Alhabib KF, Bahonar A, Swidan HM, et al. Prevalence, awareness, treatment and control of hypertension in four Middle East countries. J Hypertens. 2017;35:1457–64.
Mendis S, Armstrong T, Bettcher D, Branca F, Lauer J, Mace C, et al. In: global status report on noncommunicable diseases. 2014. https://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf?sequence=1&isAllowed=y. Accessed 19 Jan 2022.
Alsolami F, Correa-Velez I, Hou XY. Factors affecting antihypertensive medications adherence among hypertensive patients in Saudi Arabia. Am J Med Med Sci. 2015;5:181–9.
Khayyat SM, Khayyat SM, Hyat Alhazmi RS, Mohamed MM, Abdul HM. Predictors of medication adherence and blood pressure control among saudi hypertensive patients attending primary care clinics: a cross-sectional study. PLoS ONE. 2017;12: e0171255.
Alhabib KF, Batais MA, Almigbal TH, Alshamiri MQ, Altaradi H, Rangarajan S, et al. Demographic, behavioral, and cardiovascular disease risk factors in the Saudi population: results from the Prospective Urban Rural Epidemiology study (PURE-Saudi). BMC Public Health. 2020;20:1213.
Aljuraiban GS, Al Slail FY, Aldhwailea SK, Badawi AA, Beaney T, Clarke J, et al. May Measurement Month 2019: an analysis of blood pressure screening results from Saudi Arabia. Eur Heart J Suppl. 2021;23(Suppl B):128–30.
Ajabnoor GMA, Bahijri S, Alamoudi AA, Al Raddadi R, Al-Ahmadi J, Jambi H, et al. The association between hypertension and other cardiovascular risk factors among non-diabetic Saudis adults-A cross sectional study. PLoS ONE. 2021;16: e0246568.
Elsheikh E, Gharash AA, Almohammed B, AlJumaah M, Al Omaish M, Albahrani A, et al. Social knowledge of symptoms, risk factors, causes and complications of hypertension among Al-Ahsa population. Saudi Arabia Medical Science. 2021;25:1355–63.
Gosadi IM, Daghriri KA, Otayf AA, Nemri AA, Kaal AA, Qussadi AM, et al. Are patients affected by chronic non-communicable diseases aware of their own clinical and laboratory parameters? A cross-sectional study from the south of Saudi Arabia. Saudi J Biol Sci. 2021;28:2951–5.
Khafaji MA, Al Ghalayini KW, Sait MK, Alorri RA, Garoub T, Alharbi EA, et al. Prevalence of diabetes and hypertension among King Abdulaziz University employees: data from first aid and cardiopulmonary resuscitation training program. Cureus. 2021;13: e20097.
Moradi-Lakeh M, El Bcheraoui C, Tuffaha M, Daoud F, Al Saeedi M, Basulaiman M, et al. Self-rated health among Saudi adults: findings from a National Survey, 2013. J Community Health. 2015;40:920–6.
Al-Zakwani I, Al-Mahmeed W, Arafah M, Al-Hinai AT, Shehab A, Al-Tamimi O, et al. Control of risk factors for cardiovascular disease among multinational patient population in the Arabian gulf. Curr Vasc Pharmacol. 2016;14:374–81.
Al-Qahtani M, Aloraini M, AlQahtani K, Alotaibi M, Alalyani S, Alanazi S, et al. Level of awareness regarding hypercholesterolemia, Saudi Arabia, Riyadh, 2017. Indo Am J Pharm Sci. 2019;6:4484–8.
Bahakim NO, Al-Ghamdi SH, Alyahya HF, Alburayk KB, Mahzari YI, Aldawsari AM. Awareness among the general population about lipid profile screening in individuals over 20 years old in Alriyadh, Saudi Arabia. Arch Med Sci Atheroscler Dis. 2019;4:e126–33.
Murphy A, Palafox B, O’Donnell O, Stuckler D, Perel P, AlHabib KF, et al. Inequalities in the use of secondary prevention of cardiovascular disease by socioeconomic status: evidence from the PURE observational study. Lancet Glob Health. 2018;6:e292–301.
Alwhaibi M, Altoaimi M, AlRuthia Y, Meraya AM, Balkhi B, Aldemerdash A, et al. Adherence to statin therapy and attainment of LDL cholesterol goal among patients with type 2 diabetes and dyslipidemia. Patient Prefer Adherence. 2019;13:2111–8.
Enani S, Bahijri S, Malibary M, Jambi H, Eldakhakhny B, Al-Ahmadi J, et al. The association between dyslipidemia, dietary habits and other lifestyle indicators among non-diabetic attendees of primary health care centers in Jeddah Saudi Arabia. Nutrients. 2020;12:2441.
AlAyoubi F, Hayajneh A, AlAyoubi S, El Shaer F. Effect of multidisciplinary dyslipidemia educational program on adherence to guidelines directed medical therapy in Saudi Arabia. Int J Pharm Res Allied Sci. 2021;10:35–41.
Al-Zahrani J, Shubair MM, Al-Ghamdi S, Alrasheed AA, Alduraywish AA, Alreshidi FS, et al. The prevalence of hypercholesterolemia and associated risk factors in Al-Kharj population, Saudi Arabia: a cross-sectional survey. BMC Cardiovasc Disord. 2021;21:22.
Kalantan KA, Mohamed AG, Al-Taweel AA, Abdul Ghani HM. Hypertension among attendants of primary health care centers in Al-Qassim region Saudi Arabia. Saudi Med J. 2001;22:960–3.
Al-Homrany MA, Khan MY, Al-Khaldi YM, Al-Gelban KS, Al-Amri HS. Hypertension care at primary health care centers: a report from Abha, Saudi Arabia. Saudi J Kidney Dis Transpl. 2008;19:990–6.
Al-Nozha MM, Abdullah M, Arafah MR, Khalil MZ, Khan NB, Al-Mazrou YY, et al. Hypertension in Saudi Arabia. Saudi Med J. 2007;28:77–84.
Elbashir B, Al-dkheel M, Aldakheel H, Aruwished N, Alodayani N. Hypertension in Saudi Arabia: assessing life style and attitudes. Int J Translat Med Res Public Health. 2020;4:23–9.
Mitwalli AH, Harthi AA, Mitwalli H, Juwayed AA, Turaif NA, Mitwalli MA. Awareness, attitude, and distribution of high blood pressure among health professionals. J Saudi Heart Assoc. 2013;25:19–24.
Zhou B, Danaei G, Stevens GA, Bixby H, Taddei C, Carrillo-Larco RM, et al. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639–51.
Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Al-Ghamdi AJ, Al-Turki KA, Al-Baghli NA, El-Zubaier AG. A community-based screening campaign for the detection of diabetes mellitus and hypertension in the eastern province, Saudi Arabia: methods and participation rates. J Family Community Med. 2007;14:91–7.
Al-Hamdan N, Saeed A, Kutbi A, Choudhry AJ, Nooh R. Characteristics, risk factors, and treatment practices of known adult hypertensive patients in Saudi Arabia. Int J Hypertens. 2011;2010: 168739.
Al-Ramahi R. Adherence to medications and associated factors: A cross-sectional study among Palestinian hypertensive patients. J Epidemiol Glob Health. 2015;5:125–32.
Bhagavathula AS, Shah SM, Aburawi EH. Medication Adherence and Treatment-Resistant Hypertension in Newly Treated Hypertensive Patients in the United Arab Emirates. J Clin Med. 2021;10:5036.
Alotayfi MJY, Alsohaimi SA, AL-Qadi BK, Mosa Kamil S, Aththi AJH, Alhazmi GAA, et al. Poor compliance to anti-hypertensive drugs in Saudi Arabia. Egypt J Hosp Med. 2018;73:6696–701.
Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci. 2014;16:126–30.
Al-Raddadi R, Al-Ahmadi J, Bahijri S, Ajabnoor GM, Jambi H, Enani S, et al. Gender differences in the factors associated with hypertension in non-diabetic saudi adults-a cross-sectional study. Int J Environ Res Public Health. 2021;18:11371.
Alanazi RW, Alenzi AAE, Alanazi SM, Alqahtani FMF, Alharbi AHM, Al muhammisah ASS, et al. Coexistence of prehypertension and hypertension and obesity in young adults in Arar, Saudi Arabia. Egypt J Hosp Med. 2018;70:2029–33.
Silva-Antonialli MM, Tostes RC, Fernandes L, Fior-Chadi DR, Akamine EH, Carvalho MH, et al. A lower ratio of AT1/AT2 receptors of angiotensin II is found in female than in male spontaneously hypertensive rats. Cardiovasc Res. 2004;62:587–93.
Yuyun MF, Sliwa K, Kengne AP, Mocumbi AO, Bukhman G. Cardiovascular diseases in Sub-Saharan Africa compared to high-income countries: an epidemiological perspective. Glob Heart. 2020;15:15.
Gidding SS, Allen NB. Cholesterol and atherosclerotic cardiovascular disease: a lifelong problem. J Am Heart Assoc. 2019;8: e012924.
Mujamammi AH, Alluhaymid YM, Alshibani MG, Alotaibi FY, Alzahrani KM, Alotaibi AB, et al. Awareness of cardiovascular disease associated risk factors among Saudis in Riyadh City. J Family Med Prim Care. 2020;9:3100–5.
Ellahham S, Almahmeed W, Yassine L, Saeed K. Understanding the management of hypertension and dyslipidaemia in UAE population: an evidence-based mapping of literature. Saudi J Med. 2021;6:367–78.
Alburikan KA, Asiri RM, Alhammad AM, Abuelizz AA, Bawazeer GA, Aljawadi MH. Utilization and adherence to guideline-recommended lipid-lowering therapy at an academic medical center. Ann Saudi Med. 2017;37:276–81.
Alzahrani A, Alosaim M, Malibarey WM, Alhumaidi AA, M Alhawaj AHM, Alsulami NJ, et al. Saudi family physicians’ knowledge of secondary prevention of heart disease: a national assessment survey. Arch Pharma Pract. 2019;10:54–9.
Mahmoud I, Sulaiman N. Dyslipidaemia prevalence and associated risk factors in the United Arab Emirates: a population-based study. BMJ Open. 2019;9: e031969.
Al Rasadi K, Almahmeed W, AlHabib KF, Abifadel M, Farhan HA, AlSifri S, et al. Dyslipidaemia in the Middle East: current status and a call for action. Atherosclerosis. 2016;252:182–7.
Alharbi MF. An analysis of the Saudi health-care system’s readiness to change in the context of the Saudi National Health-care Plan in Vision 2030. Int J Health Sci. 2018;12:83–7.
Tourkmani AM, ALHarbi TJ, Rsheed AMB, Alrasheedy AA, ALMadani W, ALJuraisi F, et al. The impact of telemedicine on patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia: findings and implications. J Telemed Telecare. 2023;29(5):390–8. https://doi.org/10.1177/1357633X20985763.
Almansour HA, Aloudah NM, Alhawassi TM, Chaar B, Krass I, Saini B. Cardiovascular disease risk prevention services by pharmacists in Saudi Arabia: what do policymakers and opinion leaders think? J Pharm Policy Pract. 2021;14:42.
Saquib N. A call to action to improve research quality in Saudi Arabia. Int J Health Sci (Qassim). 2018;12:1–2.
Alnofal FA, Alrwisan AA, Alshammari TM. Real-world data in Saudi Arabia: current situation and challenges for regulatory decision-making. Pharmacoepidemiol Drug Saf. 2020;29:1303–6.
Al-Hazzaa HM. Physical inactivity in Saudi Arabia revisited: a systematic review of inactivity prevalence and perceived barriers to active living. Int J Health Sci (Qassim). 2018;12:50–64.
Syed Meraj A, Mohammed AM. A study on the prevalence of risk factors for diabetes and hypertension among school children in Majmaah, Kingdom of Saudi Arabia. J Public Health Res. 2017;6:829.
Al-Gelban KS, Khan MY, Al-Khaldi YM, Mahfouz AA, Abdelmoneim I, Daffalla A, et al. Adherence of primary health care physicians to hypertension management guidelines in the Aseer region of Saudi Arabia. Saudi J Kidney Dis Transpl. 2011;22:941–8.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Al-Rasadi K, Alhabib KF, Al-Allaf F, Al-Waili K, Al-Zakwani I, AlSarraf A, et al. The Gulf Familial Hypercholesterolemia Registry (Gulf FH): design, rationale and preliminary results. Curr Vasc Pharmacol. 2020;18:57–64.
Carter BL, Bosworth HB, Green BB. The hypertension team: The role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens (Greenwich). 2012;14:51–65.
Alessa T, Hawley M, de Witte L. Identification of themost suitable app to support the self-management of hypertension: systematic selection approach and qualitative study. JMIR Mhealth Uhealth. 2021;9: e29207.
Boyd CM, Vollenweider D, Puhan MA. Informing evidence-based decision-making for patients with comorbidity: availability of necessary information in clinical trials for chronic diseases. PLoS ONE. 2012;7: e41601.
Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol. 2002;31:115–23.
Acknowledgements
The authors would like to thank Akshata Rao and Dr. Palash Kumar Das (both from Tata Consultancy Services, India) for providing medical writing assistance. The authors would also like to thank Dr. Shanthakumar V from Viatris for critically reviewing the draft. The study was sponsored by Upjohn, a legacy Pfizer division, now merged with Mylan to be Viatris.
Funding
The authors received no specific funding for this work. This study was funded by Upjohn, a legacy Pfizer division, now merged with Mylan to be Viatris. The funding organization had no influence on study design, analysis, or interpretation of data.
Author information
Authors and Affiliations
Contributions
AA, MA, and RA designed the research objectives, searched, and interpreted the articles, validated the data, drafted, and reviewed the manuscript. TA, KS, MY, and AS were involved in drafting and reviewing of the manuscript. All the authors revised the manuscript critically for the intellectual content and agreed with the results and conclusions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
As this analysis used aggregated data available in public domain with no individual level data, no ethics approval was necessary.
Consent for publication
Not applicable.
Competing interests
AA received honoraria for speaker activities from Pfizer, GlaxoSmithKline, and Sanofi. MA has no relevant interests to declare. RA received honorarium for speaker activities for GlaxoSmithKline. TA received honoraria for consulting, speaker or research activities from Pfizer and Sanofi. KS is an employee of Pfizer Canada. AS is an employee of Viatris while MY was the former employee of Viatris during the development of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Definitions for each patient journey touchpoints for hypertension and dyslipidemia.
Additional file 2.
Complete search strategy with keywords and Boolean operators along with inclusion and exclusion criteria for hypertension and dyslipidemia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amir, A., Alasnag, M., Al-Raddadi, R. et al. Patient journey for hypertension and dyslipidemia in Saudi Arabia: highlighting the evidence gaps. Arch Public Health 81, 122 (2023). https://doi.org/10.1186/s13690-023-01121-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-023-01121-3