Abstract
Objectives
To examine racial and ethnic disparities in postoperative opioid prescribing.
Data sources
Electronic health records (EHR) data across 24 hospitals from a healthcare delivery system in Northern California from January 1, 2015 to February 2, 2020 (study period).
Study design
Cross-sectional, secondary data analyses were conducted to examine differences by race and ethnicity in opioid prescribing, measured as morphine milligram equivalents (MME), among patients who underwent select, but commonly performed, surgical procedures. Linear regression models included adjustment for factors that would likely influence prescribing decisions and race and ethnicity-specific propensity weights. Opioid prescribing, overall and by race and ethnicity, was also compared to postoperative opioid guidelines.
Data extraction
Data were extracted from the EHR on adult patients undergoing a procedure during the study period, discharged to home with an opioid prescription.
Principal findings
Among 61,564 patients, on adjusted regression analysis, non-Hispanic Black (NHB) patients received prescriptions with higher mean MME than non-Hispanic white (NHW) patients (+ 6.4% [95% confidence interval: 4.4%, 8.3%]), whereas Hispanic and non-Hispanic Asian patients received lower mean MME (-4.2% [-5.1%, -3.2%] and − 3.6% [-4.8%, -2.3%], respectively). Nevertheless, 72.8% of all patients received prescriptions above guidelines, ranging from 71.0 to 80.3% by race and ethnicity. Disparities in prescribing were eliminated among Hispanic and NHB patients versus NHW patients when prescriptions were written within guideline recommendations.
Conclusions
Racial and ethnic disparities in opioid prescribing exist in the postoperative setting, yet all groups received prescriptions above guideline recommendations. Policies encouraging guideline-based prescribing may reduce disparities and overall excess prescribing.
Similar content being viewed by others
Introduction
In the United States (U.S.), prescription-based opioids have been a major contributor to the opioid epidemic as they carry a risk of dependence and addiction[1, 2] and can lead to use of illicit opioids such as heroin or fentanyl.[3, 4] Long-term opioid use is also associated with gastrointestinal issues, fractures, immunosuppression, and hormonal dysregulation.[5].
In the postoperative setting, opioids are of particular concern. Reports indicate that over half of opioids prescribed for postoperative pain management at discharge go unused,[6, 7] creating a reservoir of pills for potential misuse, abuse, and diversion.[8] In recent years, several institutions have developed postoperative opioid prescribing guidelines for common surgical procedures to reduce excess prescribing and to mitigate risks associated with these medications.[9,10,11,12,13,14].
Historically, the opioid epidemic has been framed as a public health issue impacting white communities.[15,16,17,18] This has in part been attributed to misconceptions among clinicians about pain tolerance and implicit biases about illicit drug use, resulting in lower opioid prescribing to communities of color.[19,20,21,22,23] Numerous studies have reported that non-Hispanic Black (NHB), Asian (NHA), and Hispanic individuals are less likely to receive prescription-based opioids than their non-Hispanic white (NHW) counterparts, or that they are more likely to receive opioid prescriptions in lower pill quantities or of lower potency in ambulatory and emergency department settings, even for conditions that can be definitively diagnosed and are objectively painful (e.g., bone fractures).[24,25,26,27,28] Whereas some have argued that such systematic discrimination may have inadvertently shielded certain groups from the downstream effects of overprescribing, data from the Kaiser Family Foundation suggest that opioid-related deaths have been increasing in communities of color for over a decade.[17].
Prior studies on disparities in postoperative opioid prescribing have focused primarily on in-hospital opioid administration or long-term opioid use.[29, 30] Fewer studies in this setting have examined discharge opioid prescribing for adults, especially across different surgical subspecialties or service lines.[25, 31–33] In this study, we utilized electronic health records (EHR) data from a community-based, multi-hospital healthcare delivery system in Northern California to test the hypothesis that racial and ethnic minority groups receive opioid prescriptions at postoperative discharge with lower morphine milligram equivalents (MME) than NHWs. We further conducted exploratory analyses to examine opioid prescribing by race and ethnicity relative to Mayo Clinic guideline recommendations[11,12,13] and to identify the source of potential differences in prescribing by race and ethnicity, including temporal trends and whether prescriptions were written within or above clinical guideline recommendations, to help inform future public health policy.
Methods
Study setting and design
This study was conducted at Sutter Health, a large, integrated and community-based healthcare delivery system in Northern California (https://www.sutterhealth.org/). Sutter has 24 acute-care hospitals and > 100 ambulatory-care clinics across 22 state counties, composed of both urban and rural communities. The Sutter patient population is diverse in terms of race and ethnicity and is representative of the underlying geographic area.
This study was conducted as a retrospective, observational analysis using data from the Sutter Health EHR (Epic; https://www.epic.com/) between January 1, 2015 and February 2, 2020 (study period). The RAND and Sutter Health Institutional Review Boards approved this study.
Surgical procedure selection
Our analysis included procedures within service lines that are broadly performed across Sutter hospitals: General Surgery, Orthopedic Surgery, and Obstetrics and Gynecology (Ob/Gyn). We mapped procedures to opioid prescribing guidelines developed by the Mayo Clinic for postoperative, at-home pain management.[11,12,13] These guidelines recommend 5-mg oxycodone pill quantities, based on consensus of multidisciplinary teams who reviewed patient survey data (Supplemental Table 1). We refer to each group of similar procedures associated with a specific guideline as a “guideline-procedure group.”
We selected the most frequent guideline-procedure groups for General Surgery (lumpectomy with or without sentinel lymph node biopsy (lumpectomy +/- SLNB) and laparoscopic appendectomy or cholecystectomy); Orthopedics (knee arthroscopy and total knee arthroplasty [TKA]); and Ob/Gyn (minimally-invasive surgery [MIS] gynecological procedures and Cesarean delivery [C-Section]). These procedures are among the most commonly performed in the United States.[34].
We selected Mayo Clinic guidelines because they most comprehensively covered the surgical procedures of interest compared to other published guidelines. In the case of uncomplicated C-Sections, guidelines followed at the Mayo Clinic are unpublished (personal communication with Professor Elizabeth Habermann, Ph.D., MPH, March 12, 2021); however, they are consistent with guidelines published by the Johns Hopkins University.[10].
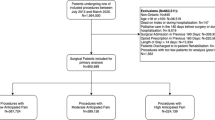
Cohort eligibility criteria
We identified adult patients (≥ 18 years of age) with a surgical procedure within guideline-procedure groups of interest during the study period and an opioid prescription written at hospital discharge. We restricted our analysis to patients with a single surgical procedure during the hospital encounter, a prescription for oral opioid pills at discharge, and those discharged to home. We applied these criteria to exclude more complex cases that may warrant higher opioid quantities than typical cases, or when opioids may be prescribed differently if patients were discharged elsewhere (e.g., nursing facility). Lastly, we excluded patients with prescriptions for > 500 pills (n = 2), as we expected these to be erroneous and would be rejected by dispensing pharmacies.
Outcome and explanatory variables
Outcomes were total MME[35] and prescriptions within or above guideline recommendations. The main explanatory variable was race and ethnicity. Sutter Health has collected self-reported race and ethnicity data since 2010, based on U.S. Census groupings.[36] For the purposes of this study, we operationalized race and ethnicity as: Hispanic, any race; NHW; NHB; NHA; and non-Hispanic other (NHO). The latter group included patients who self-identified as Native Hawaiian/Pacific Islander, Native American or Alaskan Native, mixed/more than one race, or self-reported as “other.” Individuals whose race/ethnicity were not documented in the EHR were excluded.
Covariates
We extracted EHR data on patient demographics, clinical characteristics, and encounter characteristics that might influence postoperative prescribing decisions, as well as opioid-prescriber characteristics. Patient demographics included age, sex, smoking status, and insurance payer. We further classified patients as existing primary-care patients within the health system (y/n). Patient clinical characteristics included body mass index (BMI; kg/m2), diabetes diagnosis (y/n), any chronic pain diagnosis (y/n), use of an opioid within 12 months prior hospital admission (y/n), concurrent benzodiazepine prescription (y/n), postoperative use/administration of an opioid in the 24 h before hospital discharge (y/n), and American Society of Anesthesiology (ASA) physical status[37] as documented at the time of surgery. We also attempted to identify mood disorders (e.g., major depressive disorder, bipolar disorder) and substance use disorders in the 12 months prior; however, no patients in our cohort had these documented on their problem list at the time of surgery.
Encounter characteristics included procedure name and date; procedure class (elective, emergent, or urgent/trauma); procedure duration; hospital length of stay; and discharge time of day. Opioid-prescriber characteristics included provider type (surgical, hospitalist, primary-care physician, other physician specialty, or advanced-care practitioner), years in practice, and sex. A variable was created to indicate whether the prescribing provider was the same as the surgeon who performed the procedure (y/n). Another variable was created to indicate whether the sex of the prescriber was concordant with the sex of the patient (y/n), as there is evidence that clinicians may prescribe opioid differently to patients on this basis.[38].
Covariates were classified as warranted or unwarranted in affecting opioid prescribing, based on their expected influence on pain level (or a proxy thereof) or patient safety.[13] Warranted covariates included patient age, gender, BMI, diabetes, current smoking, concurrent benzodiazepine prescription, chronic pain status, prior exposure to opioids, ASA physical status, procedure length, duration of hospital stay, guideline-procedure group, procedure type, and procedure month-year (given temporal trends in prescribing). Unwarranted covariates included patient insurance payer, existing health system patient status, and discharge time, as well as prescriber sex, specialty, years in practice, whether the prescriber was the surgeon who performed the procedure, and whether the prescriber’s sex was concordant with the patient’s sex.
Statistical analyses
Descriptive statistical analyses were performed on all variables. Continuous variables were summarized as means ± standard deviations (SD) and/or medians ± interquartile ranges (IQR). Categorical variables were summarized as percentages. Missing values for categorical variables were set to “missing/unknown.” For BMI, as a continuous variable, missing values (representing 1% of patient observations) and values < 13 or > 100 kg/m2 (representing < 1st and > 99th percentile, respectively) were imputed at the group mean.
Differences in prescribed total MME were estimated using propensity-weighted linear regression for each racial and ethnic minority group compared with the NHW group. Because total MME is not a normally distributed variable (data not shown), it was log transformed to meet modeling assumptions.[39] Model coefficients and 95% confidence intervals (CI) were back-transformed and interpreted as mean proportional differences.[40] Race and ethnicity-specific propensity weights were generated using logistic regression, by modelling the odds that an individual belonged to a minority group versus the NHW group, conditional on warranted covariates (as described above). For analyses by each race and ethnic minority group, NHW individuals received a propensity weight equal to the odds of being in the minority group, and minority group individuals received a propensity weight equal to 1. These weights shape the NHW reference group, so it is as similar as possible to the minority group on the warranted covariates. These methods have been described elsewhere.[41].
The main regression model for the primary outcome employs a technique typically referred to as doubly robust;[42] it features included covariates representing warranted variation in opioid prescribing and race and ethnicity-specific propensity-score weights to ensure comparison of equivalent groups. Models were run pooled and separately by guideline-procedure group for each race and ethnic minority group versus the NHW group. Statistical significance was set at an alpha of 0.05. For clinical interpretability, we calculated an approximate absolute difference in prescribed total MME and 5-mg oxycodone-equivalent pills using the unadjusted mean total MME for the NHW group and, from the statistical models, the mean proportional differences estimated for each racial and ethnic minority group versus the NHW group.
We conducted a series of exploratory analyses pooled and by guideline-procedure group. First, we examined opioid prescribing by race and ethnicity relative to guideline recommendations. Based on predicted values of prescribed 5-mg oxycodone-equivalent pills from the main model, we summarized excess pills prescribed relative to guideline recommendations for each racial and ethnic group; values at or below guidelines were set to 0. Second, we explored differences in opioid prescribing by race and ethnicity when prescriptions were within or above guideline recommendations. To this end, we added a variable for Mayo Clinic guideline concordance (y/n) in the main model as an interaction term with the race and ethnicity variable.
Lastly, we explored additional factors that influence differences in opioid prescribing between racial and ethnic groups by examining trends in prescribing disparities over time and by conducting a series of stepwise models and descriptively examining changes in coefficients for each racial and ethnic minority group compared to the NHW group. Model 1: race and ethnicity as the only covariate; Model 2 (main model): race and ethnicity + warranted covariates, and race and ethnicity-specific weights; Model 3: race and ethnicity + warranted and unwarranted covariates, and race and ethnicity-specific weights. These three models were repeated with opioid-prescribing provider fixed effects (Models 4–6) to control for differences in the distribution of patients by race and ethnicity within different prescribers.
Results
Cohort description
A total of 61,564 surgical patients met study eligibility criteria (Supplementary Fig. 1). Patients were on average 41.3 years of age and a majority were female (85.6%) (Table 1). Patients most frequently underwent C-Sect. (43.4%), followed by laparoscopic appendectomy/cholecystectomy (29.2%). Patients were most frequently NHW (46.4%); 27.4% were Hispanic, 12.7% were NHA, 6.2% were NHB, and 7.2% were NHO. Age and gender distributions varied by guideline-procedure group (see Supplementary Table 2).
Racial and ethnic minority groups tended to be younger than NHW patients, more frequently had diabetes, a documented chronic pain condition, and longer hospital stays (Table 1). NHB patients tended to have a higher BMI than other groups and more frequently had diabetes, more severe morbidity per ASA physical status, procedures of longer duration, and were more frequently current smokers versus other groups.
Main descriptive outcomes
Pooled mean and median prescribed total MME were 197.9 and 150, respectively (≅ 26.4 and 20.0 5-mg oxycodone-equivalent pills) (Table 2). Patients undergoing TKA had the highest mean and median MME, 578.6 and 450, respectively (≅ 77.1 and 60.0 pills), and patients undergoing lumpectomy +/- SLNB had the lowest MME (156.4 and 150.0, respectively; ≅ 20.9 and 20.0 pills). Within each guideline-procedure group, NHB patients received the highest mean total MME compared to all other racial and ethnic groups and, except for C-section, NHA patients had the lowest. No one race or ethnic group appeared to have opioid prescriptions with outlier MME quantities that could be driving higher mean values (see Supplemental Fig. 2).
Main model outcomes
After adjusting for warranted covariates, in pooled weighted linear regression analyses, statistically significant differences in opioid prescribing were observed by race and ethnicity. NHB patients received, on average, prescriptions with higher total MME than NHW patients (+ 6.4% [95% CI: 4.4%, 8.3%]), and Hispanic and NHA patients received prescriptions, on average, with lower total MME (-4.2% [-5.1%, -3.2%] and -3.6% [-4.8%, -2.3%], respectively) (Fig. 1). Differences in opioid prescribing by race and ethnicity were also observed within each guideline-procedure group, apart from MIS gynecological procedures. Specifically, mean percent difference in prescribed MME and approximate absolute total MME /5-mg oxycodone-equivalent pills for NHB patients versus NHW patients were higher for knee arthroscopy (+ 15.6% ≅ +45.0 MME or + 6.0 pills), lumpectomy +/- SLNB (+ 12.8% ≅ +20.0 MME or + 2.7 pills), and C-Section (+ 8.8% ≅ +18.1 MME or + 2.4 pills) and were lower for laparoscopic appendectomy/cholecystectomy (-5.6% ≅ -10.5 MME or -1.4 pills). Hispanic patients received lower mean opioid quantities than NHW patients for TKA (-14.5% ≅ -86.9 MME or -11.6 pills), laparoscopic appendectomy/cholecystectomy (-5.0% ≅ -9.7 MME or -1.3 pills), and C-Section (-4.6% ≅ -9.1 MME or -1.2 pills). NHA patients received lower mean opioid quantities relative to NHW patients for TKA (-24.6% ≅ -147.3 MME or -19.6 pills), lumpectomy +/- SLNB (-6.6% ≅ -10.3 MME or -1.4 pills), and laparoscopic appendectomy/cholecystectomy (-10.5% ≅ -20.1 MME or -2.7 pills). Compared to NHW patients, NHO patient received lower mean opioid quantities for laparoscopic appendectomy/cholecystectomy (-4.2% ≅ -8.0 MME or -1.1 pills).
Opioid Prescribing by Race/Ethnicity and Guideline-Procedure Group. Mean percent differences in prescribed total morphine milligram equivalents (MME) versus non-Hispanic white group were derived from statistical models, with adjustment and propensity-score weighting for warranted covariates (see Methods section). Error bars represent 95% confidence intervals. Above or below each bar is the calculated, absolute mean difference in total MME and, in parentheses, the mean difference in 5-mg oxycodone equivalent pills, for each racial and ethnic minority group relative to the NHW group based on unadjusted values for NHW patients. *Indicates statistically significant difference, at alpha of 0.05, in bold text. MIS, minimally invasive surgery; NHA, non-Hispanic Asian; NHB, non-Hispanic Black; NHO, non-Hispanic Other; SLNB, sentinel lymph node biopsy; TKA, total knee arthroplasty
Exploratory outcomes
Guideline-based prescribing
In pooled and unadjusted analyses, 72.8% of all patients received opioid prescriptions at hospital discharge that were above guideline recommendations (Table 3). Statistical models with adjustment for warranted covariates predicted an average excess of 9.0 5-mg oxycodone-equivalent pills prescribed per patient compared to the highest recommended opioid quantity for a given guideline-procedure group. Excess pill quantities were significantly higher among NHB patients (mean of 11.9 pills) and lower among Hispanic patients (mean of 8.5 pills) and NHA patients (mean of 8.7 pills) relative to NHW patients (mean of 9.0 pills). For individual guideline-procedure groups, trends in the relative differences in opioid prescribing by race and ethnicity persisted yet varied in magnitude.
The interaction between race and ethnicity and guideline-concordant prescribing was statistically significant for NHB and Hispanic patients, such that disparities in opioid prescribing were eliminated when opioid prescriptions were written within the range of 5-mg oxycodone pill quantities recommended by clinical guidelines (Supplemental Fig. 3). These interactions were also observed within several guideline-procedure groups (Supplemental Table 3).
Sources of prescribing variation
In pooled analysis of guideline-procedure groups, patterns in racial and ethnic disparities were largely consistent over the five-year study period, with no observable linear trend (Supplemental Fig. 4); however, disparities for NHA patients were not statistically significant in the last observation period between January 2019 and February 2020.
Stepwise models showed that compared to unadjusted estimates, adjusting for warranted covariates alone or in combination with unwarranted covariates could explain much, but not all of the observed differences in opioid prescribing for Hispanic, NHA, and NHO groups versus NHW patients (Model 2 and 3 vs. Model 1; Supplemental Fig. 5). Adjusting for these factors alone did not reduce disparities among NHB patients; however, disparities among NHB patients were mitigated when adjusting for individual providers in combination with warranted covariates alone or in combination with unwarranted covariates (Models 5 and 6 vs. Models 2 and 3; Supplemental Fig. 5). Nevertheless, for all minority patients, except for NHO, disparities in prescribing persisted despite being reduced. Results were similar, although not uniform, within guideline-procedure groups (Supplemental Table 4).
Discussion
In this study, differences in postoperative opioid prescribing at hospital discharge were found among racial and ethnic minority patients relative to NHW patients, overall and for most guideline-procedure groups. Findings among Hispanic and NHA patients are consistent with our hypothesis and a body of literature[21, 25, 31, 43] showing that racial and ethnic minority groups, on average, tend to receive lower opioid prescription quantities than NHW patients overall and for several guideline-procedure groups. Unexpectedly and contrary to our hypothesis, we observed heterogeneity in the direction of disparities for NHB patients. Whereas they received opioid quantities that were, on average, higher than NHW patients overall and for knee arthroscopy, lumpectomy +/- SLNB, and C-sections, they received lower opioid quantities for laparoscopic appendectomy/cholecystectomy. Disparities in prescribing across race and ethnic groups largely persisted over the five-year study period, despite many changes to the culture of opioid prescribing during this time.
To our knowledge, this is the first work that has demonstrated differences in postoperative opioid prescribing within and across service lines by race and ethnicity. While most prior literature has shown lower opioid prescribing quantities among NHB patients relative to NHW patients,[21, 25, 27, 43] our study is consistent with at least one other study by Herb et al. in the postoperative setting.[31] In their study, which focused on postoperative opioid prescribing for general surgeries conducted in late 2018 at a large academic medical center in North Carolina, the authors found that prior to the implementation of standardized opioid prescribing schedules, Black patients received prescriptions that were on average + 18.5 MME higher than white patients. That their study was conducted in a different setting than ours (academic vs. community-based institution) and in a distinct geographic region, supports the need for further investigation into postoperative opioid prescribing for NHB patients.
The opposing direction of observed differences in opioid prescribing among individuals of different racial and ethnic groups (or same racial and ethnic groups receiving different procedures) is a reminder that the mechanisms behind disparities is complex and must be considered within the context of patient, physician, hospital, and other systemic factors.[44, 45] For example, patients may ask for non-opioid alternatives after surgery depending on their receipt of anticipatory guidance, health literacy, or trust in their provider.[46] Implicit or explicit biases may also lead clinicians to prescribe differently to specific groups, related to perceptions about pain tolerance and likelihood for misuse/abuse of prescribed opioids. Bringing attention to such disparities in postoperative opioid prescribing is the first step to making changes.
Differences between racial and ethnic groups in terms of demographic, clinical, and encounter-specific factors explained a large proportion of the disparities in opioid prescribing for Hispanic and NHA patients, and completely for NHO patients, relative to NHW patients. Notably, however, differences in prescribing among NHB patients was most impacted by adjusting for individual opioid-prescribing providers (i.e., provider fixed effects), suggesting that these disparities are in part driven by NHB patients seeing providers with a greater propensity for higher opioid prescribing compared to the other groups.
Despite systematic differences in opioid prescribing by race and ethnicity, excess prescribing was observed across all groups, with approximately 73% of patients receiving prescriptions above guideline recommendations. Such excess prescribing translates to each patient receiving an average of 9 additional 5-mg oxycodone-equivalent pills per prescription. These data indicate that even when a patient belonging to one racial and ethnic group is prescribed a different opioid quantity than another –all else being equal– most patients receive more pills than they are likely to need for pain control. These findings also underscore the limitations of using specific racial and ethnic groups as a benchmark, such that prescriptions of lower opioid quantities versus NHW patients, for example, should not be interpretated as “appropriate” prescribing.
Importantly, racial and ethnic differences for Hispanic and NHB patients versus NHW patients in opioid prescribing were eliminated when prescriptions were written within guideline recommendations. Similar results were found by Herb et al., where the implementation of a standardized postoperative dosing schedule for general surgeries mitigated observed differences between NHB and NHW patients.[31] In their study and ours, this is likely because guidelines offer a narrower range of pill quantities for all patients. While this is unsurprising, it underscores secondary benefits of implementing guideline recommendations; that is, by reducing variation in care, disparities in care can also be mitigated. Whereas it is unclear why these results did not hold for NHA patients, who tended to receive lower opioid quantities than NHWs regardless of whether the prescription was within or above guideline recommendations, there may be other reasons driving specific opioid prescribing practices relative to NHW patients.
From our study, we cannot know why differences in opioid prescribing persisted for racial and ethnic minority groups after adjusting for various factors. It is especially curious that NHB patients appeared to receive higher opioid quantities for several guideline-procedure groups, which is counter to research from other settings, yet consistent with the aforementioned study by Herb and colleagues.[30] Whereas Herb et al. noted that higher opioid prescribing among NHB patients in their study could be attributed to several clinicians with outlier prescribing practices, our data do not support this explanation in terms of the direction and magnitude of observed disparities (see Supplementary Fig. 2).
This study has several limitations. First, because our study design was retrospective and observational, the potential for unmeasured confounding exists. Specifically, while we were able to adjust for numerous factors that could influence opioid prescribing, we did not have comprehensive information on all patients from their primary-care record. For example, this could explain why we were unable to identify diagnoses of mood disorders in our cohort. Postoperative pain may vary based on unmeasured clinical factors (including measures self-reported pain, which are not recorded in the EHR), warranting a higher number of MME/pills. Thus, it is possible that unmeasured comorbid conditions or self-report pain, which could influence opioid prescribing, were more prevalent among NHB patients compared to NHW patients; thus, explaining the observed higher quantity of opioids prescribed. We also did not have information on prescribing provider race and ethnicity, which has been shown to influence opioid prescribing behavior.[47].
Second, we cannot know from this study if differences in opioid prescribing was clinically important or negatively impacted the clinical course of individual patients (it is possible that residual statistically significant differences are not clinically meaningful).
Third, our study was restricted to patients who received an opioid prescription at discharge. We did not study patients who received non-opioid analgesics or no analgesics after surgery because we could not be certain if an opioid was not prescribed, or it was prescribed prior to hospital admission using a medium other than the Sutter EHR.
Fourth, in exploratory analyses we used postoperative opioid prescribing guidelines developed by one institution, the Mayo Clinic. Where guidelines overlapped with other guidelines in terms of surgical procedures, the recommendations were similar, but they were often more restrictive in terms of the range of recommended pill quantities. Of note, the guidelines used in this study were published during the study period. As such, our comparison to guidelines should not be interpreted as a compliance measure; rather, it provided a benchmark for prescribing practices that was independent of race and ethnicity.
Lastly, data from this study are from a community-based healthcare delivery system in Northern California and included select, albeit commonly performed surgical procedures; thus, we cannot know if findings are generalizable to other geographic regions or to other surgical procedures.
Despite limitations, this study has several important strengths. First, we used data from a large, diverse population that is representative of the underlying geographic area. Second, the healthcare system studied is one of the largest in the U.S. and includes multiple hospitals, spanning numerous state counties across rural and urban communities. Third, the lack of postoperative opioid prescribing guidelines in this healthcare system allowed for an examination of natural variation in prescribing behavior. Lastly, our exploratory analyses provide areas of future study that can serve as targets for future public health policy.
In summary, this work is the first to examine disparities in postoperative opioid prescribing by race and ethnicity across service lines, showing broad heterogeneity in the direction and magnitude of such disparities. Given that the majority of opioid prescriptions written in the postoperative setting were above guideline recommendations and that disparities were attenuated for NHB and Hispanic patients when prescriptions were written within guideline recommendations, future policy should focus on encouraging guideline-based postoperative opioid prescribing, dually reducing disparities and mitigating excess pills available in households and communities that have fueled the opioid epidemic.
Data Availability
The datasets analyzed during the current study may be available from the corresponding author on reasonable request.
References
Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for Perioperative Management in the Face of the opioid epidemic. Anesth Analg. 2017;125(5):1733–40.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30.
Carlson RG, Nahhas RW, Martins SS, Daniulaityte R. Predictors of transition to heroin use among initially non-opioid dependent illicit pharmaceutical opioid users: a natural history study. Drug Alcohol Depend. 2016;160:127–34.
Vadivelu N, Kai AM, Kodumudi V, Sramcik J, Kaye AD. The Opioid Crisis: a comprehensive overview. Curr Pain Headache Rep. 2018;22(3):16.
Baldini A, Von Korff M, Lin EH. A Review of Potential Adverse Effects of Long-Term Opioid Therapy: A Practitioner’s Guide. Prim Care Companion CNS Disord. 2012;14(3).
Schirle L, Stone AL, Morris MC, Osmundson SS, Walker PD, Dietrich MS, et al. Leftover opioids following adult surgical procedures: a systematic review and meta-analysis. Syst Reviews. 2020;9(1):139.
Tan WH, Yu J, Freaman S, McAllister JM, Kahan LG, Quasebarth MA, et al. Opioid medication use in the Surgical patient: an Assessment of prescribing patterns and use. J Am Coll Surg. 2018;227(2):203–11.
Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066–71.
Michigan Opiod Prescribing and Engagement Network (OPEN). Prescribing recommendations 2020 [Available from: https://opioidprescribing.info.
Overton HN, Hanna MN, Bruhn WE, Hutfless S, Bicket MC, Makary MA, et al. Opioid-prescribing guidelines for Common Surgical Procedures: an Expert Panel Consensus. J Am Coll Surg. 2018;227(4):411–8.
Glaser GE, Kalogera E, Kumar A, Yi J, Destephano C, Ubl D, et al. Outcomes and patient perspectives following implementation of tiered opioid prescription guidelines in gynecologic surgery. Gynecol Oncol. 2020;157(2):476–81.
Wyles CC, Hevesi M, Trousdale ER, Ubl DS, Gazelka HM, Habermann EB, et al. The 2018 Chitranjan S. Ranawat, MD Award: developing and implementing a Novel Institutional Guideline Strategy reduced postoperative opioid prescribing after TKA and THA. Clin Orthop Relat Res. 2019;477(1):104–13.
Thiels CA, Ubl DS, Yost KJ, Dowdy SC, Mabry TM, Gazelka HM, et al. Results of a prospective, Multicenter Initiative aimed at developing opioid-prescribing guidelines after surgery. Ann Surg. 2018;268(3):457–68.
National Academies of Sciences, Engineering, and Medicine. Framing opioid prescribing guidelines for acute pain: developing the evidence. Washington, DC: The National Academies Press; 2020. pp. 85–129.
Shiels MS, Berrington de González A, Best AF, Chen Y, Chernyavskiy P, Hartge P, et al. Premature mortality from all causes and drug poisonings in the USA according to socioeconomic status and rurality: an analysis of death certificate data by county from 2000–15. The Lancet Public Health. 2019;4(2):e97–e106.
Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. The Lancet. 2017;389(10073):1043–54.
Kaiser Family Foundation. Opioid overdose deaths by race/ethnicity, 2019 [updated 2021. Available from: https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-raceethnicity/.
Song Z. Mortality quadrupled among opioid-driven hospitalizations, notably within lower-income and disabled white populations. Health Aff. 2017;36(12):2054–61.
Santoro TN, Santoro JD. Racial Bias in the US opioid epidemic: a review of the history of systemic Bias and Implications for Care. Cureus. 2018;10(12):e3733–e.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences. 2016;113(16):4296 – 301.
Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10(12):1187–204.
Burgess DJ, Crowley-Matoka M, Phelan S, Dovidio JF, Kerns R, Roth C, et al. Patient race and physicians’ decisions to prescribe opioids for chronic low back pain. Soc Sci Med. 2008;67(11):1852–60.
Singhal A, Tien Y-Y, Hsia RY. Racial-ethnic disparities in opioid prescriptions at Emergency Department visits for conditions commonly Associated with prescription drug abuse. PLoS ONE. 2016;11(8):e0159224.
Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11–6.
Badreldin N, Grobman WA, Yee LM. Racial disparities in Postpartum Pain Management. Obstet Gynecol. 2019;134(6):1147–53.
Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in Emergency Department analgesic prescription. Am J Public Health. 2003;93(12):2067–73.
Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in Opioid Prescribing by Race/Ethnicity for patients seeking care in US Emergency Departments. JAMA. 2008;299(1):70–8.
Romanelli RJ, Shen Z, Szwerinski N, Scott A, Lockhart S, Pressman AR. Racial and ethnic disparities in opioid prescribing for long bone fractures at Discharge from the Emergency Department: a cross-sectional analysis of 22 Centers from a Health Care Delivery System in Northern California. Ann Emerg Med. 2019;74(5):622–31.
Ng B, Dimsdale JE, Rollnik JD, Shapiro H. The effect of ethnicity on prescriptions for patient-controlled analgesia for post-operative pain. Pain. 1996;66(1):9–12.
Lazar DJ, Zaveri S, Khetan P, Nobel TB, Divino CM. Variations in postoperative opioid prescribing by day of week and duration of hospital stay. Surgery. 2020.
Herb JN, Williams BM, Chen KA, Young JC, Chidgey BA, McNaull PP et al. The impact of standard postoperative opioid prescribing guidelines on racial differences in opioid prescribing: A retrospective review. Surgery. 2021.
McDonald DD. Gender and ethnic stereotyping and narcotic analgesic administration. Res Nurs Health. 1994;17(1):45–9.
Ladha KS, Neuman MD, Broms G, Bethell J, Bateman BT, Wijeysundera DN, et al. Opioid prescribing after surgery in the United States, Canada, and Sweden. JAMA Netw Open. 2019;2(9):e1910734.
Pfunter AWLM, Stocks C. Statistical Brief #149 Most Frequent Procedures Performed in U.S. Hospital, 2010. 2013. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK132428/#!po=25.0000.
U.S. Department of Health and Human Services. Calculating Total Daily Dose of Opioids for Safer Dosage. Atlanta, GA:Centers for Disease Control and Prevention.
United States Census Bureau. About Race 2020 [updated October 16., 2020. Available from: https://www.census.gov/topics/population/race/about.html.
Committee on Economics. ASA Physical Status Classification System Schaumburg, IL: American Society of Anesthesiologists. ; 2014 [updated December 13, 2020. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.
Coleman C, Lennon RP, Robinson JM, Tuan WJ, Sehgal N, Zgierska AE. Provider and patient sex disparities in opioid prescribing and patient outcomes. J Opioid Manag. 2022;18(5):435–45.
Poole MA, O’Farrell PN. The assumptions of the linear regression model. Trans Inst Br Geogr. 1971:145–58.
Benoit K. Linear regression models with logarithmic transformations. Lond School Econ Lond. 2011;22(1):23–36.
McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for evaluating Causal Effects in Observational Studies. Psychol Methods. 2004;9(4):403–25.
Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005;61(4):962–73.
Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4(3):277–94.
Haider AH, Scott VK, Rehman KA, Velopulos C, Bentley JM, Cornwell EE, et al. Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg. 2013;216(3):482–92. e12.
Torain MJ, Maragh-Bass AC, Dankwa-Mullen I, Hisam B, Kodadek LM, Lilley EJ, et al. Surgical disparities: a comprehensive review and new conceptual framework. J Am Coll Surg. 2016;223(2):408–18.
Vallerand AH, Hasenau S, Templin T, Collins-Bohler D. Disparities between Black and White Patients with Cancer Pain: the Effect of Perception of Control over Pain. Pain Med. 2005;6(3):242–50.
Badreldin N, DiTosto JD, Grobman WA, Yee LM. Association between patient-prescriber racial and ethnic concordance and Postpartum Pain and Opioid Prescribing. Health Equity. 2022;6(1):198–205.
Acknowledgements
None.
Funding
This work was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R01DA046226.
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Contributions
RJR conceived the study, analyzed and interpreted the data, drafted the manuscript. RS interpreted data and edited the manuscript. MCM interpreted the data, drafted and edited the manuscript; SM procured the data and edited the manuscript; LTM interpreted findings and edited the manuscript; ZW interpreted findings and edited the manuscript; KAZ interpreted findings and edited the manuscript; AK interpreted data and edited the manuscript; KEW interpreted the data and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. This study was approved by the Sutter Health Institutional Review Board.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.





Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Romanelli, R.J., Shenoy, R., Martinez, M.C. et al. Disparities in postoperative opioid prescribing by race and ethnicity: an electronic health records-based observational study from Northern California, 2015–2020. Arch Public Health 81, 83 (2023). https://doi.org/10.1186/s13690-023-01095-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-023-01095-2