Abstract
Background
Anemia among children aged 6–23 months is a major public health problem worldwide specifically in sub-Saharan Africa (SSA). Anemia during the childhood period causes significant short-and long-term health consequences. However, there is a paucity of evidence on Anemia among children aged 6–23 months in SSA. Therefore, this study examined the individual- and community-level factors associated with anemia among children aged 6–23 months in sub-Saharan Africa.
Methods
A secondary data analysis was done based on the most recent Demographic and Health Survey (DHS) of 32 sub-Saharan African countries. A total weighted sample of 51,044 children aged 6–23 months was included for analysis. We have used a multilevel proportional odds model to identify predictors of severity levels of anemia. Variables with p < 0.2 in the bivariable analysis were considered for the multivariable analysis. In the multivariable multilevel proportional odds model, the Adjusted Odds Ratio (AOR) with the 95% Confidence Interval (CI) was reported to declare the statistical significance and strength of the association.
Results
In this study, about 76.6% (95% CI: 76.2%, 76.9%) of children aged 6–23 months in sub-Saharan Africa were anemic. In the multivariable multilevel proportional odds model, being female, being aged 18–23 months, higher level of maternal education, being larger size at birth, belonging to a wealthier household, getting four ANC visits and above, advanced maternal age, and belonging to a community with high maternal education were significantly associated with lower odds of higher levels of anemia. On the other hand, being twin birth, being smaller size at birth, being of a higher order of birth, having fever in the last two weeks, and distance to a health facility were significantly associated with higher odds of higher levels of anemia.
Conclusion
The study found that more than three-fourths of children aged 6–23 months in sub-Saharan Africa were anemic. This finding proved that the severity levels of anemia among children in sub-Saharan Africa remain a serious public health concern. Therefore, to curve this problem enhancing maternal education, promoting maternal health service utilization, and improving health care access is crucial. In addition, health care providers better give special emphasis to twin births, higher-order birth, and those belonging to poor households to reduce the incidence of anemia among children aged 6–23 months in SSA.
Similar content being viewed by others
Background
Globally, micronutrient deficiencies are the most prevalent nutritional problem among children [1, 2]. Anemia among children is the commonest micronutrient deficiency especially in sub-Saharan African countries [3]. According to the World Health Organization (WHO), anemia among children is defined as a hemoglobin value less than 11 g/dl [4]. Anemia affects all age groups but under two years children are the most vulnerable segment of the community [5, 6]. In the first two years of life, the child has rapid mental development and physical growth which demands the highest nutritional supply [7]. As of 2019, an estimated 269 million children suffered from anemia with nearly two-thirds in Asia and Africa [8, 9]. The highest prevalence of anemia among children was observed in sub-Saharan Africa (46%—66%) [3, 10, 11].
Anemia during childhood has short-and long-term consequences on physical growth, mental development, and productivity [12,13,14]. It causes mental retardation [15], poor physical performance [16], and poor motor development and control [17]. In the long term, it leads to reduced academic achievement [18,19,20]. The causes of anemia can be nutritional, medical, or genetic [21]. Nevertheless, nutritional deficiency is the commonest cause of anemia specifically iron deficiency [22]. Apart from ID, other micronutrient deficiencies (folic acid, zinc, and vitamin B12) [23], parasitic infections (hookworm, schistosomiasis, ascariasis, and malaria) [24], and blood disorders (sickle cell anemia and thalassemia) [25] can cause anemia.
Previous studies revealed that residence [26], mothers age [27], mothers educational status [28], child age [29], child sex [30], child twin status [31], number of Antenatal Care (ANC) visits [32, 33], place of delivery [34], birth weight [35], media exposure [11], distance to health facility [36], household wealth status [37, 38], birth order [39], maternal anemia [40], infectious diseases (malaria, tuberculosis, and hookworm) [41], and child nutritional status (stunting, wasting and underweight) [42] were significant factors associated with anemia.
Studies have proven that anemia among children aged 6–23 months is a serious public health problem in SSA. However, there is a paucity of evidence on the prevalence, severity level, and predictors of anemia among children aged 6–23 months in SSA. In addition, even though anemia has ordinal nature (not anemic, mild, moderate, or severe), previous studies treat anemia as a binary outcome (anemic vs non-anemic). Therefore, treating anemia as binary could result in loss of information and is not informative for decision-makers as well as public health programmers. Therefore, this study examined the individual-and community-level factors associated with anemia among children aged 6–23 months in SSA using a multilevel ordinal logistic regression model.
Methods
Data source and sampling procedure
This study was based on the most recent Demographic and Health Survey (DHS) of 32 sub-Saharan African countries. DHS is conducted every five years to generate updated health and health-related indicators. A two-stage stratified sampling technique was employed to select the study subjects. In the first stage, Enumeration Areas (EAs) were randomly selected while in the second stage households were selected.
To assess the anemia status of children, hemoglobin testing was carried out among children in the selected households using HemoCue rapid testing methodology. For the test, a drop of capillary blood was taken from a child's fingertip or heel and was drawn into the micro cuvette which was then analyzed using the photometer that displays the hemoglobin concentration. There are different datasets in DHS and for this study, we used the Kids Record (KR) file. We extracted the data from the KR dataset based on literature and then appended using the STATA command “append using”. The final sample size for this study was 51,044 children aged 6–23 months.
Study variables and measurements
Dependent variable
Our outcome variable of interest was severity levels of anemia among children aged 6–23 months, which we grouped into four ordinal categories; mildly anemic (hemoglobin level 10.0–10.9 g/dl, moderately anemic (hemoglobin level 7.0–9.9 g/dl), severely anemic (hemoglobin level < 7.0 g/dl), and not anemic (hemoglobin ≥ 11.0 g/dl). It was assessed based on the hemoglobin concentration in blood adjusted to the altitude. At elevations above 1000 m, hemoglobin concentrations increase as an adaptive response to the lower partial pressure of oxygen and reduced oxygen saturation of the blood. The compensatory increase in red cell production ensures that sufficient oxygen is supplied to tissues.
Independent variables
The independent variables were considered from two sources; individual-and community-level variables. Child age, child sex, household wealth status, maternal education, maternal age, sex of household head, child twin status, child nutrition status, birth order, media exposure, number of ANC visits, place of delivery, fever in the last two weeks, husband education, had diarrhea in the last two weeks, birth size, and preceding birth interval were individual-level variables. Residence, sub-Saharan African region, distance to the health facility, community poverty, and community maternal education were community-level variables.
Media exposure was calculated by aggregating three variables such as watching television, listening to the radio, and reading newspapers. Then categorized as having media exposure if a mother has been exposed to at least one of the three and not if she had no exposure to any of the media sources. These two community-level variables (community maternal education and community poverty) were generated by aggregating maternal education and household wealth status at the cluster/enumeration area levels. Then categorized as higher community maternal education and poverty based on the national median value of the proportion of maternal education and poverty since they were not normally distributed.
Data management and analysis
STATA version 17 statistical software was used for the data management and analysis. anemia was polychotomous and has ordinal nature. Therefore, an ordinal logistic regression model was considered to analyze factors associated with severity levels of anemia (no anemia, mild, moderate, and severe anemia). There are different ordinal logistic regression models such as Proportional Odds Model (POM), Partial Proportional Odds Model with Restrictions (PPOMR), Partial Proportional Odds Model without Restrictions (PPOMWR), Continuous Ratio Model (CRM), and Stereotype Model (SM). In epidemiological studies, Proportional Odds Model (Cumulative Logit Model) is the most commonly used ordinal logistic regression model. The fundamental assumption in an ordinal logistic regression model is the Proportional Odds (PO) assumption. If the data satisfies the PO assumption, the proportional odds model can be used, if not the partial proportional model should be used. To choose the appropriate ordinal model for the data, we have checked the PO assumptions, which state that the effects of all independent variables are constant across categories of the outcome variable. The Brant test revealed that the PO assumption was fulfilled (p > 0.05). Besides, the DHS data has a hierarchical nature. Therefore, children and mothers were nested within a cluster, and we assume that study subjects in the same cluster may share similar characteristics to participants in another cluster. This implies the need to take into account the heterogeneity between clusters by using an advanced model. Therefore, a multilevel proportional odds model was performed.
As a result, because the Brant test was met, the multilevel proportional odds model gave a single Odds Ratio (OR) for an explanatory variable (severe vs moderate/mild/non-anemia, severe/moderate vs mild/non-anemia, and severe/moderate/mild vs non-anemic. The Brant test stated that the effects of all the independent variables are constant across categories of severity levels of anemia (global test; p > 0.05). In addition to the global test, we assessed each variable in the model to identify the variables for which the PO assumption was fulfilled and all the variables had a p-value > 0.05. Likelihood Ratio (LR) test, Variance Partition Coefficient (VPC), and Median Odds Ratio (MOR) were computed to measure the variation of anemia across clusters. The VPC quantifies the degree of heterogeneity of anemia between clusters (the proportion of the total observed variation in anemia that is attributable to cluster variations) [43].
Where: the standard logit distribution has a variance of \({\uppi }^2/3\), \({{\sigma }_{\mu }}^{2}\) indicates the cluster variance.
The MOR quantifies the variation or heterogeneity in anemia between clusters in terms of the odds ratio scale and is defined as the median value of the odds ratio between the cluster with a high likelihood of anemia and the cluster at lower risk when randomly picking out individuals from two clusters (EAs) [44].
Four models were constructed for the multilevel logistic regression analysis. The first model was a null model without explanatory variables to determine the extent of cluster variation in childhood anemia. The second model was adjusted with individual-level variables; the third model was adjusted for community-level variables while the fourth was fitted with both individual and community-level variables simultaneously. Model comparison was made based on deviance (-2Log-Likelihood Ratio (LLR)) since the models were nested models, and a model with the lowest deviance was the best-fitted model for the data.
In the null model, about 7.4% of the total variation in anemia was due to unobserved community-level factors (VPC = 7.4%). This result was not suggestive of using a multilevel ordinal model rather than a single-level model. Then, we have further examined whether the multilevel ordinal logistic regression model was significant over the single-level ordinal logistic regression model using the LR test as VPC is descriptive and we don’t rely on its value as it is not directly estimated, unlike continuous outcome variables. The LR test was statistically significant (p < 0.05), indicating that the multilevel ordinal logistic regression model was best fitted to the single-level ordinal logistic regression analysis. In addition, MOR revealed that if we randomly select two children aged 6–23 months from different clusters and transfer children aged 6–23 months from the cluster with a lower likelihood of higher levels of anemia to a cluster with a higher likelihood of higher levels of anemia, could have 1.32 times higher levels of anemia. Therefore, the LR-test and MOR are suggestive of using a multilevel ordinal logistic regression model. Four models were fitted and the final model was chosen since it has the lowest deviance value.
Variables with a p-value ≤ 0.2 in the bi-variable multilevel proportional odds model were considered for the multivariable multilevel proportional odds model. In the multivariable multilevel proportional odds model, the Adjusted Odds Ratio (AOR) with 95% Confidence Interval (CI) was reported to declare the strength of association, and the statistical significance for the final model was set at p < 0.05.
Ethical consideration
This study was based on publicly accessible survey data from the MEASURE DHS program, and no need for ethical approval and participant consent. We have granted permission from http:/www.dhsprogram.com to download and use the data for this study. In the datasets, there are no names of persons or household addresses recorded.
Results
Individual-level characteristics of study participants
A total of 51,044 children aged 6–23 months were included. Of them, about 25,664 (50.3%) were males. More than half (52.5%) of mothers were aged 20–29 years and about 36.6% of mothers didn’t attend formal education. About 27.3% and 25.4% of the children had symptoms of fever and diarrhea within two weeks, respectively. About 53.5% of the mothers had four ANC visits and above during pregnancy, and the vast majority (70.5%) of the children were born at the health facility (Table 1).
Community-level characteristics of the study participants
The majority of the children were from West Africa (39.9%) followed by East Africa (38.6%). More than two-thirds (69.0%) of respondents were living in rural areas. Regarding community maternal education and poverty, about 27,580 (54.0%) and 3,639 (7.1%) of the respondents were from the community with high maternal education and high poverty, respectively (Table 2).
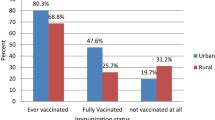
Prevalence of anemia among children aged 6–23 months in SSA
The prevalence of anemia among children aged 6–23 months in SSA was 76.6% (95% CI: 76.2%, 76.9%). The prevalence varied from 64.5% in Southern Africa to 84.3% in West Africa. Based on severity levels of anemia, the prevalence of mild, moderate and severe anemia among children aged 6–23 months in SSA were 26.9% (95% CI: 26.5%, 27.3%), 45.5% (95% CI: 45.0%, 45.9%) and 4.2% (95% CI: 4.1%, 4.4%), respectively (Fig. 1).
Multivariable multilevel proportional odds model analysis results
Individual and community-level factors associated with anemia
Sex of child, child age, maternal education, larger size at birth, household wealth status, number of ANC visits, maternal age, being in southern Africa, and higher community maternal education was significantly associated with lower risk of higher levels of anemia. In contrast, twin status, smaller size at birth, birth order, health facility delivery, and being born in Central and West Africa were significantly associated with higher risks of higher levels of anemia.
The odds of having higher levels of anemia among female children decreased by 22% (AOR = 0.78, 95% CI: 0.76, 0.81) compared to male children. The odds of having higher levels of anemia were decreased by 27% (AOR = 0.73, 95% CI: 0.70, 0.76) for children aged 18–23 months compared to children aged 6–11 months. The odds of having higher levels of anemia among children of mothers who attained a primary, secondary and higher level of education were decreased by 20% (AOR = 0.80, 95% CI: 0.77, 0.84), 30% (AOR = 0.70, 95% CI: 0.66, 0.74) and 51% (AOR = 0.49, 95% CI: 0.43, 0.55) compared to children of mothers who didn’t have formal education, respectively.
Children who were smaller size at birth were 1.16 times (AOR = 1.16, 95% CI: 1.11, 1.21) times higher odds of having higher levels of anemia compared to those of average size at birth. On the other hand, the odds of having higher levels of anemia among children with a larger size at birth were decreased by 9% (AOR = 0.91, 95% CI: 0.88, 0.95) than those average size at birth. Being sixth birth order or above had 1.12 times (AOR = 1.12, 95% CI: 1.04, 1.20) higher odds of higher levels of anemia compared to first order birth. The odds of having higher levels of anemia among children belonged to the middle, richer, and richest household wealth were decreased by 9% (AOR = 0.89, 95% CI: 0.87, 0.96), 9% (AOR = 0.91, 95% CI: 0.86, 0.96) and 22% (AOR = 0.78, 95% CI: 0.73, 0.84) compared to children belonging to the poorest household wealth, respectively.
Children who had a fever in the last two weeks had 1.40 times (AOR = 1.40, 95% CI: 1.35, 1.45) higher odds of higher levels of anemia compared to those who didn’t have a fever. The odds of having higher levels of anemia among children born to mothers aged 20–29, 30–39 and 40–49 years were decreased by 14% (AOR = 0.86, 95% CI: 0.80, 0.91), 27% (AOR = 0.73, 95% CI: 0.68, 0.79) and 36% (AOR = 0.64, 95% CI: 0.58, 0.71) compared to children born to mothers aged 15–19 years, respectively. The odds of having higher levels of anemia among children born to mothers who had four and above ANC visits were decreased by 9% (AOR = 0.91, 95% CI: 0.86, 0.96) compared to children born to children whose mothers didn’t have ANC visits during pregnancy.
Children born to mothers who reported distance to a health facility as a big problem had 1.06 times (AOR = 1.06, 95% CI: 1.03, 1.10) higher odds of higher levels of anemia compared to their counterparts. Children in Central Africa and West Africa had 1.17 times (AOR = 1.17, 95% CI: 1.12, 1.23) and 2.09 times (AOR = 2.09, 95% CI: 2.01, 2.18) higher odds of higher levels of anemia than those in East Africa whereas children in Southern Africa had decreased odds of higher levels of anemia (AOR = 0.89, 95% CI: 0.82, 0.97) than children in East Africa. The odds of having higher levels of anemia among children in the community with higher maternal education were decreased by 8% (AOR = 0.92, 95% CI: 0.86, 0.99) compared to children in the community with low maternal education (Table 3).
Discussion
The prevalence of anemia among children aged 6–23 months in SSA was 76.6% (95% CI: 76.2%, 76.9%) which varied across regions, indicating anemia is a serious public health problem in SSA [45]. This was higher than in previous studies [46,47,48,49,50], this might be due to the long-standing undernutrition among children due to long-standing poverty in SSA [51]. Moreover, poor socioeconomic conditions in African countries make children more susceptible to infectious diseases, which in turn compromises the absorption, and utilization of nutrients like vitamin B9, B12, and iron [52, 53].
Child sex, child age, maternal educational status, child size at birth, household wealth status, number of ANC visits, maternal age, having fever in the last two weeks, sub-Saharan African region, community maternal education, child twin status, birth order and distance to health facility were significantly associated with the severity levels of anemia. In line with this study [10, 54, 55], previous studies revealed that female children were at lower odds of having higher levels of anemia compared to male children. The possible justification might be due to too early initiation of complementary feeding for male children and the community’s belief to give better care to male children than females, this could expose them to different infectious diseases and malabsorption problems [56, 57]. In addition, male children in the first two years of life are at a state of rapid growth which increases their micronutrient demands including vitamin B9, B12, and iron compared to female children [58, 59].
Twin children were at higher odds of having higher levels of anemia compared to singletons. This is supported by a study reported in India [60], this might be due to twin births being prone to prematurity, low birth weight, and undernutrition than singletons, in turn, they are at higher risk of anemia [61, 62]. Children aged 18–23 months had lower odds of higher levels of anemia compared to children aged 6–11 months. This is in line with previous studies reported in developing countries [54, 63], this is because prenatal iron store depletion is pronounced at six months of birth and made them at higher risk of anemia [64].
As the level of maternal education increased, the odds of higher levels of anemia decreased. It is consistent with studies reported in Korea [63], Indonesia [65], and Mexico [66]. This might be because children of mothers who had formal education are more likely to have healthy child-feeding practices [67, 68]. In addition, a mother with a higher level of education has better nutrition and utilizes health services [69, 70]. Many studies have reported maternal anemia as the commonest risk factor for anemia among children [40, 71]. Being small size at birth was significantly associated with increased odds of higher levels of anemia while large size at birth was significantly associated with lower odds of higher levels of anemia. These were in agreement with studies reported in India [72] and Pakistan [73], this could be due to small size at birth being associated with maternal anemia [74], which in turn children born to anemic mothers may not have enough iron storage [40, 75].
Children from households with middle, richer, and richest wealth quantile had decreased odds of having higher levels of anemia compared to those from a household with the poorest wealth quintile. This is consistent with study findings in SSA [39], Sri Lanka [76], and Bangladesh [77], this could be because children in the wealthiest household are capable of providing a balanced diet rich in macro and micronutrients including minerals and vitamins to their child [78, 79]. In addition, children from rich households have more chance of health care access for common illness which causes childhood anemia [80]. The odds of having higher levels of anemia among children born to mothers who had four and above ANC visits during pregnancy were lower than those born to mothers who didn’t have ANC visits. This might be due to pregnant mothers may have the benefit of iron-folate supplementation as well as prompt diagnosis and treatment of diseases such as malaria, visceral leishmaniasis, and hookworm which are identified as the leading causes of anemia, which in turn reduces the risk of child anemia [81, 82].
Children of mothers aged 20–29, 30–39, and 40–49 years had lower odds of higher levels of anemia compared to children of a mother aged 15–19 years. This was in agreement with study findings in Haiti [29], Brazil [83], and India [84], this might be due to mothers aged 20 years and above are physiologically mature and are at lower risk of having low birth weight babies compared to young women [85, 86]. Higher birth order was significantly associated with increased odds of having higher levels of anemia compared to first-order birth. This was in concordance with study findings in SSA [39], India [87, 88], this is because higher birth order is related to extensive maternal nutrition depletion including iron, folate, and vitamin B12 and this could increase the risk of childhood anemia [89, 90]. In addition, a large number of children are associated with increased socio-economic and health problems due to competition for food, infections, and cross contaminations.
Children who had a fever in the last two weeks had higher odds of higher levels of anemia compared to their counterparts. This is consistent with different studies reported elsewhere [11, 91, 92], this is could be due to fever is commonly manifested due to malaria and other common infectious diseases in a situation where both anemia and fever coexist [93, 94]. In agreement with previous studies [40, 95], the odds of having higher levels of anemia among children of mothers perceiving distance to a health facility as a big problem were higher than their counterparts. This might be due to the big distance to the nearby health facility being linked to poor health service utilization for basic services. To mention a few, malaria and hookworm infections are common in children aged 6–23 months in almost all African countries, and if they are not timely and effectively treated, they could result in a severe form of anemia.
Strengths and limitations of the study
Our study findings should be interpreted within the context of the following limitation. We are unable to draw cause-effect relationships because of the cross-sectional nature of DHS data. In addition, in this study, only children surviving during the data collection were included and deaths that could have resulted from complications due to anemia were missed (survivor bias). Moreover, we were not considered important predictors such as malaria infection, visceral leishmaniasis, hookworm, and congenital infections, because these variables were not available in DHS. Despite the abovementioned limitations, this study has the following strengths. This study was based on a pooled nationally representative DHS survey of the 32 sub-Saharan African countries. In addition, the data was weighted and a multilevel ordinal logistic regression analysis was done to get a reliable estimate and standard error. Besides, this study was based on a large sample size that had adequate power to detect the true effect of the independent variables.
Conclusion
Anemia among children aged 6–23 months in sub-Saharan Africa was a serious public health problem. Both individual and community level variables were found significant predictors of severity levels of anemia among children aged 6–23 months. Child age, child sex, size at birth, maternal education, maternal age, fever in the last two weeks, birth order, twin status, and household wealth status were among individual-level predictors of severity levels of anemia among children aged 6–23 months. Among community-level variables, sub-Saharan African regions, distance to health facilities, and community maternal education were found significant predictors of severity levels of anemia. Improving maternal education, providing treatment for febrile illness, and strengthening the economic status of the family are recommended to reduce anemia among children aged 6–23 months. In addition, to cater anemia fortification or supplementation with iron and micronutrients could contribute for the better reduction in the risk of anemia and improvements in hemoglobin levels among children.
Availability of data and materials
Data is available online and you can access it from www.measuredhs.com.
Abbreviations
- AIC:
-
Akaike Information Criteria
- AOR:
-
Adjusted Odds Ratio
- BIC:
-
Bayesian Information Criteria
- CI:
-
Confidence Interval
- DHS:
-
Demographic health survey
- EAs:
-
Enumeration areas
- ID:
-
Iron Deficiency
- HAZ:
-
Z-score for Height-for-Age
- IUGR:
-
Intra uterine growth restriction
- LLR:
-
Log likelihood ratio
- LR:
-
Likelihood ratio
- POM:
-
Proportional Odds Model
- PPOM:
-
Partial Proportional Odds Model
- SDG:
-
Sustainable Development Goal
- SSA:
-
Sub-Saharan Africa;
- WAZ:
-
Z-score for Weight-for-Age
- WHO:
-
World Health Organizations
- WHZ:
-
Z-score for Weight-for-Height
References
Tulchinsky TH. Micronutrient deficiency conditions: global health issues. Public Health Rev. 2010;32(1):243–55.
Ritchie H, Roser M. Micronutrient deficiency. Our World in data; 2017.
Lemoine A, Tounian P. Childhood anemia and iron deficiency in sub-Saharan Africa–risk factors and prevention: a review. Arch Pediatr. 2020;27(8):490–6.
Patel KV. Epidemiology of anemia in older adults. In: Seminars in hematology. Elsevier; 2008.
Joo EY, et al. Iron deficiency anemia in infants and toddlers. Blood research. 2016;51(4):268–73.
Lozoff B, Kaciroti N, Walter T. Iron deficiency in infancy: applying a physiologic framework for prediction. Am J Clin Nutr. 2006;84(6):1412–21.
Martorell R. Improved nutrition in the first 1000 days and adult human capital and health. Am J Hum Biol. 2017;29(2):e22952.
Stevens GA, et al. National, regional, and global estimates of anaemia by severity in women and children for 2000–19: a pooled analysis of population-representative data. Lancet Glob Health. 2022;10(5):e627–39.
Balarajan Y, et al. Anaemia in low-income and middle-income countries. Lancet. 2011;378(9809):2123–35.
Moschovis PP, et al. Individual, maternal and household risk factors for anaemia among young children in sub-Saharan Africa: a cross-sectional study. BMJ Open. 2018;8(5):e019654.
Tesema GA, et al. Prevalence and determinants of severity levels of anemia among children aged 6–59 months in sub-Saharan Africa: a multilevel ordinal logistic regression analysis. PLoS One. 2021;16(4):e0249978.
Lozoff B, et al. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr Rev. 2006;64(suppl_2):S34–43.
Booth I, Aukett M. Iron deficiency anaemia in infancy and early childhood. Arch Dis Child. 1997;76(6):549–54.
Levy A, et al. Anemia as a risk factor for infectious diseases in infants and toddlers: results from a prospective study. Eur J Epidemiol. 2005;20(3):277–84.
Pollitt E. Early iron deficiency anemia and later mental retardation. Oxford University Press; 1999. p. 4–5.
Woodman R, Ferrucci L, Guralnik J. Anemia in older adults. Curr Opin Hematol. 2005;12(2):123–8.
DeRossi SS, Raghavendra S. Anemia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(2):131–41.
Taras H. Nutrition and student performance at school. J Sch Health. 2005;75(6):199–213.
Karande S, Kulkarni M. Poor school performance. Indian J Pediatr. 2005;72(11):961–7.
Soemantri A, Pollitt E, Kim I. Iron deficiency anemia and educational achievement. Am J Clin Nutr. 1985;42(6):1221–8.
Zimmermann MB, Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370(9586):511–20.
Cook JD, et al. Nutritional deficiency and anemia in Latin America: a collaborative study. Blood. 1971;38(5):591–603.
Green R, Miller JW. Folate deficiency beyond megaloblastic anemia: hyperhomocysteinemia and other manifestations of dysfunctional folate status. In: Seminars in hematology. Sheboygan: Grune & Stratton,[c1964-; 1999.
Chaparro CM, Suchdev PS. Anemia epidemiology, pathophysiology, and etiology in low-and middle-income countries. Ann N Y Acad Sci. 2019;1450(1):15–31.
Jamwal M, Sharma P, Das R. Laboratory approach to hemolytic anemia. Indian J Pediatr. 2020;87(1):66–74.
Dey S, Raheem E. Multilevel multinomial logistic regression model for identifying factors associated with anemia in children 6–59 months in northeastern states of India. Cogent Mathematics. 2016;3(1):1159798.
Finlay JE, Özaltin E, Canning D. The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: evidence from 55 low-and middle-income countries. BMJ Open. 2011;1(2):e000226.
Choi H-J, et al. Effects of maternal education on diet, anemia, and iron deficiency in Korean school-aged children. BMC Public Health. 2011;11(1):1–8.
Ayoya MA, et al. Prevalence and risk factors of anemia among children 6–59 months old in Haiti. Anemia. 2013;2013:502968.
Gebreegziabiher G, Etana B, Niggusie D. Determinants of anemia among children aged 6–59 months living in Kilte Awulaelo Woreda Northern Ethiopia. Anemia. 2014;2014:245870.
Li SJ, et al. Increased risk of birth defects among children from multiple births. Birth Defects Res A. 2003;67(10):879–85.
Charles AM, et al. Predictors of anemia among pregnant women in Westmoreland Jamaica. Health Care Women Int. 2010;31(7):585–98.
Sharma H, Singh S, Srivastava S. Socio-economic inequality and spatial heterogeneity in anaemia among children in India: evidence from NFHS-4 (2015–16). Clin Epidemiol Global Health. 2020;8(4):1158–71.
Wilunda C, et al. Prenatal anemia control and anemia in children aged 6–23 months in sub-Saharan Africa. Matern Child Nutr. 2017;13(3):e12375.
Kejo D, et al. Prevalence and predictors of anemia among children under 5 years of age in Arusha District, Tanzania. Pediatr Health Med Ther. 2018;9:9.
Woodruff BA, et al. Determinants of stunting, wasting, and anemia in Guinean preschool-age children: an analysis of DHS data from 1999, 2005, and 2012. Food Nutr Bull. 2018;39(1):39–53.
Prieto-Patron A, et al. Association between anaemia in children 6 to 23 months old and child, mother, household and feeding indicators. Nutrients. 2018;10(9):1269.
Nambiema A, Robert A, Yaya I. Prevalence and risk factors of anemia in children aged from 6 to 59 months in Togo: analysis from Togo demographic and health survey data, 2013–2014. BMC Public Health. 2019;19(1):1–9.
Obasohan PE, et al. A scoping review of the risk factors associated with anaemia among children under five years in sub-Saharan African countries. Int J Environ Res Public Health. 2020;17(23):8829.
Ntenda PA, et al. Maternal anemia is a potential risk factor for anemia in children aged 6–59 months in Southern Africa: a multilevel analysis. BMC Public Health. 2018;18(1):1–13.
Ekvall H. Malaria and anemia. Curr Opin Hematol. 2003;10(2):108–14.
Caulfield LE, et al. Stunting, wasting, and micronutrient deficiency disorders. In: Disease control priorities in developing countries. 2nd ed. 2006.
Rodriguez G, Elo I. Intra-class correlation in random-effects models for binary data. Stand Genomic Sci. 2003;3(1):32–46.
Merlo J, et al. Individual and collective bodies: using measures of variance and association in contextual epidemiology. J Epidemiol Community Health. 2009;63(12):1043–8.
Lopez JH. Pro-poor growth: a review of what we know (and of what we don’t). The world bank; 2004.
Molla A, et al. Prevalence of anemia and associated factors among infants and young children aged 6–23 months in Debre Berhan Town, North Shewa Ethiopia. J Nutr Metab. 2020;2020:2956129.
Malako BG, Teshome MS, Belachew T. Anemia and associated factors among children aged 6–23 months in Damot Sore District, Wolaita Zone South Ethiopia. BMC Hematol. 2018;18(1):1–9.
Shenton LM, Jones AD, Wilson ML. Factors associated with anemia status among children aged 6–59 months in Ghana, 2003–2014. Matern Child Health J. 2020;24(4):483–502.
Osório MM, et al. Prevalence of anemia in children 6–59 months old in the state of Pernambuco Brazil. Rev Panam Salud Publica. 2001;10:101–7.
Huang Y, et al. Prevalence and causes of anaemia in children aged 6–23 months in rural Qinghai, China: findings from a cross-sectional study. BMJ Open. 2019;9(9):e031021.
Harttgen K, Klasen S, Vollmer S. Economic growth and child undernutrition in sub-Saharan Africa. Popul Dev Rev. 2013;39(3):397–412.
Hansen C, Paintsil E. Infectious diseases of poverty in children: a tale of two worlds. Pediatr Clin. 2016;63(1):37–66.
Alsan MM, et al. Poverty, global health, and infectious disease: lessons from Haiti and Rwanda. Infect Dis Clin. 2011;25(3):611–22.
Woldie H, Kebede Y, Tariku A. Factors associated with anemia among children aged 6–23 months attending growth monitoring at Tsitsika Health Center, Wag-Himra Zone, Northeast Ethiopia. J Nutr Metab. 2015;2015:928632.
Osazuwa F, Ayo OM, Imade P. A significant association between intestinal helminth infection and anaemia burden in children in rural communities of Edo state, Nigeria. N Am J Med Sci. 2011;3(1):30.
Semahegn A, Tesfaye G, Bogale A. Complementary feeding practice of mothers and associated factors in Hiwot Fana Specialized Hospital Eastern Ethiopia. Pan Afr Med J. 2014;18:143.
Rao S, et al. Study of complementary feeding practices among mothers of children aged six months to two years-A study from coastal south India. Australas Med J. 2011;4(5):252.
Tepper RS, et al. Physiologic growth and development of the lung during the first year of life. Am Rev Respir Dis. 1986;134(3):513–9.
Alur P. Sex differences in nutrition, growth, and metabolism in preterm infants. Front Pediatr. 2019;7:22.
Sinha N, Deshmukh P, Garg B. Epidemiological correlates of nutritional anemia among children (6–35 months) in rural Wardha, Central India. Indian J Med Sci. 2008;62(2):45–54.
Chauhan SP, et al. Twins: prevalence, problems, and preterm births. Am J Obstet Gynecol. 2010;203(4):305–15.
Behrman RE, Butler AS. Preterm birth: causes, consequences, and prevention. 2007.
Huang Z, et al. Prevalence and risk factors of anemia among children aged 6–23 months in Huaihua Hunan Province. BMC Public Health. 2018;18(1):1–11.
Breymann C. Iron deficiency anemia in pregnancy. Semin Hematol. 2015;52(4):339–47 WB Saunders.
Souganidis ES, et al. Relationship of maternal knowledge of anemia with maternal and child anemia and health-related behaviors targeted at anemia among families in Indonesia. Matern Child Health J. 2012;16(9):1913–25.
Villalpando S, et al. Prevalence of anemia in children 1 to 12 years of age: results from a nationwide probabilistic survey in Mexico. Salud pública de México. 2003;45:490–8.
Guldan GS, et al. Maternal education and child feeding practices in rural Bangladesh. Soc Sci Med. 1993;36(7):925–35.
Prickett KC, Augustine JM. Maternal education and investments in children’s health. J Marriage Fam. 2016;78(1):7–25.
Frost MB, Forste R, Haas DW. Maternal education and child nutritional status in Bolivia: finding the links. Soc Sci Med. 2005;60(2):395–407.
Bicego GT, Boerma JT. Maternal education and child survival: a comparative study of survey data from 17 countries. Soc Sci Med. 1993;36(9):1207–27.
Habte D, et al. Maternal risk factors for childhood anaemia in Ethiopia. Afr J Reprod Health. 2013;17(3):110–8.
Kawo KN, Asfaw ZG, Yohannes N. Multilevel analysis of determinants of anemia prevalence among children aged 6–59 months in ethiopia: classical and bayesian approaches. Anemia. 2018;2018:3087354.
Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children< 5 years of age: evidence from 2012–2013 Pakistan demographic and health survey. BMC Public Health. 2019;19(1):1–15.
Mir MK, et al. Maternal anemia is a risk factor for low birth weight babies at term. Pak J Med Health Sci. 2016;10:741–3.
Abu-Ouf NM, Jan MM. The impact of maternal iron deficiency and iron deficiency anemia on child’s health. Saudi Med J. 2015;36(2):146.
Malkanthi R, Silva K, Jayasinghe-Mudalige UK. Risk factors associated with high prevalence of anemia among children under 5 years of age in paddy-farming households in Sri Lanka. Food Nutr Bull. 2010;31(4):475–82.
Rahman MS, et al. Association between malnutrition and anemia in under-five children and women of reproductive age: evidence from Bangladesh Demographic and Health Survey 2011. PLoS ONE. 2019;14(7):e0219170.
Headey D, et al. Rural food markets and child nutrition. Wiley Online Library; 2019
Kanjilal B, et al. Nutritional status of children in India: household socio-economic condition as the contextual determinant. Int J Equity Health. 2010;9(1):1–13.
Houweling TA, et al. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ. 2007;85:745–54.
Cogswell ME, et al. Iron supplementation during pregnancy, anemia, and birth weight: a randomized controlled trial. Am J Clin Nutr. 2003;78(4):773–81.
Yip R. Iron supplementation during pregnancy: is it effective? Am J Clin Nutr. 1996;63(6):853–5.
Leal LP, et al. Prevalence of anemia and associated factors in children aged 6–59 months in Pernambuco Northeastern Brazil. Rev Saude Publica. 2011;45:457–66.
Dutta M, et al. Prevalence and risk factors of anemia among children 6–59 months in India: a multilevel analysis. Clin Epidemiol Global Health. 2020;8(3):868–78.
Shiono PH, Behrman RE. Low birth weight: analysis and recommendations. Future Child. 1995;5:4–18.
Rahman MS, et al. Association of low-birth weight with malnutrition in children under five years in Bangladesh: do mother’s education, socio-economic status, and birth interval matter? PLoS ONE. 2016;11(6):e0157814.
Goswami S, Acharjee R, Dey S. Determinants of anaemia among children aged under five years in Assam, India. Int J Contemp Pediatr. 2020;7(11):1.
Goswami S, Das KK. A study of some predictors of anaemia in children of under-five years in India. Asian J Med Sci. 2014;5(2):26–32.
Chellan R, Paul L. Prevalence of iron-deficiency anaemia in India: results from a large nationwide survey. J Popul Soc Stud. 2010;19(1):59–80.
Amir-ud-Din R, et al. Impact of high-risk fertility behaviours on underfive mortality in Asia and Africa: evidence from demographic and health surveys. BMC Pregnancy Childbirth. 2021;21(1):1–14.
Kiggundu VL, et al. High prevalence of malaria parasitemia and anemia among hospitalized children in Rakai, Uganda. PLoS ONE. 2013;8(12):e82455.
Semba RD, et al. Diarrhea and fever as risk factors for anemia among children under age five living in urban slum areas of Indonesia. Int J Infect Dis. 2008;12(1):62–70.
Oakley MS, et al. Clinical and molecular aspects of malaria fever. Trends Parasitol. 2011;27(10):442–9.
Filmer D. Fever and its treatment among the more and less poor in sub-Saharan Africa. Health Policy Plan. 2005;20(6):337–46.
Teshale AB, et al. Anemia and its associated factors among women of reproductive age in eastern Africa: a multilevel mixed-effects generalized linear model. PLoS ONE. 2020;15(9):e0238957.
Acknowledgements
We would like to thank the measure DHS program for providing the datasets.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
BLS and GAT conceived the study. BLS and GAT analyzed the data, drafted the manuscript, and reviewed the article. BLS and GAT extensively reviewed the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Seifu, B.L., Tesema, G.A. Individual-and community-level factors associated with anemia among children aged 6–23 months in sub-Saharan Africa: evidence from 32 sub-Saharan African countries. Arch Public Health 80, 183 (2022). https://doi.org/10.1186/s13690-022-00950-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-022-00950-y