Abstract
Background
Most maternal and infant deaths occurred within the first month after birth. Nearly half of the maternal deaths and more than a million newborn deaths occurred within the first day of life but these were preventable through early initiation of postnatal care (PNC) services. However, the available evidence on the level of early initiation of PNC service utilization was not adequate to inform policy decisions. Therefore, this study aimed to assess time to early initiation of postnatal care and its predictors using the 2016 Ethiopian Demography and Health Survey (EDHS) datasets.
Methods
Two-stage stratified cluster sampling technique by separating each region into urban and rural areas. A total weighted sample of 6364 women of the 2016 EDHS datasets who gave birth within 2 years preceding the survey was used. Time to early initiation of the PNC visit was estimated using the Kaplan-Meier (K-M) method. Shared frailty model with baseline distributions (Weibull, Gompertz, exponential, log-logistic, and lognormal) and frailty distributions (gamma and inverse Gaussian) were used by taking enumeration areas/clusters as a random effect for predictors of time to early initiation of PNC visit. The adjusted hazard ratio (AHR) with a 95% confidence interval (CI) and p-value less than 0.05 were used to declare the significant predictor variables for time to early initiation of the PNC service utilization.
Results
The prevalence of women who utilized PNC services within 42 days was 13.27% (95% CI, 12.46, 14.13). Among these women, only 1.73% of them had got within the first 24 h of birth; 4.66% of them received within 48–72 h and 1.74% of them also had got within 7–14 days. Variables, such as parity (AHR = 1.61, 95% CI: 1.21, 2.15), media exposure (AHR = 1.42, 95% CI: 1.21, 1.68), place of delivery (AHR = 14.36, 95% CI: 11.76, 17.53), caesarean delivery (AHR = 2.17, 95% CI: 1.60, 2.95) and antenatal care visit (AHR = 2.07, 95% CI: 1.63, 2.63) had the higher hazard for PNC services utilization. On the other hand, women who faced with healthcare access problems (AHR = 0.74, 95% CI: 0.60, 0.87) had a lower hazard of PNC service utilization.
Conclusion
The overall postnatal care service utilization among women in the survey was low, particularly within the first 24 h of delivery. Policy-makers and implementers should promote the utilization of antenatal care and institutional delivery using mass media to increase the continuum of maternity care. The government should also design a new approach to enhance the uptake of postnatal care services for poor households and to scale up the PNC services, including the different possibilities for women who give births at the health facilities and homes. Future researchers had better assess the capacity and accessibility of the local health systems, the level of decentralized decision making, common cultural practices, knowledge, attitude, and perception of mothers towards PNC service utilization.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Postnatal care is care given to the mother and her newborn baby immediately after the birth of the placenta and the first 42 days of life. The postnatal period is the days and weeks following childbirth and it is a critical phase in the lives of mothers and newborn babies. All mothers and babies need at least four postnatal checkups in the first 6 weeks. These visits are on the first day (24 h), day 3 (48–72 h), between days 7–14, and 6 weeks [1]. Almost half of the postnatal maternal deaths occur within the first 24 h of birth, and 66% occur during the first week of birth [2]. In 2013, about 2.8 million newborns died in their first month of life and 1 million of these died on the first day of birth. The majority of maternal and neonatal deaths occur during childbirth and the postnatal period and approximately 303,000 maternal deaths occurred globally in 2015 [3].
To curb this problem, the new globally adopted agenda between 2016 and 2030 as a part of the sustainable development goal aimed to reduce the maternal mortality ratio to 70 per 100,000 live births by addressing all maternal health care services for every woman as a top priority [4]. A substantial number of women had an antenatal visit before getting other subsequent maternal health care services in many countries, however, they failed to access skilled birth attendants and postnatal care [5]. Only 67 and 48% of women gave birth with the assistance of skilled personnel in South-East Asia and sub-Saharan Africa, respectively [6]. Below half of the women received a postnatal care visit within the first 2 days of childbirth. The findings from the 23 sub-Saharan African countries indicated that only 13% of women who delivered at home received postnatal care within the first 2 days of birth [7].
Ethiopia is organized in the nine national regional states and the two city administrations. The nine regions are Tigray, Afar, Amhara, Benishangul-Gumuz, Gambela, Harari, Oromia, Somali, and Southern Nations, Nationalities, and People’s of Region (SNNP) regions, and the two city administrations are Addis Ababa and Dire-Dawa. Each region and city administrations have its own autonomous Regional Health Bureau (RHB). The healthcare delivery in Ethiopia is organized in a three-tier System. The first, at the district level, is the Primary Healthcare Unit (PHCU). The PHCU comprises one primary hospital, four health, and five health posts that are attached to each health center. The second level comprises general hospitals, while the third level comprises specialized hospitals.
In the Ethiopian healthcare system, some public health services have been provided to all citizens free of charge regardless of the level of income. This has occurred because of the nature of these activities and the need to promote the use of certain health care services. These services are tuberculosis treatment and follow-up, HIV/AIDS testing and treatment, immunization service, maternal health care services, including antenatal care, delivery care, postnatal care, and family planning service.
Ethiopia is one of the countries with low coverage of both access to basic health services and health service utilization, a high geographical (urban-rural area) disparity as well as a high catastrophic out-of-pocket spending for healthcare services. However, exemption services or cost-sharing for high-priority interventions are the key strategies of the government of Ethiopia to achieve Universal Health Coverage (UHC) [8, 9]. The PNC services are made accessible to the village level with lower or no cost in Ethiopia but only 17% of women received a postnatal check-up in the EDHS 2016 which is far from 26% of institutional delivery service utilization [10]. The PNC service utilization in Debre Markos town and Dembecha district in northwest Ethiopia was 33.5 and 34.8%, respectively [11, 12]. Moreover, PNC service utilization among women in the Jimma zone was 58.5 and 36.7% in Loma district [13], Ethiopia. Even though the trends of reproductive health service indicators had significant improvement, the gap in the continuum of maternal healthcare services remains remarkably high. This study, therefore, aimed to analyze the time to early initiation of postnatal care and its predictors among women who gave birth in the last 2 years in Ethiopia using the 2016 EDHS datasets.
Methods
Data source and sampling procedure
Secondary data analysis was conducted based on the EDHS 2016. The EDHS used a stratified two-stage cluster sampling technique selected using the 2007 Population and Housing Census as a sampling frame. A total of 84,915 Enumeration Areas (EAs) were created in Ethiopia and stratification was done by dividing each of the nine regions into urban and rural areas and a total of 21 sampling strata were formed. In the first stage, 645 enumeration areas (202 in the urban area) were selected with proportional allocation to the size of the enumeration areas (EAs) with an independent selection of each sampling stratum. A total of 243 EAs that have less than 10 observations per cluster (a total of 1225 observations) were dropped. A total of 402 EAs were, therefore, included for analysis to get a reliable estimate. A minimum of 10 and maximum of 21 women or on average 15 women per EAs were selected using systematic sampling technique. A total weighted sample of 6364 women who gave birth within 2 years preceding the survey were included for this study (Fig. 1). The detailed sampling procedure was presented in the full EDHS 2016 report [14].
Study variables
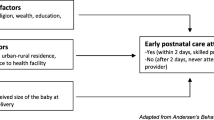
Women who gave birth within 2 years preceding the survey were considered in this study and those who had PNC visits within 42 days of birth were considered as a success while those who didn’t have a visit were treated as a failure. It is defined as the time of first PNC checkup within the first 42 days of birth. The time to first PNC visit was recorded in days if the women have a PNC visit within 42 days of birth. The event is binary form, coded as “1” if a woman had a PNC visit within 42 days of birth and “0” if the women didn’t have a PNC visit within the 42 days. The independent variables considered for this study were categorized as socio-demographic and economic variables (residence, region, religion, maternal education, husband education, maternal occupation, sex of household head, distance to the health facility, and wealth status), and obstetric related factors (the type of gestation, preceding birth interval, ANC visit, place of delivery, mode of delivery, parity, birth order).
Data management and analysis
The data were weighted using sampling weight, primary sampling unit, and strata before any statistical analysis to restore the representativeness of the survey and to take into account the sampling design to get reliable statistical estimates. STATA version 14 software was used for the descriptive as well as for the frailty analysis. Because of the hierarchical structure of EDHS data, women are nested within a cluster and we expect that women within the same cluster may be more similar to each other than women in the rest of the country. This violates the assumption of the traditional regression model which is the independence of observations and equal variance across clusters. A total of 243 EAs that have less than 10 observations per cluster (a total of 1225 observations) were dropped from the analysis to balance the size of clusters and detect the random effect efficiently. The standard survival analysis models are applicable when the time to event data is independent but the EDHS was a cluster survey that has hierarchical nature and assumed to be correlated at the cluster level. The correlation could be due to unobserved cluster or EAs specific covariates and assumes that time to early initiation of PNC service of a mother is a function of measured variables and a random (frailty) on the baseline hazard to the unobserved cluster effect. Schoenfeld residual global test was applied to check the Proportional Hazard (PH) assumption, and it was violated with a p-value < 0.05 (Supplementary file 1).
Parametric survival models were fitted since the PH assumption was violated. The EDHS data has a hierarchical structure and a frailty model (random effect survival model) was used to check whether there is clustering or not. The theta was significant at the null model (θ = 1.47, 95% CI: 1.26, 1.72). It indicates that there was unobserved heterogeneity or shared frailty in which women in one cluster were more likely to be correlated with women in the same cluster. Shared frailty model with baseline distributions (Weibull, Gompertz, Exponential, log-logistic, and lognormal) and frailty distributions (gamma and inverse Gaussian) were used by taking EAs of v001 as a random effect for predictors of time to early initiation of PNC visit among women who gave births. A Weibull gamma shared frailty model was the best-fitted model for this data since it has the smallest deviance and AIC values. Variables with a p-value less 0.20 in the uni-variable of the Weibull gamma shared frailty analysis were included in the multivariable analysis. The Hazard Ratio (HR) with 95% Confidence Interval (CI) and p-value less than 0.05 were used to declare the significant predictor variables for time to early initiation of the PNC service utilization.
The model was formulated as:
For time to event data, where i (1 ………., n) denotes the cluster, while j (1, ……, n) denotes the subjects (woman) within the cluster. The frailty, u i is a random positive quantity shared within groups, whereas hij (t│xij,ui) is the probability of women initiating PNC service at time t; h0(t) is the baseline hazard and Xij is a vector of covariates with the associated vector of fixed parameters β. Time to early initiation of the PNC visit was estimated using the Kaplan-Meier (K-M) method. The log-rank test was used to compare survival time between groups of categorical variables.
Results
Socio-demographic and economic characteristics of women
A total of 6364 women who gave birth within 2 years the survey was included in the study. Of these, 2825 (44.4%) were in the Oromia region, and 6033 (94.8%) were rural residents. Half (49.7%) of the women were in the age groups of 25–34 years. About 4267 (67.1%) of the women and 2967 (46.6%) of their husbands had no formal education (Table 1).
Obstetric related characteristics of women
A total of 2595 (40.8%) mothers had 2–4 births and 4745 (75.6%) gave births at home among 6364 women who gave birth in the last 2 years. The majority (59%) of women had ANC visits during pregnancy and only 1.2% gave birth through caesarean section. About 5366 (84.3%) of the women had a preceding birth interval of 2 or more years, and 95 (1.5%) of mothers had twin birth (Table 2).
Predictors of time to early initiation of PNC
The overall prevalence of women who had utilized postnatal care services within 42 days was 13.27% (95% CI: 12.46, 14.13). Among these women, only 1.73% of them had got within the first 24 h of birth and 4.66% of them received within 48–72 h. On top of that, 1.74% of women received their first PNC from 7 to 14 days of the postpartum period. Kaplan Meier’s failure curve was used to compare PNC service utilization within 42 days among categories of independent variables graphically. The Kaplan Meier(K-M) failure curve was done for all possible predictors. The K-M curve differs for various educational categories of women, ANC visit, and place of delivery, birth outcome, and mode of delivery. The overall Kaplan-Meier failure curve indicated that the probability of PNC visits was highest on the first-day postpartum period that is relatively increased as follow-up time increases (Fig. 2).
Log-rank test for the predictors of PNC
Residence, ANC, birth outcome, place of delivery, preceding birth interval, region, maternal education, husband education, respondent age, twin pregnancy, parity, and wealth index showed a statistically significant difference in probability of early initiation of PNC visit with the log-rank test of p < 0.05 (Supplementary file 2).
Model comparison and diagnostics for PNC
The theta was significant at the null model (θ = 16, 95% CI: 0.10, 0.29), LR test of theta = 0: chibar2(01) = 22.60, Prob > = chibar2 = 0.0001. The shared frailty model with the Weibull baseline hazard function with gamma frailty had the smallest AIC, BIC, deviance, and theta value than the other models and was the best-fitted model for identifying predictors of time to early initiation of PNC service (Supplementary file 3).
Multivariable survival analysis
In the multivariable gamma shared Weibull model; type of birth, parity, preceding birth interval, media exposure, health care access problem, place of delivery, ANC visit, and mode of delivery were significant predictors of early initiation of PNC checkup. Women who had twin births 2.05 times (AHR = 2.05, 95% CI: 1.32, 3.18) more likely to utilize PNC service than singletons. Mothers who had 2–4 births and 5 or more births were 1.52 times (AHR = 1.52, 95% CI: 1.23, 1.87) and 1.61 times (AHR = 1.61, 95% CI: 1.21, 2.15) higher likelihood of PNC service utilization compared with their counterparts, correspondingly. Mothers who had media exposure (AHR = 1.42, 95% CI: 1.21, 1.68), institutional delivery (AHR = 14.36, 95% CI: 11.76, 17.53), and caesarean delivery (AHR = 2.17, 95% CI: 1.60, 2.95) had the higher hazard of PNC service utilization compared with their counterparts, respectively. Similarly, women who made ANC visit had two folds (AHR = 2.07, 95% CI: 1.63, 2.3) higher likelihood of PNC service utilization compared with those who had no ANC attendance. On the contrary, women who faced big healthcare access problems (AHR = 0.74, 95% CI: 0.63, 0.87) decreases the hazard of PNC service utilization by 26% (Table 3).
Discussion
Despite the significant improvement in maternal and child healthcare interventions, maternal mortality ratio (MMR) was 412 per 100,000 live births and the neonatal mortality rate was 29 per 1000 livebirths in Ethiopia [10]. These are still our challenges to achieve the HSTP goals of MMR of 199 per 100,000 live births and neonatal mortality of 10 per 1000 live births in the country [15]. Most neonatal deaths usually occur in the first 24 h of life, and three -quarters of neonatal deaths occur in the first week after birth [16]. Provide PNC in the first 24 h to all mothers and babies, regardless of where the birth occurs is desirable [17]. The movement of mothers and babies is culturally restricted for a period of seclusion after delivery, particularly in African communities. Keeping mothers and babies indoors for the first month after birth, and seeking formal health care is often delayed when mothers or babies become ill during the period of seclusion [18, 19].
This study has investigated the association of socioeconomic, demographic, and environmental.
factors with the likelihood of PNC service utilization used by accounting for gamma-distributed shared frailties at the cluster-level. In this study, about 13.27% of mothers received postnatal check-ups from a trained health service provider within 42 days of delivery. This result was higher than in Abi Adi town, Ethiopia (11.90%) [20]. On the contrary, the finding was lower than the studies conducted in Jabitena, Ethiopia (20.20%) [21], North Shoa (928.4%) [22], Ambo (33.4%) [23], Assela (72.7%) [24], Jimma (58.5%) [25], Debre Markos (33.5%) [11], Dembecha (34.8%) [12], Loma (36.7%) [13], Lemo (51.4%) [26], Ethiopia, South Africa (59.6%) [27], North Eastern Nigeria (16.9%) [28], Bangladesh (55.6%) [29], Myanmar(25.2%) [30] and Nepal (34%) [31]. Moreover, only 1.73 and 6.39% of mothers received PNC services within the first 24 and 72 h of the postpartum period in the survey. This was lower than the studies done in Bangladesh (27.3%) [29] and Nepal (19%) [31]. The possible justification for this variation might be due to the differences in study settings, areas, participant characteristics, design, and period. This could be some of the previous studies might be done only among urban women who attended health facilities since these participants might have a higher chance to access media exposure and maternal healthcare services.
The hazard of PNC service utilization was higher for women who had media exposure than media non-users. This finding was supported by the studies done in India [32] and Nepal [31]. This might be due to those women who had media exposure could have adequate information about maternal health care services. Women who had twin births and a greater number of parities had a higher hazard of PNC service utilization compared with their counterparts. This could be because mothers who had twin births and more parities are tending to have greater perceived susceptibility to a wide range of complications therefore frequent visits to the health institution would be the strategy to minimize their perceived risks. On the contrary, this finding contradicted studies conducted in North Shoa, Ethiopia, and Nepal [31]. This might be justified by the fact that first-time mothers are usually dependent upon the support of health professionals and their families for infant care and feeding practices. Besides, they would be very curious about the health of their newborn baby, thus, these needs might be satisfied through frequent contact with health facilities.
Mothers who had ANC follow up had a higher hazard for PNC service utilization. This result was in line with the studies conducted in Ambo [23], Assela [24], Jimma [25], Dembecha [12], Lemo [26], Ethiopia, South Africa [27], and Nepal [31]. The possible explanation for the strong positive association between ANC attendance and PNC service utilization might be that mothers and their families receive health education and advise during ANC visits and thus become access to learn about the benefits of PNC services follow up in health care facilities.
The hazard of PNC service was higher among health facility delivery attended women compared with home-delivered mothers. The finding was in line with the studies done in Abi Adi town, Ethiopia [20], Gulele Sub-city, Addis Ababa [33], Jimma [25], Debre Markos [11], Jabitena [21], Gondar Zuria [34], Loma [13], Lemo [26], Ethiopia, Royal king of Cambodia [35], Bangladesh [36], and South Africa [27], which indicates that giving birth at health institution has significantly associated with PNC service utilization. The possible explanation could be attributed to the fact that women who gave their last birth in health institution have a greater opportunity for health education related to PNC services at the time of delivery and thus get access to learning about the types, benefits, and availabilities of PNC services during their stay in the health institutions. This exposure increases healthcare-seeking behavior to prevent maternal and neonatal complications compared to those mothers who gave birth at home. Furthermore, those women who gave birth at home belong to a more traditional cohort and thus become less likely to use postnatal care services [37].
Women who gave birth by caesarean section had a higher hazard of postnatal care service utilization compared with women who gave birth via spontaneous vaginal delivery. This finding was supported by the studies done in North Shoa [22], Debre Markos [11], Ethiopia, and Tanzania [38]. The possible justification could be mothers who had operative delivery are tending to have greater perceived susceptibility to a wide range of postoperative complications therefore frequent return to the health institution would be the strategy to minimize their perceived risks.
On the contrary, women who faced healthcare access problems had a lower hazard of PNC service utilization than mothers who did not face healthcare access problems. This could be because the availability of services and understanding of the importance of postnatal care is vital to improving its uptake, however, physical distance limits women’s willingness and ability to seek health care, particularly when appropriate transportation is scarce and communications and the terrain are difficult [39].
This finding indicated that the PNC services are among the weakest of all reproductive and child healthcare services in Ethiopia. This might alarm the policy on how can they increase the coverage of early initiation of PNC services to provide integrated maternal and newborn care in the postnatal period. This can also give a chance for policymakers to decide and integrate the PNC services with the existing strategies and programs, especially in childbirth care, Integrated Management of Childhood Illness (IMCI), nutrition promotion, prevention of mother-to-child transmission of HIV, and immunization. This might also give a hint to evaluate the approaches used to promote maternal healthcare services that have been delivered using the community health workers (CHWs), mother support group (MSG), women health development army (HAD), and the use of mass media for maternal services.
The Weibull gamma shared frailty model to identify the significant predictors for the early initiation of PNC visits. This model was chosen since the DHS data has hierarchical nature and could violate the basic assumptions of standard survival models. Frailty model is therefore important to get a reliable estimate and standard error since it takes into account the clustering effect while estimating the coefficients and standard errors by introducing the EAs as a random effect. The standard survival model could not give a reliable estimate and standard error for such data. A comparison of the survival models was done using deviance, AIC, and theta values to decide which model is appropriate for the data because the appropriate model is needed to get valid evidence for policymakers. The use of a weighted nationally representative EDHS data and the use of advanced survival model (Gompertz gamma shared frailty model) were therefore the strengths of the study. On the other hand, the limitations of this study could be that the EDHS survey did not incorporate the communities’ and respondents’ knowledge, attitude, and perception towards PNC service utilization, such as the community’s level of awareness, norms, and beliefs towards PNC. This study also lacks the assessment of the capacity and accessibility of the local health systems, the level of decentralized decision making, and common cultural practices, particularly cultural practices regarding seclusion that may reduce care-seeking. Moreover, the data were collected based on the mother’s or caregiver’s report and might introduce the possibility of social desirability and recall bias.
Conclusion
The study indicated that early initiation of postnatal care utilization was low in Ethiopia. A very low proportion of women received postnatal care within the most critical period (within 24 h) after delivery. It is important to ascertain further why postnatal care rates are so low. Though barriers to receiving postnatal care were antenatal care, media exposure, place of delivery, mode of delivery, and access to maternal health services were important predictors for the utilization of early postnatal care. The policymakers and implementers should promote the utilization of antenatal care and institutional delivery service utilization through mass media. The government should also design a new approach to enhance the uptake of postnatal care services for poor households and to scale up the PNC services, including the different possibilities for women who give births at the health facilities and homes. Future researchers had better assess the capacity and accessibility of the local health systems, the level of decentralized decision making, common cultural practices, knowledge, attitude, and perception of mothers towards PNC service utilization.
Availability of data and materials
The datasets used during the current study are available at Measure DHS website: http://www.measuredhs.com.
Abbreviations
- ANC:
-
Antenatal Care
- EA:
-
Enumeration Area
- EDHS:
-
Ethiopia Demography Health Survey
- PNC:
-
Post Natal Care
- SD:
-
Standard Deviation
- USD:
-
US Dollar
- WHO:
-
World Health Organization
References
World Health Organization: Postnatal Care for Mothers and Newborns Highlights from the World Health Organization 2013 Guidelines. 2015.
Nour N. An introduction to maternal mortality. Rev Obstet Gynecol. 2008;1(2):77–81.
World Health Organization. Maternal deaths fell 44% since 1990–UN: Report from WHO, UNICEF: UNFPA, World Bank Group and the United Nations Population Division; 2015.
Freedman LP. Implementation and aspiration gaps: whose view counts? Lancet. 2016;388(10056):2068–9. https://doi.org/10.1016/S0140-6736(16)31530-6.
Vidler M, et al. Utilization of maternal health care services and their determinants in Karnataka State, India. Reprod Health. 2016;13(1):37.
WHO. World Health Statistics 2014. Geneva: WHO; 2014.
Warren CDP, Toure L, Mongi P. In: Lawn J, Kerber K, editors. Postnatal Care in Opportunities for Africa’s Newborns: Practical Data Policy and Programmatic Support for Newborn Care in Africa. Cape Town: Partnership for Maternal, Newborn and Child Health; 2006. p. 79–90.
Federal Democratic Republic of Ethiopia Ministry of Health. Health sector transformation plan 2008–2012 EFY. Addis Ababa: Federal Democratic Republic of Ethiopia Ministry of Health; 2015.
Federal Democratic Republic of Ethiopia Ministry of Health. Envisioning Ethiopia’s path towards universal health coverage through strengthening primary health care. Addis Ababa. IIfPHC-E; 2015.
Central Statistical Agency. Ethiopian Demographic and Health Survey. Central Statistical Agency Addis Ababa. Maryland: Ethiopia ICF International Calverton; 2011.
Limenih MA, Endale ZM, Dachew BA. Postnatal Care Service Utilization and Associated Factors among Women Who Gave Birth in the Last 12 Months prior to the Study in Debre Markos Town, Northwestern Ethiopia: A Community-Based Cross-Sectional Study. Int J Reprod Med. 2018;2016.
Hordofa MA, Almaw SS, Berhanu MG, Lemiso HB. Postnatal Care Service Utilization and Associated Factors Among Women in Dembecha District, Northwest Ethiopia. Sci J Public Health. 2015;3(2).
Yarinbab TE, Tona WC. Postnatal Care Utilization and Its Determinants in Loma District, Southwest Ethiopia: A Community Based Cross Sectional Study. J Womens Health Gyn. 2018;5.
ICF CSACEa. Ethiopia Demographic and Health Survey 2016. Addis Ababa and Rockville: CSA and ICF; 2016.
Federal Democratic Republic of Ethiopia Ministry of Health. HSTP Health Sector Transformation Plan 2015/16–2019/20 (2008–2012 EFY): Federal Democratic Republic of Ethiopia Ministry of Health; 2015.
Lawn JE, Cousens S, Zupan J, Team LNSS. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. https://doi.org/10.1016/S0140-6736(05)71048-5.
Organization WH: Postnatal care for mothers and newborns: Highlights from the World Health Organization 2013 Guidelines. Avaible from: http://www.who.int/maternal_child_adolescent/publications/WHOMCA-PNC-2014-Briefer_A2015,4. Accessed April 2015
Baiden F, Hodgson A, Adjuik M, Adongo P, Ayaga B, Binka F. Trend and causes of neonatal mortality in the Kassena–Nankana district of northern Ghana, 1995–2002. Tropical Med Int Health. 2006;11(4):532–9. https://doi.org/10.1111/j.1365-3156.2006.01582.x.
Li X, Fortney J, Kotelchuck M, Glover L. The postpartum period: the key to maternal mortality. Int J Gynecol Obstet. 1996;54(1):1–10. https://doi.org/10.1016/0020-7292(96)02667-7.
Alemayeh H, Assefa H, Adama Y. Prevalence and Factors Associated with Post Natal Care Utilization in Abi-Adi Town, Tigray, Ethiopia: A Cross Sectional Study. IJPBSF Int J Pharm Biol Sci Fundam. 2014;8(1).
Workineh YG, Hailu DA. Factors affecting utilization of postnatal care service in Jabitena district, Amhara region, Ethiopia. Sci J Public Health. 2013;2:169–76.
Akibu M, Tsegaye W, Megersa T, Nurgi S. Prevalence and Determinants of Complete Postnatal Care Service Utilization in Northern Shoa, Ethiopia. J Pregnancy. 2018;2018:8625437. https://doi.org/10.1155/2018/8625437.
Moreda TB, Gebisa K. Assessment of Postnatal Care Service Utilization and Associated Factors among Mothers Attending Antinatal Care at Ambo Health Facilities. Epidemiol Int J. 2018;2(2).
Tumbure A, Argaw D, Fantahun E, Negusu M, Yitbarek T, Tadesse L, et al. Assessment of postnatal care service utilization and associated factors in Asella town, Arsi zone, Oromiya regional state, Ethiopia. Glob J Reprod Med. 2018;6(1).
Chemir F, Gelan M, Sinaga M. Postnatal Care Service Utilization and Associated Factors among Mothers Who Delivered in Shebe Sombo Woreda, Jimma Zone, Ethiopia. Int J Womens Health Wellness. 2018;4(2).
Tefera B, Ayanos T, Tamiru B. Postnatal Care Service Utilization and Associated Factors among Mothers in Lemo Woreda, Ethiopia. J Womens Health Care. 2016;5(3).
Larsen A, Cheyip M, Aynale G, Dinh T-h, Jackson D, Ngandu N, et al. Uptake and predictors of early postnatal follow–up care amongst mother–baby pairs in South Africa: Results from three population–based surveys, 2010–2013. J Glob Health. 2017;7(2).
Takai IU, Dlakwa HD, Bukar M, Audu BM, Kwayabura AS. Factors responsible for under-utilization of postnatal care services in Maiduguri, North-Eastern Nigeria. Sahel Med J. 2015;18:109–15.
Syed U, Asiruddin S, Helal MS, Mannan II, Murray J. Immediate and Early Postnatal Care for Mothers and Newborns in Rural Bangladesh. J Health Popul Nutr. 2006;24(4).
Mon AS, Phyu MK, Thinkhamrop W, Thinkhamrop B. Utilization of full postnatal care services among rural Myanmar women and its determinants: a cross-sectional study. F1000Research. 2018;7.
Dhakal S, Chapman GN, Simkhada PP, van Teijlingen ER, Stephens J, Raja AE. Utilisation of postnatal care among rural women in Nepal. BMC Pregnancy Childbirth. 2007;7(1):19. https://doi.org/10.1186/1471-2393-7-19.
Yesudian PP. Impact of women's empowerment, autonomy and attitude on maternal health care utilisation in India. Glob Forum Health Res. 2005;8.
Abera S, Ayalneh BGA. Postnatal care services utilization and its associated factors among women who gave birth in the past one year in Gulele sub city, Addis Ababa, Ethiopia. J Health Med Nurs. 2018;46:238–46.
Tesfahun F, Worku W, Mazengiya F, Kifle M. Knowledge, perception and utilization of postnatal care of mothers in Gondar Zuria District, Ethiopia: a cross-sectional study. Matern Child Health J. 2014;18(10):2341–51.
Ith P, Dawson A, Homer CSE, Whelan AK. Practices of skilled birth attendants during labour, birth and the immediate postpartum period in Cambodia. Midwifery. 2013;29(4):300–7.
Mosiur Rahman M, Haque SE, Sarwar Zahan M. Factors affecting the utilisation of postpartum care among young mothers in Bangladesh. Health Soc Care Commun. 2011;19(2):138–47. https://doi.org/10.1111/j.1365-2524.2010.00953.x.
Berhe H, Tilahun W, Aregay A, Bruh G, Gebremedhim H. Utilisation and associated factors of postnatal care in Adwa town, Tigray, Ethiopia-a cross sectional study. Adv Res Pharm Biol. 2013;3(1):353–9.
Mohan D, Gupta S, LeFevre A, Bazant E, Killewo J, Baqui AH. Determinants of postnatal care use at health facilities in rural Tanzania: multilevel analysis of a household survey. BMC Pregnancy Childbirth. 2015;15:282.
van MA E, Bles HM, Odhiambo F, Ayisi GJ, Blokland EI, Rosen HD, et al. Use of antenatal and delivery care among women in rural western Kenya: a community based survey. Reprod Health. 2006;3(2).
Acknowledgments
The authors would like to thank MEASURE DHS for sharing the data for further analysis. We are also grateful to thank others who are directly or indirectly involved during the preparation of this manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AD and GAT conceived the study, involved in the study design, data analysis, drafted and critically reviewed the manuscript. All authors read and approved the final manuscript.
Authors’ information
AD is an Assistant Professor of Health Service Management at the Department of Health Systems and Policy, Institute of Public Health, University of Gondar, Gondar, Ethiopia, and GAT is a lecturer in Epidemiology working as an instructor at the Department of Epidemiology and Biostatistics, Institute of Public Health, University of Gondar, Gondar, Ethiopia.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The 2016 EDHS data are available to the general public by request in different formats from the Measure DHS website http://www.measuredhs.com. We submitted a request to the Measure DHS by briefly stating the objectives of this analysis and thereafter received permission to download the maternal and children’s dataset in STATA format.
Consent for publication
Not applicable as there is no image or other confidentiality related issues.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Proportional hazard assumption for the incidence of early initiation of PNC utilization and its predictors among women who gave births in the last 2 years in Ethiopia, 2016
Additional file 2.
Log rank test for the predictors of PNC services utilizations among mothers who gave birth in the last 2 years, 2016
Additional file 3.
Model comparison and diagnostics for PNC service utilization among mothers in Ethiopia, 2016
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Debie, A., Tesema, G.A. Time to early initiation of postnatal care service utilization and its predictors among women who gave births in the last 2 years in Ethiopia: a shared frailty model. Arch Public Health 79, 51 (2021). https://doi.org/10.1186/s13690-021-00575-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-021-00575-7