Abstract
Background
Developmental and Epileptic Encephalopathies (DEEs) are defined by drug-resistant seizures and neurodevelopmental disorders. Over 50% of patients have a genetic cause. Studies have shown that patients with DEEs, regardless of genetic diagnosis, experience a central visual function disorder known as Cerebral (cortical) Visual Impairment (CVI). The prevalence of CVI in DEE patients is currently unknown. A quantitative synthesis of existing data on the prevalence rates of this condition would aid in understanding the magnitude of the problem, outlining future research, and suggesting the need for therapeutic strategies for early identification and prevention of the disorder.
Methods
The protocol followed the PRISMA-P statement for systematic review and meta-analysis protocols. The review will adhere to the JBI Manual for Evidence Synthesis (Systematic Reviews of Prevalence and Incidence) and use the CoCoPop framework to establish eligibility criteria. We will conduct a comprehensive search of several databases, including MEDLINE, EMBASE, Science Direct, Scopus, PsychINFO, Wiley, Highwire Press, and Cochrane Library of Systematic Reviews. Our primary focus will be determining the prevalence of cerebral visual impairments (Condition) in patients with developmental and epileptic encephalopathy (Population). To ensure clarity, we will provide a narrative summary of the risk of bias in the studies we include. The Cochrane Q statistic will be used to assess heterogeneity between studies. If the quantitative synthesis includes more than 10 studies, potential sources of heterogeneity will be investigated through subgroup and meta-regression analyses. Meta(bias)es analysis will also be performed. The quality of evidence for all outcomes will be evaluated using the Grading of Recommendations Assessment Development and Evaluation (GRADE) working group methodology.
Discussion
This protocol outlines a systematic review and meta-analysis to identify, collect, evaluate, and integrate epidemiological knowledge related to the prevalence of CVI in patients with DEEs. To the best of our knowledge, no other systematic review and meta-analysis has addressed this specific issue. The results will provide useful information for understanding the extent of the problem, outlining future research, and suggesting the need for early identification strategies.
Systematic review registrations
This Systematic Review Protocol was registered in PROSPERO (CRD42023448910).
Similar content being viewed by others
Introduction
Background and rationale
Developmental and Epileptic Encephalopathies (DEEs) are characterized by epileptic seizures, mainly drug-resistant, neurodevelopmental disorders (neuro- and psychomotor regression, intellectual disability, cognitive impairment, behavioural disorders, and relational difficulties) [1]. In both clinical and pre-clinical studies, it has been observed that patients with DEEs, regardless of the genetic diagnosis, present a disorder of visual functions of central origin defined in the literature as “Cerebral (cortical) Visual Impairment” (CVI) [1]. The clinical features of CVI differ from patient to patient [2] and are represented by a broad spectrum of visual disorders that include ophthalmological, oculomotor and perceptual anomalies [3]. Patients with DEEs may present with oculomotor and perceptual alterations, and visuospatial and visuo-perceptual dysfunctions [1]. The clinical presentations are attributable to anomalies of the primary visual pathway and associated visual areas. Abnormalities of the oculomotor apparatus and ocular system can be associated.
The ILAE Task Force on Nosology and Syndrome Definition divides DEEs according to the age of onset of the first seizure [1]. More than half of patients have a genetic aetiology.
To date, the relationship between epileptic seizures, neurodevelopmental disorders and CVI is very complex and severe neuro- and psychomotor delay and intellectual disability often have a strong negative impact on the quality of life of patients and their caregivers/families.
Different studies conducted in recent years [4,5,6,7,8,9] in patients with CDKL5 Developmental and Epileptic Encephalopathy (CDKL5-DEE) have shown that CVI is one of the main features of the disease. Similarly, studies conducted in the early 2000s in patients with West Syndrome [10,11,12] demonstrated that visual function skills were already impaired at the onset of the spasms. Studies with similar results have been conducted in patients with Dravet syndrome [13, 14]. Furthermore, CVI is a common feature of other forms of DEEs. For instance, it has been identified in patients with mutations in the KCNQ2 [15], SCN3A [16], SCN8A [17] and GRIN2B [18] genes. Nowadays, the prevalence of CVI in patients with DEEs, regardless of genetic diagnosis, is unknown. A quantitative summary of the existing data on the prevalence rates of this condition would aid in comprehending the extent of the problem, outlining future research, and suggesting the need for therapeutic strategies for early identification and prevention of the disorder. Early identification allows the implementation of “early intervention” programs necessary to address difficulties already emerging as risk conditions for neuro-developmental disorders during “critical periods” of neuronal plasticity [19]. Cortical circuits show a maximum sensitivity to sensory stimuli induced by experience in the postnatal period [20] compared to adulthood. Exposure to an “enriched environment”, as occurs in early neuro-rehabilitative intervention, stimulates axonal plasticity and synaptic reorganization [21] and has been shown to accelerate the development of the visual system [22, 23]. In this theoretical framework, the quantitative analysis of the prevalence rate of CVI in patients with a diagnosis of DEEs, according to the ILAE classification [1], is therefore necessary. A preliminary search for previous systematic reviews was conducted in the Cochrane Library, PubMed and PROSPERO.
Objectives
This systematic review aims to describe the prevalence of Cerebral Visual Impairment (CVI) among patients with a diagnosis of Developmental and Epileptic Encephalopathies (DEEs) according to the 2021 International League Against Epilepsy (ILAE) classification [1].
The proposed systematic review will address the following questions:
-
1.
What is the prevalence of CVI among patients with DEEs?
-
2.
What study methodological characteristics explain the heterogeneity in results?
Methods
This study followed the PRISMA-P statement [24] for systematic review and meta-analysis protocols and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) network [25]. The JBI Manual for Evidence Synthesis (Systematic Reviews of Prevalence and Incidence) [24] will be used for the review [26].
Inclusion criteria
We will use the condition, context and population framework (CoCoPop) for the systematic review of prevalence and incidence to formulate the eligibility criteria [27].
Condition: CVI must have been diagnosed and examined by a physician in clinical studies with an objective neuro-visual assessment. The diagnosis of CVI is indicated for children showing abnormal visual responses that cannot be attributed to the eyes themselves. Despite intense stimulation, a child may not be able to fixate and follow, and his/her reaction to faces is abnormal [2,3,4].
Context: there will be no restrictions by type of setting.
Population: We will include clinical studies examining patients with Developmental and Epileptic Encephalopathies (DEE) of broad genetic aetiologies. There will be no restrictions based on sex, age, race/ethnicity, or geographic region. DEEs described in eligible clinical studies must have been diagnosed by a physician based on the criteria from the ILAE Epilepsy Diagnosis.org Task Forces [1]. DEEs are defined as diseases where there is a developmental impairment related to both the underlying aetiology independent of epileptiform activity and epileptic encephalopathy. We will include studies involving patients with “Early Infantile DEE” with onset under 3 months of age and other syndromes which either typically present after 3 months of age or have a spectrum of onset encompassing early and late infancy.
Studies: We will include all completed publications reporting the assessment of CVI in patients with DEEs in clinical (observational, cohort studies, cross-sectional studies, retrospective studies) and pre-clinical (in vivo) studies.
Outcome measure: the primary outcome will be the prevalence of CVI indicating the number of people with DEEs that have the disorder at a given point in time. The secondary outcome will be the prevalence of a specific genetic mutation in the group of patients with DEEs and associated CVI, by calculating the number of patients with a specific genetic diagnosis of DEEs and CVI divided by the total number of patients with DEE and CVI.
Language: We will include articles reported in English and Italian.
Search strategy
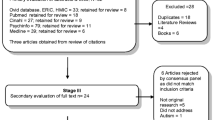
Comprehensive literature searches of electronic bibliographic databases will be conducted. The specific search strategies will be created by a Health Sciences Librarian with expertise in systematic review searching using Medical Subject Headings (MeSH) and text words related to CVI and DEEs. An independent librarian, not associated with the project, will peer-review the MEDLINE strategy developed by the project team. A draft search strategy for PubMed is provided in Additional file 1. We will search MEDLINE, EMBASE, Science Direct, Scopus, PsychINFO, Web of Science, Wiley and Highwire Press and Cochrane Library of Systematic Reviews. No time restrictions will be placed on the date of publication. Upon completion, identified citations will be exported to a cloud-based citation manager for study selection. A final grey literature search will be conducted on medical books and reports from experts, as well as a review of a trial register for any ongoing and unpublished studies. Further, to ensure literature saturation we will scan the reference lists of included studies or relevant reviews identified through the search. Duplicate citations will be removed. The search strategies will be updated until the end of the review.
Study selection
All records will be independently assessed by two reviewers and reported using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. Following the initial search, titles and abstracts of articles will be screened for eligibility. Second, full texts will be reviewed. As a final step, references will be manually searched for all articles considered to identify relevant reports that were missed in the search strategy. A discussion will be conducted between the reviewers in case of disagreements.
Data collection process
A data extraction form will be designed to extract equivalent information from each study report. From each eligible study, data will be extracted independently and in duplicate by two reviewers. Before starting the review, calibration exercises will be conducted to ensure consistency across reviewers. When data are ambiguous or missing from the published study, we will contact the corresponding authors of the included studies to obtain any key information. Furthermore, we will discuss the potential impact of missing data as a limitation. Data extraction will be independently cross-checked.
Data items
Data collection will include the following items:
-
Study Details:
-
1)
Reviewer: details and ID of the primary reviewer
-
2)
Study ID/ Record number
-
3)
Date when the data extraction will be filled
-
4)
Study title: full title of the study
-
5)
Author’s name,
-
6)
Year of publication
-
7)
Journal in which the article is published
-
1)
-
Study method:
-
1)
Aims of the study
-
2)
Study design (cross-sectional. Cohort, or randomized control trial)
-
3)
Setting (hospital-or community-based)
-
4)
Follow-up or study duration for cohort studies and clinical trials
-
5)
Study population: sample size, mean or median age, age range, sex ratio, inclusion and exclusion criteria of participants
-
6)
Primary outcome: CVI
-
7)
Secondary outcome: genetic diagnosis DEEs
-
1)
-
Covariates: method used to assess CVI, mean or median age at diagnosis of DEEs, proportion of patients without CVI, acquired neurodevelopmental milestones, developmental quotient (DQ) and Intellectual Quotient (IQ).
-
Results:
-
1)
Prevalence estimates (e.g. number of subjects with the disorder, proportion and 95% confidence interval), where prevalence is not directly reported and is feasible, it will be calculated using reported case numbers and sample sizes in individual studies
-
2)
Prevalence estimates of genetic diagnosis of DEEs and CVI will be calculated using reported case numbers divided by the total sample size
-
3)
Author’s comments
-
4)
Reviewer comments.
-
1)
Risk of bias assessment
The “JBI Critical Appraisal Checklist for Studies reporting prevalence data” [27] conceived by the JBI research organization based in the Faculty of Health and Medical Sciences at the University of Adelaide, South Australia will be used to assess the risk of bias in prevalence studies on selected articles. The tool includes 9 questions and the overall appraisal (include, exclude, seek further info). Quality assessment will be undertaken by two reviewers independently. The reviewers will then discuss the results of the critical appraisal for the final appraisal. Disagreements will be resolved by discussion, and a third reviewer may be required.
Data synthesis and meta-analysis
Investigation of heterogeneity
Heterogeneity between studies will be assessed using Cochran’s Q statistic (p > 0.05). In addition, the I2 statistic will be used to measure the percentage of inter-study variability [28]. The value of I2 will be classified as small if 0 < I2 < 25%, medium if 25% < I2 ≤ 50%, and large if I2 > 50% [28]. The category of the I2 statistic will determine whether a meta-analysis is possible.
Characteristics of included studies will be presented in summary tables and narrative text. In expectation of prevalence varying between studies and populations, pooled prevalence estimates for the prespecified outcomes of interest will be calculated by applying a random-effects model [29]. The results will be presented graphically in a forest plot. R software version 3.6.1 (R Core Team, Vienna, Austria) will be used to combine data, along with 95% confidence intervals (95% CI).
If the I2 is large, then a meta-analysis will be considered not possible, and a narrative qualitative summary will be done. The narrative description will include a presentation of the quantitative data reported in individual studies, along with the point and interval estimates for the effects, where available. Otherwise, a meta-analysis will be deemed feasible.
Additional analyses
If more than 10 studies are included in the quantitative synthesis, the potential sources of heterogeneity will be investigated by subgroup and meta-regression analyses [29, 30]. The potential effect modifiers considered will be the following: genetic diagnosis of DEEs, child neurodevelopment, DQ or IQ, or neurodevelopmental regression, seizure onset, type of studies (observational vs experimental), and type of CVI assessments.
We will use the model F value and its statistical significance to assess whether there is evidence for an association between any of the covariates and the outcome; all covariates with p-value < 0.1 in bivariate models will be added to the multivariable model, in which a p-value < 0.05 will be considered statistically significant. The model fit will be assessed using the proportion of the between-study variance explained by the covariates (adjusted R2) [31]. To control for the risk of type I error when performing meta-regression with multiple covariates, we will perform Monte Carlo permutation tests to calculate P values adjusted for type 1 error and we will check if there is a change in statistical significance [32].
Meta-bias(es)
A. Publication bias across studies
If 10 or more eligible studies are found, the symmetry of the funnel chart will be used to assess publication bias, supplemented by quantitative analysis using Egger’s test. The test represents a regression analysis in which the precision of each included study is defined as the independent variable, while the ratio between its effect size and its standard error is the dependent variable. If the test is not statistically significant, it is possible to reject the hypothesis in favour of the presence of a publication bias [33].
B. Sensitivity analyses
The robustness of the results will be assessed by performing sensitivity analyses to measure the impact of low-quality studies (identified through the risk of bias). Low-quality studies will be removed one by one and the meta-analysis will be rerun. We will then compare the results of meta-analyses with and without assessed studies, also considering the study sample size, the strength of evidence, and the impact on aggregated effect size. However, if all included studies are at high risk of bias, no sensitivity analysis will be performed.
Confidence in cumulative estimate
GRADE assessment
The quality of evidence for all outcomes will be judged using the Grading of Recommendations Assessment Development and Evaluation (GRADE) working group methodology [34] as suggested in the literature study on conducting systematic reviews of the literature on the prevalence of a given pathology in a category of individuals [35]. The quality of evidence will be assessed in all areas of risk of bias. Additional domains may be considered where appropriate. Quality will be adjudicated as high, moderate, low or very low [36, 37].
Discussion
The systematic review and meta-analysis presented in this protocol will identify, collect, evaluate and integrate the epidemiological knowledge underlying the prevalence of CVI in patients with DEEs. We are not aware of another systematic review and meta-analysis addressing the specific issue. In our opinion, this systematic review will fill the gap by estimating the pooled global prevalence of CVI in DEE patients useful for understanding the extent of the problem, outlining future research, and suggesting the need for early identification strategies.
The results of this study will be of interest to multiple audiences, including patients, their families, caregivers, clinicians, researchers, scientists, and policymakers.
Scientific communities can better understand how and what to implement in protocols and intervention programs for patients with DEEs by having objective data on the prevalence of this disorder. In addition, this may be useful for the creation of neuro-visual assessment protocols to be used in clinical practices and to incorporate patients into neuro-rehabilitation programs (early intervention) as soon as possible.
Strengths and limitations
The intended systematic review and meta-analysis will fill the knowledge gap on the prevalence of CVI in patients with DEEs. The eligible studies will be identified through a methodical literature search followed by a rigorous screening process; we will then use robust meta-analysis tools to pool the data and provide reliable estimates of the global prevalence of CVI in DEE patients. We anticipate that we will identify knowledge gaps to be filled by new epidemiological research considering that the prevalence of CVI in patients with DEEs has been poorly covered in the literature. In this regard, implications for future epidemiological research will be discussed in the final manuscript.
Conclusions
The purpose of this systematic review is to provide evidence supporting or refuting the hypothesis that CVI is prevalent in a large percentage of patients with DEEs, regardless of genetic diagnosis.
Overall, the review will complement the evidence base on the causes of developmental and epileptic encephalopathies. Similarly, it can provide scientific evidence for a neurovisual assessment protocol that can be validated and then proposed to epilepsy clinics and paediatric neurological departments.
Thus, a patient can be included in an “early intervention” program to prevent and support neuro and psychomotor development, as well as in a precision medicine program to prevent/treat epileptic seizures at the onset.
Availability of data and materials
Not applicable.
Abbreviations
- CDKL5-DEE:
-
CDKL5 Developmental and Epileptic Encephalopathies
- CoCoPop:
-
Condition, Context and Population framework
- CVI:
-
Cerebral Visual Impairment
- DEEs:
-
Developmental and Epileptic Encephalopathies
- DQ:
-
Developmental Quotient
- GRADE:
-
Grading of Recommendations Assessment Development and Evaluation
- ILAE:
-
International League Against Epilepsy
- IQ:
-
Intellectual Quotient
- MeSH:
-
Medical Subject Headings
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
References
Zuberi SM, Wirrell E, Yozawitz E, et al. ILAE classification and definition of epilepsy syndromes with onset in neonates and infants: Position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2020;63(6):1349–97.
Malkowicz DE, Myers G, Leisman G. Rehabilitation of cortical visual impairment in children. Int J Neurosci. 2006Sep;116(9):1015–33.
Fazzi E, Signorini SG, Bova SM, et al. Spectrum of visual disorders in children with cerebral visual impairment. J Child Neurol. 2007;22(3):294–301.
Demarest S, Olson HE, Moss A, et al. CDKL5 Deficiency Disorder: Relationship between genotype, epilepsy, cortical visual impairment and development. Epilepsia. 2019Aug;60(8):1733–42.
Brock D, Fidell A, Thomas J, et al. Cerebral Visual Impairment in CDKL5 Deficiency Disorder Correlates With Developmental Achievement. J Child Nurol. 2021;36(11):974–80.
Olson HE, Costantini JA, Swanson LC, et al. Cerebral visual impairment in CDKL5 deficiency disorder: vision as an outcome measure. Dev Med Child Neurol. 2021;63(11):1308–15.
Quintiliani M, Ricci D, Petrianni M, et al. Cortical Visual Impairment in CDKL5 Deficiency Disorder. Front Neurol. 2022;12:1–8.
Saby JN, Mulcahey PJ, Zavez AE, et al. Electrophysiological biomarkers of brain function in CDKL5 deficiency disorder. Brain. 2022;4:1–15
Olson HE, Demarest ST, Pestana-Knight EM, et al. Cyclin-Dependent Kinase-Like 5 Deficiency Disorder: Clinical Review. Ped Neurol. 2019;97:18–25.
Guzzetta F, Frisone MF, Ricci D, et al. Development of Visual Attention in West Syndrome. Epilepsia. 2002;43(7):757–63.
Randò T, Bancale A, Baranello G, et al. Visual Function in Infants with West Syndrome: Correlation with EEG patterns. Epilepsia. 2004;45(7):781–6.
Guzzetta F, Cioni G, Mercuri E, et al. Neurodevelopmental evolution of West Syndrome: A 2-year prospective study. Eu J Ped Neurol. 2008;12:387–97.
Chieffo D, Ricci D, Baranello G, et al. Early development in Dravet syndrome; visual function impairment precedes cognitive decline. Epilepsy Res. 2011;93:73–9.
Ricci D, Chieffo D, Battaglia D, et al. A prospective longitudinal study on visuo-cognitive development in Dravet syndrome: Is there a “dorsal stream vulnerability”? Epilepsy Res. 2015;109:57–64.
Berg AT, Mahida S, Poduri A, et al. KCNQ2-DEE: developmental or epileptic encephalopathy? ANNALS of Clinical and Translational Neurology. 2021;8(3):666–76.
Helbig KL, Goldberg EM, et al. SCN3A-Related Neurodevelopmental Disorder. In: Adam MP, Everman DB, Mirzaa GM, et al., editors. GeneReviews. Seattle (WA): University of Washington; 2021. p. 1993–2022.
Gardella E, Marini C, Trivisano M, et al. The phenotype of SCN8A developmental and epileptic encephalopathy. Neurology. 2018;91:e1112–24.
Platzer K, Yuan H, Schütz H, et al. GRIN2B encephalopathy: novel findings on phenotype, variant clustering, functional consequences and treatment aspects. J Med Genet. 2017;54(7):460–70.
Inguaggiato E, Sgandurra G, Cioni G. Brain plasticity and early development: Implications for early intervention in neurodevelopmental disorders. Neuropsychiatrie de l’Enfance et de l’Adolescence. 2017;65(5):299–306.
Spolidoro M, Sale A, Berardi N, Maffei L. Plasticity in the adult brain: lessons from the visual system. Exp Brain Res. 2009Jan;192(3):335–41.
Caleo M, Tropea D, Rossi C, et al. Environmental enrichment promotes fiber sprouting after deafferentation of the superior colliculus in the adult rat brain. Exp Neurol. 2009;216(2):515–9.
Sale A, Berardi N, Maffei L. Enrich the environment to empower the brain. Trends Neurosci. 2009Apr;32(4):233–9.
Guzzetta A, Baldini S, Bancale A, et al. Massage accelerates brain development and the maturation of visual function. J Neurosci. 2009;29(18):6042–5.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147–53.
Migliavaca CB, Stein C, Colpani V, et al. Meta-analysis of prevalence: I2 statistic and how to deal with heterogeneity. Res Syn Meth. 2022;13(3):363–7.
von Hippel PT. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:35.
Higgins JPT, Li T. Exploring Heterogeneity. In: Egger M, Higgins JPT, Davey Smith G, editors. In Systematic Reviews in Health Research. 2022.
Miles J. R Squared, Adjusted R Squared. In: Balakrishnan N, Colton T, Everitt B, Piegorsch W, Ruggeri F, Teugels JL, editors. In Wiley StatsRef: Statistics Reference Online. 2014.
Ding D, Gandy A, Hahn G. A simple method for implementing Monte Carlo tests. Comput Stat. 2020;35:1373–92.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed). 2008;336(7650):924–6.
Borges Migliavaca C, Stein C, Colpani V, et al. How are systematic reviews of prevalence conducted? A methodological study. BMC Med Res Methodol. 2020;20:96.
Guyatt GH, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011;64(4):395–400.
Acknowledgements
This work was developed within the Framework of the DINOGMI Department of Excellence of MIUR 2018-2022 (legge 232 del 2016). Research supported by PNRR-MUR-M4C2 PE0000006 Research Program “MNESYS”—A multiscale integrated approach to the study of the nervous system in health and disease. IRCCS ‘G. Gaslini’ is a member of ERN-Epicare.
Funding
The open publication fee was paid by funding 'HUMANITAS MIRASOLE SPA - NET2019' granted to PS.
Author information
Authors and Affiliations
Contributions
M.G.P, M.A conceived and designed the analysis and developed the theoretical framework. M.G.P wrote the protocol. A.R, G.B contributed to the design and implementation of the protocol. M.S.V, E.A worked on the manuscript. S.D, A.V, P.S supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable. No ethical approval is required to conduct this study. Modifications made to this protocol will be outlined and reported in the final manuscript. Results will be disseminated through conference presentations and publication in a peer-reviewed journal. All data underlying the findings reported in the final manuscript will be deposited in a cross-disciplinary public repository.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Perinelli, M.G., Abbott, M., Balagura, G. et al. Prevalence of cerebral visual impairment in developmental and Epileptic Encephalopathies: a systematic review protocol. Syst Rev 13, 223 (2024). https://doi.org/10.1186/s13643-024-02638-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02638-6