Abstract
Background
Mobile health tools have gained prominence in global health care in recent years. Mobile health (mHealth) interventions have demonstrated their impact on managing healthcare service users’ health. A pilot search revealed many systematic reviews on the effectiveness of mobile health tools on service users’ health outcomes. However, how the role of healthcare professionals in promoting the adoption of mobile health may lead to improved outcomes needs to be clarified. Therefore, this systematic review aims to synthesise existing systematic reviews that examine both the impact of mobile health interventions on service users’ outcomes and the role of healthcare professionals in facilitating the adoption of mobile health solutions.
Methods
Five electronic databases will be searched: EMBASE, CINHAL Plus, MEDLINE, Web of Science, and the Cochrane Library for systematic reviews exploring the impact of mobile health interventions on service users’ outcomes and the role of healthcare professionals in facilitating the adoption of mobile health solutions. Systematic reviews published in English dated from January 2015 to June 2024 will be included. Screening and selection of the reviews against inclusion and exclusion criteria will be performed by three independent reviewers, as well as data extraction and quality assessment.
Discussion
Current systematic reviews in mHealth have primarily focused on assessing the effectiveness of mHealth interventions for managing a range of conditions. While these reviews provide valuable input into the outcomes for mHealth, more is needed to know about the impact of the involvement of health professions on service users’ outcomes when adopting mHealth. This systematic review of systematic reviews aims to bridge this critical gap in the literature by critically appraising and synthesising the evidence of mHealth interventions’ impact on service user outcomes and the level of involvement of health professionals.
Systematic review registration
PROSPERO CRD 42023414435.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The exponential growth of chronic diseases and the ageing population worldwide pose increasing challenges to adequate healthcare provision [1]. The crisis of the COVID-19 pandemic has highlighted the practical impact of digital technologies to provide health solutions [2]. Various digital technologies are being developed and used to help in the medical field, including mobile health technology, which has been harnessed in healthcare services [3]. Mobile health (mHealth)involves delivering comprehensive medical and health aid to individuals seeking healthcare via mobile phones, laptops, tablets, and wearable devices [4]. Mobile health technology significantly influences individuals’ health-related behaviours, including physical activity, dietary choices, alcohol consumption, sexual conduct, and adherence to medication regimens [5]. There has been significant growth in the body of literature concerning mHealth over the last decade [6], with the USA and the UK being the most active countries in mHealth research [7]. mHealth interventions are considered powerful tools that have led to revolutionary changes in digital health, particularly in access, monitoring, education, and intervention [8]. For example, a recent systematic review found that mHealth interventions could monitor patients’ conditions remotely, deliver clinical consultation, enhance their engagement, and increase their autonomy in their health management [9].
Furthermore, there is considerable potential for mHealth in various healthcare domains encompassing preventive measures and wellness initiatives, remote and self-diagnostic capabilities, monitoring medication adherence, dissemination of health-related information, and managing chronic diseases [10]. Therefore, mHealth interventions have received recognition and support from global regulatory institutions [11]. For example, the World Health Organisation (WHO) and the National Institute for Health and Care Excellence (NICE) have both acknowledged the potential benefits of mHealth on patient outcomes, disease prevention, and reducing the workload of healthcare providers [12]. The European Commission also described using mHealth as crucial to addressing the healthcare system’s challenges in Europe [13]. In the United Kingdom (UK), National Health Services (NHS) Digital and other organisations have highlighted the importance of mHealth interventions in managing health problems to meet the high public demand for health services [14].
During the outbreak of COVID-19, mHealth significantly impacted the management of health issues. In India, patients’ engagement and utilisation of mHealth increased dramatically during the lockdown [15]. In Brazil, a randomised controlled trial (RCT) found that using mHealth tools to effectively communicate with the public enhanced people’s adherence to preventive measures for COVID-19 [16]. Similarly, in Australia, mHealth interventions were used to provide information about symptoms of COVID-19, prevention, vaccination, and changing behaviour with lifestyle modification for older people [17]. Likewise, other studies worldwide have reported that mHealth technology successfully fought the COVID-19 pandemic [18].
Furthermore, in the UK, the NHS long-term plan (2019–2024) recommends that health professionals be supported to develop digital literacy to use mobile access to digital services. [19]. The latest evidence indicates that integration is crucial, as is assuring the ethical implementation of these technologies [20]. The subsequent steps entail a synthesised methodology that combines innovative elements.
However, the global literature from high-income countries suggests that there is hesitation among health professionals to implement and advocate for the use of digital health technologies in their practice [21,22,23]. This was echoed by a study conducted in Catalonia, which revealed that only 6.5% of the surveyed nurses consistently advocated for integrating digital technology into their regular provision of patient care [24]. Because there is a breadth of literature in digital health, especially in mobile health, this review aims to conduct a systematic review of systematic reviews to assess the current state of evidence on the impact of mHealth adoption on service users’ outcomes and the influence of health professions in the adoption of mHealth on their service users.
Review questions
-
1.
What is the state of the systematic review evidence on interventions designed to influence service user adoption of mobile health to improve health outcomes?
-
2.
What is the state of the systematic review evidence on interventions that are actively attempting to engage health professions to improve service user outcomes with mobile health?
-
3.
Which patient health outcomes are addressed in those reviews of evidence attempting to engage/health professionals when using mobile health?
-
4.
What is the methodological quality of the systematic reviews of evidence of interventions attempting to engage health professionals in using mobile health technology that is explicitly designed to improve service user health outcomes?
Search strategy
An initial scoping search was undertaken to develop the search terms for this review (Table 1). The initial search will combine the search terms across multiple databases. Five electronic databases will be used: EMBASE, CINHAL Plus, MEDLINE, Web of Science, and the Cochrane Library. For a systematic review of systematic reviews, The Joanna Briggs Institute (JBI) recommends searching for research syntheses between 5 and 10 years that will reveal original research from 30 + years ago [25]. Furthermore, da Silva and colleagues undertook a state-of-science review on health in 2015 [26], with further research underpinning the European Green paper [27]. Therefore, the literature search was limited to publications from 2015 to 2023 to identify the most up-to-date and comprehensive breadth of systematic reviews. A revised search will be carried out from January 2023 until June 8, 2024, to incorporate the latest studies.
Study designs
Systematic reviews published in peer-reviewed English language Journals will be included.
Identification of search terms
The following four search terms will be used in this review: health care professional*, digital health, patient care, and systematic review augmented by MESH terms and combined using Boolean logic (Table 1).
Inclusion and exclusion criteria
Studies will be selected based on the following criteria and a list of inclusion and exclusion criteria, as illustrated in Table 2.
Population
This systematic review examines two primary populations: healthcare service users who utilise mobile health (mHealth) tools for managing their health outcomes and healthcare professionals who advocate for using mHealth tools among their service users to enhance health outcomes. This multifaceted focus enables a thorough evaluation of the effects of mHealth interventions on both service users and the involvement of healthcare professionals in promoting the adoption of mHealth. This review excludes studies that focus only on telemedicine or consider mHealth tools only as communication aids among healthcare professionals, as they fall beyond the defined scope of this review.
Intervention
The review will focus on interventions involving mHealth with service users, mHealth interventions measuring service user outcomes, and the engagement of health professionals using mobile health to improve service user outcomes. Systematic reviews not focused on mHealth interventions or service user outcomes will be excluded.
Comparator
This review will focus on mHealth interventions compared with usual care. Usual care can be delivered with non-mobile health technology.
Primary outcomes
The main outcome of this review has two primary outcomes:
-
1.
To assess the impact of mobile health interventions on health-related outcomes of service users. Examples of relevant outcomes may include enhancing service user self-management of wellness and disease prevention and improving their accessibility to health services anxiety, adherence to medications, hospital admission, follow-up, behaviour change, and improving their accessibility to health services.
-
2.
How the role of health professions in promoting the adoption of mobile health influences service users’ health-related outcomes. Examples may include adoption and utilisation rates, service users’ satisfaction and engagement, health literacy and empowerment of health professions, health outcomes for the service users, and the cost-effectiveness of promoting mobile health services by health professionals.
Additional outcomes
Factors affecting service users in adopting mobile health and health professions in promoting mobile health to their service users.
Data exclusion
The characteristics of excluded reviews and reasons for exclusion are listed in a table.
Screening and selection
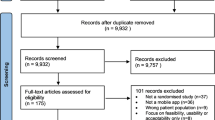
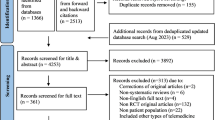
Records were collated, and duplicates were removed using Endnote software. The data will be managed using Microsoft Excel software. A team of four reviewers will review title abstracts and full papers: three reviewers will independently screen the titles, abstracts, and papers, with a third reviewer available for disagreements. The selection process for the papers will be recorded in detail in the PRISMA-P flow diagram [28] as indicated in Fig. 1.
Data extraction
This review will implement a rigorous data extraction procedure to systematically collect and categorise essential data from the included reviews. The purpose of this process is to ensure consistency and accuracy in the analysis. A standardised data extraction form will be developed by the reviewers to provide guidance for the reviewers. To ensure comprehensive and unbiased data extraction, four reviewers will extract the data independently. Interrater reliability will be assessed to ensure consistency. The data extraction process will require a thorough examination of each study included. The data collected from these studies will be organised into tables to enhance clarity and accessibility for further analysis. The following details will be extracted from each study: author names, publication year, journal name, type of systematic review (if applicable), country of origin, range of years covered by the included studies, study settings, quality appraisal tool used, number of included studies, types of health conditions investigated, types of mHealth tools used, intervention descriptions, measured outcomes, and relevant role of health professions. A well-organised and thorough data extraction process is crucial for ensuring transparency, rigour, and reliability in our systematic review. This process ultimately enhances the validity of our research findings.
Data quality assessment
Four reviewers will independently assess the quality of systematic reviews by using AMSTAR 2 (A MeaSurement Tool to Assess Systematic Reviews), and if there are any discrepancies, they will discuss them with the third reviewer. The AMSTAR 2 is a critical appraisal tool to assess the methodological quality of systematic reviews [29]. It is composed of 16 questions, including seven critical domains with an overall rating based on the weaknesses of critical domains. The results of the risk of bias assessment will be documented in the findings and discussion.
Data synthesis
A narrative review will be used to synthesise the findings of systematic reviews to address the review questions. This review will apply thematic analysis to identify main themes and subthemes emerging from the findings based on similarities and differences of mHealth interventions on service users’ outcomes, types of interventions, types of mHealth tools, types of outcomes, the impact of health professions on service users’ outcomes, factors affecting adoption of mHealth by the service users, and factors affecting health professions in promoting the adoption of mHealth among their service users. Thematic analysis will be carried out manually by four independent reviewers. A coding technique will be used to classify and code the identified themes and subthemes. The primary research questions and topics of focus will inform the creation of this framework. The coding process will be progressive, with code reviews occurring at various stages. Periodically throughout the analytic process, intercoder reliability will be evaluated to ensure rigour and consistency. Coding discrepancies will be discussed and resolved at regularly scheduled meetings. Existing themes from the reviews will be discussed with the support of evidence from systematic reviews. Comparisons and contrasts will be highlighted. These findings will be critically analysed, taking into consideration the strengths and limitations of the included reviews. The implications of these findings for clinical practice and the identification of any gaps in the existing reviews will be discussed. The synthesis of the findings will provide recommendations for clinical practice, policy, and future research.
Discussion
Current systematic reviews in mHealth have primarily focused on assessing the effectiveness of mHealth interventions for managing disease conditions. While these reviews provide valuable input into the outcomes of such interventions, more information is needed about the impact of the involvement of health professions on service users’ outcomes when adopting mHealth. This systematic review of systematic reviews aims to bridge this critical gap in the literature by critically appraising and synthesising the evidence of mHealth interventions’ impact on service user outcomes and the level of involvement of health professionals. A recent systematic review and meta-analysis highlighted that mHealth supports health professionals in making clinical decisions, managing and communicating with patients, and monitoring patients remotely [30]. Despite the clear benefits highlighted by various studies, the involvement of health professionals in promoting mHealth to their patients is limited [31, 32]. There is a large body of evidence in the field of mHealth interventions in the field of digital health. Therefore, this review will review the current evidence on mHealth interventions on service user outcomes while providing a unique perspective on the health professions’ influence on mHealth adoption and service user outcomes. This review will contribute significantly to the existing body of knowledge by understanding the role of health professions in guiding health service users towards mHealth solutions, exploring the impact of the involvement of health professions on service users’ outcomes to inform clinical practice, and recommending future research. Additionally, findings from this systematic review of systematic reviews will inform policymakers on policy and framework considerations to enhance the adoption of mHealth interventions into practice.
Availability of data and materials
Not applicable.
Abbreviations
- AMSTAR2:
-
A Measurement Tool to Assess Systematic Reviews
- JBI:
-
The Joanna Briggs Institute
- CINAHL:
-
Cumulative Index to Nursing and Allied Health Literature
- MEDLINE:
-
Medical Literature Analysis and Retrieval System Online
- MeSH:
-
Medical Subject Headings
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- EMBASE:
-
Excerpta Medica database
- PROSPERO:
-
International prospective register of systematic reviews
- NICE:
-
The National Institute for Health and Care Excellence
- WHO:
-
World Health Organisation
- NHS:
-
National Health Service
References
United Nations. Migration and human mobility. http://www.unfpa.org/migration. Accessed 15 Feb 2023.
Willems SH, Rao J, Bhambere S, Patel D, Biggins Y, Guite JW. Digital solutions to alleviate the burden on health systems during a public healthcare crisis: Covid-19 as an opportunity. JMIR mHealth uHealth. 2021;9(6); https://doi.org/10.2196/21127.
Park Y. Emerging new era of mobile health technologies. Healthc Inform Res. 2016;22(4):253. https://doi.org/10.4258/hir.2016.22.4.253.
Aslani N, Lazem M, Mahdavi S, Garavand A. A review of mobile health applications in epidemic and pandemic outbreaks: lessons learned for COVID-19. Arch Clin Infect Dis. 2020;15(4). https://doi.org/10.5812/archcid.103649.
Milne-Ives M, Lam C, De Cock C, Van Velthoven MH, Meinert E. Mobile apps for health behavior change in physical activity, diet, drug and alcohol use, and mental health: systematic review. JMIR mHealth uHealth. 2020;8(3):https://doi.org/10.2196/17046
Cao J, Lim Y, Sengoku S, Guo X, Kodama K, Exploring the shift in international trends in mobile health research from,. to 2020: Bibliometric analysis. JMIR mHealth uHealth. 2000;2021:9. https://doi.org/10.2196/22994.
Ratanawong P, Naslund A, Mikal P, Grande W. Achieving the potential of mHealth in medicine requires challenging the ethos of care delivery. Prim Health Care Res Dev. 2022;23; https://doi.org/10.1017/S1463423622000101.
Osei E, Mashamba-Thompson TP. Mobile health applications for disease screening and treatment support in low-and middle-income countries: A narrative review. Heliyon. 2021;7(3); https://doi.org/10.1016/j.heliyon.2021.e06639.
Kitsiou S, Paré G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: An overview of systematic reviews. PLOS ONE. 2017;12(3) ;https://doi.org/10.1371/journal.pone.0173160.
Sahin C. Rules of engagement in mobile health: What does mobile health bring to research and theory? Contemp Nurse. 2018;54(4–5):374–87. https://doi.org/10.1080/10376178.2018.1448290.
Wang Y, Wu T, Chen Z. Active usage of mobile health applications: cross-sectional study. J Med Internet Res. 2021;23(12) ;https://doi.org/10.2196/25330.
Lucivero F, Jongsma R. A mobile revolution for healthcare? setting the agenda for bioethics. J Med Ethics. 2018;44(10):685–9. https://doi.org/10.1136/medethics-2017-104741.
Commission E. GREEN PAPER on mobile health (“mHealth”) COM 219. Brussels: European Commission; 2014.
Chidambaram S, Erridge S, Kinross J, Purkayastha S. Observational study of UK mobile health apps for covid-19. Lancet Digit Health. 2020;2(8):90. https://doi.org/10.1016/S2589-7500(20)30144-8.
Rathi S, Chakrabarti AS, Chatterjee C, Hegde A. Pandemics and technology engagement: new evidence from m-Health intervention during Covid-19 in India. Rev Dev Econ. 2022;26(4):2184–217. https://doi.org/10.1111/rode.12872.
Boruchowicz C, López Bóo F, Finamor Pfeifer F, Russo GA, Souza Pacheco T. Are behaviorally informed text messages effective in promoting compliance with covid-19 preventive measures?: evidence from an RCT in the city of São Paulo. 2021-IDB-TN; https://doi.org/10.18235/0002722.
Abbaspur-Behbahani S, Monaghesh E, Hajizadeh A, Fehresti S. Application of mobile health to support the elderly during the COVID-19 outbreak: a systematic review. Health Policy Technol. 2022;11(1): 100595. https://doi.org/10.1016/j.hlpt.2021.100595.
Alkhaldi O, McMillan B, Maddah N, Ainsworth J. Interventions aimed at enhancing healthcare providers’ behavior toward the prescription of mobile health apps: Systematic review. JMIR mHealth uHealth. 2023;11; https://doi.org/10.2196/40416.
The NHS Long Term Plan. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf. Accessed 09 Aug 2023.
Albulushi A, Al Kindi D, Moawwad N, Kamel A, Khan A, Moustafa M, Al KA. Digital health technologies in enhancing patient and caregiver engagement in heart failure management: opportunities and challenges. Int J Cardiol. 2024;408: 132116. https://doi.org/10.1016/j.ijcard.2024.132116.
Slevin P, Kessie T, Cullen J, Butler MW, Donnelly SC, Caulfield B. Exploring the barriers and facilitators for the use of digital health technologies for the management of COPD: a qualitative study of clinician perceptions. QJM. 2019;112(8):567–73. https://doi.org/10.1093/qjmed/hcz241.
El Amrani L, Oude Engberink A, Ninot G, Hayot M, Carbonnel F. Connected health devices for healthcare in French general medicine practice: Cross-sectional study. JMIR mHealth uHealth. 2017;5(12); https://doi.org/10.2196/mhealth.7427.
Safi S, Thiessen T, Schmailzl KJ. Acceptance and resistance of new digital technologies in medicine: qualitative study. JMIR Res Protoc. 2018;7(12) ;https://doi.org/10.2196/11072.
Mayer A, Rodríguez Blanco O, Torrejon A. Use of health apps by nurses for professional purposes: Web-based survey study. JMIR mHealth uHealth. 2019;7(11); https://doi.org/10.2196/15195.
Joanna Briggs Institute. The systematic review of economic evaluation evidence. https://jbi.global/. Accessed 22 May 2023.
Silva B, Rodrigues G, Díez I, López-Coronado M, Saleem K. Mobile-health: Review of current state in 2015. J Biomed Inform. 2015;56:265–72. https://doi.org/10.1016/j.jbi.2015.06.003.
Commission E. Mobile health reconciling technological innovation with data protection. Brussels: European Commission; 2015.
Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7); https://doi.org/10.1371/journal.pmed.1000097.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358; https://doi.org/10.1136/bmj.j4008.
Rowland SP, Fitzgerald JE, Holme T, Powell J, McGregor A. What is the clinical value of mHealth for patients? NPJ Digit Med. 2020;3:4. https://doi.org/10.1038/s41746-019-0206-x.
Leigh S, Ashall-Payne L, Andrews T. Barriers and facilitators to the adoption of mobile health among healthcare professionals from the United Kingdom: Discrete choice experiment. JMIR mHealth uHealth. 2020;8(7)https://doi.org/10.2196/17704.
Gagnon M, Ngangue P, Payne-Gagnon J, Desmartis M. m-Health adoption by healthcare professionals: a systematic review. J Am Med Inform Assoc. 2016;23:212–20. https://doi.org/10.1093/jamia/ocw084.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
FA assisted in conceiving the study, carried out search strategies, participated in the design and coordination of the study, and drafted the study manuscript. CBW helped conceive the study, participated in the design and coordination of the study, and revised the manuscript critically. DR participated in the design and was involved in revising the manuscript. JB participated in the critical appraisal of the reviews and in revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alkhuzaimi, F., Rainey, D., Wilson, C.B. et al. The impact of mobile health interventions on service users’ health outcomes and the role of health professions: a systematic review of systematic reviews—protocol. Syst Rev 13, 199 (2024). https://doi.org/10.1186/s13643-024-02624-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02624-y