Abstract
Background
Patients with heart failure with preserved ejection fraction (HFpEF) commonly experience exercise intolerance, resulting in reduced cardiorespiratory fitness. This is characterised by a decreased maximal oxygen uptake (V̇O2peak), which is determined by the product of cardiac output (CO) and arteriovenous oxygen difference (a-vDO2). While exercise training has been shown to improve V̇O2peak in HFpEF patients, the effects on CO remain unclear. The aim of this study is to systematically review and analyse the current evidence on the effects of supervised exercise training on CO in patients with HFpEF.
Methods
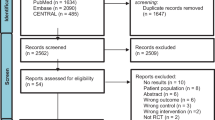
We will systematically search for literature describing the effects of supervised exercise training on CO in patients with HFpEF. All eligible studies published before 30 June 2023 in the following electronic databases will be included: MEDLINE (Ovid), Embase (Ovid), SPORTDiscus (EBSCOhost), and CENTRAL (Cochrane Library). Effect sizes will be extracted for CO before and after a supervised exercise training intervention at rest and maximal exercise. Mass of heterogeneity (I2) will be calculated, and either fixed-effect models or random-effect models will be used for meta-analysis. To detect a potential publication bias, funnel plot analyses will be performed.
Discussion
While several studies have reported a positive effect of supervised exercise training on cardiorespiratory fitness, attempts to assess the underlying determinants of V̇O2peak, CO, and a-vDO2 are much scarcer, especially in patients with HFpEF. From a physiological perspective, measuring CO before and after supervised exercise training seems to be a reasonable way to accurately operationalise a potential improvement in cardiac function.
Systematic review registration
PROSPERO CRD42022361485.
Similar content being viewed by others
Strengths and limitations of this study
-
To the best of our knowledge, this is the first protocol planning to calculate the pooled effect estimate of supervised exercise training on CO in patients with HFpEF.
-
By focusing on the specific physiological parameter CO, the systematic review will provide valuable insights into the impact of exercise training on cardiovascular function.
-
A possible limitation will be the inclusion of studies written in English, French, and German only.
-
A second possible limitation will be the possible heterogeneity in exercise training interventions. Variations in exercise duration, intensity, and frequency may have an impact on comparability and generalisability of the results.
Introduction
Heart failure with preserved ejection fraction (HFpEF) is estimated to be prevalent in approximately 50% or more of individuals diagnosed with heart failure (HF) [1, 2]. It is defined as left ventricular ejection fraction > 50%, elevated levels of brain natriuretic peptides, objective evidence of structural heart disease or diastolic dysfunction [3], and associated with increased mortality, and health care expenditures [4]. A key characteristic of HFpEF is reduced cardiorespiratory fitness, defined as the maximal oxygen uptake (V̇O2peak) [4]. V̇O2peak is the product of two main determinants: cardiac output (CO) and arteriovenous oxygen difference (a-vDO2). CO is the product of the heart rate (HR), the number of heart beats per minute, and the stroke volume (SV; the volume of blood pumped from the ventricle per beat). CO and a-vDO2 (and consequently V̇O2peak) are limited [5]. Nevertheless, in supervised exercise training studies, only the two markers V̇O2peak and peak power output are usually reported [6], but neither CO nor a-vDO2.
While several studies have investigated the physiological mechanism underlying the reduced V̇O2peak in patients with HF with reduced ejection fraction (HFrEF) [7,8,9], considerably, less is known about the mechanism in patients with HFpEF [10]. Although several studies have demonstrated that exercise training improves V̇O2peak in patients with HFpEF [11,12,13,14,15], less is known about the effect of exercise training on CO in patients with HFpEF. Abudiab et al. showed that reduced cardiorespiratory fitness is associated with an insufficient CO in relation to metabolic demand [16]. In contrast, Haykowsky et al. reported that increased a-vDO2 is primarily contributing to improved V̇O2peak in patients with HFpEF, while SV and CO were not significantly altered after 16 weeks of endurance training [17]. Similar to these results, Fu et al. demonstrated that improvement in V̇O2peak with high-intensity interval training was associated with an improved a-vDO2. However, maximal HR, SV index, and cardiac index remained unchanged after training [18].
On a general note, the improvement in exercise capacity is mainly operationalised with V̇O2peak, which does not provide clear indications of training effects on direct cardiac function like CO. As there is still a lack of understanding concerning adaption processes in patients with HFpEF, a thorough examination of the effect of supervised exercise training on CO at rest and maximal exercise is crucial and will assist the development of valuable therapeutic recommendations [19].
Furthermore, existing reviews have focused on parameters such as the ratio of peak early to late mitral inflow velocities (E/A ratio), the ratio of early diastolic mitral inflow to annular velocities (E/E’ ratio), or changes in left ventricular ejection fraction during resting conditions. These reviews and meta-analyses contributed significantly to the understanding of HFpEF pathophysiology [20,21,22,23,24,25,26].
However, our review aims to specifically examine the impact of exercise training on cardiac output at rest and during exercise in patients with HFpEF. By exploring the dynamic changes in cardiac output during exercise, our review seeks to elucidate novel insights into the pathophysiology of HFpEF. We believe that this approach will provide a comprehensive understanding of the physiological response to exercise in HFpEF, thereby advancing the current knowledge base in this field.
Why it is important to do this review
Given the limited success of medical treatments in improving prognosis for patients with HFpEF [27,28,29] and the current therapeutic approaches primarily focused on relieving HF symptoms [19], it is crucial to better understand the effects of exercise training on V̇O2peak and the underlying determinants CO and a-vDO2.
Therefore, to enhance the design of future studies and pinpoint therapeutic targets, a more comprehensive understanding of the basic mechanisms contributing to V̇O2 limitation in HFpEF is crucial [16].
This review is also important because it is still not clear which exercise intensity is best to improve the cardiorespiratory fitness in patients with HFpEF. Wisløff et al. (2007) demonstrated that high-intensity interval training (HIIT) was superior to moderate continuous training (MCT) in terms of improving cardiorespiratory fitness in heart failure patients [30]. Later, smaller studies were able to confirm these findings in patients with HFpEF [11, 12], but the recently published OptimEx study refuted previous findings and did not find superiority of HIIT compared to MCT in patients with HFpEF [31]. In order to determine which training protocol or exercise training is superior to another, an improvement in V̇O2peak has often been considered as the crucial factor. It would, however, be beneficial to also obtain more information regarding the improvement of CO, as it is a critical determinant of exercise performance, and there is no consensus yet about the superior training protocol [11, 12, 31].
Furthermore, to the best of our knowledge, there is currently no systematic review and meta-analysis focusing on the effects of exercise training on CO in HFpEF. Therefore, reviewing and meta-analysing the literature to identify studies measuring CO in patients with HFpEF are a first step to determine whether exercise can improve CO, potentially assisting in the development of valid therapeutic recommendations for patients with HFpEF.
Aim and review question
This study aims at systematically reviewing and meta-analysing the literature on effects of exercise training on CO in patients with HFpEF. As hypothesis with potential falsification, it shall be stated that an exercise training intervention as compared to standard of care has no effect on CO.
Material and methods
This systematic review protocol is reported according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) [32]. The protocol was submitted for registration in International Prospective Register of Systematic Reviews (PROSPERO) on 20 September 2022 and registered on 5 October 2022 (registration number CRD42022361485). The research question was formulated according to PICOS (Population, Intervention, Comparison, Outcome, Study type) framework (Table 1) with the aim of capturing the current evidence regarding the impact of exercise compared to standard care on the difference in CO from pre-to post-intervention.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Study eligibility criteria
Given the variability and challenge associated with the diagnosis of HFpEF [33], we have defined HFpEF by the following signs and symptoms: left ventricular ejection fraction > 50%, elevated levels of brain natriuretic peptides (BNP > 35 pg·ml−1 or NTproBNP > 125 pg·ml−1), objective evidence of structural heart disease, or diastolic dysfunction usually provided by echocardiography [3], without acute or severe coronary, valvular, or pulmonary disease that could mimic HF symptoms.
It is acknowledged that there might be diversity within the study populations concerning the definition of HFpEF. Therefore, we intend to provide a detailed description and discussion of the different definitions of HFpEF in the manuscript.
Inclusion criteria
-
All studies investigating the effect of a supervised exercise training on CO in patients with HFpEF.
-
All clinical studies, which were published until the date of the last search and have the design of a randomised controlled trial (with standard care applied to a control group)
-
Studies measuring CO or SV at rest before and after a supervised exercise training
-
All forms of supervised exercise training that can be considered having more than a single training session.
Exclusion criteria
-
Studies reporting estimated CO
-
Studies published in languages other than English, German, and French
-
Study designs other than randomised controlled trial or non-original articles (for example editorials, letters, reviews), meta-analyses, case reports, and conference abstracts
Information sources and search strategy
Search strategies were developed in collaboration with an information specialist (C. A.-H.) using the Peer Review of Electronic Search Strategies framework [34]. We will search MEDLINE (Ovid), Embase (Ovid), SPORTDiscus (EBSCOhost), and CENTRAL (Cochrane Library) for randomised controlled trials using database-specific subjects headings and text-word synonyms around the concepts HFpEF, exercise training, and CO. Nonhuman studies and conference abstracts will be excluded. The detailed search strings can be found in online supplemental document.
To complement the results of database searching, the bibliographic references and citing articles of all included articles will be collected from citationchaser, Scopus, and the Web of Science, deduplicated and screened for eligibility (backward and forward citation searching).
Study records: data management, selection process, and data collection
Studies were imported into EndNote (version 21), to remove duplicates, and then entered into Rayyan [35] for the screening process. The titles and abstracts of retrieved records will be reviewed independently by two authors (P. B. and R. S.). Articles will be categorised as ‘include’,’exclude’, or ‘uncertain’ based on the prespecified eligibility criteria. For articles categorized as ‘include’ or ‘uncertain’, the full text will be retrieved and independently reviewed for eligibility by two authors (P. B. and R. S.). Any discrepancies during title/abstract or full-text screening will be resolved through discussion between the two screening authors. If no resolution can be found, a third party (B.) will make the final judgement. Data will be extracted from the full texts and entered into a standardised Excel form. One author will extract the data (B. G.), and a second author will independently check the extractions (R. S.). Any discrepancies will be resolved through discussion, involving a third party (A. S. T.) if necessary. Corresponding authors will be contacted twice via email in case of any missing or unclear data. Publications will be excluded from meta-analysis if there is no response or if the required data cannot be provided. The data to be extracted are shown in Table 2. If there are more than two assessment time points (beyond pre-post), the initial assessment and the one closest to the end of the intervention will be considered.
Outcome and prioritisation
The primary outcome evaluated in this study is the difference in CO levels at rest and under peak power from before to after a supervised exercise training in subjects with HFpEF.
Risks-of-bias (quality) assessment
The risk of bias at study level will be assessed using the RoB 2 tool by two authors independently (P. B. and R. S.) [36]. Discrepancies will be resolved through discussion (or with a third party, if necessary, AST).
Data synthesis
Standard mean differences (SMD) at the study level will be calculated as the difference in mean change of CO before versus after exercise training or standard care for the control group. SMD will be interpreted as small d = 0.2, moderate d = 0.5, or large d ≥ 0.8. Furthermore, to detect the effect of exercise training, we will compare and meta-analyse the pre- versus post-differences in CO in the exercise training group and the control group by calculating a pooled SMD. Cochran’s Q statistic will be calculated, providing a measure of the variance between the SMD (with p < 0.05 indicating evidence for heterogeneity), while I2 provides a measure of the amount of variance between studies in terms of heterogeneity (with I2 > 50% indicating substantial heterogeneity) [37, 38]. Thereby, heterogeneity variance shall be estimated using restricted maximum likelihood method (REML). If study heterogeneity is substantial (I2 > 50%), random-effect models shall be used for meta-analysis of SMD (otherwise fixed-effect models). Statistical analyses will be conducted using Review Manager software (version 5.3, Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration 2014) and R (version 4.1.1) [39].
Additional analysis
No additional analyses will be conducted.
Meta-bias(es)
If 10 or more studies will be found, funnel plots according to Egger will be calculated to detect a potential publication bias [40].
Certainty of cumulative evidence
The certainty of evidence will be evaluated with the Grading of Recommendations Assessment, Development and Evaluation system, which is a tool classifying evidence into one of four categories ranging from very low to high [41].
Ethics and dissemination
The present work is a systematic review and meta-analysis protocol. No human participants will be involved; therefore, no ethics approval is required. It is planned to communicate the study results in a peer-reviewed journal and as a conference presentation.
Conclusion
The aim of this systematic review and meta-analysis is to investigate the effects of supervised exercise training on CO in patients with HFpEF.
This research is of utmost importance because current exercise training interventions primarily focus on improving V̇O2peak, while the impact on CO, a critical determinant of exercise performance, remains largely unknown, and CO is crucial for understanding exercise intolerance in patients with HFpEF.
The systematic review and meta-analysis aims to address this knowledge gap and determine whether supervised exercise training has an effect on CO in patients with HFpEF in order to achieve a potential improvement of the therapeutic recommendations in the future.
Availability of data and materials
All data will be included in the final published systematic review and meta-analysis article.
Abbreviations
- a-vDO2 :
-
Arteriovenous oxygen difference
- BMI:
-
Body mass index
- BNP:
-
Brain natriuretic peptides
- CO:
-
Cardiac output
- CPET:
-
Cardiopulmonary exercise testing
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- HIIT:
-
High-intensity interval training
- HR:
-
Heart rate
- MCT:
-
Moderate continuous training
- NTproBNP:
-
N-terminal pro-B-type natriuretic peptide
- PRISMA-P:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- RCT:
-
Randomised controlled trial
- REML:
-
Restricted maximum likelihood
- SMD:
-
Standard mean difference
- SV:
-
Stroke volume
- V̇O2peak :
-
Maximal oxygen uptake
References
Maeder MT, Kaye DM. Heart failure with normal left ventricular ejection fraction. J Am Coll Cardiol. 2009;53(11):905–18.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Haykowsky MJ, Kitzman DW. Exercise physiology in heart failure and preserved ejection fraction. Heart Fail Clin. 2014;10(3):445–52.
Fu Q, Levine BD. Exercise and the autonomic nervous system. Handb Clin Neurol. 2013;117:147–60.
Gasser BA, Boesing M, Schoch R, Brighenti-Zogg S, Kröpfl JM, Thesenvitz E, et al. High-intensity interval training for heart failure patients with preserved ejection fraction (HIT-HF)-rational and design of a prospective, randomized, controlled trial. Front Physiol. 2021;12: 734111.
Esposito F, Mathieu-Costello O, Shabetai R, Wagner PD, Richardson RS. Limited maximal exercise capacity in patients with chronic heart failure: partitioning the contributors. J Am Coll Cardiol. 2010;55(18):1945–54.
Sullivan MJ, Knight JD, Higginbotham MB, Cobb FR. Relation between central and peripheral hemodynamics during exercise in patients with chronic heart failure. Muscle blood flow is reduced with maintenance of arterial perfusion pressure. Circulation. 1989;80(4):769–81.
Wilson JR, Mancini DM, Dunkman WB. Exertional fatigue due to skeletal muscle dysfunction in patients with heart failure. Circulation. 1993;87(2):470–5.
Haykowsky MJ, Brubaker PH, John JM, Stewart KP, Morgan TM, Kitzman DW. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. J Am Coll Cardiol. 2011;58(3):265–74.
Angadi SS, Mookadam F, Lee CD, Tucker WJ, Haykowsky MJ, Gaesser GA. High-intensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: a pilot study. J Appl Physiol (1985). 2015;119(6):753–8.
da Donelli Silveira A, de Beust Lima J, da Silva Piardi D, Dos Santos Macedo D, Zanini M, Nery R, et al. High-intensity interval training is effective and superior to moderate continuous training in patients with heart failure with preserved ejection fraction: a randomized clinical trial. Eur J Prev Cardiol. 2020;27(16):1733–43.
Edelmann F, Gelbrich G, Düngen HD, Fröhling S, Wachter R, Stahrenberg R, et al. Exercise training improves exercise capacity and diastolic function in patients with heart failure with preserved ejection fraction: results of the Ex-DHF (Exercise training in Diastolic Heart Failure) pilot study. J Am Coll Cardiol. 2011;58(17):1780–91.
Kitzman DW, Brubaker PH, Morgan TM, Stewart KP, Little WC. Exercise training in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. Circ Heart Fail. 2010;3(6):659–67.
Smart NA, Haluska B, Jeffriess L, Leung D. Exercise training in heart failure with preserved systolic function: a randomized controlled trial of the effects on cardiac function and functional capacity. Congestive heart failure (Greenwich, Conn). 2012;18(6):295–301.
Abudiab MM, Redfield MM, Melenovsky V, Olson TP, Kass DA, Johnson BD, Borlaug BA. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail. 2013;15(7):776–85.
Haykowsky MJ, Brubaker PH, Stewart KP, Morgan TM, Eggebeen J, Kitzman DW. Effect of endurance training on the determinants of peak exercise oxygen consumption in elderly patients with stable compensated heart failure and preserved ejection fraction. J Am Coll Cardiol. 2012;60(2):120–8.
Fu TC, Yang NI, Wang CH, Cherng WJ, Chou SL, Pan TL, Wang JS. Aerobic interval training elicits different hemodynamic adaptations between heart failure patients with preserved and reduced ejection fraction. Am J Phys Med Rehabil. 2016;95(1):15–27.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Lin B, Siskin M, Wang B, Natarajan S. Does exercise training improve exercise tolerance, quality of life, and echocardiographic parameters in patients with heart failure with preserved ejection fraction? A systematic review and meta-analysis of randomized controlled trials. Heart Fail Rev. 2023;28(4):795–806.
Edwards JJ, O’Driscoll JM. Exercise training in heart failure with preserved and reduced ejection fraction: a systematic review and meta-analysis. Sports Medicine - Open. 2022;8(1):76.
Zhuang C, Luo X, Wang Q, Wang W, Sun R, Zhang X, Yu J. The effect of exercise training and physiotherapy on diastolic function, exercise capacity and quality of life in patients with heart failure with preserved ejection fraction: a systematic review and meta-analysis. Kardiol Pol. 2021;79(10):1107–15.
Fukuta H, Goto T, Wakami K, Kamiya T, Ohte N. Effects of exercise training on cardiac function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Fail Rev. 2019;24(4):535–47.
Chan E, Giallauria F, Vigorito C, Smart NA. Exercise training in heart failure patients with preserved ejection fraction: a systematic review and meta-analysis. Monaldi Arch Chest Dis. 2016;86(1–2):759.
Dieberg G, Ismail H, Giallauria F, Smart NA. Clinical outcomes and cardiovascular responses to exercise training in heart failure patients with preserved ejection fraction: a systematic review and meta-analysis. J Appl Physiol (1985). 2015;119(6):726–33.
Pandey A, Parashar A, Kumbhani D, Agarwal S, Garg J, Kitzman D, et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ Heart Fail. 2015;8(1):33–40.
Burkhoff D. Mortality in heart failure with preserved ejection fraction: an unacceptably high rate. Eur Heart J. 2012;33(14):1718–20.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet (London, England). 2012;380(9851):1387–95.
Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115(24):3086–94.
Mueller S, Winzer EB, Duvinage A, Gevaert AB, Edelmann F, Haller B, et al. Effect of high-intensity interval training, moderate continuous training, or guideline-based physical activity advice on peak oxygen consumption in patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2021;325(6):542–51.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Pieske B, Tschöpe C, de Boer RA, Fraser AG, Anker SD, Donal E, et al. How to diagnose heart failure with preserved ejection fraction: the HFA–PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019;40(40):3297–317.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
BMJ Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327(7414):557–60.
Langan D, Higgins JPT, Simmonds M. Comparative performance of heterogeneity variance estimators in meta-analysis: a review of simulation studies. Research synthesis methods. 2017;8(2):181–98.
R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2021.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed). 1997;315(7109):629–34.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed). 2008;336(7650):924–6.
Acknowledgements
Not applicable.
Funding
Open access funding provided by University of Basel This study was supported by the Swiss National Science Foundation (Grant number: 185217) and the Department of Sport, Exercise and Health of the University of Basel, Division of Sports and Exercise Medicine, Switzerland.
Author information
Authors and Affiliations
Contributions
BG and RS conceptualised the study. CA-H and RS designed the search string. BG and RS wrote the protocol. AST, CA-H, and PB critically revised it. CA-H was responsible for the search strategy. CA-H and BG designed the data synthesis strategy. BG registered the protocol in PROSPERO. PB and RS will conduct the systematic review and BG and RS the meta-analysis. The final manuscript will be written by BG and RS. All authors read and approved the final protocol.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Schoch, R., Gasser, B., Beck, P. et al. Effects of exercise training on cardiac output in subjects with heart failure with preserved ejection fraction (HFpEF) — a protocol for a systematic review and meta-analysis. Syst Rev 13, 159 (2024). https://doi.org/10.1186/s13643-024-02529-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02529-w