Abstract
Background
Intravenous (IV) medication is commonly administered and closely associated with patient safety. Although nurses dedicate considerable time and effort to rate the control of IV medications, many medication errors have been linked to the wrong rate of IV medication. Further, there is a lack of comprehensive studies examining the literature on rate control of IV medications. This study aimed to identify the attributes of errors, facilitators, and barriers related to rate control of IV medications by summarizing and synthesizing the existing literature.
Methods
This scoping review was conducted using the framework proposed by Arksey and O’Malley and PRISMA-ScR. Overall, four databases—PubMed, Web of Science, EMBASE, and CINAHL—were employed to search for studies published in English before January 2023. We also manually searched reference lists, related journals, and Google Scholar.
Results
A total of 1211 studies were retrieved from the database searches and 23 studies were identified from manual searches, after which 22 studies were selected for the analysis. Among the nine project or experiment studies, two interventions were effective in decreasing errors related to rate control of IV medications. One of them was prospective, continuous incident reporting followed by prevention strategies, and the other encompassed six interventions to mitigate interruptions in medication verification and administration. Facilitators and barriers related to rate control of IV medications were classified as human, design, and system-related contributing factors. The sub-categories of human factors were classified as knowledge deficit, performance deficit, and incorrect dosage or infusion rate. The sub-category of design factor was device. The system-related contributing factors were classified as frequent interruptions and distractions, training, assignment or placement of healthcare providers (HCPs) or inexperienced personnel, policies and procedures, and communication systems between HCPs.
Conclusions
Further research is needed to develop effective interventions to improve IV rate control. Considering the rapid growth of technology in medical settings, interventions and policy changes regarding education and the work environment are necessary. Additionally, each key group such as HCPs, healthcare administrators, and engineers specializing in IV medication infusion devices should perform its role and cooperate for appropriate IV rate control within a structured system.
Similar content being viewed by others
Background
Medication errors are closely associated with patient safety and the quality of care [1, 2]. In particular, medication errors, which denote a clinical issue of global importance for patient safety, negatively affect patient morbidity and mortality and lead to delays in discharge [3, 4]. The National Health Service in the UK estimates that 237 million medication errors occur each year, of which 66 million cause clinically significant harm [5]. The US Food and Drug Administration reported that they received more than 100,000 reports each year associated with suspected medication errors [6]. Additionally, it was estimated that 40,000–98,000 deaths per year in the USA could be attributed to errors by healthcare providers (HCPs) [7]. Previous studies have revealed that medication errors account for 6–12% of hospital admissions [8].
Intravenous (IV) medication is a common treatment in hospitalized patient care [9]. It is used in wards, intensive care units (ICUs), emergency rooms, and outpatient clinics in hospitals [9, 10]. As direct HCPs, nurses are integral in patient safety during the IV medication process which could result in unintended errors or violations of recommendations [3]. As many drugs injected via the IV route include high-risk drugs, such as chemotherapy agents, insulin, and opioids [10], inappropriate dose administration could lead to adverse events (AEs), such as death and life-threatening events [11, 12].
IV medication process is a complex and multistage process. There are 12 stages in the IV medication process, which can be classified as follows: (1) obtain the drug for administration, (2) obtain the diluent, (3) reconstitute the drug in the diluent, (4) take the drug at the patient’s bedside, (5) check for the patient’s allergies, (6) check the route of drug administration, (7) check the drug dose, (8) check the patency of the cannula, (9) expel the air from the syringe, (10) administer the drug, (11) flush the cannula, and (12) sign the prescription chart [13]. IV medication errors can occur at any of these stages. It is imperative to administer the drug at the correct time and rate during the IV medication process [13]. The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) defined an error in IV medication rates as “too fast or too slow rate than that intended” [14]. Maintaining the correct rate of IV medication is essential for enhancing the effectiveness of IV therapy and reducing AEs [9].
Infusion pumps are devices designed to improve the accuracy of IV infusions, with drug flow, volume, and timing programmed by HCPs [15]. A smart pump is an infusion pump with a software package containing a drug library. During programming, the smart pump software warns users about entering drug parameters that deviate from the recommended parameters, such as the type, dose, and dosage unit of the drug [15]. In the absence of a device for administering IV medication, such as an infusion pump or smart pump, the IV rate is usually controlled by counting the number of fluid drops falling into the drip chamber [9].
According to the previous study, applying an incorrect rate was the most prevalent IV medication error, accounting for 536 of 925 (57.9%) total IV medication errors [16]. Although rate control of IV medications is critical to patient safety and quality care, few studies review and map the relevant literature on rate control of IV medications. Therefore, this study aimed to identify the attributes of errors, facilitators, and barriers related to rate control of IV medications by summarizing the existing literature.
The specific research questions of this study are as follows:
-
1)
What are the general characteristics of the studies related to rate control of IV medications?
-
2)
What are the attributes of errors associated with rate control of IV medications?
-
3)
What are the facilitators and barriers to rate control of IV medications?
Methods
This scoping review followed the framework suggested by Arksey and O’Malley [17] and developed by Levac et al. [18] and Peters et al. [19]. Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) developed in 2020 by the Joanna Briggs Institute (JBI) were used to ensure reliability in the reporting of methodology (Additional file 1) [19].
Search strategy
According to the JBI Manuals for Evidence Synthesis, a three-step search strategy was adopted [19]. First, a preliminary search in PubMed was conducted based on the title, abstract, keywords, and index terms of articles to develop our search strategy. In the preliminary search, we used keywords such as “patients,” “nurse,” “IV therapy,” “monitoring,” “rate,” and “medication error.” The search results indicated that studies on medical devices and system-related factors were excluded. Therefore, we decided to exclude the keywords “patients” and “nurse” and focus on “IV therapy,” “monitoring,” “rate,” and “medication error” to comprehensively include studies on factors associated with rate control of infusion medications. Secondly, we used all identified keywords and index terms across all included databases following consultations with a research librarian at Yonsei University Medical Library to elaborate our search strategy. Four databases—PubMed, CINAHL, EMBASE, and Web of Science—were searched using the keywords, index terms, and a comprehensive list of keyword variations to identify relevant studies published before January 2023. The details of the search strategy are described in Additional file 2. All database search results were exported into Endnote version 20. Finally, we manually searched the reference lists of the included articles identified from the database search. Furthermore, we manually searched two journals related to medication errors and patient safety, and Google Scholar to comprehensively identify the relevant literature. When performing a search on Google Scholar, keywords such as “medication,” “rate,” “IV therapy,” “intravenous administration,” and “medication error” were appropriately combined using search modifiers.
Eligibility criteria
Inclusion criteria were established according to the participants, concept, and context (PCC) framework recommended by the JBI manuals for scoping reviews [19]. The participants include patients receiving IV therapy, HCPs involved in administering IV medications, and experts from non-healthcare fields related to rate control of IV medications. The concepts were facilitators and barriers to rate control of IV medications, and the contexts were the environments or situations in which errors in rate control of IV medications occurred. While screening the literature identified by the three-step search based on the inclusion criteria, we refined the exclusion criteria through discussion among researchers. The exclusion criteria were as follows: (1) not available in English, (2) not an original article, (3) studies of medication errors in general, (4) not accessible, or (5) prescription error.
Study selection
Once duplicates were automatically removed through Endnote, two independent researchers assessed the eligibility of all articles by screening the titles and abstracts based on the inclusion and exclusion criteria. Studies identified via database searches were screened by GWR and YK and studies identified via other methods were screened by SBY and YK. Full-text articles were obtained either when the studies met the inclusion criteria or when more information was needed to assess eligibility and the researchers independently reviewed the full-text articles. In case of any disagreement in the study selection process, a consensus was reached through discussion among three researchers (GWR, SBY, and YK) and a senior researcher (JP).
Data extraction
Through consensus among the researchers, a form for data extraction was developed to extract appropriate information following the JBI manuals for scoping reviews [19]. The following data were collected from each study: author information, publication year, country, study design, study period, aims, participants or events (defined as the occurrences related to patient care focused on in the study), contexts, methods, errors related to the control of IV medications (observed results or intervention outcomes), error severity, facilitators, and barriers according to the NCC MERP criteria. Three researchers (GWR SBY, and YK) independently conducted data charting and completed the data extraction form through discussion.
Data synthesis
The general characteristics of included studies such as publication year, country, study design, and study period were analyzed using descriptive statistics to identify trends or patterns. The aims, participants, events, contexts, and methods of the included studies were classified into several categories through a research meeting including a senior researcher (JP) to summarize and analyze the characteristics of the included studies comprehensively. Attributes of errors associated with rate control of IV medications were analyzed and organized through consensus among researchers based on extracted data. Facilitators and barriers to rate control of IV medications were independently classified according to NCC MERP criteria by three researchers (GWR, SBY, and YK) and iteratively modified. Discrepancies were resolved by discussion and re-reading the articles, with the final decision made in consultation with the senior researcher (JP).
Results
Study selection
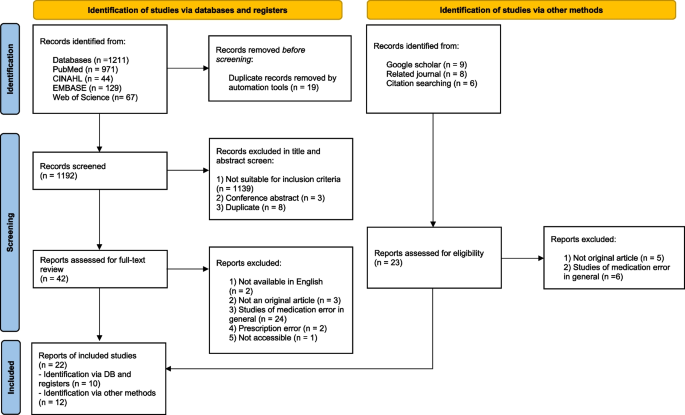
A total of 1211 studies were selected through a database search. After reviewing the titles and abstracts of the studies, 42 studies were considered for a detailed assessment by the three researchers. In particular, 2 were not available in English, 3 were not original articles, 24 were studies of medication error in general without details on rate control of IV medications, 2 were regarding prescription errors, and 1 was not accessible. Finally, 10 studies were identified through a database search. Additionally, 23 studies were identified from a manual search. Among the 23, 5 were not original articles, and 6 were studies on medication error in general. Finally, 12 studies were identified via other methods. Hence, 22 studies were included in the data analysis (Fig. 1, Additional file 3).
Characteristics of the studies
General characteristics
Table 1 presents the general characteristics of the included studies. Two of the included studies had a publication year before 2000 [20, 21], and more than half of the studies (n = 15) were published in 2010 and later. A majority of the included studies were conducted in Western countries (n = 15) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36], four were conducted in Asia [20, 37,38,39], two were conducted in Australia [21, 40], and one was conducted in Egypt [2]. In terms of the study design, most studies were project studies (n = 7) [22, 24, 27, 28, 30, 34, 39] or prospective observational studies (n = 5) [2, 20, 29, 32, 40], followed by retrospective studies (n = 3) [21, 25, 35], qualitative or mixed-methods studies (n = 3) [23, 26, 33], and descriptive cross-sectional studies (n = 2) [36, 38]. Additionally, there was one controlled pre-posttest study [37] and one simulation laboratory experiment study [31]. The study period also varied greatly from 2 days [32] to 6 years [25].
The aims of the included studies were divided into two main categories. First, 13 studies identified the current status, causes, and factors influencing errors that could occur in healthcare settings [2, 20, 21, 23, 25, 26, 29, 32, 33, 35, 36, 38, 40]. Among these, three studies were on errors that may occur in specific healthcare procedures, such as anesthesia [20], vascular access [21], and pediatric chemotherapy [25]. Additionally, three studies explored possible errors associated with specific settings and medications, such as an obstetric emergency ward [2], cardiac critical care units [38], and high-alert medications [36], and three studies investigated the errors associated with the overall IV medication preparation or administration [23, 33, 40]. Moreover, three studies aimed at identifying potential problems associated with the use of IV medication infusion devices [26, 32, 35], and one study was about errors in medication preparation and administration that could occur in a setting using a specific system connected to electronic medical records [29]. Second, nine studies described the procedure of developing interventions or identified the effect of interventions [22, 24, 27, 28, 30, 31, 34, 37, 39].
Participants and events
Participants in the 22 studies included HCPs such as nurses, doctors, pharmacists, and patients. Notably, four of these studies were only for nurses [31, 37, 38, 40] and there was also one study involving only pharmacists [36]. Furthermore, there were five studies wherein people from various departments or roles participated [23, 26,27,28, 39]. There were three studies wherein the patients were participants, and two studies included both patients and medical staff [29, 33].
Among the included studies, nine studies focused on errors in IV medication preparation and administration as events [23, 26, 30, 32,33,34, 37, 38, 40] and five studies focused on the administration process only [30, 32, 34, 37, 40]. Four studies focused on problems in the administration of all types of drugs including errors associated with rate control of IV medications [2, 22, 28, 29]. Additionally, four studies focused on events that occurred with IV medication infusion devices [24, 27, 35, 39], two studies explored the events that occurred during chemotherapy [22, 25], and some analyzed events with problems in vascular access [21], iatrogenic events among neonates [28], and critical events in anesthesia cases [20].
Contexts and methods
The contexts can be largely divided into healthcare settings, including hospitals and laboratory settings. Three hospital-based studies were conducted in the entire hospital [20, 22, 24], eight studies were conducted at several hospitals, and the number of hospitals involved varied from 2 to 132 [23, 26, 32,33,34,35, 38, 40]. Furthermore, four studies were conducted in different departments within one hospital [29, 30, 37, 39], three studies were conducted in only one department [2, 27, 28], two studies considered other healthcare settings and were not limited to hospitals [21, 25], and one study was conducted in a simulation laboratory setting that enabled a realistic simulation of an ambulatory chemotherapy unit [31].
Specifically, seven out of the nine studies developed or implemented interventions based on interdisciplinary or multidisciplinary collaboration [22, 24, 28, 30, 34, 37, 39]. Two studies developed and identified the effectiveness of interventions that created an environment for nurses to improve performance and correct errors associated with medication administration [31, 39], and two intervention studies were on error reporting methods or observation tools and the processes of addressing reported errors [28, 30]. There were also a study on a pharmacist-led educational program for nurses [37], a comprehensive intervention from drug prescription to administration to reduce chemotherapy-related medication errors [22], infusion safety intervention bundles [34], the implementation of a smart IV pump equipped with failure mode and effects analysis (FMEA) [24], and a smart system to prevent pump programming errors [27].
Data collection methods were classified as a review of reported incidents [20,21,22, 25, 35], a review of medical charts [26], observations [23, 29,30,31,32,33,34, 37, 40], follow-up on every pump alert [27], and self-reporting questionnaires or surveys [36, 38]. Some studies utilized retrospective reviews of reported incidents and self-report questionnaires [39]. Also, in the study by Kandil et al., observation, nursing records review, and medical charts review were all used [2].
Attributes of errors associated with rate control of IV medications
Table 2 presents the attributes of errors related to rate control of IV medications in observed results or intervention outcomes, and error severity. Notably, 6 of 13 studies presenting observed results reported errors related to IV medication infusion devices among the rate control errors [20, 25, 32, 33, 35, 36]. Additionally, four studies reported errors in bolus dose administration or IV push and flushing lines among IV rate errors [2, 23, 36, 40]. Among the 13, nine studies reported error severity, and among these, three studies used NCC MERP ratings [25, 32, 33]. In four studies, error severity was reported by describing several cases in detail [2, 21, 23, 25], and two studies reported no injuries or damages due to errors [26, 29]. Among the nine studies that developed interventions and identified their effectiveness, four presented the frequency of incorrect rate errors as an outcome variable [28, 30, 34, 37]. Moreover, two studies suggested compliance rates for intervention as outcome variables [24, 31].
Among the nine project or experiment studies, three showed a decrease in error rate as a result of the intervention [28, 31, 34]. Three studies developed interventions to reduce rate errors but did not report the frequency or incidence of rate errors [22, 24, 27]. A study reported the frequency of rate errors only after the intervention; the effect of the intervention could not be identified [30]. Also, three studies showed the severity of errors related to rate control of IV medications [24, 30, 34], two used NCC MERP severity ratings [30, 34], and one reported that all errors caused by smart IV pumps equipped with FMEA resulted in either temporary harm or no harm [24].
Facilitators and barriers to rate control of IV medications
Table 3 presents the facilitators and barriers related to rate control of IV medications according to the NCC MERP taxonomy based on the 22 included studies. Sub-categories of human factors were classified as knowledge deficit, performance deficit, miscalculation of dosage or infusion rate, and stress. The sub-category of design factor was device. System-related contributing factors were classified as frequent interruptions and distractions, inadequate training, poor assignment or placement of HCPs or inexperienced personnel, policies and procedures, and communication systems between HCPs [14].
Human factors
Among the barriers extracted from the 22 studies, 11 factors belonged to the “knowledge deficit,” “performance deficit,” “miscalculation of dosage or infusion rate,” and “stress (high-volume workload)” in this category. Half of these factors are related to the “performance deficit.” Barriers identified in two or more studies were tubing misplacement [24, 35] and non-compliance with protocols and guidelines [2, 25], all of which belonged to the “performance deficit.” Additionally, the high workload and environmental characteristics of the ICU, which corresponded to the “stress,” were also identified as barriers to rate control of IV medications [23, 37].
Design
Most factors in this category were related to IV medication infusion devices such as infusion pumps and smart pumps. In the study by Lyons et al., the use of devices, such as patient-controlled analgesia pumps and syringe drivers, was a facilitator of rate control of IV medications [33]. In addition to the use of these devices, the expansion of capabilities [26], monitoring programming [27], and standardization [22] were also facilitators. Unexpected equipment faults, a barrier, were identified in five studies [2, 20, 25, 35, 38]. Moreover, the complex design of the equipment [23, 24] and incomplete drug libraries in smart pumps [33, 35] were identified in two studies each. Factors such as the misassembly of an unfamiliar infusion pump [21] and smart pumps not connected to electronic systems [30] were also barriers.
Contributing factors (system related)
The factors belonging to the “frequent interruptions and distractions” in this category were all barriers. Specifically, running multiple infusions at once [24, 27], air-in-line alarms, or cleaning air [24] were identified as barriers. Among the facilitators of the “training,” there were education and training on the use of smart IV pumps [24] and chemotherapy errors [22]. There are two factors in the “assignment or placement of a HCP or inexperienced personnel,” where ward-based pharmacists were facilitators [36], but nurses with less than 6 years of experience were barriers [40]. The sub-category with the most factors was “policies and procedures,” where the facilitators extracted in the four studies were double-checks through the process [22, 24, 28, 36]. Among the barriers, two were related to keep-the-vein-open, which was identified in three studies [30, 32, 33]. The lack of automated infusion pumps [2], the absence of culture for use [32, 33], and problems in the drug prescription process [33] were also identified as barriers. Communication with physicians in instances of doubt identified was the only identified facilitator in the “communication systems between HCPs” [28].
Resolutions for the barriers to rate control of IV medications
Table 4 presents the resolutions for the barriers to rate control of IV medications in the included studies. The suggested resolutions primarily belonged to the “contributing factors (system-related)” category. Resolutions in the “human factors” category were mainly related to the knowledge and performance of individual healthcare providers, and there were no studies proposing resolutions specifically addressing stress (high-volume workload), which is one of the barriers. Resolutions in the “design” category focused on the development [26, 30], appropriate use [24, 33], evaluation [26], improvement [24, 26, 30], and supply [23] of infusion pumps or smart pumps. Resolutions addressing aspects within the “contributing factors (system-related)” category can be classified into six main areas: interdisciplinary or inter-institution collaboration [23, 25, 28, 30, 34,35,36,37], training [24, 37, 40], implementation of policies or procedures [29, 31, 34, 35, 37, 39], system improvement [25, 30, 32], creating a patient safety culture [25, 37, 38], and staffing [2, 38].
Discussion
This scoping review provides the most recent evidence on the attributes of errors, facilitators, and barriers related to rate control of IV medications. The major findings of this study were as follows: (1) there were a few intervention studies that were effective in decreasing the errors related to rate control of IV medications; (2) there was limited research focusing on the errors associated with IV medication infusion devices; (3) a few studies have systematically evaluated and analyzed the severity of errors associated with rate control of IV medications; and (4) the facilitators and barriers related to rate control of IV medications were identified by NCC MERP taxonomy as three categories (human factors, design, and system-related contributing factors).
Among the nine project or experiment studies, only two interventions showed statistically significant effectiveness for IV rate control [28, 31]. Six studies did not report the specific statistical significance of the intervention [22, 24, 27, 30, 37, 39], and one study found that the developed intervention had no statistically significant effect [34]. In another study, administration errors, including rate errors, increased in the experimental group and decreased in the control group [37]. IV rate control is a major process in medication administration that is comprehensively related to environmental and personal factors [3, 41]. According to previous studies, interdisciplinary or multidisciplinary cooperation is associated with the improvement in patient safety and decreased medical errors [42,43,44]. Seven of the included studies were also project or experiment studies that developed interventions based on an interdisciplinary or multidisciplinary approach [22, 24, 28, 30, 34, 37, 39]. Additionally, an effective intervention was developed by a multidisciplinary care quality improvement team [28]. Therefore, it is crucial to develop effective interventions based on an interdisciplinary or multidisciplinary approach to establish practice guidelines with a high level of evidence related to IV rate control.
Of the 22 included studies, three identified potential problems associated with the use of IV medication infusion devices [26, 32, 35], and four described the application of interventions or explored the effects of the intervention developed to reduce errors that occur when using IV medication infusion devices [24, 27, 34, 39]. IV medication infusion devices, such as infusion pumps and smart pumps, are widely used in healthcare environments and allow more rigorous control in the process of administering medications that are continuously infused [45]. Smart pumps are recognized as useful devices for providing safe and effective nursing care [15]. However, the use of IV medication infusion devices requires an approach different from traditional rate monitoring by counting the number of fluid drops falling into the drip chamber [9]. However, there exist many problems, such as bypassing the drug library, device maintenance, malfunction, tubing/connection, and programming in the use of IV medication infusion devices [32, 35]. None of the four studies that described the application of interventions or explored the effects of the intervention demonstrated statistically significant effects. All four studies had no control group [24, 27, 34, 39] and two studies had only post-test designs [24, 27]. Therefore, further research needs to be conducted to analyze errors in rate control related to IV medication infusion devices and develop effective interventions.
A few studies have systematically evaluated and analyzed the severity of errors associated with rate control of IV medications. Among the 12 studies that reported the severity of errors associated with rate control of IV medications, five studies used NCC MERP, an internationally validated and reliable tool for assessing error severity, and one study used the Severity Assessment Code (SAC) developed by the New South Wales Health Department. Six studies did not use tools to assess error severity. The term “error severity” means the degree of potential or actual harm to patients [46]. Evaluating the severity of medication errors is a vital point in improving patient safety throughout the medication administration process. This evaluation allows for distinguishing errors based on their severity to establish the development of risk mitigation strategies focused on addressing errors with the great potential to harm patients [47, 48]. Specifically, errors associated with rate control of IV medications were categorized as A to E on the NCC MERP and to groups 3 and 4 on the SAC. Additionally, errors associated with rate control of IV medications caused direct physical damage [2, 21] and necessitated additional medication to prevent side effects or toxicity [23]. Therefore, as errors in rate control of IV medications are likely to cause actual or potential harm to the patient, research systematically evaluating and analyzing error severity should be conducted to provide the basis for developing effective risk reduction strategies in the rate control of IV medications.
Facilitators and barriers were identified as human, design, and system-related contributing factors. Among the human factors, “performance deficit” included failure to check equipment properly, tubing misplacement, inadequate monitoring, non-compliance with protocols and guidelines, and human handling errors with smart pumps. Nurses play a major role in drug administration; thus, their monitoring and practices related to IV medication infusion devices can influence patient health outcomes [3, 49]. A major reason for the lack of monitoring was overwork, which was related to the complex working environment, work pressure, and high workload [3, 11, 49]. Moreover, two of the included studies identified high workload as a barrier to rate control of IV medications [23, 37]. Therefore, to foster adequate monitoring of rate control of IV medications, a systematic approach to alleviating the complex working environment and work pressure should be considered.
Most facilitators and barriers in the devices category were related to IV medication infusion devices. In particular, expanding pump capabilities [26], monitoring pump programming [27], standardization [22], and using a pump [33] can facilitate rate control of IV medications. However, unexpected equipment faults are significant barriers, as identified in five studies among the included studies [2, 20, 25, 35, 38]. Moreover, the design [23, 24], user-friendliness [21], connectivity to electronic systems [30], and completeness of drug libraries [33, 35] are factors that can affect rate control of IV medications. Therefore, it is important to improve, monitor, and manage IV medication infusion devices so that they do not become barriers. Moreover, because rate errors caused by other factors can be prevented by devices, active utilization and systematic management of devices at the system level are required.
Although there are many benefits of infusion and smart pumps for reducing errors in rate control of IV medications, they cannot be used in all hospitals because of the limitation of medical resources. The standard infusion set, which is a device for controlling the rate of IV medication by a controller [9], is widely used in outpatient as well as inpatient settings [32]. Devices for monitoring the IV infusion rate, such as FIVA™ (FIVAMed Inc, Halifax, Canada) and DripAssist (Shift Labs Inc, Seattle, USA), which can continuously monitor flow rate and volume with any gravity drip set, have been commercialized [33]. However, they have not been widely used in hospitals. Therefore, developing novel IV infusion rate monitoring devices that are simple to use, can be used remotely, and are affordable for developing and underdeveloped countries can help nurses to reduce their workloads in monitoring IV infusion rates and thus maintain patient safety.
Most facilitators and barriers were system-related contributing factors, most of which belonged to the “policies and procedures.” In four studies, the absence of hospital policies or culture related to rate control of IV medications was identified as a barrier [2, 30, 32, 33]. Medication errors related to incorrect rate control are problems that should be approached from macroscopic levels, such as via institutional policies and safety cultures. Therefore, large-scale research including more diverse departments and institutions needs to be conducted.
The second most common categories in system-related contributing factors were “frequent interruptions and distractions” and “training.” Although nurses experienced frequent interruptions and distributions during work, only one of the included studies was on interventions that were developed to create an environment with reduced interruptions [31]. Additionally, four studies found that education for nurses who are directly associated with medication administration is mandatory [22,23,24, 36]. Therefore, education and a work environment for safety culture should be created to improve IV rate control.
Based on resolutions for barriers to rate control of IV medications, key groups relevant to rate control of IV medications include HCPs, healthcare administrators, and engineers specializing in IV medication infusion devices. HCPs directly involved in the preparation and administration of IV medications need to enhance their knowledge of drugs, raise awareness for the importance of rate control of IV medications, and improve performance related to IV infusion device monitoring. Engineers specializing in IV medication infusion devices should develop these devices by integrating various information technologies used in clinical settings. Additionally, they should identify issues related to these devices and continuously enhance both software and hardware. Healthcare administrators play a crucial role in establishing and leading interdisciplinary or inter-institution collaborations. They should foster leadership, build a patient safety culture within the organization, and implement training, interventions, and policies for correct rate control of IV medications. Decreasing medication errors, including errors in IV rate control, is closely linked to the various key groups [50,51,52,53], and multidisciplinary collaboration is emphasized for quality care [54,55,56,57]. Therefore, each key group should perform its role and cooperate for appropriate IV rate control within a structured system.
This review has some limitations that should be considered. As there was no randomized controlled trial in this review, the causal relationship between wrong rate errors and their facilitators or barriers could not be determined. Moreover, only limited literature may have been included in this review because we included literature published in English and excluded gray literature. Since we did not evaluate the quality of the study, there may be a risk of bias in data collection and analysis. Despite these limitations, this study provides a meaningful assessment of published studies related to rate control of IV medications. This contribution will provide an important basis for new patient safety considerations in IV medication administration when determining future policies and device development.
Conclusions
The findings of this review suggest that further research is needed to be conducted to develop effective interventions to improve the practice of IV rate control. Moreover, given the rapid growth of technology in medical settings, research on IV medication infusion devices should be conducted. Additionally, to establish effective risk reduction strategies, it is necessary to systematically evaluate and analyze the severity of errors related to the rate control of IV medications. Several facilitators and barriers to rate control of IV medications were identified in this review to ensure patient safety and quality care, interventions and policy changes related to education and the work environment are required. Additionally, the development of a device capable of monitoring the flow of IV medication is necessary. This review will be useful for HCPs, hospital administrators, and engineers specializing in IV medication infusion devices to minimize errors in rate control of IV medications and improve patient safety.
Availability of data and materials
The corresponding author can provide the datasets that were utilized and/or examined during the present study upon reasonable request.
Abbreviations
- AE:
-
Adverse event
- HCP:
-
Healthcare provider
- ICU:
-
Intensive care unit
- IV:
-
Intravenous
- JBI:
-
Joanna Briggs Institute
- NCC MERP:
-
The National Coordinating Council for Medication Error Reporting and Prevention
References
Cousins DD, Heath WM. The National Coordinating Council for medication error reporting and prevention: promoting patient safety and quality through innovation and leadership. Jt Comm J Qual Patient Saf. 2008;34(12):700–2. https://doi.org/10.1016/s1553-7250(08)34091-4.
Kandil M, Sayyed T, Emarh M, Ellakwa H, Masood A. Medication errors in the obstetrics emergency ward in a low resource setting. J Matern Fetal Neonatal Med. 2012;25(8):1379–82. https://doi.org/10.3109/14767058.2011.636091.
Parry AM, Barriball KL, While AE. Factors contributing to registered nurse medication administration error: a narrative review. Int J Nurs Stud. 2015;52(1):403–20. https://doi.org/10.1016/j.ijnurstu.2014.07.003.
Vrbnjak D, Denieffe S, O’Gorman C, Pajnkihar M. Barriers to reporting medication errors and near misses among nurses: a systematic review. Int J Nurs Stud. 2016;63:162–78. https://doi.org/10.1016/j.ijnurstu.2016.08.019.
Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 2021;30(2):96–105. https://doi.org/10.1136/bmjqs-2019-010206.
U.S. Food and Drug Administration (FDA) . Working to reduce medication errors [Internet]. U.S. Food and Drug Administration (FDA). 2019. Available from: https://www.fda.gov/drugs/information-consumers-and-patients-drugs/working-reduce-medication-errors. Cited 27 Dec 2022
Institute of Medicine (US). Committee on quality of health care in America. In: Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: building a safer health system. Washington: National Academies Press (US); 2000. PMID: 25077248.
EscriváGracia J, Brage Serrano R, Fernández GJ. Medication errors and drug knowledge gaps among critical-care nurses: a mixed multi-method study. BMC Health Serv Res. 2019;19(1):640. https://doi.org/10.1186/s12913-019-4481-7.
Park K, Lee J, Kim SY, Kim J, Kim I, Choi SP, et al. Infusion volume control and calculation using metronome and drop counter based intravenous infusion therapy helper. Int J Nurs Pract. 2013;19(3):257–64. https://doi.org/10.1111/ijn.12063.
Marwitz KK, Giuliano KK, Su WT, Degnan D, Zink RJ, DeLaurentis P. High-alert medication administration and intravenous smart pumps: a descriptive analysis of clinical practice. Res Social Adm Pharm. 2019;15(7):889–94. https://doi.org/10.1016/j.sapharm.2019.02.007.
Kale A, Keohane CA, Maviglia S, Gandhi TK, Poon EG. Adverse drug events caused by serious medication administration errors. BMJ Qual Saf. 2012;21(11):933–8. https://doi.org/10.1136/bmjqs-2012-000946.
Yoon J, Yug JS, Ki DY, Yoon JE, Kang SW, Chung EK. Characterization of medication errors in a medical intensive care unit of a university teaching hospital in South Korea. J Patient Saf. 2022;18(1):1–8. https://doi.org/10.1097/pts.0000000000000878.
McDowell SE, Mt-Isa S, Ashby D, Ferner RE. Where errors occur in the preparation and administration of intravenous medicines: a systematic review and Bayesian analysis. Qual Saf Health Care. 2010;19(4):341–5. https://doi.org/10.1136/qshc.2008.029785.
National Coordinating Council for Medication Error Reporting and Prevention. Taxonomy of medication errors. NCC MERP. 2001. Available from: https://www.nccmerp.org/taxonomy-medication-errors. Cited 27 Dec 2022
Moreira APA, Carvalho MF, Silva R, Marta CB, Fonseca ERD, Barbosa MTS. Handling errors in conventional and smart pump infusions: a systematic review with meta-analysis. Rev Esc Enferm USP. 2020;54:e03562. https://doi.org/10.1590/s1980-220x2018032603562.
Sutherland A, Canobbio M, Clarke J, Randall M, Skelland T, Weston E. Incidence and prevalence of intravenous medication errors in the UK: a systematic review. Eur J Hosp Pharm. 2020;27(1):3–8. https://doi.org/10.1136/ejhpharm-2018-001624.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:1–9.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10. https://doi.org/10.1097/xeb.0000000000000277.
Short TG, O’Regan A, Lew J, Oh TE. Critical incident reporting in an anaesthetic department quality assurance programme. Anaesthesia. 1993;48(1):3–7. https://doi.org/10.1111/j.1365-2044.1993.tb06781.x.
Singleton RJ, Webb RK, Ludbrook GL, Fox MA. The Australian incident monitoring study. Problems associated with vascular access: an analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21(5):664–9. https://doi.org/10.1177/0310057x9302100531.
Goldspiel BR, DeChristoforo R, Daniels CE. A continuous-improvement approach for reducing the number of chemotherapy-related medication errors. Am J Health Syst Pharm. 2000;15(57 Suppl 4):S4-9. https://doi.org/10.1093/ajhp/57.suppl_4.S4. PMID: 11148943.
Taxis K, Barber N. Causes of intravenous medication errors: an ethnographic study. Qual Saf Health Care. 2003;12(5):343–7. https://doi.org/10.1136/qhc.12.5.343.
Wetterneck TB, Skibinski KA, Roberts TL, Kleppin SM, Schroeder ME, Enloe M, et al. Using failure mode and effects analysis to plan implementation of smart i.v. pump technology. Am J Health Syst Pharm. 2006;63(16):1528–38. https://doi.org/10.2146/ajhp050515.
Rinke ML, Shore AD, Morlock L, Hicks RW, Miller MR. Characteristics of pediatric chemotherapy medication errors in a national error reporting database. Cancer. 2007;110(1):186–95. https://doi.org/10.1002/cncr.22742.
Nuckols TK, Bower AG, Paddock SM, Hilborne LH, Wallace P, Rothschild JM, et al. Programmable infusion pumps in ICUs: an analysis of corresponding adverse drug events. J Gen Intern Med. 2008;23:41–5.
Evans RS, Carlson R, Johnson KV, Palmer BK, Lloyd JF. Enhanced notification of infusion pump programming errors. Stud Health Technol Inform. 2010;160(Pt 1):734–8 PMID: 20841783.
Ligi I, Millet V, Sartor C, Jouve E, Tardieu S, Sambuc R, Simeoni U. Iatrogenic events in neonates: beneficial effects of prevention strategies and continuous monitoring. Pediatrics. 2010;126(6):e1461–8. https://doi.org/10.1542/peds.2009-2872.
Rodriguez-Gonzalez CG, Herranz-Alonso A, Martin-Barbero ML, Duran-Garcia E, Durango-Limarquez MI, Hernández-Sampelayo P, Sanjurjo-Saez M. Prevalence of medication administration errors in two medical units with automated prescription and dispensing. J Am Med Inform Assoc. 2012;19(1):72–8. https://doi.org/10.1136/amiajnl-2011-000332.
Ohashi K, Dykes P, McIntosh K, Buckley E, Wien M, Bates DW. Evaluation of intravenous medication errors with smart infusion pumps in an academic medical center. AMIA Annu Symp Proc. 2013;2013:1089–98 PMID: 24551395; PMCID: PMC3900131.
Prakash V, Koczmara C, Savage P, Trip K, Stewart J, McCurdie T, et al. Mitigating errors caused by interruptions during medication verification and administration: interventions in a simulated ambulatory chemotherapy setting. BMJ Qual Saf. 2014;23(11):884–92. https://doi.org/10.1136/bmjqs-2013-002484.
Schnock KO, Dykes PC, Albert J, Ariosto D, Call R, Cameron C, et al. The frequency of intravenous medication administration errors related to smart infusion pumps: a multihospital observational study. BMJ Qual Saf. 2017;26(2):131–40. https://doi.org/10.1136/bmjqs-2015-004465.
Lyons I, Furniss D, Blandford A, Chumbley G, Iacovides I, Wei L, et al. Errors and discrepancies in the administration of intravenous infusions: a mixed methods multihospital observational study. BMJ Qual Saf. 2018;27(11):892–901. https://doi.org/10.1136/bmjqs-2017-007476.
Schnock KO, Dykes PC, Albert J, Ariosto D, Cameron C, Carroll DL, et al. A multi-hospital before-after observational study using a point-prevalence approach with an infusion safety intervention bundle to reduce intravenous medication administration errors. Drug Saf. 2018;41(6):591–602. https://doi.org/10.1007/s40264-018-0637-3.
Taylor MA, Jones R. Risk of medication errors with infusion pumps: a study of 1,004 events from 132 hospitals across Pennsylvania. Patient Safety. 2019;1(2):60–9. https://doi.org/10.33940/biomed/2019.12.7.
Schilling S, Koeck JA, Kontny U, Orlikowsky T, Erdmann H, Eisert A. High-alert medications for hospitalised paediatric patients - a two-step survey among paediatric clinical expert pharmacists in Germany. Pharmazie. 2022;77(6):207–15. https://doi.org/10.1691/ph.2022.12025.
Nguyen HT, Pham HT, Vo DK, Nguyen TD, van den Heuvel ER, Haaijer-Ruskamp FM, Taxis K. The effect of a clinical pharmacist-led training programme on intravenous medication errors: a controlled before and after study. BMJ Qual Saf. 2014;23(4):319–24. https://doi.org/10.1136/bmjqs-2013-002357.
Bagheri-Nesami M, Esmaeili R, Tajari M. Intravenous medication administration errors and their causes in cardiac critical care units in Iran. Mater Sociomed. 2015;27(6):442–6. https://doi.org/10.5455/msm.2015.27.442-446.
Tsang LF, Tsang WY, Yiu KC, Tang SK, Sham SYA. Using the PDSA cycle for the evaluation of pointing and calling implementation to reduce the rate of high-alert medication administration incidents in the United Christian Hospital of Hong Kong, China. J Patient Safety Qual Improv. 2017;5(3):577–83. https://doi.org/10.22038/PSJ.2017.9043.
Westbrook JI, Rob MI, Woods A, Parry D. Errors in the administration of intravenous medications in hospital and the role of correct procedures and nurse experience. BMJ Qual Saf. 2011;20(12):1027–34. https://doi.org/10.1136/bmjqs-2011-000089.
Daker-White G, Hays R, McSharry J, Giles S, Cheraghi-Sohi S, Rhodes P, Sanders C. Blame the patient, blame the doctor or blame the system? A meta-synthesis of qualitative studies of patient safety in primary care. PLoS ONE. 2015;10(8):e0128329. https://doi.org/10.1371/journal.pone.0128329.
Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Arch Intern Med. 2003;163(17):2014–8. https://doi.org/10.1001/archinte.163.17.2014.
Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev. 2006;63(3):263–300. https://doi.org/10.1177/1077558706287003.
O’Leary KJ, Buck R, Fligiel HM, Haviley C, Slade ME, Landler MP, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–84. https://doi.org/10.1001/archinternmed.2011.128.
Yu D, Obuseh M, DeLaurentis P. Quantifying the impact of infusion alerts and alarms on nursing workflows: a retrospective analysis. Appl Clin Inform. 2021;12(3):528–38. https://doi.org/10.1055/s-0041-1730031. Epub 2021 Jun 30. PMID: 34192773; PMCID: PMC8245209.
Gates PJ, Baysari MT, Mumford V, Raban MZ, Westbrook JI. Standardising the classification of harm associated with medication errors: the harm associated with medication error classification (HAMEC). Drug Saf. 2019;42(8):931–9. https://doi.org/10.1007/s40264-019-00823-4.
Assunção-Costa L, Ribeiro Pinto C, Ferreira Fernandes Machado J, Gomes Valli C, de PortelaFernandes Souza LE, Dean FB. Validation of a method to assess the severity of medication administration errors in Brazil: a study protocol. J Public Health Res. 2022;11(2):2022. https://doi.org/10.4081/jphr.2022.2623.
Walsh EK, Hansen CR, Sahm LJ, Kearney PM, Doherty E, Bradley CP. Economic impact of medication error: a systematic review. Pharmacoepidemiol Drug Saf. 2017;26(5):481–97. https://doi.org/10.1002/pds.4188.
Khalil H, Shahid M, Roughead L. Medication safety programs in primary care: a scoping review. JBI Database Syst Rev Implement Rep. 2017;15(10):2512–26. https://doi.org/10.11124/jbisrir-2017-003436.
Atey TM, Peterson GM, Salahudeen MS, Bereznicki LR, Simpson T, Boland CM, et al. Impact of partnered pharmacist medication charting (PPMC) on medication discrepancies and errors: a pragmatic evaluation of an emergency department-based process redesign. Int J Environ Res Public Health. 2023;20(2):1452. https://doi.org/10.3390/ijerph20021452.
Atey TM, Peterson GM, Salahudeen MS, Bereznicki LR, Wimmer BC. Impact of pharmacist interventions provided in the emergency department on quality use of medicines: a systematic review and meta-analysis. Emerg Med J. 2023;40(2):120–7. https://doi.org/10.1136/emermed-2021-211660.
Hanifin R, Zielenski C. Reducing medication error through a collaborative committee structure: an effort to implement change in a community-based health system. Qual Manag Health Care. 2020;29(1):40–5. https://doi.org/10.1097/qmh.0000000000000240.
Kirwan G, O’Leary A, Walsh C, Grimes T. Economic evaluation of a collaborative model of pharmaceutical care in an Irish hospital: cost-utility analysis. HRB Open Res. 2023;6:19. https://doi.org/10.12688/hrbopenres.13679.1.
Billstein-Leber M, Carrillo CJD, Cassano AT, Moline K, Robertson JJ. ASHP guidelines on preventing medication errors in hospitals. Am J Health Syst Pharm. 2018;75(19):1493–517. https://doi.org/10.2146/ajhp170811.
Lewis KA, Ricks TN, Rowin A, Ndlovu C, Goldstein L, McElvogue C. Does simulation training for acute care nurses improve patient safety outcomes: a systematic review to inform evidence-based practice. Worldviews Evid Based Nurs. 2019;16(5):389–96. https://doi.org/10.1111/wvn.12396.
Mardani A, Griffiths P, Vaismoradi M. The role of the nurse in the management of medicines during transitional care: a systematic review. J Multidiscip Healthc. 2020;13:1347–61. https://doi.org/10.2147/jmdh.S276061.
L Naseralallah D Stewart M Price V Paudyal 2023 Prevalence, contributing factors, and interventions to reduce medication errors in outpatient and ambulatory settings: a systematic review Int J Clin Pharm https://doi.org/10.1007/s11096-023-01626-5
Funding
This research was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (Project Number: RS-2020-KD000077) and Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. 2020R1A6A1A03041989). This work also supported by the Brain Korea 21 FOUR Project funded by National Research Foundation (NRF) of Korea, Yonsei University College of Nursing.
Author information
Authors and Affiliations
Contributions
Conceptualization: JP; study design: JP; data collection: GWR, YK, SBY; data analysis: JP, GWR, YK, SBY; administration: JP; funding acquisition: JP; writing—original draft: JP, GWR, YK; writing—review and editing: JP, YK.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist.
Additional file 2:
Search queries and strategies by electronic databases.
Additional file 3:
Studies included in the data analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, J., You, S.B., Ryu, G.W. et al. Attributes of errors, facilitators, and barriers related to rate control of IV medications: a scoping review. Syst Rev 12, 230 (2023). https://doi.org/10.1186/s13643-023-02386-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02386-z