Abstract
Background
Subjective cognitive impairment (SCI) substantially increases dementia risk and is often conceptualised as the preclinical asymptomatic phase of the cognitive decline continuum. Due to the lack of pharmacological interventions available to treat SCI and reduce dementia risk, and the popularity of herbal and nutritional medicines, the primary aim of this review was to investigate the efficacy on cognitive function and safety of herbal and nutritional medicines (relative to a control) for older adults with and without SCI. The secondary aims were to describe the study characteristics and assess the methodological quality of included studies.
Method
Five databases (Cochrane, MEDLINE, CINAHL, PsycInfo, and EMBASE) were searched from database inception with weekly alerts established until review finalisation on 18 September 2022. Articles were eligible if they included the following: study population of older adults with and without SCI, herbal and nutritional medicines as an intervention, evaluated cognitive outcomes and were randomised control trials.
Results
Data were extracted from 21/7666 eligible full-text articles, and the risk of methodological bias was assessed (with SCI = 9/21; without SCI = 12/21). Most studies (20/21) employed parallel, randomised, placebo-controlled designs and were 12 weeks in length. Herbal supplements were widely used (17/21), namely a form of Ginkgo biloba (8/21) or Bacopa monnieri (6/21). Measures of cognition varied across studies, with 14/21 reporting improvements in at least one domain of cognitive functioning over time, in the intervention group (compared to control). A total of 14/21 studies were deemed as having an overall high methodological risk of bias, 6/21 had some concerns, and only one study (using an SCI population) was assessed as having a low risk of methodological bias.
Conclusions
Overall, this review found that there is a low quality of evidence regarding the efficacy of cognitive function and safety of herbal and nutritional medicines for older adults with and without SCI, due to a high risk of bias across studies. Additionally, further work needs to be done in classifying and understanding SCI and selecting appropriate trial primary outcomes before future studies can more accurately determine the efficacy of interventions for this population.
Similar content being viewed by others
Introduction
Subjective cognitive impairment (SCI) is a self-perceived worsening of cognitive functioning, particularly in the area of memory, that cannot be verified by neuropsychological tests [1, 2]. SCI lies on a continuum of healthy cognitive ageing and is conceptualised as the preclinical phase of dementia (healthy cognitive ageing, to preclinical SCI, followed by prodromal mild cognitive impairment (MCI), then dementia) [2,3,4]. SCI is estimated to double the risk of future objective decline (MCI or dementia) [5, 6], carries an increased prevalence of Alzheimer’s disease biomarkers and impacts mental health (1 in 3 people) and functional ability (1 in 2 people) [7], making it an important area of focus for secondary prevention research and care.
It is estimated that the prevalence of SCI is 1 in 4 older adults aged 60 years and above, worldwide, with these numbers increasing rapidly each year [2]. Currently, there are no approved pharmacological interventions available, with many older adults experiencing SCI seeking alternative treatments [8]. Difficulty also lies with the assessment of SCI, as current diagnostic tools have been developed for MCI or dementia [8, 9]. Furthermore, inconsistencies in the categorisation of SCI (namely the division between healthy adults without SCI and those with SCI) are apparent in research [8, 9]. Due to the increased risk of dementia and high prevalence of SCI, high-quality research into effective treatments to improve cognitive functioning and prolong further decline is needed.
A review and meta-analysis conducted in 2018 investigated a variety of interventions (group psychological, cognitive, lifestyle and complementary and alternative medicines) for the treatment of SCI and their efficacy on psychological well-being, metacognition and objective cognitive performance [9]. The authors found that studies were generally of low quality; hence, no firm conclusions could be made about the efficacy of the interventions employed [9]. Whilst this review/meta-analysis is of great importance to furthering SCI treatment research, it did not explore the efficacy of single interventions on cognitive functioning, nor did they investigate this usage and efficacy in older adults without SCI.
Complementary medicines (CMs) are defined as a broad range of health care approaches that are not thought to be part of conventional medical care [10, 11]. CMs are classified into three primary categories of delivery: nutritional (e.g. herbs, dietary supplements), psychological (e.g. meditation, relaxation therapy) and physical (e.g. acupuncture, massage) [10]. CMs are becoming more widely available and used by older adults, particularly herbal and nutritional medicines for the treatment of chronic health conditions including, cardiovascular disease [12], diabetes [13] and dementia [14, 15]. Herbal medicines contain herbal substances or herbal preparations, with nutritional supplements/medicines containing vitamins, minerals and in combination formulas and herbal substances/preparations as well [11, 16]. The natural properties of these medicines make them attractive to individuals wanting to improve their general health and well-being [11].
The primary aim of this review was to investigate the efficacy of cognitive function and safety of herbal and nutritional medicines (compared to an appropriate control group) for older adults with and without SCI. The secondary aims were to describe the study characteristics and assess the methodological quality of included studies, utilising the Cochrane risk of methodological bias (ROB 2) tool. This is the first review, to our knowledge, that has investigated the use of herbal and nutritional medicines for older adults with and without SCI, in depth.
Methods
This review is structured according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17] and registered with the PROSPERO international database of systematic reviews on 7 May 2021 (#CRD42021244631). A protocol was not published for this review.
Eligibility criteria
A scoping review was conducted in line with the study eligibility criteria which were determined as per the PICOS principles for systematic reviews [18]:
-
1.
Population: older adultsFootnote 1 with and without subjective cognitive impairment (subjective cognitive impairment is a self-perceived worsening of cognitive functioning) [1, 2]
-
2.
Intervention: herbal and nutritional medicines (herbal medicines containing herbal substances or herbal preparations, and/or nutritional supplements/medicines containing vitamins, minerals, fatty acids etc., separately or in combination formulas) [11, 16]
-
3.
Comparisons: appropriate control group (non-active orally ingested placebo, orally ingested active control)
-
4.
Outcome: measures of cognition (both standardised/validated and non-standardised/non-validated testing measures)
-
5.
Study design: randomised control trials (parallel or cross-over)
The following are the inclusion criteria: chronic dosing studies over a period of 2 weeks or more, peer-reviewed articles fully accessible online and written in English that met the above PICOS criteria. The following are the exclusion criteria: reviews, case studies, editorials, conference proceedings, preclinical studies (both in vitro and in vivo), trial protocols, trial registrations, book chapters, abstracts only, peer-reviewed articles in which the study population had a diagnosis of mild cognitive impairment or dementia, did not include cognition as a primary or secondary endpoint, or employed a co-intervention such as cognitive training.
Search strategy
Two researchers (AEC, GZS) reviewed the search strategy in consultation with an experienced librarian, prior to the commencement of scoping. Four databases were searched for peer-reviewed articles: Cochrane, MEDLINE, CINAHL and PsycInfo from inception to 4 August 2018, and a further fifth database, EMBASE, was searched on 14 September 2022. Weekly alerts were established across the five databases until review finalisation on 18 September 2022. A full list of keywords is detailed below in Table 1. The only modification to the search strategy was the exclusion of non-randomised controlled trials from the Cochrane database to reduce the number of records for screening. Reference lists of included studies were also searched to identify any further eligible studies. Studies that included multiple age groups were also included if they reported demographics and outcomes separately for older participants in line with the eligibility criteria.
Data extraction and appraisal
All titles and abstracts were first screened by one author (AEC) for inclusion or exclusion from the review. If there were uncertainties regarding suitability for inclusion, the second reviewer (GZS) would assist to collaboratively make a final decision. Full-text articles were reviewed by the two authors with disagreements of acceptability resolved by discussion. Study characteristics were then extracted for each full-text article. These characteristics included author(s) and study location, aim, study population (group, sex, mean age, standard deviation and range), diagnosis criteria/global cognition measure, study design and outcome measurement frequencies, intervention, dose and duration, measures of cognition and results (cognition, retention, adherence and adverse events).
A methodological risk of bias assessment was conducted in accordance with the Cochrane Review Process for Randomised Trials (ROB 2) [19]. The quality of trial design, conduct and reporting of the included studies was assessed. Separate risk of bias assessments was conducted for parallel [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] and cross-over design studies [40]. The risk of bias tool evaluates five domains: bias arising from the randomisation process, deviations from intended interventions (effect of assignment and adherence to intervention), bias due to missing outcome data and in the measurement of the outcome, and bias in the selection of the reported result [19]. The sixth domain of bias arising from period and carryover effects was also evaluated for the cross-over study [19]. One author (AEC) independently conducted the risk of bias assessment, with the second author (GZS), reviewing the outcomes.
Individual studies were assessed as low risk, some concerns regarding methodology and high risk based on each of the above-mentioned domains. Studies with one or more domains assessed as high risk or with some concerns for multiple domains were deemed overall as high risk. Those with at least one domain with some concerns were evaluated in this category. The risk of bias process was conducted to assess the methodological quality of studies in their published form; study authors were not contacted for further information. A qualitative synthesis approach to this review was taken due to the large variation of interventions and cognitive assessments utilised across the studies, for each of the populations.
Results
Study selection
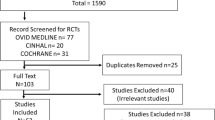
Figure 1 outlines the study selection process, with twenty-one studies meeting the eligibility criteria [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. Nine studies involved older adults with SCI [20,21,22, 26, 28, 33, 35, 37, 38], and the remaining twelve, older adults without SCI [23,24,25, 27, 29,30,31,32, 34, 36, 39, 40].
Study characteristics
Table 2 details a summary of the characteristics of the nine [20,21,22, 26, 28, 33, 35, 37, 38] SCI studies, and Table 3 details the twelve studies in older adults without SCI [23,24,25, 27, 29,30,31,32, 34, 36, 39, 40]. Both tables outline the study aim, population (group, sex, mean age, standard deviation and range), diagnosis/global cognition measure, design, intervention and dose, duration, measures of cognition and results (cognitive outcomes, retention and adherence, and adverse events).
Across both populations, all studies were randomised, double-blind, placebo-controlled trials [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. Twenty studies employed a parallel design [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39], and one study utilised a cross-over design [40]. Three studies utilised the same intervention with two different doses (three comparison groups in total, including placebo) [20, 22, 28], and one study utilised two different interventions compared to a single control [29].
Eight studies were conducted in the USA [24, 25, 27,28,29,30,31, 36], three each in Australia [23, 32, 38] and Italy [26, 33, 39], two in India [21, 35] and one each in Korea [20], the Netherlands [22], the UK [34], China [37] and Japan [40]. Two studies were published from 1995 to 1998 [22, 33], ten published between 2000 and 2010 [21, 23,24,25, 27, 30,31,32, 35, 36], with the remaining nine between 2012 and 2020 [20, 26, 28, 29, 34, 37,38,39,40].
Fifteen studies reported methods of recruitment [20, 22,23,24,25,26, 28, 29, 32, 35,36,37,38,39,40], with twelve studies conducted in community settings (audio, visual, and print media, universities) [20, 23,24,25, 28, 29, 32, 35,36,37,38, 40] and three in clinical settings (general practice and outpatient clinics) [22, 26, 39].
Participants
Across the included studies, the total sample size (at baseline) was N = 1891, with 19/21 studies reporting participant sex (N = 1798; 61% were female) [20,21,22,23,24,25, 28,29,30,31,32,33,34,35,36,37,38,39,40]. The mean age of participants reported across 20/21 studies was 65.43 years [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34, 36,37,38,39,40], SDpooled = 13.95 (for 17 studies) [20,21,22,23, 25, 27,28,29,30,31,32,33, 36,37,38,39,40]. Individual studies ranged from 28 [40] to 262 participants [31]. A total of 755 participants were from the nine SCI studies [20,21,22, 26, 28, 33, 35, 37, 38], compared to 1136 from the twelve studies in older adults without SCI [23,24,25, 27, 29,30,31,32, 34, 36, 39, 40].
Eligibility criteria and global cognition measures
All twenty-one studies utilised cognitive scales or tests [20,21,22, 25,26,27,28,29,30,31,32,33, 35, 36, 38, 39], medical questionnaires [23, 37], self-reports of cognitive function [22, 24, 26, 27, 29,30,31, 34, 40] or clinical questionnaires [23, 24, 32, 38], to determine the eligibility for their respective study. Nineteen of these studies utilised a validated measure to test cognitive functioning [20,21,22,23,24,25,26,27,28,29,30,31,32,33, 35, 36, 38,39,40]. Fifteen out of twenty-one studies utilised the Mini-Mental State Exam (MMSE), as a measure of global cognition [20,21,22, 25,26,27,28,29,30,31,32,33, 35, 36, 38, 39]. The MMSE cut-off score for participant inclusion varied between studies and populations. For SCI studies, one utilised a cut-off of ≥ 20 [22], another a range of 20–27 [26], one with ≤ 24 [35], four studies with a cut-off of ≥ 24 [21, 28, 33, 38] and one of ≥ 25 [20]. For studies on older adults without SCI, one reported a cut-off of ≥ 23 [29], one with a range of 24–29 [25], three with a cut-off of ≥ 24 [27, 30, 32], one ≥ 26 [31] and one each > 26 [36] and ≥ 27 [39]. Overall, studies with an SCI population reported lower cut-off scores and ranges for participant inclusion.
Other scales included the Blessed Orientation Memory Scale (BOMC) [24], Weschler Memory Scale (WMS) [28, 29, 35], Clinical Dementia Rating (CDR) Scale [20], Memory Complaint Questionnaire (MAC-Q) [28] and Short Portable Mental Status Questionnaire (SPMSQ) [29]. Overall, four studies utilised a global cognition measure as their primary or secondary outcome measure, with three of these using the MMSE [26, 29, 39], and one the WMS (logical subset score of < 6) [35].
Intervention and control type
Seventeen out of twenty-one studies used a herbal supplement [21, 23,24,25,26, 28,29,30,31,32,33, 35,36,37,38,39,40] with most studies utilising a form of Ginkgo biloba [23, 25, 29,30,31, 36,37,38] or Bacopa monnieri as a primary ingredient in their intervention [21, 24, 26, 32, 35, 39]. Two of these seventeen studies used a combination formula (one containing Ginkgo biloba and 45 other herbs, minerals and vitamins specifically made for women [38]) (the other containing Bacopa monnieri, lycopene, astaxanthin and vitamin B12 [39]). In addition, one study each used a spearmint extract (Mentha spicata L.) [28], a standardised ginseng extract (G115) [33] and a diosgenin-rich yam extract (diopower 15) containing vitamins, oils and beeswax [40], and one used a nutritional supplement (OPC Synergy® plus Catalyn) containing buckwheat, teas, and fruit and vegetable extracts, as a secondary intervention [29].
Two of the remaining four studies utilised a herbal combination via a liquid solution (Ginkgo biloba, alcohol/water solution [22] and SRM [Salvia officinalis L., Rosmarinus officinalis L. and Melissa officinalis L.]) [34], one study utilised a nutrient based juice (sweetened cranberry juice) [27], and one study used an oral capsule containing a type of fungus (Tremella fuciformis) [20]. Twenty out of twenty-one studies reported a method of administration [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34, 36,37,38,39,40] with ten administering the intervention orally via capsule [20, 21, 25, 26, 28,29,30, 33, 37, 40], seven utilised tablets [23, 24, 31, 32, 36, 38, 39] and three a liquid solution [22, 27, 34].
In terms of the control groups, all studies stated that they utilised a form of placebo. Nineteen out of twenty-one studies detailed the type of placebo employed [20,21,22,23,24,25,26,27,28, 30,31,32,33,34, 36,37,38,39,40], with ten studies utilising a capsule [20, 21, 25, 26, 28, 30, 33, 36, 37, 40], six a tablet [23, 24, 31, 32, 38, 39] and three an oral liquid [22, 27, 34]. Eight out of twenty-one studies (38%) provided some information on the ingredients contained in the placebo [22, 28, 29, 34, 36,37,38,39]. Five of these studies used a form of placebo containing active herbal or nutritional ingredients [22, 29, 34, 38, 39], with the remaining three using a placebo containing inert substances [28, 36, 37]. Overall, 17/21 studies stated that they matched their placebo with the intervention [20,21,22,23,24,25,26,27, 30,31,32,33, 36,37,38,39,40]. Nineteen out of the twenty-one studies sufficiently detailed the dose of intervention [20,21,22,23,24,25,26,27,28,29,30,31,32, 34,35,36, 38,39,40], and seventeen detailed the dose of placebo [20,21,22, 24,25,26,27,28, 30, 31, 33, 34, 36,37,38,39,40].
The total duration of studies ranged from 2 weeks [34] to 9 months [33]. The majority of studies were 12 weeks [21, 23, 24, 32, 35, 37], 6 weeks [27, 30, 31, 36] or 8 weeks [20, 26, 39] in length. Four studies employed a washout, run-in or withdrawal period; two before the trial began [22, 39], one between two cognitive testing periods (midpoint-12 weeks and endpoint-24 weeks) [21] and one for 6 weeks separating the intervention cross-over period [40]. One study utilised a 6-week placebo intake period for the control group, with 12 weeks of intervention for the treatment group [24].
Primary and secondary measures of cognition
Measures of cognition varied across the included studies. The most common were the Wechsler Adult Intelligence Scale (WAIS; n = 6) [21, 24, 27, 29, 31, 36], the Weschler Memory Scale (WMS; n = 6) [21, 27, 30, 31, 35, 36], the Rey Auditory Verbal Learning Test (RAVLT; n = 5) [21, 22, 24, 32, 39], the Stroop Colour and Word Test (SCWT; n = 4) [24, 27, 29, 30], the Trail Making Test (TMT; n = 4) [27, 29, 32, 39] and the Mini-Mental State Examination (MMSE; n = 4) [26, 29, 39, 40].
Retention and adherence
Nineteen of the twenty-one studies consistently reported retention, with an average retention rate of 92% across the studies [20,21,22,23,24,25,26, 28, 30,31,32,33,34,35,36,37,38, 38,39,40]. Comparatively, only 7/21 studies specifically reported treatment adherence, with an overall average of 93% across both intervention and placebo usage [20, 22, 24, 26, 28, 33, 38, 38].
Risk of bias within and across studies
Figures 2 and 3 (parallel studies) and Fig. 4 (cross-over study) provide a summary of each of the risk of bias domains, and an overall risk of bias assessment, for each of the twenty-one included studies. Green circles indicate that the domain or study has been evaluated as low risk, yellow as having some concerns and red as high risk.
Each article was assessed in terms of randomisation, intended interventions (effect of assignment and effect of adhering to the intervention), missing outcome data, measurement of outcomes and selection in reported results. In terms of the overall risk of bias assessment, only one study was deemed as low risk [26], some concerns were found for 6/21 studies [20, 24, 27, 28, 33, 39] and the remaining fourteen were deemed to be high risk [21,22,23, 25, 29,30,31,32, 34,35,36,37,38, 40]. Between populations, three SCI studies were assessed as having some concerns [20, 28, 33], five were deemed high risk [21, 22, 35, 37, 38] and one was deemed low risk [26]. For the non-SCI studies, three were assessed as having some methodological concerns [24, 27, 39], and the remaining nine were deemed as high risk [23, 25, 29,30,31,32, 34, 36, 40].
Despite all twenty-one studies stating the method of intervention assignment was randomised, only fourteen sufficiently detailed the randomisation process and were deemed as low risk [21,22,23, 25,26,27, 29,30,31,32, 36,37,38, 40]. Intended interventions (effect of assignment to interventions) were adequately reported in five studies (low risk) [20, 26, 28, 29, 36], nine were assessed as high risk [21,22,23, 25, 30,31,32, 38, 40] and the remaining seven have some concerns [24, 27, 33,34,35, 37, 39]. Thirteen studies were assessed as low risk for reporting on intended interventions (effect of adhering to the intervention) [20, 22,23,24, 26,27,28,29,30,31, 33, 38, 39] and eight as high risk [24, 29, 32, 34,35,36,37, 40].
In terms of missing outcome data (domain three), 17/21 studies were evaluated as low risk [20,21,22, 24, 26,27,28,29,30,31, 33,34,35,36,37, 39, 40], and the remaining four were assessed as high risk [23, 25, 32, 38]. Within domain 4 (measurement of outcomes), 18/21 studies were deemed as low risk [20,21,22,23,24,25,26,27,28,29,30,31,32,33, 36,37,38,39], and the remaining three were as high risk [34, 35, 40]. Eighteen out of twenty-one studies were assessed as low risk for selection in reported results (domain 5) [20,21,22, 24,25,26,27,28,29, 31,32,33,34,35,36,37,38,39], with some concerns for only three studies [23, 30, 40]. In terms of bias arising from period or carryover effects (domain S) in the cross-over study, this was deemed as low risk [40].
Study results
Results for all twenty-one studies are outlined below including intervention efficacy on cognitive function, adverse events and risk of bias.
Intervention efficacy in low risk of bias study
Only one study was deemed to be low risk for all domains, in terms of the overall methodological assessment. This 2017 randomised, double-blind placebo-controlled trial was conducted by Cicero and colleagues [26]. Participants were 30 older adults with self-perceived cognitive decline and ingested either a Bacopa monnieri formulation or a placebo capsule for 8 weeks; MMSE was measured at each time point. In terms of intervention efficacy, a significant increase in MMSE score was found from baseline to endpoint in the treatment arm. Furthermore, a significant increase in score was also found in the treatment group at the endpoint, compared to placebo, demonstrating a significant improvement in cognitive function for the intervention group across time and between groups [26]. Only one adverse event was reported an aftertaste from active product intake.
Intervention efficacy in remaining SCI studies
Across time, a significant improvement in at least one cognitive outcome for participants in the intervention group (compared to placebo) was found in 6/8 of the remaining SCI studies [20, 21, 28, 33, 35, 38]. Improvements were mostly found in the areas of memory (working, spatial, short-term, retention and logical) [20, 28, 33, 35, 38] and executive functioning [20, 21, 35]. Three of the eight studies utilised a capsule containing a herbal extract: one contained Bacopa monnieri [21], one spearmint extract (Mentha spicata L.) [28] and one standardised ginseng extract [33]. One study used a combination supplement (tablet), containing 46 herbs, vitamins and minerals (mainly consisting of Ginkgo biloba, Silybum marianum dry fruit (St. Mary’s thistle) and Vitis vinifera dry seed (grape seed)) [38]. An additional study utilised a capsule containing Tremella fuciformis (a type of fungus) [20], and the last study did not specify an administration method but used a standardised extract of Bacopa monnieri [35].
Of these six studies, mild to moderate adverse events were reported in three of them [28, 35, 38]. Knee pain, myalgia, headaches and heartburn were reported in the study conducted by Herrlinger and colleagues utilising Mentha spicata L. as their intervention [28]. These adverse events were reported for both the treatment and placebo groups; however, heartburn experienced by a participant in the 600 mg/day Mentha spicata L. group was deemed as ‘probably related’, compared to all other events deemed as ‘not related’ [28]. One participant withdrew due to maculopapular rashes in the intervention group (Bacopa monnieri), in the study conducted by Raghav and colleagues [35]. Two participants withdrew from the study conducted by Macpherson and colleagues using a combination formula containing Ginkgo biloba (intervention) [38]. One participant withdrew due to nausea and vomiting in the intervention group and one in the placebo group due to a mild rash [38].
In relation to the risk of methodological bias for all six SCI studies with an improvement in cognitive functioning, two of the studies utilising Bacopa monnieri [21, 35] and one using Ginkgo biloba (combination supplement) [38] were deemed as being high-risk. The remaining three were assessed as having some concerns in terms of methodological reporting [20, 28, 33].
For the two studies that did not find an improvement in cognitive functioning between groups (intervention cf. placebo) or across time, both reported adverse events with the use of Ginkgo biloba alcohol/water extract (drops) [22] and a herbal/dietary supplement also containing Ginkgo biloba [37]. Gastrointestinal upset was reported as the main adverse reaction for both studies [22, 37] with dizziness, headaches and sleep disturbance also reported in the Ginkgo biloba alcohol/water extract study [22]. In total, Brautigam and colleagues reported adverse events for 25 participants across both the placebo and intervention groups [22]. In terms of the second study, it is not known whether the two participants who reported adverse events were receiving the intervention or placebo [37]. Overall, both studies were deemed as high risk in terms of the methodological risk of bias assessment.
Intervention efficacy in non-SCI studies
Overall, 7/12 non-SCI studies reported a significant improvement in cognitive functioning in the intervention group (compared to placebo), across time [23, 24, 30,31,32, 39, 40]. The most common improvements were in memory (long-term storage, retrieval, delayed recall, recognition) [23, 24, 31, 32], executive functioning [24, 30, 39, 40] and language [30, 39, 40]. Two studies used a form of Ginkgo biloba capsule [23, 30]; one used a Ginkgo biloba tablet [31]; two used a form of Bacopa monnieri tablet [24, 32]; one used an antioxidant combination formula (tablet) containing Bacopa monnieri, lycopene, astaxanthin and vitamin B12 [39]; and one a diosgenin-rich yam extract capsule [40]. An additional study reported a significant improvement in executive functioning across time, using a combined herbal and nutritional supplement containing Ginkgo (Ginkgo Synergy® plus Choline) [29]. A significant improvement in verbal fluency was also found in the secondary intervention group (across time, compared to the Ginkgo and placebo groups) using OPC Synergy®, a dietary supplement (plus Catalyn) [29]. A further study using a Ginkgo biloba-based supplement found a significant improvement in a list learning strict task in the placebo group only, across time [25].
Seven of the nine total studies were deemed as having a high methodological risk of bias [23, 25, 29,30,31,32, 40], with the remaining two (using a form of Bacopa monnieri) having some concerns [24, 39]. Five of the nine studies reported adverse events, in both the placebo and intervention groups (Ginkgo or Bacopa monnieri interventions) [24, 25, 29, 31, 32]. An additional two studies reported adverse events only occurring in the intervention group using a Ginkgo biloba capsule [23] or an antioxidant combination formula containing Bacopa monnieri [39]. The most common events reported across 6/7 studies were gastrointestinal issues (including nausea, abdominal cramps, digestive problems) [24, 25, 31, 32] and sleep disturbance, with the use of Ginkgo biloba [23] or placebo [29]. Exacerbation of sinusitis (n = 1) and a serious but short-term event of hepatitis E (n = 1) were reported as non-treatment-related adverse events in the remaining study [39].
For the three remaining non-SCI studies, all reported no significant improvements across time in cognitive functioning (for both intervention and placebo groups), nor between groups [27, 34, 36]. One study used a Ginkgo tablet [36], one used a sweetened cranberry juice [27] and the other used a liquid solution of SRM Salvia officinalis L., Rosmarinus officinalis L. and Melissa officinalis L. [34].
Adverse events were monitored in two of the three studies; however, no events were reported in one (SRM solution) [34], and the other study did not report serious events or document mild/minor events (sweetened cranberry juice intervention) [27]. Two of the three studies were deemed as having a high methodological risk of bias [34, 36], and the remaining one had some concerns [27].
Discussion
Overall, twenty-one studies were identified for inclusion in this review, nine with an SCI population [20,21,22, 26, 28, 33, 35, 37, 38] and twelve studies utilising older adults without SCI [23,24,25, 27, 29,30,31,32, 34, 36, 39]. Outcomes were mainly positive, with 14/21 studies overall reporting improvements in at least one area of cognitive functioning across time, in the intervention group (compared to placebo) [20, 21, 23, 24, 26, 28, 30,31,32,33, 35, 38,39,40]. Overall, only one study (using an SCI population) was assessed as having a low methodological risk of reporting, conduct and quality of trial design bias [26]. Due to the heterogeneous nature of eligible studies (including cognitive measures and interventions used and the type of data analysis and reporting conducted) and the large number of studies (14/21) with a high methodological risk of bias [21,22,23, 25, 29,30,31,32, 34,35,36,37,38, 40], a certainty of evidence analysis (GRADE) was not conducted.
Extent of literature using herbal and nutritional medicines for older adults with and without SCI
Despite the growing interest in the prevention and treatment of cognitive decline in older adults [8, 9], review search outcomes were not reflective of this interest, given that most of the articles eligible for this review were conducted prior to 2018. Editorials, book chapters, reviews and opinion articles seem to be more common formats of evidence, compared to research using the ‘gold standard’ method, randomised control trials (RCTs) [41, 42] (Fig. 1).
Measurement of cognitive change was not common in the literature; rather, relevant population studies focussed on biochemistry or progression to MCI or dementia. This was an unexpected outcome during the records search. Cognitive testing and assessment are generally affordable and accessible methods of providing insights into an individual’s current cognitive functioning and any decline over time [43]. However, there are currently no recommendations for specific primary or secondary outcome measures of cognition to determine a clinically significant improvement in cognitive function [44]. It has recently been recommended that composite outcomes including the monitoring of dementia risk factors alongside changes in cognition may be advantageous in preclinical dementia [44].
For cognitive outcome measures, an effect size of 0.40 has been reported as a clinically meaningful improvement for cognitive training interventions in healthy older adults and those with MCI or dementia [45]. This could be applied in studies utilising cognitive outcomes in people with SCI to determine whether a change in cognitive function is clinically meaningful, particularly in light of potential ceiling effects in this relatively unimpaired group. Future research should strive to investigate appropriate cognitive measures to detect a clinically significant change in SCI and implement gold standard, high-quality research methods to produce informative and translational outcomes.
Study characteristics
In terms of participant characteristics, across the twenty-one studies, there were more females (61%) compared to male participants. It is difficult to ascertain the true difference in the prevalence of SCI between the sexes, as a larger number of females (rather than males) are participating in these studies. Furthermore, inconsistencies in reporting prevalence between the sexes are typical in this field, again making it hard to determine whether SCI affects more females or males [2]. However, research within the area of cognitive decline suggests that females have a greater cognitive reserve but have a faster rate of cognitive decline (particularly, in the areas of global cognition and executive function) compared to males [46]. This outcome has been confirmed in dementia research. Dementia is reported to be the leading cause of death in women, with twice as many females compared to males being affected by the disease [47]. Further SCI prevalence research needs to be conducted to determine the true prevalence of SCI, between the sexes.
A high number of older adults reporting SCI are within the 60–64 year age range [2], compared to studies included in this review that saw an overall average age of 65 years for participants. Sex and age outcomes derived from this review highlight the importance of finding a way to address low research participation in males and monitoring the faster rate of female decline.
In terms of participant retention and adherence to treatment, these were both surprisingly high across the studies at an average of 92% and 93%, respectively, despite the literature suggesting these figures are quite difficult to achieve [48]. These outcomes should be considered with caution due to the subpar methodologies used to treat missing values.
Study methodologies
Reflective on previous research, the eligibility criteria for participation across the SCI and non-SCI studies were inconsistent [8, 9], with varying scales, tests and questionnaires used, particularly for the MMSE [20,21,22, 25,26,27,28,29,30,31,32,33, 35, 36, 38, 39]. Research investigating the diagnostic accuracy (sensitivity, specificity, positive and negative predictive power) of MMSE cut-off scores in detecting cognitive dysfunction found that scores of ≤ 26 showed optimal sensitivity and specificity balance, with a correct classification of MCI and dementia in older adults to be 90% [49]. The varying MMSE cut-offs used here (≥ 20, > 25 and ≤ 24) may have incorrectly classified participants (with and without SCI), potentially impacting the study outcomes. This interpretation is further supported by the identification of all eligible studies in this review not using a combination of self-report cognitive concerns (in line with the definition of SCI), cognitive scales (such as the MMSE), a general health questionnaire (including non-diagnosis of MCI or dementia) and screening of mental health conditions. Reliability on only one or two measures for classification of an impairment (or no impairment) is problematic and certainly requires future attention within this area of clinical practice and research.
An additional concern regarding the methodologies of accepted studies in this review is the large number of those deemed as having a high risk of bias, particularly within the bias due to assignment and adherence domains [21,22,23, 25, 29,30,31,32, 34,35,36,37,38, 40]. Either intention-to-treat (ITT) or modified intention-to-treat (mITT) approaches were not employed for participants with missing outcomes or outlier data, with participants being excluded completely from the analysis despite being randomised. Future studies in this field should consider using appropriate analysis to treat missing or outlier data, for post-randomisation outcomes as detailed above. The blinding of participants and other individuals involved in the trial was also identified as a concern. However, it is difficult to ascertain whether it was in fact the blinding process itself that was not conducted appropriately in these studies or if it was simply not reported sufficiently according to the ROB assessment standards. Future studies should look to adopting greater transparency and accuracy in the process (specifically stating who was blinded and how), as this would go a long way in demonstrating non-biassed outcomes.
Intervention efficacy on cognitive function and safety
Despite the majority of studies reporting positive results [20, 21, 23, 24, 26, 28, 30,31,32,33, 35, 38,39,40], a large number of these were deemed as having an overall high methodological risk of bias [21, 23, 30,31,32, 35, 38, 40]. These methodological concerns unfortunately do not assist in determining the true efficacy of herbal and nutritional medicines on cognitive functioning for older adults with and without SCI. This is particularly the case for Ginkgo biloba [23, 25, 29,30,31, 36,37,38] and Bacopa monnieri [21, 24, 26, 32, 35, 39], given how common they were as interventions across the accepted studies of this review.
The efficacy of Ginkgo biloba has been consistently unclear across the spectrum of cognitive decline. An earlier review investigating RCTs using Ginkgo biloba for the treatment of dementia [50] highlighted the concerns around the low quality of studies available, namely to do with utilisation of unsatisfactory methods. However, on a positive note, adverse effects found with the use of Ginkgo biloba (across the accepted studies in this review) appeared to be consistent with those reported with the use of a placebo [23, 29, 31, 38], indicating that Ginkgo biloba may be comparable in terms of safety with placebo intake. These results are in line with what has been found previously in a dementia population [50].
Strengths and limitations of the review
This review had several strengths. A broad and extensive literature search was conducted (in accordance with the aims and PICOS criteria of the review), comprehensively summarising the overall current state of the field. The lack of high-quality research has been addressed, highlighting the specific aspects which require improvement in future studies. The concerns surrounding the classification of SCI and the disparities between current research outcomes and clinical statistics have been presented.
There were a number of limitations to this review. First, the establishment of article alerts from 2018 until the completion of the review meant that despite the authors’ best efforts to monitor the addition of newly published research in each database, it is acknowledged that alerts may not have been the most appropriate way to capture all potential studies for inclusion. Furthermore, a meta-analysis was not feasible due to the inconsistent classification of SCI and non-SCI samples and the varying cognitive testing measures. The infancy of this area of research (despite broad interest from the general public) makes it difficult to conduct such an analysis at this time. The population was difficult to define due to the inherent heterogeneity of definitions and lack of consensus within the field, particularly with reference to the age range selected (despite being guided by the US CDC’s definition), and the terminology and language used (e.g. person-centred terminology). It is also acknowledged that the current review did not take into consideration the varying terminology utilised to classify ‘older adults’. The exclusion of non-English language studies, the initial article screening conducted by one reviewer and the search strategy developed in consultation with only one librarian were further limitations.
Recommendations for future research
First and foremost, an increased understanding and awareness of the features and characteristics of SCI needs to occur [8, 9]. This should be considered in collaboration with the difference between the presentation of older adults without SCI and those with MCI, in line with the cognitive decline continuum [2]. Future research should aim at clarifying the characteristics, classification measures and features of SCI to allow for more homogeneous sample classification. Overall, by better understanding of SCI, this may provide greater support for outcomes in high-quality efficacy studies utilising herbal and nutritional medicines as a means of managing self-perceived (or subtle) cognitive decline and, ideally, lowering dementia risk or facilitating the secondary prevention of dementia.
The development of a standardised outcome measure package (including cognitive testing, medical questionnaires, self-reports and mental health questionnaires) for use in SCI clinical trials would be the next step in moving the field forward. Increased accuracy in the differentiation between healthy older adults (without SCI) and those with SCI would assist in determining whether herbal and nutritional medicines have a positive effect on cognitive outcomes for this population.
Conclusions
Whilst most studies deemed eligible for inclusion in the review found positive results (particularly, those that used Ginkgo biloba or Bacopa monnieri), these outcomes need to be considered with caution, due to the high risk of methodological bias found. The literature in this area is in its infancy, with concerns around population and intervention heterogeneity evident. The use of supplements for cognition by older people is an area that attracts much interest from the community, yet our review shows that high-quality research on efficacy and safety is somewhat lagging.
This review has provided an insight into the current state and quality of the literature on the safety and efficacy of cognitive function of herbal and nutritional medicines in older adults with and without SCI.
Availability of data and materials
Not applicable.
Notes
Older adults (with and without SCI) were defined as aged 45 years and older, in accordance with the US Centers for Disease Control and Prevention (CDC) population-based statistics on Subjective Cognitive Decline and Aging [7].
References
Cedars Sinai. Subjective cognitive impairment (SCI). 2021. https://www.cedars-sinai.org/health-library/diseases-and-conditions/s/subjective-cognitive-impairment-sci.html. Accessed on 1 Jan 2022.
Röhr S, Pabst A, Riedel-Heller SG, Jessen F, Turana Y, Handajani YS, et al. Estimating prevalence of subjective cognitive decline in and across international cohort studies of aging: a COSMIC study. Alzheimers Res Ther. 2020;12(1):1–14. https://doi.org/10.1186/s13195-020-00734-y.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9. https://doi.org/10.1016/j.jalz.2011.03.008.
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–92. https://doi.org/10.1016/j.jalz.2011.03.003.
Pike KE, Cavuoto MG, Li L, Wright BJ, Kinsella GJ. Subjective cognitive decline: level of risk for future dementia and mild cognitive impairment, a meta-analysis of longitudinal studies. Neuropsychol Rev. 2021. https://doi.org/10.1007/s11065-021-09522-3.
van Harten AC, Mielke MM, Swenson-Dravis DM, Hagen CE, Edwards KK, Roberts RO, et al. Subjective cognitive decline and risk of MCI: the Mayo Clinic study of aging. Neurology. 2018;91(4):e300–12. https://doi.org/10.1212/WNL.0000000000005863.
Centers for Disease Control and Prevention. Subjective cognitive decline—a public health issue. 2019. https://www.cdc.gov/aging/data/subjective-cognitive-decline-brief.html. Accessed on 10 Sep 2022.
Si T, Xing G, Han Y. Subjective cognitive decline and related cognitive deficits. Front Neurol. 2020;11:1–13. https://doi.org/10.3389/fneur.2020.00247.
Bhome R, Berry AJ, Huntley JD, Howard RJ. Interventions for subjective cognitive decline: systematic review and meta-analysis. BMJ Open. 2018;8:1–10. https://doi.org/10.1136/bmjopen-2018-021610.
U.S. Department of Health and Human Services, National Institutes of Health. National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What’s In a Name? 2021. https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name. Accessed on 3 Feb 2022.
World Health Organization. WHO global report on traditional and complementary medicine 2019. 2019. https://apps.who.int/iris/handle/10665/312342. Accessed on 1 Jan 2022.
Than MC, Anam A, Nurfarahi K, Asma’ A, Hayati MY. Knowledge, use of complementary alternative medicine and health-related quality of life among cardiovascular disease patients. Food Res. 2019;3(5):604–16. https://doi.org/10.26656/fr.2017.3(5).118.
Raja R, Kumar V, Khan MA, Sayeed KA, Hussain SZM, Rizwan A. Knowledge, attitude, and practices of complementary and alternative medication usage in patients of type II diabetes mellitus. Cureus. 2019;11(8):1–12. https://doi.org/10.7759/cureus.5357.
Steiner GZ, Mathersul DC, MacMillan F, Camfield DA, Klupp NL, Seto SW, et al. A systematic review of intervention studies examining nutritional and herbal therapies for mild cognitive impairment and dementia using neuroimaging methods: study characteristics and intervention efficacy. Evid Based Complement Alternat Med. 2017;1–21. https://doi.org/10.1155/2017/6083629.
Steiner GZ, George ES, Metri N, MacMillan F, Dubois S, Moyle W, et al. Use of complementary medicines and lifestyle approaches by people living with dementia: exploring experiences, motivations and attitudes. Int J Older People Nurs. 2021;16(5). https://doi.org/10.1111/opn.12378.
Agbabiaka TB, Wider B, Watson LK, Goodman C. Concurrent use of prescription drugs and herbal medicinal products in older adults: a systematic review. Drugs Aging. 2017;34(12):891–905. https://doi.org/10.1007/s40266-017-0501-7.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021(71):1–9. https://doi.org/10.1136/bmj.n71.
Petticrew M, Roberts H. Starting the review: refining the question and defining the boundaries. In: Systematic reviews in the social sciences. USA: Wiley; 2006. p. 27–56. https://doi.org/10.1002/9780470754887.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:1–8. https://doi.org/10.1136/bmj.l4898.
Ban S, Lee SL, Jeong HS, Lim SM, Park S, Hong YS, et al. Efficacy and safety of Tremella fuciformis in individuals with subjective cognitive impairment: a randomized controlled trial. J Med Food. 2018;21(4):400–7. https://doi.org/10.1089/jmf.2017.4063.
Barbhaiya HC, Desai RP, Saxena VS, Pravina K, Wasim P, Geetharani P, et al. Efficacy and tolerability of BacoMind® on memory improvement in elderly participants: a double blind placebo controlled study. J Pharmacol Toxicol. 2008;3(6):425–34. https://doi.org/10.3923/jpt.2008.425.434.
Brautigam MRH, Blommaert FA, Verleye G, Castermans J, Jansen Steur ENH, Kleijnen J. Treatment of age-related memory complaints with Ginkgo biloba extract: a randomized double blind placebo-controlled study. Phytomedicine. 1998;5(6):425–34. https://doi.org/10.1016/S0944-7113(98)80038-X.
Burns NR, Bryan J, Nettelbeck T. Ginkgo biloba: no robust effect on cognitive abilities or mood in healthy young or older adults. Hum Psychopharmacol Clin Exp. 2006;21(1):27–37. https://doi.org/10.1002/hup.739.
Calabrese C, Gregory WL, Leo M, Kraemer D, Bone K, Oken B. Effects of a standardized Bacopa monnieri extract on cognitive performance, anxiety, and depression in the elderly: a randomized, double-blind, placebo-controlled trial. J Altern Complement Med. 2008;14(6):707–13. https://doi.org/10.1089/acm.2008.0018.
Carlson JJ, Farquhar JW, DiNucci E, Ausserer L, Zehnder J, Miller D, et al. Safety and efficacy of a Ginkgo biloba–containing dietary supplement on cognitive function, quality of life, and platelet function in healthy, cognitively intact older adults. J Am Diet Assoc. 2007;107(3):422–32. https://doi.org/10.1016/j.jada.2006.12.011.
Cicero AF, Bove M, Colletti A, Rizzo M, Fogacci F, Giovannini M, et al. Short-term impact of a combined nutraceutical on cognitive function, perceived stress and depression in young elderly with cognitive impairment: a pilot, double-blind, randomized clinical trial. J Prev Alzheimers Dis. 2016;4(1):12–5. https://doi.org/10.14283/jpad.2016.110.
Crews WD, Harrison DW, Griffin ML, Addison K, Yount AM, Giovenco MA, et al. A double-blinded, placebo-controlled, randomized trial of the neuropsychologic efficacy of cranberry juice in a sample of cognitively intact older adults: pilot study findings. J Altern Complement Med. 2005;11(2):305–9. https://doi.org/10.1089/acm.2005.11.305.
Herrlinger KA, Nieman KM, Sanoshy KD, Fonseca BA, Lasrado JA, Schild AL, et al. Spearmint extract improves working memory in men and women with age-associated memory impairment. J Altern Complement Med. 2018;24(1):37–47. https://doi.org/10.1089/acm.2016.0379.
Lewis JE, Melillo AB, Tiozzo E, Chen L, Leonard S, Howell M, et al. A double-blind, randomized clinical trial of dietary supplementation on cognitive and immune functioning in healthy older adults. BMC Complement Altern Med. 2014;14:1–9. https://doi.org/10.1186/1472-6882-14-43.
Mix JA, Crews WD. An examination of the efficacy of Ginkgo biloba extract EGb 761 on the neuropsychologic functioning of cognitively intact older adults. J Altern Complement Med. 2000;6(3):219–29. https://doi.org/10.1089/acm.2000.6.219.
Mix JA, Crews WD. A double-blind, placebo-controlled, randomized trial of Ginkgo biloba extract EGb 761® in a sample of cognitively intact older adults: neuropsychological findings. Hum Psychopharmacol Clin Exp. 2002;17(6):267–77. https://doi.org/10.1002/hup.412.
Morgan A, Stevens J. Does Bacopa monnieri improve memory performance in older persons? Results of a randomized, placebo-controlled, double-blind trial. J Altern Complement Med. 2010;16(7):753–9. https://doi.org/10.1089/acm.2009.0342.
Neri M, Andermarcher E, Pradelli JM, Salvioli G. Influence of a double blind pharmacological trial on two domains of well-being in subjects with age associated memory impairment. Arch Gerontol Geriatr. 1995;21(3):241–52. https://doi.org/10.1016/0167-4943(95)00659-9.
Perry NSL, Menzies R, Hodgson F, Wedgewood P, Howes MJR, Brooker HJ, et al. A randomised double-blind placebo-controlled pilot trial of a combined extract of sage, rosemary and melissa, traditional herbal medicines, on the enhancement of memory in normal healthy subjects, including influence of age. Phytomedicine. 2018;39:42–8. https://doi.org/10.1016/j.phymed.2017.08.015.
Raghav S, Singh H, Dalal P, Srivastava J, Asthana O. Randomized controlled trial of standardized Bacopa monniera extract in age-associated memory impairment. Indian J Psychiatry. 2006;48(4):238–42. https://doi.org/10.4103/0019-5545.31555.
Solomon PR, Adams F, Silver A, Zimmer J, DeVeaux R. Ginkgo for memory enhancement: a randomized controlled trial. JAMA. 2002;288(7):835–40. https://doi.org/10.1001/jama.288.7.835.
Zhu J, Shi R, Chen S, Dai L, Shen T, Feng Y, et al. The relieving effects of BrainPower Advanced, a dietary supplement, in older adults with subjective memory complaints: a randomized, double-blind, placebo-controlled trial. Evid Based Complement Alternat Med. 2016;2016:1–16. https://doi.org/10.1155/2016/7898093.
Macpherson H, Ellis KA, Sali A, Pipingas A. Memory improvements in elderly women following 16 weeks treatment with a combined multivitamin, mineral and herbal supplement: a randomized controlled trial. Psychopharmacology. 2012;220(2):351–65. https://doi.org/10.1155/2016/7898093.
Crosta F, Stefani A, Melani F, Fabrizzi P, Nizzardo A, Grassi D, et al. Improvement of executive function after short-term administration of an antioxidants mix containing bacopa, lycopene, astaxanthin and vitamin B12: the BLAtwelve study. Nutrients. 2020;13(1):56. https://doi.org/10.3390/nu13010056.
Tohda C, Yang X, Matsui M, Inada Y, Kadomoto E, Nakada S, et al. Diosgenin-rich yam extract enhances cognitive function: a placebo-controlled, randomized, double-blind, crossover study of healthy adults. Nutrients. 2017;9(10):1–13. https://doi.org/10.1155/2016/7898093.
Akobeng AK. Understanding randomised controlled trials. Arch Dis Child. 2005;90(8):840–4. https://doi.org/10.1136/adc.2004.058222.
Hariton E, Locascio JJ. Randomised controlled trials - the gold standard for effectiveness research: study design: randomised controlled trials. BJOG Int J Obstet Gynaecol. 2018;125(13):1716–1716. https://doi.org/10.1111/1471-0528.15199.
Frerichs R, Tuokko H. A comparison of methods for measuring cognitive change in older adults. Arch Clin Neuropsychol. 2005;20(3):321–33. https://doi.org/10.1016/j.acn.2004.08.002.
Rentz DM, Wessels AM, Annapragada AV, Berger A, Edgar CJ, Gold M, et al. Building clinically relevant outcomes across the Alzheimer’s disease spectrum. Alzheimers Dement Transl Res Clin Interv. 2021;7(1):e12181. https://doi.org/10.1002/trc2.12181.
Yun S, Ryu S. The effects of cognitive-based interventions in older adults: a systematic review and meta-analysis. Iran J Public Health. 2022;51(1):1–11. https://doi.org/10.18502/ijph.v51i1.8286.
Levine DA, Gross AL, Briceño EM, Tilton N, Giordani BJ, Sussman JB, et al. Sex differences in cognitive decline among US adults. JAMA Netw Open. 2021;4(2):1–13. https://doi.org/10.1001/jamanetworkopen.2021.0169.
Australian Government, Australian Institute of Health and Welfare. Dementia-Snapshot. 2020. https://www.aihw.gov.au/reports/australias-health/dementia. Accessed on 3 Feb 2022.
Zheng W, Chang B, Chen J. Improving participant adherence in clinical research of traditional Chinese medicine. Evid Based Complement Alternat Med. 2014;2014(376058):1–5. https://doi.org/10.1155/2014/376058.
O’Bryant SE, Humphreys JD, Smith GE, Ivnik RJ, Graff-Radford NR, Petersen RC, et al. Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol. 2008;65(7):963–7. https://doi.org/10.1001/archneur.65.7.963.
Birks J, Grimley EJ. Ginkgo biloba for cognitive impairment and dementia (review). Cochrane Database Syst Rev. 2009;1:1–75. https://doi.org/10.1002/14651858.CD003120.pub3.
Acknowledgements
Not applicable.
Funding
AEC’s contribution was supported by PhD scholarship from FIT-BioCeuticals Pty Ltd. and NICM Health Research Institute, Western Sydney University. GZS’s contribution was supported by funding from a National Health and Medical Research Council (NHMRC)-Australian Research Council (ARC) Dementia Research Development Fellowship (APP1102532) and an NHMRC Investigator Grant (APP1195709). The funders played no role in this study.
Author information
Authors and Affiliations
Contributions
AEC and GZS contributed to the conceptualisation and design of the review. AEC took the lead in drafting the review paper. GZS provided guidance throughout. All authors provided critical feedback and reviewed the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
As a medical research institute, NICM Health Research Institute receives research grants and donations from foundations, universities, government agencies, individuals, and industry. Sponsors and donors provide untied funding for work to advance the vision and mission of the institute. The project that is the subject of this article was not undertaken as part of a contractual relationship with any organisation other than the funding declared below. It should also be noted that NICM conducts clinical trials relevant to this topic area, for which further details can be provided on request. AEC has received PhD scholarship support from FIT-BioCeuticals Pty Ltd.; the funder played no role in this study. AEC, DHC, and GZS are all based at NICM Health Research Institute but have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cave, A.E., Chang, D.H., Münch, G.W. et al. A systematic review of the safety and efficacy on cognitive function of herbal and nutritional medicines in older adults with and without subjective cognitive impairment. Syst Rev 12, 143 (2023). https://doi.org/10.1186/s13643-023-02301-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02301-6