Abstract
Background
Patients receiving thoracic aortic repair suffer from long-term impairment in daily functioning and quality of life following intervention due to a combination of their life-threatening condition (i.e. aortic aneurysm or dissection), undergoing major surgery, as well as long-term exercise restrictions thereafter. Despite the known risks of exercise, it is vital that patients regain physical activity in order to recover their daily functioning and quality of life. Cardiac rehabilitation could be a safe and effective treatment to support patients to become physically active by providing exercise training, comprehensive rehabilitation services, and safety recommendations. Despite new insights in recent literature and clinical practice, international guidelines do not recommend cardiac rehabilitation due to limited evidence. We aim to fill this knowledge gap by performing a systematic review and meta-analysis on the effectiveness of cardiac rehabilitation in patients following thoracic aortic repair.
Methods
This protocol has been developed following the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P). MEDLINE, Embase, and CINAHL will be searched for eligible observational and interventional studies from inception up to April 2022. Screening (title/abstract and full text), data extraction, risk of bias assessment, and therapeutic validity rating will be conducted by two independent reviewers. A random-effects model will be used to meta-analyse performance-based outcomes, patient-reported outcomes, clinician-reported outcomes, and researcher-reported outcomes. Subsequently, meta-bias and confidence in evidence will be analysed by two independent reviewers.
Discussion
To exercise or not to exercise in patients following thoracic aortic repair has been a topic of discussion for years. The intended systematic review and meta-analysis will provide comprehensive evidence on the effectiveness of phase III outpatient exercise-based cardiac rehabilitation in patients following thoracic aortic repair. Findings from this review may inform future guidelines for the management of patients with thoracic aortic disease.
Systematic review registration
PROSPERO CRD42022301204.
Similar content being viewed by others
Background
Thoracic aortic aneurysm or dissection, also known as thoracic aortic disease, is a life-threatening condition [1]. The incidence of thoracic aortic disease is 3–9 per 100,000 people per year [2]. There are surgical techniques to repair thoracic aortic disease via sternotomy, thoracotomy, thoracophrenolaparotomy or endovascular procedures with increasing survival rates in recent decades [3]. However, results following surgery show that patients suffer from long-term impairment in daily functioning and quality of life [4, 5]. Furthermore, there is a risk of aneurysm or dissection in another part of the aorta [6].
Cardiac rehabilitation could be a promising strategy to improve outcomes such as daily functioning and quality of life following thoracic aortic repair. It consists of several core components, including exercise training, lifestyle coaching, medication monitoring to support cardio-vascular risk reduction, healthy behaviour, psychosocial well-being, and an active lifestyle in patients with heart disease [7]. The effects of cardiac rehabilitation are well known for patients with heart failure [8], coronary heart disease [9], and following cardiac surgery [10]. For example, patients with heart failure improved standardised exercise capacity (standardised mean difference 0.98, 95% confidence interval 0.59 to 1.37) [11] and walking capacity (mean 21.0 m; 95% confidence interval 1.57 to 40.4 m) [12] after cardiac rehabilitation compared to controls. Furthermore, patients with coronary artery disease increased health related quality of life (standardised mean change 0.28, 95% confidence interval 0.05 to 0.50) after cardiac rehabilitation [13]. Much less is known about the outcomes of cardiac rehabilitation in patients following thoracic aortic repair.
International guidelines are restraint on cardiac rehabilitation recommendations for patients following thoracic aortic repair. The 2010 ACCF/AHA guideline [14] and 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases [15] do not specify cardiac rehabilitation. Both guidelines recommend to support physically active behaviour and regular aerobic exercise in patients, however, they do not provide treatment strategies for healthcare professionals [14, 15]. The only recommendation is to avoid isometric exercise, strenuous (weight)lifting, pushing and straining (Level III evidence) as this might lead to a superimposed increase in intrathoracic pressure with systolic pressures reaching 300 mmHg that might trigger new aortic rupture [14, 16]. The 2020 ESC guidelines on sports cardiology provide a risk classification and recommends to avoid high and very high intensity exercise, contact, and power-sports [17]. Unfortunately, no recommendations on how to restart other types of exercise are provided. The 2014 Canadian Cardiovascular Society guideline [18] is the first to mention cardiac rehabilitation in patients following thoracic aortic repair as a safe treatment with the potential to reduce mortality. However, they formulated no official treatment recommendation due to a lack of high-quality evidence.
Recent studies indicate that there is an urgent need for cardiac rehabilitation in patients following thoracic aortic repair [4, 5, 19,20,21]. Patients are challenged by severe exercise restrictions that impair daily functioning and quality of life [5]. An increasing body of evidence questions the need for exercise restrictions and indicate they can do more harm than good [4, 19]. Restrictions result in sedentary behaviour, while being physically active is of great importance for this at-risk patient population [4]. Improving physical activity by cardiac rehabilitation must of course be safe, however, this seems possible by applying safety recommendations such as (1) an early start, (2) tight control of blood pressure, (3) specific training instructions, and (4) strictly avoid competitive sports and isometric training [20]. To our knowledge, there are currently no outcomes known of cardiac rehabilitation in patients following thoracic aortic repair. Although this is important to consider both benefits and risks. Therefore, the main objective of this study is to systematically review current literature and perform a meta-analysis on the outcomes (i.e. daily functioning and quality of life) after cardiac rehabilitation in patients following thoracic aortic repair.
Methods
Design
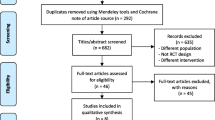
Our study protocol follows the Preferred Items for Systematic Reviews and Meta-Analysis – protocol (PRISMA-P) statement [22] and has been registered on PROSPERO CRD42022301204. The systematic review and meta-analysis will be reported in accordance with the PRISMA 2020 statement [23]. The start of the review will be April 2022 and the estimated date for completion is set to December 2022. A summary of the study design is provided in Fig. 1.
Information sources
A comprehensive electronic search will be conducted in MEDLINE (Ovid), Embase (Ovid), and CINAHL (Cumulative Index to Nursing and Allied Health Literature) Plus (EBSCO) from inception up to April 2022. Additional studies will be identified from (1) reviewing the reference lists of eligible full-text studies through a hand search (backward citation searching) and (2) screening studies that cited the eligible full-text studies according to Web of Science (forward citation searching). Conference proceedings, bibliographies of systematic reviews and trial registers will not be searched. No language or other limitations will be used.
Search strategy
Observational studies (i.e. cohort studies and registries) and interventional studies (i.e. pilot studies and randomised controlled trials) will be searched for outcomes after cardiac rehabilitation. The search fields ‘Title’, ‘Abstract’, and ‘Medical Subject Headings (MeSH)/Thesaurus’ will be applied to ensure the best possible study retrieval. Detailed search strategies will be developed for each electronic database searched with input from a medical librarian (online supplementary file 1). Pre-searches in MEDLINE to identify search terms and develop a search string were conducted in January-March 2022.
Eligibility criteria
We will include observational and interventional studies reporting outcomes after phase III cardiac rehabilitation in patients following surgical repair of thoracic aortic aneurysm or dissection. Details of the eligibility criteria are provided in Table 1.
Study selection
Retrieved studies will be uploaded to Rayyan software (Rayyan Systems Inc.) [24]. After removing duplicates, two reviewers (NK and HvZ) will independently screen the study against the eligibility criteria. Full text of the (potentially) eligible studies will be thoroughly assessed for inclusion. Reasons for full-text exclusion will be reported (i.e. wrong patient population, wrong outcomes, or wrong intervention). For studies without an available abstract, full-text articles will be obtained unless the article can be confidently excluded by its title alone. Disagreements will be solved by consensus. Where no consensus can be reached, a third party (TS) will arbitrate. In the event of multiple studies reporting findings on the same population, the study with the largest study population will be included. The process of study selection will be summarised using a PRISMA flow diagram [23].
Data collection and data management
Data on study characteristics, participant characteristics, and interventions will be extracted to a predefined Excel sheet by two independent reviewers (NK and HvZ). Extracted data will include information on study author(s), year of publication, journal, study design, inclusion criteria, exclusion criteria, number of participants, outcome measures, and follow-up. Details regarding participants in each study will include sex, age, cardiovascular risk factors (i.e. active smoker, alcohol abuse, abdominal circumference, body mass index, diabetes mellitus, dyslipidaemia, family history, and medically treated hypertension), pharmaceutical treatment (i.e. beta blockers), diagnosis received (i.e. aneurysm versus dissection), and medical history (i.e. connective tissue disease such as Marfan or Loeys-Dietz). Details of the intervention will be extracted about the rehabilitation program (frequency, intensity, time per session, duration, and type of exercise training [25]; content of education; specifics of psychological input; and safety recommendations) and surgery (type of surgery and level of surgery).
Outcomes
Data on outcomes will be extracted to the predefined Excel sheet by two reviewers independently (NK and HvZ). Depending on the data reported in the studies, we will collect the raw data, the aggregated outcomes or both. In studies reporting aggregated data, the estimates (i.e. means and medians) will be extracted along with their variation (i.e. 95% confidence intervals, standard error, standard deviation, or range). Details of the outcomes will be extracted about performance-based, patient-reported, clinician-reported, and researcher-reported outcomes (Table 1).
Risk of bias
The Risk of Bias In Non-randomised Studies of Interventions (ROBINS-I) tool will be used to assess the risk of bias of non-randomised interventional studies [26]. Studies will be independently assessed by two reviewers (NK and HvZ) on confounding, selection bias, information bias, and reporting bias. The Cochrane Risk of Bias Tool 2.0 will be used for randomised interventional studies and independently assessed on the following domains: randomisation process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results [27].
Therapeutic validity
Therapeutic validity will be scored with the International Consensus on Therapeutic Exercise and Training (i-CONTENT) tool and considers the following seven items: patient selection, dosage of exercise program, type of exercise program, qualified supervisor, type and timing of outcome assessment, safety of exercise program, and adherence to exercise program (online supplementary file 2) [28]. Two reviewers (NK and HvZ) will independently rate the therapeutic validity of the cardiac rehabilitation programmes as either “low risk” or “high risk” of ineffectiveness of the exercise intervention. In case of uncertainty, the item will be evaluated as “probably done” or “probably not done”. Each evaluation will be substantiated with a rationale, which is essentially more important than the low-risk or high-risk score itself.
Missing data
We will try to contact the original investigators to request missing data. If estimates and variation (i.e. mean and 95% confidence intervals) were reported differently between studies (i.e. median and range), the formula of Hozo et al. [29] will be used to estimate mean and 95% confidence intervals with use of median, range, and sample size. Headrick’s formula [30] will be used to combine means when separate means describe results of one study group. Data from figures will be extracted with the WebPlotDigitizer app (https://automeris.io/WebPlotDigitizer) if not reported in text.
Data synthesis
If possible, a meta-analysis will be conducted using Review Manager [31]. Extracted data are entered into Review Manager by the first author (NK) and checked by the second author (HvZ). A meta-analysis is possible if outcomes are reported in at least two studies with conceptually the same intervention (i.e. phase III outpatient exercise-based cardiac rehabilitation), outcome domain (e.g. maximal oxygen uptake), and follow-up (e.g. approximately 6 weeks). A random-effects meta-regression model will be used to calculate variance-weighed pooled mean differences and 95% confidence intervals between outcomes before cardiac rehabilitation versus after cardiac rehabilitation. Studies that do not report variance data will be included in the literature review but excluded from the meta-analysis. I2 statistics are used to assess the heterogeneity, with I2 statistics ≤ 25% representing low heterogeneity and ≥ 75% (p < 0.10) representing high heterogeneity [32]. A subgroup analysis might be performed based on the type of surgery (sternotomy versus other) or diagnosis (patients with connective tissue disease versus other) [17]. No sensitivity analysis will be performed.
Meta-bias
For the assessment of meta-bias, outcome reporting bias will be assessed by comparing outcomes listed in the study protocol or methods section with the actually reported outcomes [33]. Publication bias will be visually assessed using a funnel plot [34]. In the presence of publication bias, the funnel plot should resemble an asymmetrical funnel.
Confidence in evidence
The overall confidence in the body of evidence will be determined with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach [35]. Two reviewers (NK and HvZ) will independently score five categories of reasons for rating down the quality of evidence, and three categories for rating up, with a yes/no decision regarding rating up or down of each outcome. Observational studies will start at a low quality of evidence and can be upgraded accordingly [36]. Studies excluded from the meta-analysis will be excluded from the GRADE assessment. GRADE results will be used to inform conclusions on the overall strength of outcomes after cardiac rehabilitation in patients following repair of thoracic aortic aneurysm or dissection.
Discussion
A paradigm shift is perceptible in the recent scientific literature. Healthcare professionals are willing to provide cardiac rehabilitation in patients following thoracic aortic repair. However, they do not know what the benefits are, which safety recommendations apply, and whether the risk of adverse events outweighs the benefits [4]. To our knowledge, this will be the first systematic review and meta-analysis that analyses the health benefit of cardiac rehabilitation programmes in patients following thoracic aortic repair. A scoping review was recently published and concluded that the literature is gradually increasing and that the topic is worth studying [37].
There are limitations to this study protocol. First, we excluded studies using endovascular procedures. We acknowledge that thoracic endovascular aortic repair is a promising, safe, and effective procedure to treat descending thoracic aortic aneurysms showing similar perioperative and long-term results compared to open thoracic aortic repair [38]. However, endovascular procedures are not the first-choice solution for ascending aortic repair and aortic arch repair [14]. In addition, some patients are not suitable candidates for endovascular procedures due to an absence of proper ‘landing zones’, too large width of the aorta, lack of vascular access sites, comorbidities, or aetiology [14, 15]. It is important to realise that despite the lower impact of endovascular procedures, cardiac rehabilitation could still be an effective treatment, as has been shown in patients following transcatheter aortic valve implantation [39]. Second, pooled estimates that also include data from patients after isolated cardiac surgery will be excluded from our meta-analysis in order to avoid contamination of the effect-size for patients following thoracic aortic repair.
Availability of data and materials
All data generated or analysed during the systematic literature review and meta-analysis will be included in the published article (and its supplementary information files).
Abbreviations
- CINAHL:
-
Cumulative Index to Nursing and Allied Health Literature
- MeSH:
-
Medical Subject Headings
- PRISMA:
-
Preferred Items for Systematic Reviews and Meta-Analysis
- QUIPs:
-
Quality in Prognostic Studies
References
Goldfinger JZ, Halperin JL, Marin ML, Stewart AS, Eagle KA, Fuster V. Thoracic aortic aneurysm and dissection. J Am Coll Cardiol. 2014;64(16):1725–39.
Mokashi SA, Svensson LG. Guidelines for the management of thoracic aortic disease in 2017. Gen Thorac Cardiovasc Surg. 2019;67(1):59–65.
Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. 2018;137(17):1846–60.
Chaddha A, Eagle KA, Braverman AC, Kline-Rogers E, Hirsch AT, Brook R, et al. Exercise and physical activity for the post–aortic dissection patient: the clinician’s conundrum. Clin Cardiol. 2015;38(11):647–51.
Pasadyn SR, Roselli EE, Artis AS, Pasadyn CL, Phelan D, Blackstone EH. From court to couch: exercise and quality of life after acute type a aortic dissection. Aorta (Stamford). 2021;9(5):171–9.
Isselbacher EM, Bonaca MP, Di Eusanio M, Froehlich J, Bassone E, Sechtem U, et al. Recurrent aortic dissection: observations from the international registry of aortic dissection. Circulation. 2016;134(14):1013–24.
Buckingham S, Taylor R, Jolly K, Zawada A, Dean S, Cowie A, et al. Home-based versus centre-based cardiac rehabilitation: abridged Cochrane systematic review and meta-analysis. Open heart. 2016;3(2): e000463.
Long L, Mordi IR, Bridges C, Sagar VA, Davies EJ, Coats AJ, et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst Rev. 2019;1:CD003331.
Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;1:CD001800.
Powell R, McGregor G, Ennis S, Kimani PK, Underwood M. Is exercise-based cardiac rehabilitation effective? a systematic review and meta-analysis to re-examine the evidence. BMJ Open. 2018;8(3): e019656.
Lewinter C, Doherty P, Gale CP, Crouch S, Stirk L, Lewin RJ, et al. Exercise-based cardiac rehabilitation in patients with heart failure: a meta-analysis of randomised controlled trials between 1999 and 2013. Eur J Prev Cardiol. 2020;22(12):1504–12.
Taylor RS, Walker S, Smart NA, Piepoli MF, Warren FC, Ciani O, et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure. J Am Coll Cardiol. 2019;73(12):1430–43.
Francis T, Kabboul N, Rac V, Mitsakakis N, Pechlivanoglou P, Bielecki J, et al. The effect of cardiac rehabilitation on health-related quality of life in patients with coronary artery disease: a meta-analysis. Can J Cardiol. 2019;35(3):352–64.
Foundation ACoC, Guidelines AHATFoP, Surgery AAfT, Radiology ACo, Association AS, Anesthesiologists SoC, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. 2010;55(14):e27-e129.
members ATF, Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(41):2873–926.
Palatini P, Mos L, Munari L, Valle F, Del Torre M, Rossi A, et al. Blood pressure changes during heavy-resistance exercise. J Hypertens Suppl. 1989;7(6):S72–3.
Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease: The Task Force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J. 2020;42(1):17–96.
Boodhwani M, Andelfinger G, Leipsic J, Lindsay T, McMurtry MS, Therrien J, et al. Canadian cardiovascular society position statement on the management of thoracic aortic disease. Can J Cardiol. 2014;30(6):577–89.
Spanos K, Tsilimparis N, Kölbel T. Exercise after aortic dissection: to run or not to run. Eur J Vasc Endovasc Surg. 2018;55(6):755–6.
Schwaab B, Rauch B, Völler H, Benzer W, Schmid J-P. Beyond randomised studies: recommendations for cardiac rehabilitation following repair of thoracic aortic aneurysm or dissection. Eur J Prev Cardiol. 2021;28(17):e17–9.
Acosta S, Kumlien C, Forsberg A, Nilsson J, Ingemansson R, Gottsäter A. Engaging patients and caregivers in establishing research priorities for aortic dissection. SAGE Open Medicine. 2019;7:2050312118822632.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Johnson N, Phillips M. Rayyan for systematic reviews. J Electron Resour Librariansh. 2018;30(1):46–8.
Franklin B, Whaley M, Howley E, Medicine ACoS. Guidelines for exercise testing and prescription. ACSM’s guidelines for exercise testing Philadelphia: Lea & Febiger. 2000.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. bmj. 2016;355.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions: John Wiley & Sons; 2019.
Hoogeboom TJ, Kousemaker MC, van Meeteren NL, Howe T, Bo K, Tugwell P, et al. i-CONTENT tool for assessing therapeutic quality of exercise programs employed in randomised clinical trials. Br J Sports Med. 2021;55(20):1153–60.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):1–10.
Headrick TC. Statistical simulation: Power method polynomials and other transformations: CRC Press; 2009.
Henderson LK, Craig JC, Willis NS, Tovey D, Webster AC. How to write a Cochrane systematic review. Nephrology. 2010;15(6):617–24.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Page MJ, Higgins JP. Rethinking the assessment of risk of bias due to selective reporting: a cross-sectional study. Syst Rev. 2016;5(1):1–8.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004;4(1):1–7.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3 .rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Feng D, Ke J, Huang S, Lang X. A scoping review of exercise-based cardiac rehabilitation for patients with aortic dissection. Rev Cardiovasc Med. 2021;22(3):613–24.
Howard C, Sheridan J, Picca L, Reza S, Smith T, Ponnapalli A, et al. TEVAR for complicated and uncomplicated type B aortic dissection—systematic review and meta-analysis. J Card Surg. 2021;36(10):3820–30.
Ribeiro GS, Melo RD, Deresz LF, Dal Lago P, Pontes MR, Karsten M. Cardiac rehabilitation programme after transcatheter aortic valve implantation versus surgical aortic valve replacement: systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24(7):688–97.
Acknowledgements
We acknowledge On Ying Chan, information specialist at the Radboud University Medical Centre, for her contribution to the search strategies.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NK, HvZ, MS, and TS conceptualised the research question. NK and HvZ planned the data extraction methods. NK and TS designed the analysis plan. All authors contributed to protocol drafting and writing. All authors read and approved the final version. NK registered the study on PROSPERO.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Concept search strings.
Additional file 2.
i-CONTENT tool.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Koenders, N., van Zetten, H., Smulders, M. et al. Outcomes after cardiac rehabilitation in patients following repair of thoracic aortic aneurysm or dissection: a protocol for a systematic review and meta-analysis. Syst Rev 12, 16 (2023). https://doi.org/10.1186/s13643-023-02180-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02180-x