Abstract
Background
Patients with chronic kidney disease (CKD) require a personalised strategy for cardiovascular risk management (CVRM) to reduce their high risk of cardiovascular morbidity and mortality. Despite their high risk, patients with CKD appear to be underrepresented in randomised controlled trials (RCTs) for pharmacological CVRM interventions to reduce cardiovascular risk (pharmacological CVRM interventions). As a result, it remains unclear whether the efficacy of these interventions found in patients without CKD is similarly applicable to patients with CKD. This evidence map aims to provide an overview of the availability of the evidence from pharmacological CVRM trials for patients with CKD by assessing how often patients with reduced kidney function are specifically excluded or included from RCTs on pharmacological CVRM interventions and whether studies report efficacy estimates of interventions specifically for kidney patients.
Methods
We will perform a systematic literature search in ClinicalTrials.gov to identify relevant planned, ongoing, and completed RCTs on a broad range of CVRM medications after which we will retrieve the published protocols and papers via ClinicalTrials.gov itself, Embase, MEDLINE, or Google Scholar. We will include RCTs that investigate the efficacy of platelet inhibitors, anticoagulants, antihypertensives, glucose-lowering medication, and lipid-lowering medication on all-cause mortality, cardiovascular mortality, cardiovascular morbidity, and end-stage kidney disease in patients with a cardiovascular history or a major risk factor for cardiovascular disease. Two reviewers will independently screen trial records and their corresponding full-text publications to determine eligibility and extract data. Outcomes of interest are the exclusion of patients with reduced kidney function from RCTs and whether the study population was restricted to kidney patients or subgroup analyses were performed on kidney function. Results will be visualised in an evidence map.
Discussion
The availability of evidence on the efficacy and safety of pharmacological CVRM interventions in patients with CKD might be limited. Hence, we will identify knowledge gaps for future research. At the same time, the availability of evidence, or lack thereof, might warrant caution from healthcare decision-makers in making strong recommendations based on the extrapolation of results from studies to patients who were explicitly excluded from participation.
Systematic review registration
PROSPERO CRD42022296746.
Similar content being viewed by others
Background
Chronic kidney disease (CKD) is highly prevalent accounting for 1.2 million deaths globally every year [1]. Patients with CKD are at high risk for cardiovascular disease (CVD) independent of diabetes or hypertension [2, 3]. CVD is the main cause of death for patients with CKD stages 3 to 5 (estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73m2) [3]. CVD risk already increases in patients with an eGFR of 75 ml/min/1.73m2 or lower [4, 5]. In fact, the vast majority of patients with CKD are at greater risk for CVD and cardiovascular mortality than for progressing to end-stage kidney disease (ESKD) [6, 7].
The high risk of CVD in patients with CKD makes cardiovascular risk management (CVRM) indispensable for them. In order to provide personalised CVRM treatment for patients with CKD, the efficacy of pharmacological CVRM interventions should be determined specifically for this patient population. Patients with CKD are a very heterogeneous patient population in terms of age, comorbidities, CKD stage, and cause of kidney failure and have competing risks for mortality and ESKD [8,9,10]. Consequently, the effects of interventions may differ for patients with and without CKD or for patients with different stages of CKD.
Evidence for the efficacy of pharmacological CVRM interventions in patients with CKD is likely to be scant. Even if patients with CKD are included in randomised controlled trials (RCTs), authors do not necessarily investigate whether the treatment effects differ between patients with normal and reduced kidney function. Results from four reviews including RCTs published between 1985 and 2014 suggest that patients with CKD are systematically underrepresented in clinical trials on pharmacological CVRM interventions [11,12,13,14]. Since then, the CVRM landscape has vastly changed with the introduction of, for example, direct oral anticoagulants (DOACs), proprotein convertase subtilisin/kexin type 9 (PCSK-9) inhibitors, and sodium-glucose co-transporter-2 (SGLT-2) inhibitors. The previous reviews are also likely to have missed studies published in smaller journals, since their search was predominantly limited to the major general medicine, cardiology, and nephrology journals. In addition, they restricted themselves to RCTs investigating the efficacy of a selection of antihypertensives, antiplatelets, anticoagulants, and statins on all-cause mortality and coronary artery disease in patients with pre-established CVD.
Despite the urgency for personalised CVRM for patients with CKD, no review has investigated for which pharmacological CVRM interventions the efficacy for patients with reduced kidney function has been determined in RCTs. Therefore, we will create an evidence map to provide an overview of the available evidence for pharmacological CVRM interventions on cardiovascular and kidney endpoints for patients with CKD. We will explore how often patients with reduced kidney function are excluded from RCTs on pharmacological CVRM interventions and whether the authors restricted the study population to patients with reduced kidney function or performed subgroup analysis to determine the effect in patients with reduced kidney function.
Methods/design
The protocol is registered in the International Prospective Register for Systematic Reviews (PROSPERO CRD42022296746) and was written based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) [15].
Eligibility criteria
Study design
We will include only RCTs. Reviews, meta-analyses, observational studies, case reports, animal studies, and cross-over trials will be excluded. No restrictions will be applied on language and publication status.
Population
We will include RCTs whose study population consists of adults with a history of CVD or adults without a history of CVD with at least one cardiovascular risk factor. History of CVD will be defined as the presence of coronary artery disease, atrial fibrillation, congestive heart failure, peripheral arterial disease, stroke, or aortic aneurysm. Patients with one or more of the following cardiovascular risk factors will also be included: overweight or obesity, hypertension, hyperglycaemia or diabetes mellitus, or chronic- or end-stage kidney disease (Table 1) [3, 16, 17]. Studies with a sample size < 100 and studies in paediatric patients will be excluded. Studies in both paediatric and non-paediatric patients will be included if stratified analyses were performed for non-paediatric patients.
Interventions and comparators
We will include studies that examine pharmacological interventions recommended by the European Society of Cardiology (ESC), the American Heart Association (AHA), the American Stroke Association (ASA), the American College of Cardiology (ACC), or the American Diabetes Association (ADA) for the prevention of cardiovascular disease in general and treatment of cardiovascular risk factors [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. Broadly speaking, these concern antihypertensives, cholesterol-lowering medication, glucose-lowering medication, anticoagulants, or anti-platelets (for a full list, see Table 2). Interventions must be compared against placebo, no treatment, usual care, another therapy, or a different dosage or duration of treatment. Studies that investigated a combination of pharmacological and non-pharmacological interventions (e.g., coronary artery bypass graft (CABG) + antiplatelet therapy vs CABG only) will be included. Studies in which the intervention is first administered in an acute setting or during a cardiac or vascular procedure will be included if the intervention is continued during the follow-up. Studies that compare different treatment targets (e.g. systolic blood pressure < 140 mmHg vs < 130 mmHg) will be excluded.
Outcomes
We will restrict ourselves to studies which report patient-important outcomes since these are most likely to drive clinical decision-making [40,41,42]. Included studies must report at least one of the following endpoints: all-cause mortality, cardiovascular mortality, major cardiovascular event (MACE) or another composite cardiovascular endpoint, coronary artery disease (myocardial infarction, angina, coronary artery bypass grafting, percutaneous coronary intervention, or as defined by authors), cerebrovascular disease (stroke, transient ischaemic attack, or as defined by authors), peripheral arterial disease (bypass, amputation, aortic aneurysm, or as defined by authors), hospitalisation for heart failure or development of heart failure stage III or IV (New York Heart Association classification), or ESKD (initiation of dialysis, kidney transplant, or as defined by authors). Studies reporting only surrogate endpoints will be excluded.
Search and study selection
Our search strategy will consist of a two-step approach. First, we will perform a search in Cochrane Central to identify relevant planned, ongoing, and completed RCTs in the ClincialTrials.gov trial registry using a combination of keywords for cardiovascular disease and the interventions of interest (Appendix 1). After identifying relevant RCTs in ClinicalTrials.gov, we will retrieve the publications related to the trial record in ClinicalTrials.gov. If no publications are listed in ClinicalTrials.gov, we will perform an additional search on clinical trial record number (NCT number) and study acronym in Embase, MEDLINE, and Google Scholar. If no publications can be retrieved, the record will be excluded.
Conducting a literature search through a trial registry is a relatively new approach. Since 2005, it is mandatory to register new RCTs in a trial registry [43]. Consequently, it should be possible to identify relevant RCTs through such a trial registry. As a substudy, we will validate our search strategy to identify relevant RCTs from a trial registry by comparing the Clinicaltrials.gov search results with the search results from a search in MEDLINE, Embase, and Google Scholar (Appendix 2). Additionally, we will evaluate selective outcome reporting by comparing the outcomes reported in the trial records and those reported in the study publications and publication bias from the number of studies that have published a protocol (in ClinicalTrials.gov or as separate publication) but have never published results or vice versa. For this validation study, we will limit ourselves to RCT anticoagulants conducted in the past 10 years (2012 to 2022). For the validation search, we will use a comparable set of keywords and MeSH terms as for the search in ClinicalTrials.gov and apply a RCT filter and publication date filter (between 2011 and 2021) [44].
Screening and data collection
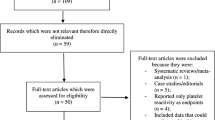
First, we will screen trial records on title and trial description to select RCTs for full-text screening. Next, we will screen the retrieved full-text articles linked to the trial record to determine if RCTs meet the inclusion criteria. Pairs of reviewers will work independently for both the screening of the trial records and the full-text papers. Disagreements between reviewers on eligibility will be resolved by consensus or by means of an adjudicator. The whole screening process is visualised in Fig. 1.
Pairs of reviewers will independently extract data on patient characteristics such as age, sex, and kidney function with standardised data extraction forms and study characteristics such as study design, reported endpoints, and exclusion of patients on hypertension, pre-diabetes, or smoking (for a full list, see Table 3). For the methodological substudy, we will extract whether results have been published and compare reported outcomes from ClinicalTrials.gov and the published articles.
The two outcomes of interest are (1) the exclusion of patients with reduced kidney function from RCTs and (2) subgroup analyses on kidney function or restriction of the study population to patients with reduced kidney function. Exclusion of patients with CKD will be extracted according to the definition of the authors of the included studies and categorised into one of the following categories: (e)GFR or creatinine clearance, serum creatinine, kidney insufficiency, pre-established kidney disease, end-stage kidney disease or maintenance dialysis, or an ambiguous kidney-related exclusion criterion. If authors do not explicitly state kidney function or kidney disease as exclusion criterion, we will presume that these patients were not excluded. We will compare the rate of exclusion from RCTs on pharmacological CVRM interventions on CKD with the exclusion on smoking, diabetes, and hypertension, which are other major risk factors for CVD. Subgroup analysis based on kidney function will be defined as performing an analysis based on one exclusion criteria for kidney disease described above.
Risk of bias assessment
We will not perform a risk of bias assessment because bias in study design will not compromise the data synthesis and conclusions of our study.
Data synthesis
The data will be summarised descriptively, based on the mean ± standard deviation (SD) and median [interquartile range, IQR] for continuous variables and frequency (percentage) for categorical variables. Results will be presented narratively and in tables and figures. We will report the proportion of studies that exclude patients with reduced kidney function, smoking, diabetes, and hypertension, and the proportion of studies that perform subgroup analyses on kidney function. We will provide an overview of kidney-related exclusion criteria of studies that exclude patients with CKD. Characteristics of studies that include or exclude patients with reduced kidney function, perform subgroup analyses, and report kidney function at baseline will be compared using chi-square tests, independent t-tests or non-parametric tests. For the assessment of subgroup analyses and restriction of the study population to patients with reduced kidney function, we will create a visual overview of the available studies with an evidence map in which studies will be clustered on CKD stage, serum creatinine levels, dialysis, or kidney transplant, intervention, and reported outcomes. No meta-analyses of clinical outcomes (e.g. morbidity and mortality) will be performed.
For our methodological substudy, we will match the search results from ClinicalTrials.gov with the search results from a bibliographic database search and report the proportion of matches identified. We will estimate publication bias by the number of studies that have a published protocol (in ClinicalTrials.gov) but which have never published results. Studies that were expected to be finished after 1 January 2019 will not be classified under reporting bias because they might still publish results. Vice versa, as an indication of good research practice, we will look at the proportion of publications of RCTs that do not have a registration in ClinicalTrials.gov. Additionally, for studies that have both a ClinicalTrials.gov registration and a publication of the trial results, we will compare the outcomes that were stated in the registration to the outcomes that were reported in the publication.
Ethical considerations and dissemination of results
This study does not fall under the Dutch Medical Research Involving Human Subjects Act as it does not involve patients or individual patient data. Therefore, no ethical approval was sought from a medical ethics committee. We intend to disseminate the results of our study through peer-reviewed scientific journals, conferences, and meetings with patient organisations. Since CVRM for CKD patients does not only concern nephrologists but also other medical disciplines like general practitioners, cardiologists, endocrinologists, and vascular medicine specialists, we will target journals that have a broader audience.
Discussion
Although CVRM is of paramount importance for CKD patients, uncertainty remains about the availability of evidence on pharmacological CVRM interventions specifically for this patient population. This study will provide an overview of how often patients with CKD are excluded from cardiovascular RCTs. Looking at subgroup analyses on kidney function and studies restricted to patients with CKD will allow us to create an overview of what evidence exists for different interventions for specific groups of CKD patients. Hence, we will identify whether an evidence gap exists for certain interventions for this patient population. We will not determine the efficacy of specific interventions due to the large number of expected RCTs, the expected heterogeneity in study designs, and the fact that the efficacy of interventions lies outside the scope of our research objective.
We have taken several steps to increase the relevance of our results for clinical practice. We have limited ourselves to RCTs as these are generally considered to provide the highest level of evidence to determine the effectiveness of such interventions [45, 46] Contrary to previous reviews, we have opted to include both patients with and without pre-established CVD which ensures that we cover the whole spectrum of patients with CKD. We will include the interventions currently recommended in international guidelines as these are most likely prescribed in today’s clinical practice and include a broad set of patient-important outcomes to cover the whole spectrum of preventive indications. We deliberately will not include studies that only report surrogate endpoints such as change in blood pressure, HbA1c, or cholesterol since these outcomes are less relevant to patients and less likely to guide clinical decision-making [40, 41].
Our substudy will have both methodological and clinical implications. A trial registry search may be more efficient means to identify relevant RCTs for a literature search than a search in traditional bibliographic databases. RCTs frequently publish more than one article. Instead of having to screen all the individual articles, one might be able to limit the screening process to the information provided in the trial registry. Validating our search in ClinicalTrials.gov with a bibliographic database search will provide insight into the comprehensiveness of our search results and the viability of performing a literature search in a trial registry. Our substudy will also give an indication of the extensiveness of publication bias in RCTs on CVRM interventions and accuracy of reporting of study protocols in trial registries.
This study will likely have some limitations. We might miss some RCTs when the publications are not linked to the trial record or not registered in the trial registry that we searched. We expect this will include most RCTs conducted before February 2000, when ClinicalTrials.gov became available [47]. We also expect to miss some of the RCTs between February 2000 and September 2007 because in that period registration of a clinical trial in ClinicalTrials.gov was optional [47]. Especially in a fast-pacing field like CVRM, clinical decision-making is largely based on recent trials. Therefore, we will be able to give insight into the current evidence for pharmacological interventions for patients with reduced kidney function. Finally, we will not perform a formal risk of bias assessment since none of our outcomes of interest is related to the methodological aspects usually assessed in a risk of bias assessment.
Availability of data and materials
Not applicable.
Abbreviations
- ACC:
-
American College of Cardiology
- ADA:
-
American Diabetes Association
- AHA:
-
American Heart Association
- ASA:
-
American Stroke Association
- CABG:
-
Coronary artery bypass graft
- CKD:
-
Chronic kidney disease
- CVD:
-
Cardiovascular disease
- CVRM:
-
Cardiovascular risk management
- DOAC:
-
Direct oral anticoagulant
- eGFR:
-
Estimated glomerular filtration rate
- ESC:
-
European Society of Cardiology
- ESKD:
-
End-stage kidney disease
- IQR:
-
Interquartile range
- MACE:
-
Major cardiovascular event
- MeSH:
-
Medical Subject Headings
- PCSK-9:
-
Proprotein convertase subtilisin–kexin type 9
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols
- PROSPERO:
-
Prospective Register for Systematic Reviews
- RCT:
-
Randomised controlled trial
- SD:
-
Standard deviation
- SGLT-2:
-
Sodium-glucose cotransporter-2
References
Bikbov B, Purcell CA, Levey AS, Smith M, Abdoli A, Abebe M, et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2020;395(10225):709–33.
System USRD. 2020 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2020.
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–52.
Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073–81.
van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey A, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011;79(12):1341–52.
de Jong PE, van der Velde M, Gansevoort RT, Zoccali C. Screening for chronic kidney disease: where does Europe go? Clin J Am Soc Nephrol. 2008;3(2):616–23.
Packham DK, Alves TP, Dwyer JP, Atkins R, de Zeeuw D, Cooper M, et al. Relative incidence of ESRD versus cardiovascular mortality in proteinuric type 2 diabetes and nephropathy: results from the DIAMETRIC (Diabetes Mellitus Treatment for Renal Insufficiency Consortium) database. Am J Kidney Dis. 2012;59(1):75–83.
Jiang Y, Fine JP, Mottl AK. Competing risk of death with end-stage renal disease in diabetic kidney disease. Adv Chronic Kidney Dis. 2018;25(2):133–40.
NEFROVISIE. RENINE annual report 2019. 2019.
Liu P, Quinn RR, Lam NN, Al-Wahsh H, Sood MM, Tangri N, et al. Progression and regression of chronic kidney disease by age among adults in a population-based cohort in Alberta, Canada. JAMA Netw Open. 2021;4(6):e2112828.
Charytan D, Kuntz RE. The exclusion of patients with chronic kidney disease from clinical trials in coronary artery disease. Kidney Int. 2006;70(11):2021–30.
Coca SG, Krumholz HM, Garg AX, Parikh CR. Underrepresentation of renal disease in randomized controlled trials of cardiovascular disease. JAMA. 2006;296(11):1377–84.
Konstantinidis I, Nadkarni GN, Yacoub R, Saha A, Simoes P, Parikh CR, et al. Representation of patients with kidney disease in trials of cardiovascular interventions: an updated systematic review. JAMA Intern Med. 2016;176(1):121–4.
Maini R, Wong DB, Addison D, Chiang E, Weisbord SD, Jneid H. Persistent underrepresentation of kidney disease in randomized, controlled trials of cardiovascular disease in the contemporary era. J Am Soc Nephrol. 2018;29(12):2782–6.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Levey AS, Eckardt K-U, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005;67(6):2089–100.
Federation ID. The IDF consensus worldwide definition of the metabolic syndrome. 2006.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498.
Collet J-P, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2021;42(14):1289–367.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. 2020;41(3):407–77.
Aboyans V, Ricco J-B, Bartelink M-LEL, Björck M, Brodmann M, Cohnert T, et al. ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763–816.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334–57.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39(33):3021–104.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2020;41(1):111–88.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease. J Am Coll Cardiol. 2021;77(4):e25–197.
American Diabetes A. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S111.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol. 2019;74(10):e177–232.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation. J Am Coll Cardiol. 2014;64(21):e1–76.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. J Am Coll Cardiol. 2019;73(24):e285–350.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2018;71(19):e127–248.
Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: Executive Summary. J Am Coll Cardiol. 2017;69(11):1465–508.
Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021;52(7):e364–467.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2021;42(34):3227–337.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;60(4):ehab395.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–726.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur Heart J. 2020;41(2):255–323.
Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Wittes J, Lakatos E, Probstfield J. Surrogate endpoints in clinical trials: cardiovascular diseases. Stat Med. 1989;8(4):415–25.
Pino C, Boutron I, Ravaud P. Outcomes in registered, ongoing randomized controlled trials of patient education. PLoS ONE. 2012;7(8):e42934.
Gandhi GY, Murad MH, Fujiyoshi A, Mullan RJ, Flynn DN, Elamin MB, et al. Patient-important outcomes in registered diabetes trials. JAMA. 2008;299(21):2543–9.
ClinicalTrials.gov. History, policies, and law 2021 [Available from: https://clinicaltrials.gov/ct2/about-site/history.
Kaul T, Colombijn JMT, Vernooij RWM, Spijker R, Damen JAAG, Hooft L. Clinical Trial Registers as Primary Search Databases for Systematic Reviews of Randomized Controlled Trials Involving Interventions. 2022. https://doi.org/10.17605/OSF.IO/WJ9BA.
Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128(1):305–10.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
ClinicalTrials.gov. 2021 [Available from: https://clinicaltrials.gov/ct2/manage-recs/fdaaa.
Acknowledgements
We acknowledge the support from the Dutch CardioVascular Alliance, an initiative with support of the Dutch Heart Foundation, 2020B008 RECONNEXT.
Funding
No sponsors are involved in this study.
Author information
Authors and Affiliations
Contributions
JC and RV designed the study. JC, RV, DI, and KvdB designed the methodological substudy. JC, RV, RS, DI, and KvdB devised the search strategy. JC drafted the manuscript, tables, and figures. All authors provided intellectual input of critical importance, critically revised the manuscript, and approved the final version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agreed to the submission of the final manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
search strategy in ClinicalTrials.gov. Appendix 2. search strategy for validation study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Colombijn, J.M.T., Idema, D.L., van der Braak, K. et al. Evidence for pharmacological interventions to reduce cardiovascular risk for patients with chronic kidney disease: a study protocol of an evidence map. Syst Rev 11, 238 (2022). https://doi.org/10.1186/s13643-022-02108-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-022-02108-x