Abstract
Background
Indigenous young people worldwide are at greater risk of developing mental health concerns due to ongoing inequity and disadvantage. Digital mental health (dMH) interventions are identified as a potential approach to improving access to mental health treatment for Indigenous youth. Although involvement in the development and evaluation of dMH resources is widely recommended, there is limited evidence to guide engagement of Indigenous young people in these processes. This scoping review aims to examine the methods used to involve Indigenous young people in the development or evaluation of dMH interventions.
Methods
Articles published in English, involving Indigenous young people (aged 10–24 years) in the development or evaluation of dMH interventions, originating from Australia, New Zealand, Canada and the USA will be eligible for inclusion. PubMed, Scopus and EBSCOhost databases (Academic Search Premiere, Computer and Applied Science complete, CINAHL, MEDLINE, APA PsychArticles, Psychology and Behavioural Sciences collection, APA PsychInfo) will be searched to identify eligible articles (from January 1990 onwards). Infomit and Google Scholar (limited to 200 results) will be searched for grey literature. Two reviewers will independently screen citations, abstracts and full-text articles. Study methods, methodologies, dMH intervention details, participant information and engagement, and dissemination methods will be extracted, analysed (utilising content analysis), and qualitatively assessed for alignment with best practice ethical guidelines for undertaking Indigenous health research. A narrative summary of findings will be presented. Reporting will follow the Consolidated Criteria for Strengthening Reporting of Health Research involving Indigenous peoples (CONSIDER) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guidelines.
Discussion
To date, there are no reviews which analyse engagement of Indigenous young people in the development and evaluation of dMH interventions. This review will appraise alignment of current practice with best practice guidelines to inform future research. It will highlight appropriate methods for the engagement of young people in study processes, providing guidance for health practitioners, policy makers, and researchers working in the field of Indigenous youth and dMH.
Systematic review registration
Open Science Framework (osf.io/2nkc6).
Similar content being viewed by others
Background
The majority of Indigenous young people worldwide are resilient, proud of their culture, and possess social capital beyond any other recent generation [1,2,3]. Despite this, they remain at heightened risk of developing mental illness in adolescence compared with their non-Indigenous counterparts [4]. We use the collective term ‘Indigenous’ to describe people who originate from a particular region but acknowledge the rich diversity of cultures and knowledge represented by this term. Despite the need, Indigenous young people worldwide are less likely to access mental health treatment than non-marginalised young people [5, 6]. Barriers to accessing mental health treatment include stigma, fear, shame, intergenerational trauma, distrust of services and being unable to identify signs and symptoms of illness [5, 6]. Furthermore, the location of populations in need are often decentralised, meaning long distances and increased costs and challenges in the delivery of services [5, 7]. Treatment services are often non-existent, underfunded or occur in a localised or prescribed manner within Indigenous communities, limiting their ability to affect meaningful sustained change. Considerations of language, diversity and worldview differences are sometimes overlooked, resulting in programs that are less meaningful or acceptable to the young people they are intended to serve [8, 9]. Despite the need for culturally safe, effective and early intervention treatments, there remain relatively few approaches which are evidence-based. Recent increased availability of technology and connectivity has been identified as an opportunity to increase access to health services within underserved communities and marginalised youth populations [6].
dMH is identified as “mental health, suicide prevention and alcohol and other drugs services delivered via a digital platform” [10]. There remains limited adaptation to cultural diversity in the dMH field, despite the potential of dMH to increase access to treatment for Indigenous populations [11,12,13]. To date, five systematic or scoping reviews have been conducted in the area of health technologies for Indigenous populations [14,15,16,17,18] but only one has focused on young people and mental health interventions [18]. One other related article contains a literature review and a case study [19]. There is consensus among the authors of these reviews that meaningful engagement of end users in design, development or evaluation is a necessary component of digital health solutions [14, 16,17,18]. However, none comprehensively examine the strategies undertaken to engage Indigenous young people in the development or evaluation process.
Despite widespread recognition of the importance of end-user involvement in the development and evaluation of dMH interventions [10, 20, 21], there remains a lack of clear reporting on the methods and processes undertaken [22, 23]. A popular methodology outlined in the literature is Participatory Design (PD), which involves end users in the co-creation and evaluation of digital health resources as partners [24]. This process allows an iterative approach whereby digital resource design is continually reviewed and updated throughout all design, development and evaluation phases [21], as recommended in the National Safety and Quality Digital Mental Health Standards [10].
Furthermore, ethical guidelines on the conduct of research with Indigenous communities emphasise the importance of cultural considerations when engaging Indigenous people in research practices [25,26,27,28,29]. Most of these guidelines highlight the importance of (1) accessible, clear and co-constructed benefits to the community or individual, (2) meaningful relationships, consultation and participation of Indigenous people within all stages of research processes, (3) respecting and upholding Indigenous knowledge and practices and (4) Indigenous self-determination and governance [25, 27,28,29,30]. Meaningful engagement of Indigenous youth potentially protects young people and communities from being detrimentally affected and disempowered and allows better opportunity for self-determination [25, 31, 32]. Critically reviewing research practices ensures ethical guidelines are upheld and safeguards and informs the best practice into the future [31]. Such reviews have resulted in specific guidelines, such as the Consolidated Criteria for Strengthening Reporting of Health Research involving Indigenous peoples (CONSIDER statement), which aims to improve the quality of reporting of research practices involving Indigenous peoples [33]. Guidelines or recommendations for the involvement of Indigenous young people in dMH development or evaluations do not currently exist.
International research has identified strengths unique to Indigenous young people which help build and maintain resilience [34, 35]. Strong connections with land, culture, lore, family and community assist Indigenous young people to develop strong identities, physical health, mental health and well-being. These connections provide the foundation for healthy development into adulthood [34, 36,37,38]. Their unique strengths, coupled with an affinity for creative technological innovation and design [14, 39, 40], and willingness to embrace empowerment and self-determination [1] provide a strong foundation for the involvement of Indigenous young people in the development and design of dMH interventions [41]. To ensure an ethical and culturally responsive process, it is essential to understand best practice methods for the engagement of Indigenous young people in the development and evaluation of dMH solutions. Therefore, the objectives of this review are to comprehensively synthesise research reporting on the methods used to involve Indigenous young people (aged 10 to 24) in the development or evaluation of dMH interventions and to examine the degree to which those methods align with the best practice ethical guidelines for undertaking Indigenous health research [26,27,28, 30].
Methods
Study design
Scoping reviews are particularly useful in providing an overview of research on a given topic where evidence is emerging [42] and to review research processes on a given topic [43]. For these reasons, a scoping review was considered the most appropriate methodology. This scoping review will be conducted according to guidelines proposed by Arksey and O’Malley [44] and the subsequent modifications proposed by Levac et al. [42] and Peters et al. [45]. It involves a six-stage process which includes (1) identifying the research question; (2) identifying relevant studies; (3) developing a study selection and data extraction method, which is refined using an iterative process [42]; (4) charting the data; and (5) collating, summarising and reporting results. Additionally, Step 6, consultation, engages two senior Indigenous researchers (PPRJM) throughout scoping review processes, a minimum of three times, ensuring analysis and findings are informed by Indigenous worldviews. Given the iterative nature of a scoping review, changes to the protocol can be expected [45], and any changes are detailed and justified in the final reporting.
Protocol registration and reporting information
This scoping review protocol is being reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement (see Additional file 1) and has been registered with Open Science Framework (registration identifier: osf.io/2nkc6). The proposed scoping review will be reported in accordance with the reporting guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) extension for Scoping Reviews (PRISMA-ScR) [46].
Eligibility criteria
Type of studies
All primary research study designs will be eligible for inclusion, such as experimental studies (e.g. randomised controlled trials, non-randomised controlled trials), observational studies (e.g. cross-sectional studies, cohort studies), quasi-experimental studies and qualitative studies. Systematic reviews, meta-analyses, opinion pieces and narrative reviews will be excluded.
Participants
Studies involving Indigenous young people, originating from Australia (Aboriginal and Torres Strait Islander), New Zealand (Maori), Canada (Inuit, First Nations people) and the USA (First Nations people) are eligible for inclusion. Indigenous people in these developed first world countries have experiences of colonisation, persistent health inequities and notable rural and remote residence. In addition, Indigenous people’s health worldviews, language and cultural needs differ from mainstream populations. Young people, for the purposes of this review, refer to those who are aged 10−24 years, representative of a broader definition of adolescence, as described by Sawyer et al. [47].
Intervention
dMH services are identified as “mental health, suicide prevention and alcohol and other drugs services delivered via a digital platform”, which include the “provision of information, digital counselling services, treatment services (including assessment, triage and referral services) and peer-to-peer support services” [10]. Some examples of dMH services for Indigenous people include interventions delivered via smartphone applications [48], therapist-supported digital interventions on tablet devices [49], online CBT programs [50] and gamified CBT interventions [51]. For the purposes of this review, we will include studies reporting on the design, development or evaluation of mental health interventions, which use a digital platform (e.g. smartphone, tablet device, website, computer, wearable devices) to deliver mental health services (e.g. health promotion/psycho-education, prevention/early intervention, crisis intervention/suicide prevention, treatment, recovery and mutual/peer support). Studies describing interventions such as telepsychiatry and videopsychiatry without the significant use of other computerised methods (e.g. websites, online game or SMS support) will not be eligible, as these services are more closely aligned with face-to-face services than dMH services which rely on computerised systems and are designed to be less resource dependent and easily replicated to the wider population [52, 53]. The primary treatment focus of the dMH intervention must be improvement of mental health or well-being outcomes, which include psychological distress, anxiety/stress management, suicidality, substance use and smoking, to be eligible for inclusion. Studies with a primarily physical health focus (e.g. diabetes, HIV management) will be excluded. Electronic health or medical records, decision support tools for clinicians, analytic services, services that primarily provide support and education to health professionals, clinical practice management software, and clinical workflow and communication software are excluded [10]. A full list of inclusion and exclusion criteria is included in Table 1.
Outcomes
There are two broad categories of outcomes that are of interest: (1) study methodology and methods and (2) alignment of methods with relevant ethical guidelines. Specifically, methods will be assessed in terms of accessible, clear and co-constructed benefits to the community or individual; meaningful relationships, consultation and participation of Indigenous people within all stages of research processes; respect and recognition of Indigenous knowledge and practices and Indigenous self-determination and governance [27,28,29,30].
Information sources and search strategy
Following recommendations by Joanna Briggs Institute, a three-step search process will be used. First, two independent reviewers (JP, BR) will undertake a limited search of the databases (EBSCOhost and PubMed). Search terms for EBSCOhost database are included in supplementary file 2. Titles, abstracts and keywords of retrieved articles will be reviewed to find additional search terms, before three reviewers (JP, BR, MT) meet to finalise keywords. Search terms will then be updated. The primary source of literature will be a structured search of multiple electronic databases from January 1990 onwards—considering the emergence of the internet in the mid 1990’s provided opportunities for health professionals to explore alternatives to face-to-face care [54]. Databases will include EBSCOhost databases (Academic Search Premiere, Computer and Applied Science complete, CINAHL Plus with Full text, MEDLINE with full text, APA PsychArticles, Psychology and Behavioural sciences collection, APA PsychInfo); PubMed; Scopus. The secondary source of potentially relevant material will be a search of the grey or difficult-to-locate literature, including Informit and Google Scholar (limited to the first 200 results). We will perform hand-searching of the reference lists of included studies, relevant reviews, or other relevant documents. Content experts and authors who are prolific in the field will be contacted. If full text is not available, corresponding authors will be contacted.
Screening and selection procedure
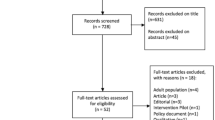
First, the titles and abstracts of articles returned from initial searches will be screened based on the eligibility criteria outlined above. Two reviewers (JP, BP) will independently review a 10−15% subset of the complete set of search results to establish a good inter-rating agreement (defined as kappa of 0.81 or above). Once good inter-rater reliability is established, one reviewer (JP) will then continue to screen the rest of the articles before proceeding to full-text review. The same procedure will be carried out for the second screening stage using full texts. In the third stage, references of all considered articles will be hand-searched to identify any relevant studies missed in the search strategy. Any disagreements will be resolved by discussion to meet a consensus, if necessary. If consensus is not reached throughout each stage of study selection, a third reviewer (MT) will review the articles in question. A flow chart showing details of studies included and excluded at each stage of the study selection process will be provided [46].
Data extraction
Data extraction variables, outlined in Table 2, are converted into simple tables prior to data extraction. Data extraction forms will be independently tested by two reviewers (JP, BR) on a random sample of five studies to ensure accuracy, consistency and validity of captured information [42, 55]. One reviewer (JP) will then extract relevant data. If data are missing upon review of full text, corresponding authors will be contacted.
Collating, summarising and reporting results
Relevant references will be exported into Endnote X9, including full text. Endnote X9 allows reviewers to collaboratively manage duplicates, group and code references and add annotations and notes. Data will be grouped by dMH intervention attributes, study design and alignment with research best practice and synthesised in table format. Qualitative content analysis will be undertaken [56]. Revision and refinement of themes will occur within the research team through a series of meetings. Results will be reported in narrative format, using tables to summarise important findings (e.g. dMH intervention attributes, study design and detail, alignment with best practice).
Consultation
Emerging themes will be documented and used to facilitate discussion with two Senior Indigenous Research Officers (PPJRM) on at least three occasions, and written notes will be taken during consultation meetings [42]. Discussion between consultants and the research team will review and refine preliminary findings, aiming to reach consensus. This consultation phase, originally outlined by Arksey and O’Malley [44] and later refined and defined as necessary, by Levac et al. [42] enhances rigour, provides additional sources of information, perspectives, and meaning, and increases the applicability of research findings.
Discussion
This scoping review aims to provide a comprehensive overview of current methods described in the literature regarding the involvement of Indigenous young people in development or evaluation of dMH interventions. The systematic nature of this review will ensure all relevant information on study methods is captured. Findings will provide insight into how methods align with best practice guidelines for the involvement of Indigenous people in ethical research and will inform recommendations for future projects aiming to develop or evaluate dMH interventions with Indigenous young people. As the design and use of dMH with Indigenous populations is an emerging field, potential limitations may be the small number of studies reported in the peer-reviewed literature as well as variations in study design and rigour. Therefore, broad definitions of inclusion terms will be used and the identification of relevant grey literature will expand data sources, allowing the identification of evidence gaps.
The findings from this review will assist researchers, clinicians and technology developers through establishing best practice processes for engagement of Indigenous young people in dMH approaches as well as for health research more broadly. As no other review has previously examined processes of development or evaluation in depth, this review aims to assist researchers to determine the ‘how’ of research design and develop clear methodology for respectful and culturally safe engagement with Indigenous young people.
Abbreviations
- CONSIDER:
-
Consolidated criteria for strengthening reporting of health research involving Indigenous peoples
- dMH:
-
Digital Mental Health
- PD:
-
Participatory design
- PRISMA-P :
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols
- PRISMA-Scr:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews
References
Azzopardi P, Blow N, Purcell T, Brown N, Ritchie T, Brown A. Investing in the health of Aboriginal and Torres Strait Islander adolescents: a foundation for achieving health equity. Med J Aust. 2020;212(5):202–4 e1.
Priest N, Thompson L, Mackean T, Baker A, Waters E. 'Yarning up with Koori kids' - hearing the voices of Australian urban Indigenous children about their health and well-being. Ethn Health. 2017;22(6):631–47. https://doi.org/10.1080/13557858.2016.1246418.
MacDonald JP, Ford JD, Willox AC, Ross NA. A review of protective factors and causal mechanisms that enhance the mental health of Indigenous Circumpolar youth. Int J Circumpolar Health. 2013;72(1):21775. https://doi.org/10.3402/ijch.v72i0.21775.
Azzopardi PS, Sawyer SM, Carlin JB, Degenhardt L, Brown N, Brown AD, et al. Health and wellbeing of Indigenous adolescents in Australia: a systematic synthesis of population data. Lancet. 2018;391(10122):766–82. https://doi.org/10.1016/S0140-6736(17)32141-4.
Price M, Dalgleish J. Help-seeking among indigenous Australian adolescents: Exploring attitudes, behaviours and barriers. Youth Stud Aust. 2013;32(1):10–8.
Robards F, Kang M, Usherwood T, Sanci L. How marginalized young people access, engage with, and navigate health-care systems in the digital age: systematic review. J Adolesc Health. 2018;62(4):365–81. https://doi.org/10.1016/j.jadohealth.2017.10.018.
Walker B, Stomski N, Price A, Jackson-Barrett E. Perspectives of Indigenous people in the Pilbara about the delivery of healthcare services. Aust Health Rev. 2014;38(1):1.
Cass A, Lowell A, Christie M, Snelling P, Flack M, Marrnganyin B, et al. Sharing the true stories: improving communication between Aboriginal patients and healthcare workers. Med J Aust. 2002;176(10):466–70. https://doi.org/10.5694/j.1326-5377.2002.tb04517.x.
Lowell A, Maypilama E, Yikaniwuy S, Rrapa E, Williams R, Dunn S. "Hiding the story": indigenous consumer concerns about communication related to chronic disease in one remote region of Australia. Int J Speech Lang Pathol. 2012;14(3):200–8. https://doi.org/10.3109/17549507.2012.663791.
Australian Commission on Safety and Quality in Health Care. National safety and quality digital mental health standards. Canberra: Australian Commission on Safety and Quality in Health Care; 2020.
Merry S. You can take a horse to water… lessons learned and next steps in realizing the promise and addressing the challenges of digital mental health. Keynote presentation presented at International Society for Research on Internet Interventions (ISRII): The next generation; 2019; Auckland, New Zealand.
Orji R, Mandryk RL. Developing culturally relevant design guidelines for encouraging healthy eating behavior. Int J Human - Comput Stud. 2014;72(2):207–23. https://doi.org/10.1016/j.ijhcs.2013.08.012.
Oyibo K, Orji R, Vassileva J. Developing culturally relevant design guidelines for encouraging physical activity: a social cognitive theory perspective. J Healthc Inform Res. 2018;2(4):319–52. https://doi.org/10.1007/s41666-018-0026-9.
Jones L, Jacklin K, O'Connell ME. Development and use of health-related technologies in Indigenous communities: Critical Review. J Med Internet Res. 2017;19(7):e256. https://doi.org/10.2196/jmir.7520.
Brusse C, Gardner K, McAullay D, Dowden M. Social media and mobile apps for health promotion in Australian Indigenous populations: scoping review. J Med Internet Res. 2014;16(12):e280. https://doi.org/10.2196/jmir.3614.
Hobson GR, Caffery LJ, Neuhaus M, Langbecker DH. Mobile health for First Nations populations: systematic review. JMIR Mhealth Uhealth. 2019;7(10):e14877. https://doi.org/10.2196/14877.
Reilly R, Stephens J, Micklem J, Tufanaru C, Harfield S, Fisher I, et al. Use and uptake of web-based therapeutic interventions amongst Indigenous populations in Australia, New Zealand, the United States of America and Canada: a scoping review. Syst Rev. 2020;9(1):123. https://doi.org/10.1186/s13643-020-01374-x.
Toombs E, Kowatch KR, Dalicandro L, McConkey S, Hopkins C, Mushquash CJ. A systematic review of electronic mental health interventions for Indigenous youth: results and recommendations. J Telemed Telecare. 2020:0(0);1-14;1357633X19899231.
Hensel JM, Ellard K, Koltek M, Wilson G, Sareen J. Digital health solutions for Indigenous mental well-being. Curr Psychiatry Rep. 2019;21(8):68. https://doi.org/10.1007/s11920-019-1056-6.
Orlowski SK, Lawn S, Venning A, Winsall M, Jones GM, Wyld K, et al. Participatory research as one piece of the puzzle: a systematic review of consumer involvement in design of technology-based youth mental health and well-being interventions. JMIR Hum Factors. 2015;2(2):e12. https://doi.org/10.2196/humanfactors.4361.
Thabrew H, Fleming T, Hetrick S, Merry S. Co-design of eHealth interventions with children and young people. Frontiers in Psychiatry. 2018;9(481):1–6.
Vandekerckhove P, DeMul M, Bramer W, DeBont A. Generative participatory design methodology to develop electronic health interventions: systematic literature review. J Med Internet Res. 2020;22(4):e13780. https://doi.org/10.2196/13780.
Moore G, Wilding H, Gray K, Castle D. Participatory Methods to engage health service users in the development of electronic health resources: systematic review. J Participat Med. 2019;11(1):e11474. https://doi.org/10.2196/11474.
Hagen P, Collin P, Metcalf A, Nicholas M, Rahilly K, Swainston N. Participatory design of evidence-based online youth mental health promotion, prevention, early intervention and treatment. Melbourne: Young and Well Cooperative Research Centre; 2012.
Hudson M, Milne M, Russell K, Smith B, Reynolds P, Atatoa-Carr P. The development of guidelines for indigenous research ethics in Aotearoa/New Zealand. In: Drugge A-L, editor. Ethics in Indigenous Research, Past Experiences – Future Challenges. Umea: Vaartoe Centre for Sami Research, Umea University; 2016. p. 157–74.
Hudson M, Milne M, Reynolds F, Russell CL, Smith BB. Te Ara Tika Guidelines for Māori research ethics: a framework for researchers and ethics committee members. Health Research Council of New Zealand; 2009.
NHMRC. Ethical conduct in research with Aboriginal and Torres Strait Islander Peoples and communities: guidelines for researchers and stakeholders. 2018.
Panel on Research Ethics. TCPS 2 (2018) – Chapter 9: research involving the First Nations, Inuit and Métis Peoples of Canada Cananda: Government ofCanada; 2020. [Available from: https://ethics.gc.ca/eng/tcps2-eptc2_2018_chapter9-chapitre9.html]. Accessed 22 July 2020.
National Ethics Advisory Committee. National ethical standards for health and disability research and quality improvement. Ministry of Health: Wellington; 2019.
NHMRC. National statement on ethical conduct in human research. 2007.
Fitzpatrick EFM, Martiniuk ALC, D’Antoine H, Oscar J, Carter M, Elliott EJ. Seeking consent for research with indigenous communities: a systematic review. BMC Med Ethics. 2016;17(1):65. https://doi.org/10.1186/s12910-016-0139-8.
Maar MA, Beaudin V, Yeates K, Boesch L, Liu P, Madjedi K, et al. Wise practices for cultural safety in electronic health research and clinical trials with indigenous people: secondary analysis of a randomized clinical trial. J Med Internet Res. 2019;21(11):e14203. https://doi.org/10.2196/14203.
Huria T, Palmer SC, Pitama S, Beckert L, Lacey C, Ewen S, et al. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med Res Methodol. 2019;19(1):173. https://doi.org/10.1186/s12874-019-0815-8.
Salmon M, Doery K, Dance P, Chapman J, Gilbert R, Williams R, et al. Defining the indefinable: descriptors of Aboriginal and Torres Strait Islander Peoples' cultures and their links to health and wellbeing.; 2018.
Salmon M, Skelton F, Thurber K, Gosling J, Lovett R, Walter M. Intergenerational and early life influences on the well-being of Australian Aboriginal and Torres Strait Islander children: overview and selected findings from Footprints in Time, the longitudinal study of Indigenous children. J Dev Orig Health Dis. 2019;10(1):17–23. https://doi.org/10.1017/S204017441800017X.
Australian Institute of Health Welfare. Aboriginal and Torres Strait Islander adolescent and youth health and wellbeing 2018. Canberra: AIHW; 2018.
Hinton R, Kavanagh DJ, Barclay L, Chenhall R, Nagel T. Developing a best practice pathway to support improvements in Indigenous Australians' mental health and well-being: a qualitative study. BMJ Open. 2015;5(8):e007938. https://doi.org/10.1136/bmjopen-2015-007938.
Jones R, Thurber K, Chapman J, Dunbar T, Wenitong M, Eades S, et al. Study protocol: our cultures count, the Mayi Kuwayu study, a national longitudinal study of Aboriginal and Torres Strait Islander wellbeing. BMJ Open. 2018;8(6):e256.
Kral I. Plugged in: Remote Australian Indigenous youth and digital culture. Canberrra: Australian National University; 2010.
Povey J, Mills PPJR, Dingwall KM, Lowell A, Singer J, Rotumah D, et al. Acceptability of mental health apps for Aboriginal and Torres Strait Islander Australians: a qualitative study. J Med Internet Res. 2016;18(3):e65. https://doi.org/10.2196/jmir.5314.
World Health Organisation. Engaging young people for health and sustainable development: strategic opportunities for the World Health Organization and partners. Geneva: World Health Organization; 2018.
Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5(1):69. https://doi.org/10.1186/1748-5908-5-69.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. https://doi.org/10.1186/s12874-018-0611-x.
Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616.
Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid-Based Healthcare. 2015;13(3):141–6. https://doi.org/10.1097/XEB.0000000000000050.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Sawyer S, Azzopardi P, Wickremarathne D, Patton G. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223–8. https://doi.org/10.1016/S2352-4642(18)30022-1.
Shand F, Mackinnon A, O’Moore K, Ridani R, Reda B, Hoy M, et al. The iBobbly Aboriginal and Torres Strait Islander app project: study protocol for a randomised controlled trial. Trials. 2019;20(1):198. https://doi.org/10.1186/s13063-019-3262-2.
Dingwall K, Puszka S, Sweet M, Nagel T. “Like Drawing Into Sand”: Acceptability, Feasibility, and Appropriateness of a New e-Mental Health Resource for Service Providers Working With Aboriginal and Torres Strait Islander People. Aust Psychol. 2015;50(1):60–9. https://doi.org/10.1111/ap.12100.
Titov N, Schofield C, Staples L, Dear BF, Nielssen O. A comparison of Indigenous and non-Indigenous users of MindSpot: an Australian digital mental health service. Australas Psychiatry. 2019:27(4):352–357.
Fleming T, Lucassen M, Stasiak K, Shepherd M, Merry S. The impact and utility of computerised therapy for educationally alienated teenagers: the views of adolescents who participated in an alternative education-based trial. Clin Psychol. 2016;20(2):94–102. https://doi.org/10.1111/cp.12052.
Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual research review: digital health interventions for children and young people with mental health problems – a systematic and meta-review. J Child Psychol Psychiatry. 2017;58(4):474–503. https://doi.org/10.1111/jcpp.12663.
Bergin AD, Vallejos EP, Davies EB, Daley D, Ford T, Harold G, et al. Preventive digital mental health interventions for children and young people: a review of the design and reporting of research. NPJ Digital Med. 2020;3(1):133.
Barak A, Klein B, Proudfoot J. Defining internet-supported therapeutic interventions. Ann Behav Med. 2009;8:4–17.
Joanna Briggs Institute. JBI reviewer's manual: Chapter 11: Scoping reviews [Available from: https://wiki.joannabriggs.org/display/MANUAL/Chapter+11%3A+Scoping+reviews]. Accessed 30 July 2020.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. https://doi.org/10.1111/nhs.12048.
Funding
JP was supported by Charles Darwin University, Research Training Program Stipend Scholarship and an Ian Scott Mental Health, Australian Rotary Health Scholarship. Funders were not involved in developing the protocol.
Author information
Authors and Affiliations
Contributions
JP designed and wrote the manuscript. BR, KD and MT helped design and edit the manuscript. TN, AL, MS, PPJRM and FS provided advice and reviewed and revised the manuscript. The authors read and approved the final manuscript.
Authors’ information
JP, BR, MS, KD, TN and PPJRM work at Menzies School of Health Research. FS and MT work for Black Dog Institute & University of New South Wales. AL works at Charles Darwin University. Collectively the research team have extensive experience in Indigenous Health Research, the digital mental health field and qualitative research methods.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA-P 2015 Checklist.
Additional file 2.
Search terms.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Povey, J., Raphiphatthana, B., Torok, M. et al. Involvement of Indigenous young people in the design and evaluation of digital mental health interventions: a scoping review protocol. Syst Rev 10, 133 (2021). https://doi.org/10.1186/s13643-021-01685-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-021-01685-7