Abstract
Background
Diet-related non-communicable diseases (NCDs) are rapidly increasing worldwide and constitute one of the leading causes of mortality and morbidity. Improving population diets can play an important role in preventing and managing the diseases. Effective and efficient interventions are needed to promote healthy eating behaviors among people. The objective of this review will be to evaluate the effectiveness of social marketing-based interventions to promote healthy nutrition behaviors.
Method
The following electronic databases will be searched from January 1990 onwards: PubMed/MEDLINE, EMBASE, Web of Science, and CENTRAL. We will include randomized and non-randomized trials, quasi-experimental studies, observational studies (e.g., cohort, cross-sectional, and before and after studies) evaluating the social marketing-based intervention.
The primary outcomes will be nutritional behaviors. Secondary outcomes will include the quality of life, nutritional status, and weight status. Two reviewers will independently screen all citations, full-text articles, and abstract data. The study methodological quality (or bias) will be appraised using an appropriate tool. If feasible, we will conduct random-effects meta-analysis. Additional analyses will be conducted to explore the potential sources of heterogeneity (e.g., age, sex, and socio-economic condition).
Discussion
This study will summarize the evidence regarding the interventions’ components, implementation methods, and effectiveness of interventions based on the social marketing framework to promote healthy nutrition behaviors. This review can provide policymakers with the information needed to make decisions and plan to promote healthy eating behaviors and understand the factors influencing the implementation of these programs.
Systematic review registration
Similar content being viewed by others
Background
The growing burden of non-communicable diseases (NCDs) is one of the biggest challenges facing healthcare systems worldwide in the twentyfirst century [1]. NCDs have been identified as major causes of disability and mortality globally. During 2016, about 71.3% of all deaths worldwide were claimed to be due to these diseases [2]. It has been projected that by 2030, NCDs will cause over 75% of all deaths worldwide [3]. Evidence suggests that NCDs are among the main leading causes of death in Iran. According to the latest statistics provided by the World Health Organization, NCDs are responsible for more than 76% of all deaths in Iran. Among these, coronary heart diseases make the most considerable contribution to NCD deaths (by 46%) [4]. The four modifiable behavioral risk factors for NCDs are physical inactivity, unhealthy diet, harmful alcohol use, and tobacco use. It is noteworthy that the NCD-related morbidity and mortality burden due to an unhealthy diet is much more significant than the other three risk factors [5].
During the last four decades, significant changes have taken place in global nutrition patterns. People’s diets have shifted to higher consumption of processed and ultra-processed foods low in nutrients and high in calories [6, 7]. The percentage of foods consumed outside the home, such as fast food, has increased, leading to excessive calorie intake [8]. Besides, there have been significant increases in the consumption of animal-source foods, oils, and caloric sweeteners [9]. In many countries, intakes of sodium, unhealthy fats, and added sugar in the general population are much higher than the recommended amounts [10]. It is important to note that increased consumption of unhealthy foods and beverages has been associated with a lower intake of healthy diet components, including foods with low-energy density and a high content of nutrients such as vegetables, legumes, and whole grains [9]. These dietary shifts have important implications for public health. Unhealthy eating patterns, including high consumption of added sugar, trans fats, and sodium, have been associated with obesity, cardiovascular disease, type 2 diabetes, cancer, high blood pressure, and stroke [11,12,13]. Also, such eating patterns have been reported to kill more than 14 million people worldwide each year, equivalent to 40% of deaths due to NCDs [14].
According to the World Health Organization, a healthy diet includes achieving energy balance, limiting energy intake from total fats, replacing saturated fats with unsaturated fats, eliminating trans fatty acids, limiting the intake of free sugars, limiting salt (sodium) consumption from all sources, and increasing consumption of fruits and vegetables, and legumes, whole grains, and nuts [15]. Many efforts have been made to develop nutritional interventions around the world. These primary prevention programs focus on asymptomatic individuals in the general population before an adverse health event occurs [16]. The goal of interventions at this stage is to reduce non-communicable disease risk factors by promoting healthy diets. There are powerful potential interventions that target the factors mentioned above and the cost, access to healthy foods, and individuals’ knowledge. It should be noted that such population interventions, by their nature, should be theoretically useful for all members of society, including those with a history of non-communicable diseases such as cardiovascular disease [17]. However, given the poor quality of the average diet, it is clear that current approaches to improve public nutrition have not been successful and that effective strategies are urgently needed [18].
Health-related behaviors, including nutritional behaviors, are influenced by a wide variety of factors. Understanding the multifactorial nature of these behaviors and the contexts in which they occur is essential for developing effective behavior change interventions. Having a clear theoretical underpinning has been suggested to maximize behavior change interventions [19,20,21]. Evidence shows that theory-based interventions effectively influence health-related behaviors than non-theory-based ones [22,23,24]. These types of studies provide a framework for developing and evaluating interventions [25]. They also facilitate understanding the factors influencing behavior change and the reasons for an intervention’s success or failure [26, 27]. One of the behavioral theories that is widely used to influence health behavior is social marketing.
There are many definitions of social marketing, but one of the most useful ones describes social marketing as follows: “Social marketing is the application of commercial marketing technologies to analyze, plan, implement, and evaluate programs designed to influence the voluntary behavior of the target audiences to improve their personal and social well-being” [28]. The unique feature of social marketing is that it takes learning from the commercial sector and applies it to induce, encourage, and promote social change entirely, rather than to provide ideas or information [29]. The strengths of social marketing over alternative techniques applied to behavior change include (1) focusing on the consumer—this means that interventions are designed based on the consumers’ wants and needs, not only the priorities of society as a whole [30]; (2) proposing attractive exchanges for the consumer, which makes it possible to change voluntary behavior; in other words, it focuses on convincing not on coercion [31], (3) identifying and appropriately addressing competition to make the recommended products or health behaviors more advantageous than the unhealthy ones [32], and (4) using all the marketing mix components (the basic 4 Ps: product, price, place, and promotion). In social marketing, a product is developed (key benefits, service, or behavior change), the price is evaluated (the costs of stopping an unhealthy behavior or adopting a healthy one, which can be in the form of money, time, opportunity, energy, effort, psychological factors, etc.), the place is defined (the situations in which the target audience can perform the health behavior or obtain any tangible goods or services necessary for the health behavior), and a promotion strategy is planned (selecting promotion techniques and channels) [33], (5) managing programs properly through planning, control, monitoring, implementation, and evaluation [28]. Accordingly, social marketing can be an excellent tool for promoting public health activities.
It is not a new idea to use marketing principles in health education and health promotion to achieve health or social goals [34,35,36]. Social marketing has been applied to solve behavioral problems for more than 40 years [37]. There are many examples of effective use of social marketing framework in the field of public health, including promoting healthy eating behaviors [38], prevention and control of AIDS [39], reducing alcohol consumption in youth and adolescents [40], and increasing physical activity [41]. Given the effectiveness of social marketing in changing health behaviors, the present review intends to collect interventional studies that have used the social marketing framework to promote healthy eating behaviors. The objective of this review will be to evaluate the effectiveness of social marketing-based interventions to promote healthy nutrition behaviors.
Methods
Protocol and registration
The present protocol was registered in the PROSPERO database under registration number CRD42020163972 and is being reported according to guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement [42], (see Additional file 1). The proposed systematic review will be conducted based on the methodological guidance from the Cochrane Collaboration Handbook of Systematic Reviews [43] and will be reported following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Statement [44]. Relevant changes to the protocol will be documented and published within the results of the final review.
Eligibility criteria
Types of studies
We will include different types of study designs, including randomized-controlled trials (including cluster trials), non-randomized controlled trials, quasi-experimental studies, and observational studies (including cohort studies, cross-sectional studies, and before-after studies). Pre-and post-interventions are also common and will help determine the effect (if any) of interventions within a single community. The controlled cohort studies and cross-sectional studies will help identify differences in the communities’ outcomes, either overtime or within a particular point in time, respectively.
Types of participants
All population groups, including children, adolescents, adults, or older adults, and the community in different settings (kindergarten, school, home, or community), will be examined.
Types of interventions
The following interventions will be included in the study:
Any intervention to improve eating behaviors including increasing fruit and vegetable, legumes, whole grains, and nuts intake, healthy and low-fat choices (e.g., snack or meal alternatives with lower fat, energy, salt, sugar or higher fiber), other behaviors including variety, novel foods, fiber intake, low-sodium intake, consuming healthy breakfasts, healthy school lunches, and the emphasis on daily water consumption [45,46,47,48,49,50,51,52].
Studies must be social marketing-based interventions to promote healthy nutrition behaviors. The interventions that consider all the marketing mix components to improve nutritional behaviors will be included. It consists of the basic 4 Ps of product, price, place, and promotion. Product refers to healthy eating behaviors. Price refers to the cost for the promised benefits or the barriers that may prevent the people from performing healthy eating behaviors and what methods used in interventions to remove these barriers. Place refers to the location where people can obtain information about healthy eating behaviors, and finally, promotion includes the type of persuasive communication to improve eating behaviors.
The evidence from qualitative research will also be used to explain the effect of social marketing-based interventions on nutrition behaviors.
Types of outcome measures
Studies will be included in the review if they have quantifiable measures of the primary outcome. The primary outcomes will be nutritional behaviors including the following:
-
Increased daily consumption of fruit, vegetables, legumes (e.g., lentils and beans), nuts, and whole grains servings [45].
-
Healthy choices, including snack or meal alternatives with lower fat, energy, salt, sugar, or higher fiber. Less than 5 g of salt (equivalent to about one teaspoon) per day [46].
-
Improvement in dietary intake indicators (e.g., Dietary Diversity Score (DDS) and Healthy Eating Index (HEI), diet quality indices (DQI), and Healthy Dietary Habits Index (HDHI)) [53, 54].
-
Prefer unsaturated fats (found in fish, avocado and nuts, and in sunflower, soybean, canola, and olive oils) to saturated fats (found in fatty meat, butter, palm and coconut oil, cream, cheese, ghee, and lard) and trans-fats of all kinds, including both industrially produced trans-fats (found in baked and fried foods, and pre-packaged snacks and foods, such as frozen pizza, pies, cookies, biscuits, wafers, and cooking oils and spreads) and ruminant trans-fats (found in meat and dairy foods from ruminant animals, such as cows, sheep, goats, and camels).
-
Reduced intake of saturated fats to less than 10% of total energy intake and trans-fats to less than 1% of total energy intake [49].
-
Reduced intake of industrially produced trans-fats [50, 51].
-
Less than 10% of total energy intake from free sugars [45, 52]. Free sugars are all sugars added to foods or drinks by the manufacturer, cook, consumer, and sugars naturally present in honey, syrups, fruit juices, and fruit juice concentrates.
-
Other behaviors, including variety, novel foods, consuming healthy breakfasts, healthy school lunches, and the emphasis on daily water consumption [45].
Secondary outcomes will include improvement in the quality of life, nutritional status, and weight status.
Only articles published in English will be included. We will exclude reviews, methodological articles, and conceptual documents (e.g., non-empirical studies). We will exclude studies without a control group, not reporting outcome data, and/or addressing diseased/medically diagnosed populations.
Information sources and search strategy
The primary source of literature will be a structured search of major electronic databases (from January 1990 onwards): PubMed/MEDLINE, EMBASE, Web of Science, and the Cochrane Central Register of Controlled Trials (CENTRAL). The secondary source of potentially relevant material will be a search of the grey or difficult to locate literature, including ProQuest and Google Scholar. We will perform hand-searching of the reference lists of included studies, relevant reviews, or other relevant documents. Authors who are prolific in the field will be contacted. The literature searches will be designed and conducted by the review team, including an experienced health information specialist. The search will include a broad range of terms and keywords related to nutrition behavior, social marketing, and interventions. A draft search strategy for the main databases is provided in Additional file 2.
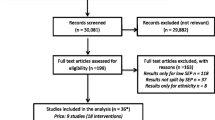
Data management and selection process
All the identified studies of different sources will be transferred to Endnote and systematically de-duplicated through The Systematic Review Assistant-Deduplication Module (SRA-DM). This freely available application has greater sensitivity and specificity than Endnote for the de-duplication process [55]. The remaining studies will be screened for eligibility by two independent reviewers. The resolution of any conflicts will be made by a third independent reviewer or by discussion. The reasons for the exclusion of any article will be documented. A full-text screening will then be carried out. A PRISMA flow chart showing details of studies included and excluded at each stage of the study selection process will be provided [56].
Data extraction
We will extract data from the included studies using the pre-standardized data extraction form (see Additional file 3). The form will be tested and adapted as necessary before using it. Data extraction form will capture the following data fields: study title, author(s), publication year, geographic origin, study design, enrolment period, sample size, duration of intervention, participant characteristics (age, sex), intervention type, and its components, primary and secondary outcomes. Two authors will independently extract the data. We will discuss any differences between the two data extraction sheets to reach a consensus or consult a third author if an agreement is impossible to achieve. We will also contact study authors to obtain any missing information or clarify unclear data by getting the original report.
Assessment of risk of bias in included studies
To estimate the potential bias that will be most relevant for the study, we will use the following tools: the Cochrane tool for assessing the risk of bias in randomized trials (RoB 2 tool) [57], the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) [58], and the Newcastle–Ottawa Scale (NOS) for observational studies [59]. Two authors (AD & MB) will independently assess the risk of bias in each included study. Potential conflicts will be resolved through discussion.
Measures of intervention effect
Where continuous scales of measurement are used to assess the effects of the intervention (e.g., mean number of servings of fruit and vegetable consumption, nutrition knowledge scores), the mean difference (MD) will be used, or the standardized mean difference (SMD) if different scales have been used. When considering studies with multiple intervention groups, we will try to combine all relevant experimental intervention groups into a single group to enable a single pairwise comparison. For considering cross-over studies, we will only use data from the first period. If the meta-analysis is not performed, the reason will be provided. At this stage, the findings will be summarized and discussed. Conclusions will also be formed based on the power of each of the studies. After summarizing the results and providing conclusions, the specific features associated with effective interventions will be identified.
Dealing with missing data
Studies with missing data will also be included in the systematic review. Any further information required from the original author will be requested by written correspondence (e.g., emailing the corresponding author) and any relevant information obtained in this manner. Attrition rates, for example, drop-outs, losses to follow-up, and withdrawals will be investigated.
Data synthesis
The data from each paper (e.g., study characteristics, context, participants, outcomes, and findings) will be used to build evidence tables of an overall description of included studies. Effect sizes (e.g., MD) will be presented along with 95% confidence intervals. If feasible and appropriate, effect sizes from primary studies will be used to perform random-effects meta-analyses. Since heterogeneity is expected a priori, we will estimate the pooled effect sizes using the random-effects model. The random-effects model assumes the study prevalence estimates follow a normal distribution, considering both within-study and between-study variation. Forest plots will be used to visualize the extent of heterogeneity among studies. We will quantify statistical heterogeneity by estimating the variance between studies using I2 statistic [60]. I2 ranges between 0% and 100% (with values of 0–25% and 75–100% taken to indicate low and considerable heterogeneity, respectively). We will also report Cochran Q test with a P value of 0.05 considered statistically significant (heterogeneity).
Additional analyses
If sufficient data are available, we will conduct a subgroup analysis to explore possible heterogeneity sources (e.g., participants, interventions, and study quality). Heterogeneity among participants could be related to age (e.g., elderly, adults, children, and adolescents), sex (male versus female), geographic location (e.g., urban versus rural, country, or region), and socio-economic condition. Heterogeneity in interventions could be related to how the intervention is delivered, components of the intervention, the duration of the intervention, and settings (kindergarten, school, home, or community). Publication bias will be assessed by inspection of the funnel plots for asymmetry and with Egger’s test [61] and Begg’s test [62], with the results considered to indicate potential small study effects when P values are < 0.10.
Software to be used
All analyses will be conducted using STATA (13.0; Stata Corporation, College Station, Texas, USA Stata).
Quality assessment of included studies
Data extraction form also includes an overall grading of the evidence related to each of the main outcomes using the GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) approach. It is the most flexible methodology for evaluating the evidence (downgrading, upgrading, handling indirect evidence, etc.) The GRADE approach defines the quality of a body of evidence as to the extent to which one can be confident that an estimate of effect or association is close to the true quantity of specific interest [63].
Discussion
There is no doubt that diet quality has a major impact on health. A higher-quality diet has always been associated with better health outcomes [64, 65]. The relationship between diet and health is an undeniable cause-and-effect one [66]. This causal relationship has been proven through very detailed studies aimed at identifying causal pathways whereby specific nutrients affect health [67] and the high-quality intervention trials such as those incorporating the Mediterranean diet [68, 69]. Diet is currently among the leading preventable causes of mortality and disability in nearly all countries [70, 71]. Given the role of unhealthy nutrition in increasing the prevalence of non-communicable diseases [72], it is not unreasonable to expect an important step to prevent diseases and reduce mortality rates by correcting eating habits and food choices. However, the critical issue is that it is challenging to implement and maintain health-promoting behaviors, including healthy eating behaviors. This issue is significantly exacerbated in environments where low nutritional value and low-cost ready-to-eat foods are readily available and frequently advertised [73, 74].
Examining the available evidence and modeling based on practical and successful studies is considered the first step to facilitate policy improvement and design effective programs to promote healthy eating behaviors. On the other hand, an essential step for the final judgment on the types of interventions and their impact on promoting healthy eating behaviors is to conduct a systematic review of related studies [75]. Therefore, the present study is intended to collect articles related to interventions based on the social marketing approach to promoting healthy eating behaviors by searching for relevant scientific literature. After the final selection and extraction of papers, the components of the interventions, implementation methods, and their effectiveness will be identified and reported in a systematic review article to guide design interventions with the same purpose.
This systematic review will be restricted to articles in English due to functional reasons, and therefore could miss relevant papers published in other languages.
The review results can provide policymakers with the information needed to make decisions and plan to promote healthy eating behaviors and understand the factors influencing the programs’ implementation.
This review is intended for publication in a peer-reviewed journal. Analyses and scripts will be made publicly available. Any changes to the protocol will be documented as well.
Availability of data and materials
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Abbreviations
- NCDs:
-
Non-communicable diseases
- WHO:
-
World Health Organization
- ISMA:
-
International Social Marketing Association
- ESMA:
-
European Social Marketing Association
- AASM:
-
Australian Association of Social Marketing
- PRISMA-P:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis Statement-Protocol Extension
- RCT:
-
Randomized controlled trial
- DDS:
-
Dietary Diversity Score
- GRADE:
-
Grades of Recommendation, Assessment, Development, and Evaluation
- SMD:
-
Standard mean difference
- MD:
-
Mean difference
References
Atun R, Jaffar S, Nishtar S, Knaul FM, Barreto ML, Nyirenda M, et al. Improving responsiveness of health systems to non-communicable diseases. Lancet. 2013;381(9867):690–7.
Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–544.
Wang Y, Wang J. Modelling and prediction of global non-communicable diseases. BMC Public Health. 2020;20:1–13.
Organization WH. Noncommunicable diseases country profiles. 2014. Available from: www.who.int/nmh/countries/irn_en.pdf?ua=1.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60.
Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–9.
Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14:21–8.
Duffey KJ, Popkin BM. Energy density, portion size, and eating occasions: contributions to increased energy intake in the United States, 1977–2006. PLoS Med. 2011;8(6):e1001050.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21.
Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozaffarian D. Global, regional and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open. 2015;5(9):e008705.
Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health. 2007;97(4):667–75.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220.
Mozaffarian D, Aro A, Willett WC. Health effects of trans-fatty acids: experimental and observational evidence. Eur J Clin Nutr. 2009;63(S2):S5.
Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366(9496):1578–82.
Organization WH. Healthy diet. 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/healthy-diet. Accessed 01 July 2020.
NICE. Prevention of cardiovascular disease. Manchester: NICE Public Health Guidance 25; 2010.
McGill R, Anwar E, Orton L, Bromley H, Lloyd-Williams F, O’Flaherty M, et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health. 2015;15(1):457.
Lenoir-Wijnkoop I, Gutiérrez-Ibarluzea I, Dubois DJ. Today’s nutrition and tomorrow’s public health: challenges and opportunities: Frontiers Media SA; 2016.
Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9(3):323–44.
Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Commun Theory. 2003;13(2):164–83.
Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399–418.
Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673.
Cane J, Richardson M, Johnston M, Ladha R, Michie S. From lists of behaviour change techniques (BCT s) to structured hierarchies: comparison of two methods of developing a hierarchy of BCT s. Br J Health Psychol. 2015;20(1):130–50.
Fadhil A, Gabrielli S, editors. Addressing challenges in promoting healthy lifestyles: the al-chatbot approach. Proceedings of the 11th EAI international conference on pervasive computing technologies for healthcare. 2017.
Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379.
Nigg CR, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: common themes advancing health behavior research. Health Educ Res. 2002;17(5):670–9.
Lubans DR, Foster C, Biddle SJ. A review of mediators of behavior in interventions to promote physical activity among children and adolescents. Prev Med. 2008;47(5):463–70.
Andreasen A. Marketing social change: changing behavior to promote health, social development and the environment. San Francisco: Jossey- Bass; 1995.
Da Silva EC, Mazzon JA. Developing social marketing plan for health promotion. Int J Public Adm. 2016;39(8):577–86.
French J, Blair-Stevens C. Social marketing national benchmark criteria. London: UK National Social Marketing Centre; 2006. Available: http://www.snh.org.uk/pdfs/sgp/A328466.pdf. Accessed 2 July 2014
Stead M, Gordon R, Angus K, McDermott L. A systematic review of social marketing effectiveness. Health Educ. 2007;107(2):126–91.
Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health. 2005;26:319–39.
Shams M. Social marketing for health: theoretical and conceptual considerations. In: Haider M, Platter H, editors. Selected issues in global health communications. London: Intechopen; 2018. p. 43–55.
Hastings G, Haywood A. Social marketing and communication in health promotion. Health Promot Int. 1991;6(2):135–45.
Wiebe GD. Merchandising commodities and citizenship on television. Public Opin Q. 1951;15(4):679–91.
Craig Lefebvre R, Flora JA. Social marketing and public health intervention. Health Educ Q. 1988;15(3):299–315.
Lefebvre RC. An integrative model for social marketing. J Soc Mark. 2011;1(1):54–72.
Young L, Anderson J, Beckstrom L, Bellows L, Johnson SL. Using social marketing principles to guide the development of a nutrition education initiative for preschool-aged children. J Nutr Educ Behav. 2004;36(5):250–7.
Meekers D. The role of social marketing in sexually transmitted diseases/HIV protection in 4600 sexual contacts in urban Zimbabwe. Aids. 2001;15(2):285–7.
Palmer RS, Kilmer JR, Larimer ME. If you feed them, will they come? The use of social marketing to increase interest in attending a college alcohol program. J Am Coll Heal. 2006;55(1):47–52.
Wong F, Huhman M, Asbury L, Bretthauer-Mueller R, McCarthy S, Londe P, et al. VERB™—a social marketing campaign to increase physical activity among youth. Prev Chronic Dis. 2004;1(3).
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Higgins J. Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 [updated March 2011]: The Cochrane Collaboration; 2011. www.cochrane-handbook.org
Welch V, Petticrew M, Tugwell P, Moher D, O'Neill J, Waters E, et al. PRISMA-Equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. 2012;9(10):e1001333.
WHO. Diet, nutrition, and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation: World Health Organization; 2003.
WHO. Guideline: sodium intake for adults and children: World Health Organization; 2012.
Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell CD, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev. 2015;8.
Joint F. Fats and fatty acids in human nutrition. Report of an expert consultation, 10-14 November 2008, Geneva. 2010.
WHO. Guidelines: saturated fatty acid and trans—fatty acid intake for adults and children. Geneva: WHO; 2018.
Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4):e1000058.
WHO. Replace trans fat: an action package to eliminate industrially-produced trans-fatty acids: World Health Organization; 2019.
WHO. Guideline: sugars intake for adults and children: World Health Organization; 2015.
Kourlaba G, Panagiotakos DB. Dietary quality indices and human health: a review. Maturitas. 2009;62(1):1–8.
Wong JE, Haszard JJ, Howe AS, Parnell WR, Skidmore PM. Development of a healthy dietary habits index for New Zealand adults. Nutrients. 2017;9(5):454.
Rathbone J, Carter M, Hoffmann T, Glasziou P. Better duplicate detection for systematic reviewers: evaluation of Systematic Review Assistant-Deduplication Module. Syst Rev. 2015;4(1):6.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj. 2016;355.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. 2019. [Cited February 12, 2020]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–34.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994:1088–101.
Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Interpreting results and drawing conclusions. Cochrane Handb Syst Rev Intervent. 2019:403–31.
Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis-art. No. A1344. Br Med J. 2008;337(7671):NIL_44-NIL_50.
Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. 2013;99(1):181–97.
Segal L, Opie RS. A nutrition strategy to reduce the burden of diet related disease: access to dietician services must complement population health approaches. Front Pharmacol. 2015;6:160.
Parletta N, Milte CM, Meyer BJ. Nutritional modulation of cognitive function and mental health. J Nutr Biochem. 2013;24(5):725–43.
De Lorgeril M, Salen P, Martin J-L, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85.
Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514–63.
Organization WH. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. Available from: http://www.who.int/iris/handle/10665/44203. Accessed 18 Aug 2018
Scarborough P, Nnoaham KE, Clarke D, Capewell S, Rayner M. Modelling the impact of a healthy diet on cardiovascular disease and cancer mortality. J Epidemiol Community Health. 2012;66(5):420–6.
Brandstetter S, Rüter J, Curbach J, Loss J. A systematic review on empowerment for healthy nutrition in health promotion. Public Health Nutr. 2015;18(17):3146–54.
Liberato SC, Bailie R, Brimblecombe J. Nutrition interventions at point-of-sale to encourage healthier food purchasing: a systematic review. BMC Public Health. 2014;14(1):919.
Khan K, Kunz R, Kleijnen J, Antes G. Systematic reviews to support evidence-based medicine: Crc Press; 2011.
Acknowledgements
This review will be conducted by the approval and funding of the Shahid Beheshti University of Medical Sciences (SBMU). The authors hereby express their gratitude to the SBMU.
Funding
This review will be financially supported by a grant from the Shahid Beheshti University of Medical Sciences to MB (Grant Number: 1397/73627). The funder had no role in developing the protocol.
Author information
Authors and Affiliations
Contributions
MB and AD conceived and designed the study. MB and AD developed the search strategy. The initial draft of the protocol was prepared, revised, and finalized by MB and AD. The authors read and approved the final protocol.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of National Nutrition and Food Technology Research Institute at Shahid Beheshti University of Medical Sciences (IR. SBMU.nnftri.1397.031).
Consent for publication
Not applicable
Competing interests
Authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Doustmohammadian, A., Bazhan, M. Social marketing-based interventions to promote healthy nutrition behaviors: a systematic review protocol. Syst Rev 10, 75 (2021). https://doi.org/10.1186/s13643-021-01625-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-021-01625-5