Abstract
Background
Epstein-Barr virus (EBV) is considered to be closely associated with nasopharyngeal carcinoma (NPC), in which EBV-encoded latent membrane protein 1 (LMP1) was found to have an oncogenic role. However, the results published on the LMP1 polymorphism are inconsistent. In the present study, we performed a meta-analysis to determine the frequency of the associations and a more precise association between NPC and EBV LMP1 gene variants (30-bp deletion (del)/XhoI-loss).
Methods
Eligible articles met the inclusion/exclusion criteria and were identified in the following electronic databases: PubMed, ScienceDirect, and SciELO. Consequently, the data of interest were extracted and plotted in a table to calculate the frequency and odds ratio (OR) of the outcomes of interest (30-bp del-LMP1/XhoI-loss) in patients with NPC. Study quality (Newcastle-Ottawa Scale (NOS)), publication bias, and heterogeneity were assessed.
Results
Thirty-one observational studies were included with a total of 2,846 individuals (NPC, n = 1,855; control, n = 991). The risk of bias in relation to study quality evaluated by NOS was considered low. The pooled estimate of the frequency of 30-bp del-LMP1 and XhoI-loss in patients with NPC was 77% (95% confidence interval (CI): 72 to 82) and 82% (95% CI: 71 to 92), respectively. There was an association between 30-bp del-LMP1 and NPC susceptibility (OR = 2.86, 95% CI: 1.35 to 6.07, P = 0.00). Similarly, there was an association between XhoI-loss and NPC (OR = 8.5, 95% CI: 1.7 to 41, P = 0.00). However, when we analyze the co-existence of the 30-bp del-LMP1 and XhoI-loss in patients with NPC, there was no association (OR = 1.09, 95% CI: 0.06 to 18.79, P = 0.002).
Conclusions
Our results suggest an association between the 30-bp del-LMP1 and XhoI-loss with NPC susceptibility. However, our data should be interpreted with caution because the sample size was small, and there was heterogeneity between the studies. Thus, future studies are needed with adjusted estimates to simultaneously evaluate multiple factors involved in the development of NPC.
Systematic review registration
PROSPERO CRD42014013496.
Similar content being viewed by others
Background
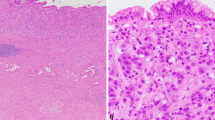
Nasopharyngeal carcinoma (NPC) is an aggressive tumor associated with Epstein-Barr virus (EBV) that initially affects the layer of epithelial cells in the nasopharynx and preferably arises in the Rosenmüller’s fossa [1,2]. NPC is also defined as a peculiar type of head and neck cancer due to its clinical status, etiology, pathology, epidemiology, and manner of response to treatment [3,4]. In view of these factors, EBV and NPC have very distinct epidemiological and clinical patterns, given that EBV is ubiquitous and causes a latent infection in 95% of the world population, with the majority of these infections being benign [5]. However, the worldwide incidence of NPC is considered rare, and affected individuals for many years had a poor prognosis that reflected in a reduced survival rate, but actually the survival of NPC patients is relatively high under the current treatment protocol and the introduction of intensity-modulated radiotherapy (IMRT) [6].
Although NPC endemicity is rare in most parts of the world [7], there is a striking geographic and ethnic distribution of cases characterized by existing areas of high endemicity (Southeast Asia), intermediate endemicity (Eastern Mediterranean and North Africa), and low endemicity (Americas). According to data provided by GLOBOCAN 2012 [8], in the same period in the world, the total number of NPC was 86,691 cases (age-standardized rate (ASR), 1.2/100,000)), while the number of deaths was 50,831 (ASR = 0.7/100,000). Among these cases, China was the country that contributed the most to these indices because it had the highest total number (33,198, ASR = 1.9/100,000) and deaths (20,404, ASR = 1.2/100,000) by NPC, followed by Indonesia (13,084 cases, ASR = 5.6/100,000 and 7,391 deaths with ASR = 3.3/100,000) and Vietnam (4,931 cases, ASR = 5.4/100,000 and 2,885 deaths with ASR = 3.3/100,000).
EBV infects the mucosal epithelium and B cells and consequently establishes a latent infection, and aberrant infection by EBV can to cause the appearance of tumors in these locations of replication [9]. Hence, infected cells may present physiological changes that result from the expression of latent genes, including mainly EB-encoded early RNAs (EBER), EBV nuclear antigens (EBNA1/2/3a,b,c) and latent membrane protein 1 or 2 (LMP1/2) [10].
The first protein from EBV to have its oncogenic properties empirically demonstrated was LMP1 [11], which is expressed on the cell surface, where it spontaneously aggregates to form a constitutively activated receptor, acting as a member of the tumor necrosis factor receptor (TNF-R) family and allowing LMP1 to exert an influence on the cell through interactions with different cellular molecules involved in an intracellular signaling cascade [12-15]. Consequently, a number of studies have shown the involvement of LMP1 in the pathogenesis of NPC [16,17], which involves the following factors: 1) an inhibition of apoptosis in the infected cells by the upregulation of Bcl-2 and A-20 genes [13,15,18]; 2) a modulation of the morphology and motility of epithelial cells [19]; 3) a downregulation of several suppressors for metastases [20]; 4) a promotion of angiogenesis [21]; and 5) an induction of the expression of proinflammatory cytokines, among other mechanisms [22,23]. LMP1 is an integral membrane protein that can be divided into three domains: 1) a short cytoplasmic N-terminal tail (amino acids 1 to 23); 2) six transmembrane alpha-helical of hydrophobic nature (amino acids 24 to 186); and 3) a long cytoplasmic C-terminal tail (amino acids 187 to 386), with this region having the highest LMP1 signaling activity. Therefore, the long cytoplasmic C-terminal tail has three distinct functional domains: C-terminal activation regions 1, 2, and 3 (CTAR1/2/3) [24,25].
The LMP1 gene has been shown to have polymorphisms, among which the occurrence of a 30-bp deletion is prominent, as compared with the prototype B95-8 LMP1, and occurs near the end of the cytoplasmic C-terminal tail and close to the functional domain CTAR2. This feature deletion has been studied, and it has been established that the 30-bp deletion results in an increased oncogenic activity of infected cells and results in a more aggressive phenotype of EBV-associated tumors [26,27]. In addition, another mutation observed in the LMP1 gene, albeit a point mutation, occurs at nucleotide position G169425T, resulting in the loss of a restriction site known as XhoI, which is present in the cytoplasmic N-terminal tail. Thus, the XhoI polymorphism has been commonly found in samples from patients with NPC but is absent in samples from healthy individuals [28,29]. However, in general, the results of the studies are ambiguous regarding the association of these variants in the EBV LMP1 gene with the risk of developing NPC. In this sense, this meta-analysis was performed to solve the problem of inadequate statistical power and of the controversial and ambiguous results.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol, which provides rules and guidelines for systematic reviews and meta-analysis [30]. The PRISMA checklist is shown in Additional file 1. In addition, we prospectively recorded the study protocol in PROSPERO with the registration number CRD42014013496, available on the website http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014013496#.VBg8HoctBdg.
The identification and eligibility of relevant studies
To address our study hypothesis, the following electronic databases were searched: PubMed, ScienceDirect, and SciELO. The selection period lasted until the beginning of September 2014, and the language of the studies to be selected should be expressed in English, Spanish, or Portuguese. Therefore, in these three electronic databases, the following keywords related to our research topic were added: Epstein-Barr virus OR EBV OR virus AND cancer OR tumor OR neoplasia OR nasopharyngeal carcinoma AND LMP1 30-bp deletion OR LMP1 variant OR BNLF1 AND XhoI polymorphism OR XhoI variants. We also adopted another strategy to search the data to reduce possible selection bias, which was the recovery of all references of ‘pre-selected’ studies to retrieve articles of interest available only in other electronic databases. Finally, the selection criteria were as follows: 1) cohort or case–control studies that analyzed the 30-bp deletion and/or XhoI-loss present in the EBV LMP1 gene of patients with NPC; and 2) studies that showed the variables of interest as previously stated were selected regardless of the place of origin of the search, age, and sex as well as the histological type of NPC presented by these individuals. The exclusion criteria included the following: 1) review studies; 2) analysis only of other cancers ‘non-NPC’; 3) duplicated previous publications; and 4) studies that did not disclose the variables of interest as the frequency of the 30-bp deletion or the XhoI polymorphism in the EBV LMP1 gene separately for patients with NPC.
Data extraction and quality assessment
The researchers independently reviewed and extracted information from the eligible studies according to the inclusion and exclusion criteria previously highlighted. Thus, the following data were extracted: the identification and design of the study, the year of publication, the number of subjects and controls who had NPC, the types of controls (healthy or pathological), the study site, the age and sex of the research subjects, the frequency of the outcomes of interest as the 30-bp deletion or XhoI-loss from the EBV LMP1 gene. To assess the methodological quality of observational studies was used Newcastle-Ottawa Scale (NOS) in which a study was judged on three categories: selection (four items, one star each), comparability (one item, up to two stars), and exposure/outcome (three items, one star each). A ‘star’ presents a ‘high-quality’ choice of individual study. The full score was 10 stars, and the high-quality study was defined as a study with ≥6 awarded stars [31].
Statistical analysis
The dichotomous data of the case–control studies were extracted and plotted in a 2 × 2 table to give the individual and combined odds ratios (OR). For the cohort studies, which have binary data, the variables were extracted to calculate an estimate of the frequency of the outcomes of interest, and a confidence interval (CI) of 95% was used whenever possible. The I2 index was used to evaluate the existence of heterogeneity between the studies; for cases where there were significant differences in terms of heterogeneity (I2 = 75% to 100%, P < 0.05) [32], the random-effect model was used for the individual and combined analysis of the data. We conducted a sensitivity analysis to test the effect of the individual influence of each study on the overall estimate, and a subgroup analysis was also performed to reduce the existence of heterogeneity. Furthermore, we evaluated the existence of publication bias by Begg’s funnel plot [33] and by Egger’s test [34]. The funnel plot for the case–control studies was developed from the standard error of the log (OR) for each analysis against the log (OR), whereas the funnel plot of the cohort studies was plotted from the standard error log (percent) against the log (percent). For all of the procedures of the meta-analysis, STATA IC/64 version 13.1 software (Stata Corporation, College Station, Texas, USA) was used.
Results
Initially, during our search for articles in the electronic databases, 1,280 reference studies were found (see Additional file 2). Subsequently, due to the selection of the inclusion and exclusion criteria, there was a refinement to 75 reference studies (see Additional file 3). Finally, 31 eligible studies remained, which constituted our database for conducting the present meta-analysis (Table 1) [29,35-64]. A total of 2,846 subjects were included in these studies, among which 1,855 and 991 individuals were placed in NPC and control groups, respectively. Regarding the sex of the individuals, there was a male predominance with a male/female ratio of 2.73 [39-42,46,49,53,54,57]. The age of the participants ranged from 8 to 87 years; however, the predominant age was approximately 50 years old [35,40,41,43,46,49,53-55]. Most of the participants came from Asia (approximately 71%) [29,35,36,38-41,43,46,47,49-51,53,55,57-59,61-64], followed by Europe (26%) [29,36,37,48,54,56,62,63], North Africa (19%) [42,44,52,56,60,62], and America (13%) [45,54,62,63]. Similarly, the samples were from at least 12 countries, consisting mainly of China, Taiwan, Russia, Malaysia, Tunisia, Indonesia, Thailand, Serbia, and Morocco. With regard to case–control studies, all had an NOS score of 7. In the cohort studies, 5 (42%) were of high quality (NOS score ≥6), with an average NOS score of 5 (see Additional file 4). Thus, the risk of bias in relation to study quality evaluated by NOS was considered low with a score ranging from 4 to 7.
A meta-analysis to estimate the frequency of the 30-bp deletion and XhoI-loss (LMP1 EBV) in samples from NPC patients
The estimated frequencies of the EBV LMP1 variants in the samples from the NPC patients were determined and are shown in Figure 1. Thus, the estimated pooled frequency of 30-bp del-LMP1 was 77% (95% CI: 72 to 82, P = 0.00). For the control groups of the healthy controls and pathological samples, the estimated pooled frequency of 30-bp del-LMP1 was 46% (95% CI: 33 to 58, P = 0.00) and 39% (95% CI: 31 to 47, P = 0.49) (Additional file 5), respectively, that is, both of the control group frequencies were lower than those in the samples from the NPC patients.
For the XhoI-loss variable, the estimated pooled frequency was 82% (95% CI: 71 to 92, P = 0.00) in the NPC patients (see Figure 1). For the healthy and pathologic groups, the pooled rate was 62% (95% CI: 33 to 91, P = 0.002) and 76% (95% CI: 68 to 84, P = 0.3), respectively (Additional file 5).
The estimated pooled frequency was 79% (95% CI: 73 to 85, P = 0.00) for 30-bp del-LMP1 in the NPC patients found in Asia, which was the largest among the regions studied. The second highest frequency was observed in America, with a pooled frequency of 64% (95% CI: 35 to 93, P = 0.78). Finally, the third highest pooled frequency was 59% (95% CI: 45 to 73, P = 0.00), which was observed in Europe and North Africa. Similarly, the pooled frequency of XhoI-loss in individuals with NPC was higher for studies conducted in Asia (92%, 95% CI: 87 to 98, P = 0.00), followed by America (29%, 95% CI: 0 to 100) and by the regions from Europe and North Africa (9%, 95% CI: 0 to 44) (Additional file 6).
A meta-analysis of the association between the 30-bp del-LMP1 and XhoI-loss with NPC susceptibility
The OR, known as an association test, was calculated to assess the relationship between the LMP1 variants and NPC. Thus, there was a significant association between the 30-bp del-LMP1/XhoI-loss and NPC susceptibility (30-bp del-LMP1: OR = 2.86, 95% CI = 1.35 to 6.07, P = 0.00; XhoI-loss: OR = 8.5, 95% CI = 1.7 to 41, P = 0.00) (Figure 2). However, when we analyzed the association of the occurrence of the simultaneous outcome, that is, the co-existence of the 30-bp del-LMP1 and XhoI-loss with the susceptibility to NPC, there was not a significant association (OR = 1.09, 95% CI: 0.06 to 18.79, P = 0.002) (data not shown). However, there was significant heterogeneity, and due to this factor, the studies were analyzed in subgroups.
The histological subsets of the NPC and LMP1 EBV variants
According to the World Health Organization (WHO), NPC can be classified into three types according to the degree of histopathological differentiation, which include type I (keratinizing squamous cells carcinoma), type IIa (non-keratinizing, previously classified as type II), and type IIb (undifferentiated carcinoma, previously classified as type III) [65]. Therefore, when the selected studies reported this information, they were divided according to the histopathological classification to assess the association between the types of NPC and the EBV LMP1 variants. Thus, a significant association was found between the occurrence of 30-bp del-LMP1 with type III NPC (OR = 2.6, 95% CI: 1.12 to 6.03, P = 0.006) and also with type I/II NPC (OR = 2.65, 95% CI: 1.45 to 4.85, P = 0.7). Similarly, there was a significant association between type III NPC and XhoI-loss (OR = 65, 95% CI: 1.8 to 2,369, P = 0.1); likewise there was an association for types I/II NPC and XhoI-loss (OR = 13.67, 95% CI: 3.12 to 60, P = 0.3) (Additional file 7).
The association between the EBV LMP1 variants and the susceptibility to NPC by study region
A significant association between 30-bp del-LMP1 and the susceptibility to NPC was found in the studies conducted in Asia (OR = 3.47, 95% CI: 1.36 to 8.86, P = 0.00), while for the studies conducted in Europe and North Africa, there was no association (OR = 1.01, 95% CI: 0.3 to 3.4, P = 0.00) (Figure 3A). Similarly, there was a higher association between XhoI-loss and NPC susceptibility for studies conducted in Asia (OR = 12.35, 95% CI: 3.98 to 38, P = 0.27). For the studies conducted in Europe and North Africa, there was no association between XhoI-loss and NPC susceptibility because the pooled OR was 0.12 (95% CI: 0.01 to 1.17, P = 0.5) (Figure 3B).
Sensitivity analysis and publication bias
The studies that presented results considered discordant were temporarily removed to assess their individual influences on the pooled ORs. The individual removal did not significantly affect the pooled OR. However, due to the large variation of the ORs between 30-bp del-LMP1 and the susceptibility to NPC found in the studies of Li et al. [38] and Tan et al. [49], the ORs were removed, and the pooled OR was reduced by 31%, reaching 2.86 (95% CI: 1.35 to 6.07) to 1.96 (95% CI: 1.05 to 3.66, P = 0.001). Similarly for XhoI-loss, the See et al. [39] and Tan et al. [49] studies exhibited an OR very different from the other studies, and when both were removed, the pooled OR was reduced by 8.5 and equaled 3.69 (95% CI: 0.75 to 18, P = 0.005). However, removing these studies did not reduce the significant heterogeneity found. Therefore, the reduction of heterogeneity observed in the studies that analyzed 30-bp del-LMP1 occurred when the following studies were removed: Senyuta et al. [35], Gurtsevitch et al. [36], Banko et al. [37], Li et al. [38], and Hahn et al. [51]. In this case, the heterogeneity was reduced to 48% (P = 0.036) with an OR of 3.51 (95% CI: 2 to 6) (data not shown).
For the studies that analyzed XhoI-loss, only the study conducted by Khanim et al. [29] was found to cause heterogeneity, and when it was removed, the heterogeneity decreased to 19% (P = 0.28) with a pooled OR of 16.83 (95% CI: 6 to 43).
For the analysis of the publication bias, a funnel plot was used, and because it was symmetrical, it indicated that the existence of a selection bias was unlikely (Additional file 8). Additionally, by Egger’s test, there was also no sign of the occurrence of a selection bias for the studies included in the estimate of the OR and for the studies that analyzed the outcome of 30-bp del-LMP1 (coefficient −1.22, 95% CI: −4 to 1.64, P value 0.36) or XhoI-loss (coefficient −8.2, 95% CI: −248 to 231, P value 0.7) in the biopsies from the NPC patients. Additionally, regarding the calculation of the frequency, there was no sign of publication bias by the funnel plot and by Egger’s test (30-bp del-LMP1, coefficient −0.9, 95% CI: −2 to 0.2, P value 0.1; XhoI, coefficient 0.2, 95% CI: −2.8 to 3.2, P value 0.9).
Discussion
This meta-analysis provided evidence that both the 30-bp deletion and XhoI-loss (EBV LMP1 gene) were more frequently found in the samples from patients with NPC than in the control groups. In this case, 30-bp del-LMP1 was 1.5 times higher in the NPC patients than in the control group. While the outcome of XhoI-loss was only 1.15 times higher in the NPC patients than in the control group, the simultaneous occurrence of the outcomes of interest (the co-existence of the 30-bp del-LMP1 and XhoI-loss), unlike our previous data, showed no association (OR = 1.9, 95% CI: 0.06 to 18.79), although this result has been found by a few studies. This result shows that LMP1 variants occur with a considerable frequency in healthy subjects; therefore, there are many other non-viral factors involved in the etiopathogenesis of NPC. Thus, it is known that the development of NPC is multifactorial, involving the existence of a genetic predisposition of the individual, along with environmental factors [66]. However, one of the factors that has been most often correlated with the risk of NPC is the viral factor.
Because the etiology of NPC is complex, other meta-analyses have emerged to analyze the involvement of various factors in the susceptibility to NPC. In this sense, Xue et al. [67] conducted a meta-analysis of cohort and case–control studies to establish the relationship between smoking and the risk of NPC. This analysis showed that individuals who smoked always had a 60% greater probability of risk for NPC compared to that of individuals who have never smoked. Regarding genetic predisposition, studies have found an association between glutathione S-transferase M1 (GSTM1) and glutathione S-transferase T1 (GSTT1) with an increased risk for the development of NPC [67,68]. Also, the role of human leukocyte antigen (HLA) in the emergence of NPC has been examined, and some specific haplotypes and/or alleles from the HLA region have been associated with NPC [69-71]. For this reason, studies have found a high prevalence of HLA allele patterns found in endemic NPC regions, for example, HLA-A2 and HLA-Bw46 [72,73], which were associated with an increased risk for the development of NPC. These results have shown that many genes may contribute to an increased susceptibility to NPC, and some interesting studies show that there is a pattern of distribution of the HLA haplotypes and/or alleles that vary in different geographical areas characterized by differences in the prevalence of NPC [72-75].
LMP1 is considered an oncogenic product from EBV, and although its expression has been positively correlated with metastasis in NPC [76], its etiopathogenesis remains poorly understood. In this context, authors have postulated that variants of LMP1 exist with greater tumorigenic potential, such as the specific 30-bp deletion at the C-terminal region and the loss of the restriction site at the N-terminus (XhoI), which were our target outcomes of interest. Consequently, our meta-analysis has found that there was a positive association, but we postulated that at this moment, this outcome alone does not explain the risk of the emergence and development of NPC because these LMP1 variants were also found with a considerable frequency in the control groups. Similarly, these LMP1 variants were found in other cancers, such as Burkitt’s lymphoma [77], gastric carcinoma [78], and Hodgkin’s lymphoma [79,80], and also in the Japanese population [81]. With this background, the two LMP1 variants cannot be considered specific markers of NPC but could be considered the predominant variants in this type of cancer.
One factor that always draws attention in NPC is its remarkable geographical distribution because, while NPC is rare in most of the world, for the Southeast Asian region, especially in the South China region, this type of cancer is endemic. For example, the incidence of NPC in some provinces of Southern China is up to 30 times higher than in the rest of the world [82]. Thus, the question inevitably arises: what are the factors that explain the higher incidence of NPC in these endemic regions? Initially, the answer was related to an increased susceptibility of the people of these regions with the 30-bp del-LMP1 variant, as this is a variant commonly found in NPC biopsies. However, Zhang et al. [50] found similar levels of this LMP1 polymorphism among samples from endemic and non-endemic regions in South and North China, respectively. Therefore, the LMP1 variant failed to explain the high incidence of NPC in China, showing that there are other complex factors. Although these regions are composed of a very similar ethnic group, most likely, there are some genetic differences among this population. Accordingly, Wang et al. [83] found a higher frequency of HLA-A (*)30 in healthy individuals from the North China region, which has been associated with NPC resistance. Additionally, Ren et al. [84] found that the risk of developing NPC increases with a family history of the disease, meaning that individuals in South China who have a greater family history and incidence of NPC consequently have a greater susceptibility to NPC.
As previously mentioned, although EBV is associated with NPC, it most likely is not the only factor that would justify the high incidence of NPC in some parts of the world. A set of factors could contribute to the emergence of NPC, such as the type of diet, especially considering that multiple dietary factors, such as a high consumption of salted fish and eggs have been associated with the risk of NPC [85]. In addition, several authors have consistently found an associated risk between NPC and individuals who often feed on salt-preserved fish. These data were obtained from regions endemic for NPC, where this type of food is traditional for the people who live in these places [86,87].
This is the first meta-analysis that evaluated an association between the 30-bp deletion and XhoI-loss (EBV LMP1 gene) on the risk of NPC. Our results suggest an association between the outcomes of interest. However, we recognize that there were some limitations in our study. First, there was significant heterogeneity in the results; thus, a sensitivity analysis and subgroups showed that the types of controls and histologic types from NPC caused heterogeneity, but we did cannot determine if other variables such as the sample size or the origin of the studies caused the heterogeneity. Second, the loss of the original data from the reviewed studies limited our evaluation of other potential interactions, such as survival analysis and the stage of NPC associated with the LMP1 variants. Third, the number of studies included in the analysis was high, but the sample sizes included in the studies were modest. This factor may reduce the statistical power of the association between the outcome of interest and the risk of cancer. Fourth, articles in the Chinese language were not included; consequently, there is a possibility of a selection bias, even with the funnel plot and Egger’s test indicating no significant publication bias. Finally, our results of the ORs are based on unadjusted estimates, which may suffer from a confounding bias; therefore, a more precise analysis is required and must be conducted and adjusted for other factors jointly, such as cancer stage, age, sex, and genetic and environmental factors involved.
Conclusions
Our results suggest an association between the 30-bp del-LMP1 and XhoI-loss with NPC susceptibility. However, our data should be interpreted with caution because the sample size was small, and there was heterogeneity between the studies. For sensitivity analysis, individual removal did not significantly affect heterogeneity and the pooled ORs. In summary, further studies with a larger number of individuals will be required to measure the overall joint association of the various factors that might be involved in the triggering of NPC.
Abbreviations
- CTAR:
-
C-terminal activation regions
- EBV:
-
Epstein-Barr virus
- GSTM1:
-
Glutathione S-transferase M1
- GSTT1:
-
Glutathione S-transferase T1
- HLA:
-
Human leukocyte antigen
- LMP:
-
Latent membrane protein
- NOS:
-
Newcastle-Ottawa Scale
- NPC:
-
Nasopharyngeal carcinoma
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
References
Pathmanathan R, Prasad U, Sadler R, Flynn K, Raab-Traub N. Clonal proliferations of cells infected with Epstein-Barr virus in preinvasive lesions related to nasopharyngeal carcinoma. N Engl J Med. 1995;333:693–8.
Sham JS, Wei WI, Zong YS, Choy D, Guo YQ, Luo Y, et al. Detection of subclinical nasopharyngeal carcinoma by fibreoptic endoscopy and multiple biopsy. Lancet. 1990;335:371–4.
Fandi A, Altun M, Azli N, Armand JP, Cvitkovic E. Nasopharyngeal cancer: epidemiology, staging, and treatment. Semin Oncol. 1994;21:382–97.
Agulnik M, Epstein JB. Nasopharyngeal carcinoma: current management, future directions and dental implications. Oral Oncol. 2008;44:617–27.
Rickinson AB, Kieff E. Epstein-Barr virus. In: Knipe DM, Howley PM, editors. Field’s Virology. 4th ed. Philadelphia, Pa, USA: Lippincott Williams & Wilkins; 2001. p. 2575–627.
Leung SW, Lee TF. Treatment of nasopharyngeal carcinoma by tomotherapy: five-year experience. Radiation Oncol. 2013;8:107.
Wei WI, Sham JST. Nasopharyngeal carcinoma. Lancet. 2005;365:2041–54.
GLOBOCAN. Estimated cancer incidence, mortality and prevalence worldwide in 2012. http://globocan.iarc.fr/Pages/summary_table_pop_sel.aspx. Accessed 14 Jan 2015.
Young LS, Rickinson AB. Epstein-Barr virus: 40 years. Nat Rev Cancer. 2004;4:757–68.
Izumi KM. Identification of EBV transforming genes by recombinant EBV technology. Semin Cancer Biol. 2001;11:407–14.
Wang D, Liebowitz D, Kieff E. An EBV membrane protein expressed in immortalized lymphocytes transforms established rodent cells. Cell. 1985;43:831–40.
Kilger E, Kieser A, Baumann M, Hammerschmidt W. Epstein-Barr virus–mediated B-cell proliferation is dependent upon latent membrane protein 1, which simulates an activated CD40 receptor. EMBO J. 1998;17:1700–9.
Tsao SW, Tramoutanis G, Dawson CW, Lo AK, Huang DP. The significance of LMP1 expression in nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12:473–87.
Morris MA, Dawson CW, Young LS. Role of the Epstein–Barr virus-encoded latent membrane protein-1, LMP1, in the pathogenesis of nasopharyngeal carcinoma. Future Oncol. 2009;5:811–25.
Li HP, Chang YS. Epstein-Barr virus latent membrane protein 1: structure and functions. J Biomed Sci. 2003;10:490–504.
Dawson CW, Port RJ, Young LS. The role of the EBV-encoded latent membrane proteins LMP1 and LMP2 in the pathogenesis of nasopharyngeal carcinoma (NPC). Semin Cancer Biol. 2012;22:144–53.
Raab-Traub N. Epstein-Barr virus in the pathogenesis of NPC. Semin Cancer Biol. 2002;12:431–41.
Zheng H, Li LL, Hu DS, Deng XY, Cao Y. Role of Epstein-Barr virus encoded latent membrane protein 1 in the carcinogenesis of nasopharyngeal carcinoma. Cell Mol Immunol. 2007;4:185–96.
Wakisaka N, Pagano JS. Epstein-Barr virus induces invasion and metastasis factors. Anticancer Res. 2003;23:2133–8.
Shen ZH, Chen XY, Chen J. Impact of up-regulating Ezrin expression by Epstein-Barr virus latent membrane protein 1 on metastasis ability of nasopharyngeal carcinoma cells. Ai Zheng. 2008;27:165–9.
Yoshizaki T, Horikawa T, Qing-Chun R, Wakisaka N, Takeshita H, Sheen TS, et al. Induction of interleukin-8 by Epstein-Barr virus latent membrane protein-1 and its correlation to angiogenesis in nasopharyngeal carcinoma. Clin Cancer Res. 2001;7:1946–51.
Busson P, Braham K, Ganem G, Thomas F, Grausz D, Lipinski M, et al. Epstein-Barr virus-containing epithelial cells from nasopharyngeal carcinoma produce interleukin-1. Proc Natl Acad Sci U S A. 1987;84:6262–6.
Huang YT, Sheen TS, Chen CL, Lu J, Chang Y, Chen JY, et al. Profile of cytokine expression in nasopharyngeal carcinomas: a distinct expression of interleukin 1 in tumor and CD4+ T cells. Cancer Res. 1999;59:1599–605.
Coffin WF, Erickson KD, Hoedt-Miller M, Martin JM. The cytoplasmic amino-terminus of the latent membrane protein-1 of Epstein-Barr virus: relationship between transmembrane orientation and effector functions of the carboxy-terminus and transmembrane domain. Oncogene. 2001;20:5313–30.
Gires O, Zimber-Strobl U, Gonnella R, Ueffing M, Marschall G, Zeidler R, et al. Latent membrane protein 1 of Epstein-Barr virus mimics a constitutively active receptor molecule. EMBO J. 1997;16:6131–40.
Li SN, Chang YS, Liu ST. Effect of a 10-amino acid deletion on the oncogenic activity of latent membrane protein 1 of Epstein-Barr virus. Oncogene. 1996;12:2129–35.
Knecht H, Bachmann E, Brousset P, Sandvej K, Nadal D, Bachmann F, et al. Deletions within the LMP1 oncogene of Epstein-Barr virus are clustered in Hodgkin’s disease and identical to those observed in nasopharyngeal carcinoma. Blood. 1993;82:2937–42.
Chen ML, Tsai CN, Liang CL, Shu CH, Huang CR, Sulitzeanu D, et al. Cloning and characterization of the latent membrane protein (LMP) of a specific Epstein-Barr virus variant derived from the nasopharyngeal carcinoma in the Taiwanese population. Oncogene. 1992;7:2131–40.
Khanim F, Yao QY, Niedobitek G, Sihota S, Rickinson AB, Young LS. Analysis of Epstein-Barr virus gene polymorphisms in normal donors and virus-associated tumors from different geographical locations. Blood. 1996;88:3491–501.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6, e1000097.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et. al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Health Research Institute. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Senyuta N, Yakovleva L, Goncharova E, Scherback L, Diduk S, Smirnova K, et al. Epstein–Barr virus latent membrane protein 1 polymorphism in nasopharyngeal carcinoma and other oral cavity tumors in Russia. J Med Virol. 2014;86:290–300.
Gurtsevitch VE, Yakovleva LS, Shcherbak LN, Goncharova EV, Smirnova KV, Diduk SV, et al. Sequence variants of LMP1 oncogene in patients with oral cavity tumors associated and not associated with Epstein-Barr virus. Mol Biol. 2013;47:863–70.
Banko A, Lazarevic I, Cupic M, Stevanovic G, Boricic I, Jovanovic T. Carboxy-terminal sequence variation of LMP1 gene in Epstein–Barr-virus-associated mononucleosis and tumors from Serbian patients. J Med Virol. 2012;84:632–42.
Li DJ, Bei JX, Mai SJ, Xu JF, Chen LZ, Zhang RH, et al. The dominance of China 1 in the spectrum of Epstein-Barr virus strains from Cantonese patients with nasopharyngeal carcinoma. J Med Virol. 2009;81:1253–60.
See HS, Yap YY, Yip WK, Seow HF. Epstein-Barr virus latent membrane protein-1 (LMP-1) 30-bp deletion and Xho I-loss is associated with type III nasopharyngeal carcinoma in Malaysia. World J Surg Oncol. 2008;6:1–10.
Tang YL, Lu JH, Cao L, Wu MH, Peng SP, Zhou HD, et al. Genetic variations of EBV-LMP1 from nasopharyngeal carcinoma biopsies: potential loss of T cell epitopes. Braz J Med Biol Res. 2008;41:110–6.
Tiwawech D, Srivatanakul P, Karalak A, Ishida T. Association between EBNA2 and LMP1 subtypes of Epstein-Barr virus and nasopharyngeal carcinoma in Thais. J Clin Virol. 2008;42:1–6.
Ayadi W, Feki L, Khabir A, Boudawara T, Ghorbel A, Charfeddine I, et al. Polymorphism analysis of Epstein-Barr virus isolates of nasopharyngeal carcinoma biopsies from Tunisian patients. Virus Gene. 2007;34:137–45.
Chang KP, Hao SP, Lin SY, Ueng SH, Pai PC, Tseng CK, et al. The 30-bp deletion of Epstein-Barr virus latent membrane protein-1 gene has no effect in nasopharyngeal carcinoma. Laryngoscope. 2006;116:541–6.
Dardari R, Khyatti M, Cordeiro P, Odda M, ElGueddari B, Hassar M, et al. High frequency of latent membrane protein-1 30-bp deletion variant with specific single mutations in Epstein-Barr virus-associated nasopharyngeal carcinoma in Moroccan patients. Int J Cancer. 2006;118:1977–83.
Chabay P, De Matteo E, Merediz A, Preciado MV. High frequency of Epstein Barr virus latent membrane protein-1 30 bp deletion in a series of pediatric malignancies in Argentina. Arch Virol. 2004;149:1515–26.
Min Z, Young-sheng Z, Jie-hua HE, Su-xia L, Bi-ling Z, Ying-jie Y. Comparison of Epstein-Barr virus infection and 30 bp-deleted LMP1 gene among four histological types of nasopharyngeal carcinoma. Chin Med J. 2004;117:608–11.
Nurhantari Y, Emoto N, Rahayu P, Matsuo M. Nasopharyngeal carcinoma in Indonesia has a low prevalence of the 30-base pair deletion of Epstein-Barr virus latent membrane protein 1. Southeast Asian J Trop Med Public Health. 2003;34:98–105.
Plaza G, Santón A, Vidal AM, Bellas C. Latent membrane protein-1 oncogene deletions in nasopharyngeal carcinoma in Caucasian patients. Acta Otolaryngol. 2003;123:664–8.
Tan EL, Peh SC, Sam CK. Analyses of Epstein-Barr virus latent membrane protein-1 in malaysian nasopharyngeal carcinoma: high prevalence of 30-bp deletion, Xho1 polymorphism and evidence of dual infections. J Med Virol. 2003;69:251–7.
Zhang XS, Song KH, Mai HQ, Jia WH, Feng BJ, Xia JC, et al. The 30-bp deletion variant: a polymorphism of latent membrane protein 1 prevalent in endemic and non-endemic areas of nasopharyngeal carcinomas in China. Cancer let. 2002;176:65–73.
Hahn P, Novikova E, Scherback L, Janik C, Pavlish O, Arkhipov V, et al. The LMP1 gene isolated from Russian nasopharyngeal carcinoma has no 30-bp deletion. Int J Cancer. 2001;91:815–21.
Henry S, Sacaze C, Berrajah L, Karray H, Drira M, Hammami A, et al. In nasopharyngeal carcinoma-bearing patients, tumors and lymphocytes are infected by different Epstein-Barr virus strains. Int J Cancer. 2001;91:698–704.
T-t K, Tsang NM. Salivary gland type nasopharyngeal carcinoma: a histologic, immunohistochemical, and Epstein-Barr virus study of 15 cases including a psammomatous mucoepidermoid carcinoma. Am J Surg Pathol. 2001;25:80–6.
D’Addario M, Chauvin P. Ethnic differences in the expression of Epstein-Barr virus latent membrane protein-1 mutations in nasopharyngeal carcinoma. Mutat Res. 2000;457:69–78.
Cheung ST, Leung SF, Lo KW, Chiu KW, Tam JSL, Fok TF, et al. Specific latent membrane protein 1 gene sequences in type 1 and type 2 Epstein-Barr virus from nasopharyngeal carcinoma in Hong Kong. Int J Cancer. 1998;76:399–406.
Grunewald V, Bonnet M, Boutin S, Yip T, Louzir H, Levrero M, et al. Amino-acid change in the Epstein-Barr virus zebra protein in undifferentiated nasopharyngeal carcinomas from Europe and North Africa. Int J Cancer. 1998;75:497–503.
Sung NS, Edwards RH, Seillier-Moiseiwitsch F, Perkins AG, Zeng Y, Raab-Traub N. Epstein-Barr virus strain variation in nasopharyngeal carcinoma from the endemic and non-endemic regions of China. Int J Cancer. 1998;76:207–15.
Cheung ST, Lo KW, Leung SF, Chan WY, Choi PH, Johnson PJ, et al. Prevalence of LMPl deletion variant of Epstein-Barr Virus in nasopharyngeal carcinoma and gastric tumors in Hong Kong. Int J Cancer. 1996;66:711–2.
Chang YS, Su IJ, Chung PJ, Shu CH, Ng CK, Wu SJ, et al. Detection of an Epstein-Barr virus variant in T-cell-lymphoma tissues identical to the distinct strain observed in nasopharyngeal carcinoma in the Taiwanese population. Int J Cancer. 1995;62:673–7.
Bouzid M, Djennaoui D, Dubreuil J, Bouguermouh A, Ellouz D, Abdelwahab J, et al. Epstein-Barr virus genotypes in NPC biopsies from North Africa. Int J Cancer. 1994;56:468–73.
Jeng KCG, Hsu CY, Liu MT, Chung TT, Liu ST. Prevalence of Taiwan variant of Epstein-Barr virus in throat washings from patients with head and neck tumors in Taiwan. J Clin Microbiol. 1994;32:28–31.
Miller WE, Edwards RH, Walling DM, Raab-Traub N. Sequence variation in the Epstein-Barr virus latent membrane protein 1. J General Virol. 1994;75:2729–40.
Abdel-Hamid M, Chen JJ, Constantine N, Massoud M, Raab-Traub N. EBV strain variation: geographical distribution and relation to disease state. Virology. 1992;190:168–75.
Hu LF, Zabarovsky ER, Chen F, Cao SL, Ernberg I, Klein G, et al. Isolation and sequencing of the Epstein-Barr virus BNLF-1 gene (LMP1) from a Chinese nasopharyngeal carcinoma. J General Virol. 1991;72:2399–409.
Shanmugaratnam K, Path FRC, Sobin LH. The World Health Organization histological classification of tumours of the upper respiratory tract and ear. A commentary on the second edition. Cancer. 1993;71:2689–97.
Laantri N, Corbex M, Dardari R, Benider A, Gueddari BE, Khyatti M. Environmental, genetic and viral risk factors of nasopharyngeal carcinoma in North Africa. BMC Proceeding. 2011;5 Suppl 1:30.
Xue WQ, Qin HD, Ruan HL, Shugart YY, Jia WH. Quantitative association of tobacco smoking with the risk of nasopharyngeal carcinoma: a comprehensive meta-analysis of studies conducted between 1979 and 2011. Am J Epidemiol. 2013;178:325–38.
Murthy AK, Kumar V, Suresh KP. Meta-analysis of GSTM1 and GSTT1 polymorphisms and risk of nasopharyngeal cancer. Asian Pacific J Cancer Prev. 2013;14:1697–701.
Chin YM, Mushiroda T, Takahashi A, Kubo M, Krishnan G, Yap LF, et al. HLA-A SNPs and amino acid variants are associated with nasopharyngeal carcinoma in Malaysian Chinese. Int J Cancer. 2014. doi:10.1002/ijc.29035.
Li X, Ghandri N, Piancatelli D, Adams S, Chen D, Robbins FM, et al. Association between HLA Class I alleles and the prevalence of nasopharyngeal carcinoma (NPC) among Tunisians. J Transl Med. 2007;5:22.
Burt RD, Vaughan TL, McKnight B, Davis S, Beckmann AM, Smith AG, et al. Associations between human leukocyte type and nasopharyngeal carcinoma in Caucasian in the Unites States. Cancer Epidemiol Biomarkers Prev. 1996;5:879–87.
Li X, Fasano R, Wang E, Yao KT, Marincola FM. HLA associations with nasopharyngeal carcinoma. Curr Mol Med. 2009;9:751–65.
Tang M, Zeng Y, Poisson A, Marti D, Guan L, Zheng Y, et al. Haplotype-dependent HLA susceptibility to nasopharyngeal carcinoma in a Southern Chinese population. Genes Immun. 2010;11:334–42.
Feng BJ, Huang W, Shugart YY, Lee MK, Zhang F, Xia JC, et al. Genome-wide scan for familial nasopharyngeal reveals evidence of linkage to chromosome 4. Nat Genet. 2002;31:395–9.
Simons MJ, Wee GB, Chan SH, Shanmugaratnam K, Day NE, De-Thé G. Immunogenetic aspects of nasopharyngeal carcinoma (NPC) III. HL-a type as a genetic marker of NPC predisposition to test the hypothesis that Epstein-Barr virus is an etiological factor in NPC. IARC Sci Publ. 1975;11:249–58.
Zhao Y, Wang Y, Zeng S, Hu X. LMP1 expression is positively associated with metastasis of nasopharyngeal carcinoma: evidence from a meta-analysis. J Clin Pathol. 2012;65:41–5.
Chen WG, Chen YY, Bacchi MM, Bachi CE, Alvarenga M, Weiss LM. Genotyping of Epstein-Barr virus in Brazilian Burkitt’s lymphoma and reactive lymphoid tissue: type A with high prevalence of deletion within the latent membrane protein gene. Am J Pathol. 1996;148:17–23.
Mori S, Itoh T, Tokunaga M, Eizuru Y. Deletions and single-base mutations within the carboxy-terminal region of the latent membrane protein 1 oncogene in Epstein-Barr virus-related gastric cancers of southern Japan. J Med Virol. 1999;57:152–8.
Dirnhofer S, Angeles-Angeles A, Ortiz-Hidalgo C, Reyes E, Gredler E, Krugmann J, et al. High prevalence of a 30-base pair deletion in the Epstein-Barr virus (EBV) latent membrane protein 1 gene and of strain type B EBV in Mexican classical Hodgkin’s disease and reactive lymphoid tissue. Hum Pathol. 1999;30:781–7.
Essop MF, Engel M, Close P, Sinclair-Smith C, Pallesen G. Epstein-barr virus in Hodgkin’s disease: frequency of a 30-bp deletion in the latent membrane protein (LMP-1) oncogene in South African patients. Int J Cancer. 1999;20:449–51.
Itakura O, Yamada S, Narita M, Kikuta H. High prevalence of a 30-base pair deletion and single-base mutations within the carboxy terminal end of the LMP-1 oncogene of Epstein-Barr virus in the Japanese population. Oncogene. 1996;13:1549–53.
Jia WH, Huang QH, Liao J, Ye W, Shugart YY, Liu Q, et al. Trends in incidence and mortality of nasopharyngeal carcinoma over a 20–25 year period (1978/1983–2002) in Sihui and Cangwu counties in southern China. BMC Cancer. 2006;6:178.
Wang R, Hu Y, Yindom LM, Huang L, Wu R, Wang D, et al. Association analysis between HLA-A, −B, −C, −DRB1, and –DQB1 with nasopharyngeal carcinoma among a Han population in Northwestern China. Hum Immunol. 2014;75:197–202.
Ren ZF, Liu WS, Qin HD, Xu YF, Yu DD, Feng QS, et al. Effect of family history of cancers and environmental factors on risk of nasopharyngeal carcinoma in Guangdong China. Cancer Epidemiol. 2010;34:419–24.
Armstrong RW, Imrey PB, Lye MS, Armstrong MJ, Yu M, Sani S. Nasopharyngeal carcinoma in Malaysian Chinese: salted fish and other dietary exposures. Int J Cancer. 1998;77:228–35.
Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2006;15:1765–77.
Yuan JM, Wang XL, Xiang YB, Gao YT, Ross RK, Yu MC. Preserved foods in relation to risk of nasopharyngeal carcinoma in Shanghai. China Int J Cancer. 2000;85:358–63.
Acknowledgements
This study was supported by Fundação de Amparo à Pesquisa do Estado de Goiás (FAPEG; N° 10/13-Apoio Programas de Pós-Graduação Stricto Sensu). The funders had no role in the study; the collection, analysis, and interpretation of data; or assembly and decision to submit this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
VGC, ACMS and MLM conceived and designed the experiments. VGC, ACMS, and MLM performed the experiments and analyzed the data. VGC contributed with analysis tools. VGC wrote the paper. All authors read and approved the final manuscript.
Additional files
Additional file 1:
PRISMA Checklist. PRISMA 2009 checklist showing guidelines for systematic reviews and meta-analysis.
Additional file 2:
PRISMA flow diagram. PRISMA 2009 flow diagram of the cohort and case–control studies included in the meta-analysis.
Additional file 3:
List of the pre-selected studies. List of the pre-selected studies that were excluded due to the appropriate justifications.
Additional file 4:
Methodologic quality of cohort and case–control studies. Methodologic quality of cohort and case–control studies included in the meta-analysis.
Additional file 5:
Forest plot of the frequency of the 30-bp del-LMP1 and XhoI-loss. Forest plot of the frequency of the 30-bp del-LMP1 and XhoI-loss in the control groups.
Additional file 6:
Forest plot of the frequency of the 30-bp del-LMP1 and XhoI-loss. Forest plot of the frequency of the 30-bp del-LMP1 (left) and XhoI-loss (right) in relation to the origin from the studies.
Additional file 7:
Forest plot of the OR regarding the histological type of NPC. Forest plot of the OR regarding the histological type of NPC associated with the 30-bp del-LMP1 (left) and XhoI-loss (right).
Additional file 8:
Funnel plot for publication bias. Funnel plot for publication bias of the 30-bp del-LMP1 and Xho-loss.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
da Costa, V.G., Marques-Silva, A.C. & Moreli, M.L. The Epstein-Barr virus latent membrane protein-1 (LMP1) 30-bp deletion and XhoI-polymorphism in nasopharyngeal carcinoma: a meta-analysis of observational studies. Syst Rev 4, 46 (2015). https://doi.org/10.1186/s13643-015-0037-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-015-0037-z