Abstract
Background
In Ireland, meat by-products (MBP) harvested at knackeries from farmed animals that have not died of an infectious or systemic disease are legally permitted to be fed to dogs in kennels and packs of hounds. There is limited information available on the risks of spreading foodborne bacteria or antimicrobial resistant (AMR) determinants to dogs, their handlers or the associated environment. The aim of this study was to investigate the distribution of Salmonella serovars, Listeria monocytogenes, Campylobacter species, enterococci, their associated AMR determinants and the level of Escherichia coli in samples of MBP from knackeries and associated equipment and kennels. For this purpose, 313 fresh and 208 frozen MBP samples from 22 knackeries, 16 swabs of mincing equipment from two of the knackeries and 138 swabs from kennels adjacent to seven of the knackeries were collected and processed over a 12-month period.
Results
From the 521 MBP samples analysed, a total of 77 Salmonella (14.8%), 101 L. monocytogenes (19.4%), 12 Campylobacter (2.3%), 271 Enterococcus faecalis (52.0%) and 127 Enterococcus faecium (24.4%) strains were recovered. The 154 analysed environmental samples from kennels and mincing equipment yielded 194 isolates (3 Salmonella, 85 E. coli, 76 E. faecalis and 30 E. faecium.). E. coli was quantifiable in 423 of the 521 MBP samples with log counts per gram ranging between 1 and 6. AMR characterisation of 168 E. coli, enterococci and Salmonella isolates from MBP and environmental samples showed high levels of AMR including multi-drug resistance (MDR) with 63.6%, 9.1%, 29% and 45.8% of E. coli, Salmonella, E. faecalis and E. faecium isolates, respectively showing resistance to three or more antimicrobials (MDR)
Conclusions
The findings of this survey confirm that MBP from fallen animals contain high levels of zoonotic and AMR-harbouring bacteria that pose a risk of transmission to dogs, their handlers, and the environment.
Similar content being viewed by others
Introduction
In Ireland, when an animal dies on a farm as a result of injury or a non-notifiable disease, the carcass must be transported to a rendering plant or to a knackery for processing and disposal. Meat by-products (MBP) harvested at knackeries from farmed animals that have not died of an infectious or systemic disease are legally permitted to be fed to dogs in kennels and packs of hounds. During 2020 there were 228,257 recorded on-farm cattle deaths (excluding stillborn) in Ireland [1].
To prevent risks to public and animal health and to ensure that fallen animals do not enter the food chain, knackeries must adhere to strict rules regarding the collection, transport, storage, use, processing and disposal of MBP. Regulation (EC) No. 1069/2009 [2] permits the feeding of dogs from listed kennels and packs of hounds and dogs in shelters with MBP harvested at approved knackeries from low risk fallen farmed animals. While greyhounds and hunting dogs are currently classified as farm animals under Irish law [3], dogs in general are recognised as carriers of zoonotic bacteria, showing no clinical signs of disease in many cases [4, 5], but there are also some descriptions of fatal salmonellosis and campylobacteriosis in dogs as a consequence of contaminated pet foods [6, 7].
In recent years, raw pet food diets have become popular for dogs and are considered both nutritious and healthy [6, 8]. While the benefits of feeding dogs with a raw meat diet have been previously claimed [6, 8], other studies have outlined potential risks with these diets, i.e., bacterial infections, parasitic disease and nutrient imbalance [9,10,11,12]. Foodborne zoonotic bacteria such as Salmonella, Listeria monocytogenes and Campylobacter have all been identified in raw pet foods [13,14,15] and disease associated with feeding Salmonella-contaminated raw feeds to greyhounds has been previously reported [16].
Data relating to bacterial contamination of MBP used as feed for kennel dogs is scarce, particularly in relation to Ireland and there is currently a lack of information available on the risks of spreading foodborne bacteria or AMR determinants to dogs, their handlers or the environment which may be associated with the practice of feeding MBP from fallen animals to dogs. Therefore, the aim of this survey was to investigate the presence of food-borne and antimicrobial resistance-harbouring bacteria in MBP, mincing equipment and kennels where MBP are fed to dogs to assess the risks associated with this practice in Ireland.
Materials and Methods
Knackery selection and sampling
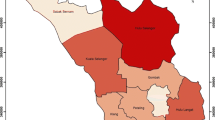
For this survey, we selected 22 of the 37 registered knackeries in the Republic of Ireland based on 1) nationwide distribution, 2) approval for harvesting MBP and 3) willingness to take part in the survey. From each premises, fresh and frozen (if available) bovine MBP 500 g samples were collected using sterile kits at regular intervals from January to December 2016 by a Department of Agriculture, Food and the Marine (DAFM) official veterinarian. A total of 313 fresh and 208 frozen MBP samples were obtained. Information on herd type, age, recent drug treatment or the health status of dogs was not available.
Mincing equipment for processing MBP was on site in two of the knackeries and, for those premises, swabs were obtained by swabbing the entire inside surface and head of the mincer using a sterile sponge (Helapet, Bedfordshire, UK). A total of 16 mincing equipment swabs were collected.
Kennels adjacent to seven knackeries were swabbed at quarterly intervals over the 12-month period. Kennels varied in size (from 10 to 100 dogs) and breed types (mainly foxhounds and greyhounds although one had numerous breeds). Six locations had kennels made from concrete (walls and floors) and kennel sizes varied from 8 x 8 ft to 12 x 14 ft. The smallest had 2-4 random breeds per kennel and the largest was a hunt kennel which housed approximately 30-40 hounds per kennel. The seventh location had random small kennels scattered around the knackery/farm and these kennels had concrete floors with wired fencing. For the majority of visits the dogs were not in the kennels when sampling took place and kennels appeared to have been hosed down prior to sampling. On occasions where cleaning had not been conducted, bedding with faeces was also collected. Five different areas within each kennel were randomly sampled, taking precautions to avoid cross contamination.
Using disposable gloves, a sterile pre-moistened sponge (Helapet, Bedfordshire, UK) was used to sample each of the five areas by dragging across a 0.24 m2 area and then returning the sponge to its sterile bag. Faecal samples, n=21, were also collected. In total 138 kennel swabs including faecal samples were collected. All samples were placed in a cool box containing ice blocks and transported to the laboratory within 6 h. Once received at the laboratory, fresh samples and environmental samples were tested within 24 h while frozen MBP samples were stored at -20°C pending testing.
Sample preparation and microbiological examination
MBP samples were processed for the detection of Salmonella, L. monocytogenes, Campylobacter (in 25 g), Enterococcus and E. coli (in 1g) and for the enumeration of E. coli. Environmental samples (i.e., equipment and kennel samples and faecal samples) were examined for the presence of Salmonella, Enterococcus and E. coli.
Detection of Salmonella was based on ISO 6579-1:2017 [17]. For each bacterial species, one suspect colony per plate was selected for confirmation. Detection of L. monocytogenes was based on ISO 11290-1:1996 [18]. Detection of thermotolerant Campylobacter spp. was based on ISO 10272-1:2006 [19] with modifications to include Bolton broth as the initial enrichment medium. Enumeration of E. coli was performed according to ISO 16649-2:2001 [20]. Detection of Enterococcus was based on Wegener et al. (1997) [21] and Ahmad et al. (2002) [22] modified to include the addition of one gram of MBP to 9 ml of Brain Heart Infusion broth (BHI; Sigma, Missouri, United States) supplemented with 6% Sodium Chloride and subsequent subculture on Slanetz-Bartley agar (E&O, Bonnybridge, Scotland). Detection of E. coli was carried out according to Tanih et al. (2015) [23] with some minor modifications.
All isolates were identified using MALDI-ToF (Matrix Assisted Laser Desorption Ionization-Time of Flight) Mass Spectrometry (Bruker Daltronics GmbH, Bremen, Germany) as described by Ramovic et al. (2020) [24]. MALDI-ToF also permitted speciation of enterococci and Campylobacter. Salmonella isolates were typed according to the Kauffman-White-Le Minor scheme, using somatic (O) and flagellar (H) antigens (Sifin Diagnostics, Berlin, Germany) as described by Prendergast et al. (2012) [25] and if necessary using Polymerase Chain Reaction (PCR) for identification of Monophasic S. Typhimurium according to Prendergast et al. 2013 [26].
Antimicrobial Susceptibility Testing
The antibiotic susceptibility profiles of the isolates were determined using the mandatory harmonised method that is outlined in the EU Commission Implementing Decision 2013/652/EU [27]. The epidemiological cut-off values and the concentration ranges that are set out in Tables 1, 2 and 3 of the decision were used.
A total of 168 isolates were selected for antimicrobial susceptibility, including 37 E. coli and 30 Salmonella from MBP, 40 E. coli (2 mincer, 31 kennels, 7 faeces), 3 Salmonella (mincer), 34 E. faecalis and 24 E. faecium (9 mincer, 39 kennels and 10 faeces) from environmental samples. Selection aimed to generate maximum information within the constraints of economic and time limitations.
Antimicrobial susceptibility testing was carried out as described by Ramovic et al. (2020) [24]. Minimum Inhibitory Concentration (MIC) for relevant antimicrobials was determined in broth microdilution antimicrobial susceptibility assays using different commercially available Sensititre plates (Thermo Fisher Scientific, Massachusetts, United States). E. coli and Salmonella isolates were tested initially using the EUVSEC plate and strains which exhibited resistance to cefotaxime, ceftazidime and/or meropenem were considered suspect extended spectrum beta-lactamase (ESBL) producers and further tested with the EUVSEC2 plate. Enterococcus strains were tested using the EUVENC plates. Suitable controls strains, E. coli 25922 and E. faecalis 29212, were tested with each batch of samples and the classification of the phenotypic results was based on EU Commission Decision 2013/652/EU [27] and the most recent EFSA recommendations as described by Ramovic et al. (2020) [24].
Isolates were deemed MDR when resistance was found to three or more antimicrobials.
Results
MBP Samples
A total of 190 strains of potentially zoonotic bacteria were isolated from MBP as shown in Table 1. L. monocytogenes was the most frequently isolated bacterium of the three classical foodborne pathogens, both in fresh and frozen samples.
Among the 77 Salmonella isolates, a total of 7 serovars were identified. S. Dublin was the most frequently isolated (n=39) followed by S. Typhimurium (n=8), S. Montevideo (n=8), Monophasic S. Typhimurium (n=5), S. Braenderup (n=4), S. Anatum (n=2) and S. Agama
(n=1). Ten Salmonella isolates’ antigenic formula could not be fully ascertained by serotyping and were therefore designated as S. Unnamed.
Campylobacter in MBP was isolated in 10 fresh and 2 frozen samples. MALDI-ToF identified the isolates as C. fetus subsp. intestinalis (n= 6), C. coli (n=4) and C. jejuni (n=2). C. fetus subsp. intestinalis was found in fresh samples only.
The recovery rate of E. faecalis from MBP was greater than that of E. faecium for both fresh and frozen samples (Table 1). E. coli was recovered from 423 of 521 (81%) of MBP samples at varied levels in fresh and frozen samples as shown in Fig. 1. The number of E. coli recovered from fresh MBP was generally numerically greater than from frozen MBP.
Environmental samples
A total of 3 Salmonella, 85 E. coli, 76 E. faecalis and 30 E. faecium isolates were recovered from environmental samples as shown in Table 2. E. coli was isolated from 77 out of 138 kennel samples and 8 out of 16 mincing equipment samples (55.8% and 50% respectively). S. Braenderup, S. Dublin and S. Typhimurium, one of each, were isolated from mincing equipment (3 out of 16, i.e., 18.8%) but not from kennels, while Enterococcus were recovered from kennel samples (67 E. faecalis and 28 E. faecium out of 138 samples or 48.6% and 20.3% respectively), and mincing equipment (9 E. faecalis and 2 E. faecium out of 16 samples or 56.3% and 12.5% respectively).
Antimicrobial Resistance
Broth microdilution AMR susceptibility testing results from the MBP and environmental isolates are shown in Tables 3, 4 and 5. Overall, isolates ranged from fully susceptible to resistant to 10 antimicrobials with a large proportion of isolates resistant to more than three antimicrobials. AMR testing on E. coli isolates recovered from MBP showed a high level of resistance to tetracycline, sulfamethoxazole, trimethoprim, ampicillin, chloramphenicol, ciprofloxacin and nalidixic acid in both MBP and environmental samples with 76% of MBP and 58% of Environmental isolates resistant to tetracycline and sulfamethoxazole. Based on the results obtained in the EUVSEC2 plate, two isolates were identified as presumptive plasmid mediated AmpC (pAmpC) and one as presumptive ESBL producing E. coli (Table 3). The two presumptive pAmpC producing E. coli were resistant to seven and nine antimicrobials and the presumptive ESBL positive isolate recovered from the environmental kennel swab was resistant to nine antimicrobials.
The monophasic S. Typhimurium isolated from frozen MBP was resistant to both ampicillin and tetracycline (Table 4). Amongst the six S. Typhimurium isolates, three were fully susceptible and three were resistant to three antimicrobials. The majority of the S. Dublin isolates were fully susceptible, and one S. Dublin isolate from a frozen MBP sample was resistant to both ciprofloxacin and nalidixic acid.
Among the 34 E. faecalis and the 24 E. faecium isolates examined for AMR, tetracycline resistance was the most common (79.4% of E. faecalis and 70.8% of E. faecium) followed by chloramphenicol and erythromycin in E. faecalis and quinupristin/dalfopristin, daptomycin, chloramphenicol and ciprofloxacin in E. faecium (Table 5).
Discussion
In Ireland it is common practice to feed MBP from knackeries to greyhounds and foxhounds as allowed under SI 252/2008 [28], and this MBP is most often fed raw. The controls governing the feeding of MBP recovered at knackeries from fallen animals to associated kennels as per EU Regulation (EC) 142/2011 [29] are much less stringent than those governing meat destined for human consumption and there are no previous studies evaluating the risks associated with such products in Ireland.
The results of our study indicate that MBP from fallen animals contain potential pathogens including Salmonella and Campylobacter. As Salmonella may be carried in the gastrointestinal tract of ruminants it was not surprising that 14.8% of MBP samples were contaminated with this pathogen. The lower recovery rate of Salmonella in frozen samples when compared to fresh may be explained by lower viability after freezing as has been observed by other authors [30].
Reported prevalence of Salmonella in bones and raw pet foods in previous studies varied greatly, from 0.2% [31], 5.9% [32], 12% [33], 20% [10], to 80% [34].
Although 14.8% of MBP contained Salmonella, Salmonella spp. was not isolated from kennels. This finding differed from published data but could be explained by the type of MBP and the limited number of kennels sampled. S. Dublin which was the most prevalent serovar from MBP is host adapted to cattle and may not persist in the gastrointestinal tract of dogs to the same extent as other serotypes; S. Dublin accounted for only 9% of Salmonella isolated from dogs in the UK from 1954 – 2012 [35].
L. monocytogenes is a ubiquitous organism commonly found on dairy and beef farms. A study conducted by Fox et al. (2009) [36] investigated the prevalence of L. monocytogenes on 16 Irish farms. Of 298 environmental samples collected, 19% of samples were positive for L. monocytogenes indicating its widespread distribution in cattle farms. Overall, this organism was the most frequently isolated pathogen in fresh (18.8%) and frozen (20.2%) samples. A clear link between cleanliness and contamination with L. monocytogenes has been established [36, 37]. As knackeries do not undertake the hygiene practices found in establishments producing meat for human consumption it is therefore not unexpected to find these contamination levels. Even higher isolation rates have been described, with 54% L. monocytogenes isolation rate in frozen raw pet food reported by Van Bree et al. (2018) [10].
A low prevalence of Campylobacter was found in this study, in agreement with published literature [38,39,40], although Bojanić et al. (2017) [41] reported a high prevalence of Campylobacter in raw dog food. C. fetus subsp intestinalis which was predominantly recovered from fresh samples, naturally resides in the gastrointestinal tract of cattle and has seldom been linked to human disease [42], while C. coli and C. jejuni are recognised pathogens of humans and are common commensals of cattle, sheep, pigs, and other species of domestic and wild animals [43]. Although the occurrence of Campylobacter in MBP in this study was low, there is still a risk of transmission to dogs [8, 44] and dogs have been reported to shed this organism after consumption of raw meat [15].
Sterilisation, heat processing or freezing prior to feeding has been reported to reduce the bacterial load [45]. In this study, fewer Salmonella, Campylobacter and E. coli were found in frozen MBP than in fresh MBP, although freezing had little impact on levels of L. monocytogenes and enterococci. Samples analysed for E. coli and enterococci showed high rates of contamination, reflecting the low standard of hygiene practices in knackeries. The level of E. coli was 4 log or greater in approximately 35% of MBP samples, thus exceeding the absolute threshold of 5,000 CFU/g stipulated in Commission Regulation (EU) No 142/2011 for raw pet food at the point of production [29]. Although this regulation does not apply to the feeding of dogs with MBP supplied directly from knackeries on site, our findings demonstrate the high level of microbial contamination in MBP.
Apart from the risks posed by the presence of zoonotic organisms in MBP, contamination with antimicrobial resistant bacteria also constitutes a potential risk for human and animal health. In recent years the role of companion animals in transmission of AMR has been investigated by several authors including Damborg et al. (2016) [5] who identified dogs as a source of infection of antimicrobial resistant bacteria. High levels of AMR to ampicillin, ciprofloxacin, chloramphenicol and tetracycline were found in both E. coli and enterococci isolates from kennels. In addition, resistance to nalidixic acid, trimethoprim and sulphamethoxazole was high in E. coli and resistance to daptomycin and quinupristin/dalfopristin in E. faecium. The patterns of AMR were similar among E. coli isolates recovered from both environmental and MBP samples. The high level of resistance to tetracyclines, sulphonamides, trimethoprim and ampicillin seen in MBP and environmental isolates of E. coli is likely the result of selective pressure as a result of antimicrobial treatment of fallen stock and/or more frequent use of these antimicrobials within veterinary medicine, resulting in E. coli strains colonising the bovine gastrointestinal tract and subsequent transmission of these resistant organisms to dogs after feeding MBP [46].
Three ESBL producing E. coli ss detected in this study. ESBL producing E. coli have been isolated from numerous different animal sources, including dogs. A study performed by Baede et al. (2015) [47], suggested a correlation between feeding dogs a raw diet that contains ESBL-producers and the presence of these E. coli in dogs. In this work, one ESBL isolate was identified in a kennel environmental sample.
Additional labelling on MBP samples to declare the presence of harmful bacteria and recommendations on handling MBP is advisable to make kennel operators more aware of the potential risks of MBP. The possible development of a standard operating procedure for harmonisation of sanitation practices across all knackeries should be considered. Comprehensive cleaning procedures to include all equipment and all surfaces before and after processing should be implemented. In addition, measures such as effective hand washing, general hygiene and personal protective equipment should be included in protocols as effective prevention measures against zoonotic infections.
Conclusion
This is the first study to document the risks associated with feeding MBP from fallen animals to dogs. The findings indicate that MBP may be a vehicle for transmission of zoonotic pathogens and antimicrobial resistant determinants to dogs, their owners and the environment. Our findings may serve as the focus for future research to understand the risks to human and animal health associated with feeding this type of product to dogs.
As MBP is a rich nutrient matrix which supports the growth of bacteria including pathogens, reducing to zero the microbial load and all risks for product handlers, dogs and their owners is not achievable and enhanced control measures should be considered instead.
References
Department of Agriculture, Food and the Marine. AIM Bovine Statistics Report 2020. In: https://www.gov.ie/en/publication/d5dc1-aim-bovine-statistics-reports/#. Accessed 23 Mar 2022.
Regulation (EC) No. 1069/2009 of the European parliament and of the council of 21 October 2009 laying down health rules as regards animal by-products and derived products not intended for human consumption and repealing Regulation (EC) No. 1774/2002 (Animal by-products Regulation). L300/1 14.11.2009. 2009. L300/1 – L300/33.
Animal Health and Welfare Act. 2013. https://www.irishstatutebook.ie/eli/2013/act/15/enacted/en/pdf. Accessed 24 Mar 2022.
Marks SL, Rankin SC, Byrne BA, Weese JS. Enteropathogenic bacteria in dogs and cats: diagnosis, epidemiology, treatment, and control. J Vet Intern Med. 2011. https://doi.org/10.1111/j.1939-1676.2011.00821.x.
Damborg P, Broens EM, Chomel BB, Guenther S, Pasmans F, Wagenaar JA, et al. Bacterial Zoonoses Transmitted by Household Pets: State-of-the-Art and Future Perspectives for Targeted Research and Policy Actions. J Comp Pathol. 2016. https://doi.org/10.1016/j.jcpa.2015.03.004.
Schlesinger DP, Joffe DJ. Raw food diets in companion animals: a critical review. Can Vet J. 2011;52:50–4.
Laflamme DP, Abood SK, Fascetti AJ, Fleeman LM, Freeman LM, Michel KE, et al. Pet feeding practices of dog and cat owners in the United States and Australia. J Am Vet Med Assoc. 2008. https://doi.org/10.2460/javma.232.5.687.
Davies RH, Lawes JR, Wales AD. Raw diets for dogs and cats: a review, with particular reference to microbiological hazards. J Small Anim Pract. 2019;60:329–39.
Morgan SK, Willis S, Shepherd ML. Survey of owner motivations and veterinary input of owners feeding diets containing raw animal products. PeerJ. 2017. https://doi.org/10.7717/peerj.3031.
van Bree FPJ, Bokken GCAM, Mineur R, Franssen F, Opsteegh M, van der Giessen JWB, et al. Zoonotic bacteria and parasites found in raw meat-based diets for cats and dogs. Vet Rec. 2018. https://doi.org/10.1136/vr.104535.
Finley R, Ribble C, Aramini J, Vandermeer M, Popa M, Litman M, et al. The risk of salmonellae shedding by dogs fed Salmonella-contaminated commercial raw food diets. Can Vet J. 2007;48:69–75.
Freeman LM, Chandler ML, Hamper BA, Weeth LP. Current knowledge about the risks and benefits of raw meat–based diets for dogs and cats. J Am Vet Med Assoc. 2013. https://doi.org/10.2460/javma.243.11.1549.
Behravesh CB, Ferraro A, Deasy M, Dato V, Moll M, Sandt C, et al. Human Salmonella Infections Linked to Contaminated Dry Dog and Cat Food, 2006-2008. Pediatrics. 2010. https://doi.org/10.1542/peds.2009-3273.
Soffer N, Abuladze T, Woolston J, Li M, Hanna LF, Heyse S, et al. Bacteriophages safely reduce Salmonella contamination in pet food and raw pet food ingredients. Bacteriophage. 2016. https://doi.org/10.1080/21597081.2016.1220347.
Fredriksson-Ahomaa M, Heikkilä T, Pernu N, Kovanen S, Hielm-Björkman A, Kivistö R. Raw Meat-Based Diets in Dogs and Cats. Vet Sci. 2017. https://doi.org/10.3390/vetsci4030033.
Morley PS, Strohmeyer RA, Tankson JD, Hyatt DR, Dargatz DA, Fedorka-Cray PJ. Evaluation of the association between feeding raw meat and Salmonella enterica infections at a Greyhound breeding facility. J Am Vet Med Assoc. 2006. https://doi.org/10.2460/javma.228.10.1524.
ISO 6579-1. Microbiology of the food chain - Horizontal method for the detection, enumeration and serotyping of Salmonella – Part 1: Detection of Salmonella spp. 2017. https://www.iso.org/standard/56712.html. Accessed 24 Mar 2022.
ISO 11290-1. Microbiology of the food chain - Horizontal method for the detection and enumeration of Listeria monocytogenes and of Listeria spp. – Part 1: Detection method 2017. https://www.iso.org/standard/60313.html. Accessed 24 Mar 2022.
ISO 10272-1. Microbiology of the food chain - Horizontal method for detection and enumeration of Campylobacter spp. Part 1: Detection method. 2017. https://www.iso.org/standard/63225.html. Accessed 24 Mar 2022.
ISO 16649-2. Microbiology of food and animal feeding stuffs - Horizontal method for the enumeration of beta -glucuronidase-positive Escherichia coli. - Part 2: colony-count technique at 44 degrees C using 5-bromo-4-chloro-3-indolyl beta D-glucuronide. 2001. https://www.iso.org/standard/29824.html. Accessed 24 Mar 2022.
Wegener HC, Madsen M, Nielsen N, Aarestrup FM. Isolation of vancomycin resistant Enterococcus faecium from food. Int J Food Microbiol. 1997;35:57–66.
Ahmad M, Smith DG, Mahboob S. Effect of NaCl on heat tolerance of Enterococcus faecium and Enterococcus faecalis. J Biol Sci. 2002;2:483–4.
Tanih NF, Sekwadi E, Ndip RN, Bessong PO. Detection of pathogenic Escherichia coli and Staphylococcus aureus from Cattle and Pigs Slaughtered in Abattoirs in Vhembe District. South Africa. Sci World J. 2015. https://doi.org/10.1155/2015/195972.
Ramovic E, Madigan G, McDonnell S, Griffin D, Bracken E, Ní Ghallchóir E, et al. A pilot study using environmental screening to determine the prevalence of Mycobacterium avium subspecies paratuberculosis (MAP) and antimicrobial resistance (AMR) in Irish cattle herds. Ir VetJ. 2020. https://doi.org/10.1186/s13620-020-0156-2.
Prendergast DM, O Grady D, McCann A, McCabe E, Fanning S, Egan J, et al. Application of PCR for rapid detection and serotyping of Salmonella spp. from porcine carcass swabs following enrichment in semi-solid agar. Food Res Int 2012; 45:993–999.
Prendergast DM, Hand D, Ní Ghallchóir Ghallchóir E, McCabe E, Fanning S, Griffin M, et al. A multiplex real-time PCR assay for the identification and differentiation of Salmonella enterica serovar Typhimurium and monophasic serovar 4,[5],12:i. Int J Food Microbiol. 2013;166:48–53.
2013/652/EU: Commission Implementing Decision of 12 November 2013 on the monitoring and reporting of antimicrobial resistance in zoonotic and commensal bacteria. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32013D0652. Accessed 24 Mar 2022.
S.I. No. 252/2008 - European Communities (Transmissible Spongiform Encephalopathies and Animal By-Products) Regulations 2008. https://www.irishstatutebook.ie/eli/2008/si/252/made/en/. Accessed 25 Mar 2022.
European Commission. Commission Regulation (EU) No 142/2011 of 25 February 2011 implementing Regulation (EC) No 1069/2009 of the European Parliament and of the Council laying down health rules as regards animal by-products and derived products not intended for human consumption and implementing Council Directive 97/78/EC as regards certain samples and items exempt from veterinary checks at the border under that Directive. Off J Eur Union. 2011; L 54/1-L 54/254.
Mattick KL, Bailey RA, Jørgensen F, Humphrey TJ. The prevalence and number of Salmonella in sausages and their destruction by frying, grilling or barbecuing. J Appl Microbiol. 2002;93:541–7.
Nemser SM, Doran T, Grabenstein M, McConnell T, McGrath T, Pamboukian R, et al. Investigation of Listeria, Salmonella, and toxigenic Escherichia coli in various pet foods. Foodborne Pathog Dis. 2014. https://doi.org/10.1089/fpd.2014.1748.
Strohmeyer RA, Morley PS, Hyatt DR, Dargatz DA, Scorza AV, Lappin MR. Evaluation of bacterial and protozoal contamination of commercially available raw meat diets for dogs. J Am Vet Med Assoc. 2006. https://doi.org/10.2460/javma.228.4.537.
Bacci C, Vismarra A, Dander S, Barilli E, Superchi P. Occurrence and Antimicrobial Profile of Bacterial Pathogens in Former Foodstuff Meat Products Used for Pet Diets. J Food Prot. 2019. https://doi.org/10.4315/0362-028x.jfp-18-352.
Joffe DJ, Schlesinger DP. Preliminary assessment of the risk of Salmonella infection in dogs fed raw chicken diets. Can Vet J. 2002;43:441–2.
Philbey AW, Mather HA, Gibbons JF, Thompson H, Taylor DJ, Coia JE. Serovars, bacteriophage types and antimicrobial sensitivities associated with salmonellosis in dogs in the UK (1954–2012). 2015; doi: https://doi.org/10.1136/vr.101864.
Fox E, O’Mahony T, Clancy M, Dempsey R, O’Brien M, Jordan K. Listeria monocytogenes in the Irish dairy farm environment. J Food Prot. 2009;72:1450–6.
Fagerlund A, Møretrø T, Heir E, Briandet R, Langsrud S. Cleaning and Disinfection of Biofilms Composed of Listeria monocytogenes and Background Microbiota from Meat Processing Surfaces. Appl Environ Microbiol. 2017. https://doi.org/10.1128/AEM.01046-17.
Schulze F, Bagon A, Müller W, Hotzel H. Identification of Campylobacter fetus subspecies by phenotypic differentiation and PCR. J Clin Microbiol 2006; doi:https://doi.org/https://doi.org/10.1128/JCM.02566-05.
Hakkinen M, Heiska H, Hänninen M-L. Prevalence of Campylobacter spp. in cattle in Finland and antimicrobial susceptibilities of bovine Campylobacter jejuni strains. Appl Environ Microbiol. 2007;73:3232–8.
Hellgren J, Hästö LS, Wikström C, Fernström L-L, Hansson I. Occurrence of Salmonella, Campylobacter, Clostridium and Enterobacteriaceae in raw meat-based diets for dogs. Vet Rec. 2019;184:442.
Bojanić K, Midwinter AC, Marshall JC, Rogers LE, Biggs PJ, Acke E. Isolation of Campylobacter spp. from Client-Owned Dogs and Cats, and Retail Raw Meat Pet Food in the Manawatu, New Zealand. Zoonoses Public HLTH. 2017. https://doi.org/10.1111/zph.12323.
Wagenaar JA, van Bergen MAP, Blaser MJ, Tauxe RV, Newell DG, van Putten JPM. Campylobacter fetus infections in humans: exposure and disease. Clin Infect Dis. 2014;58:1579–86.
Facciolà A, Riso R, Avventuroso E, Visalli G, Delia SA, Laganà P. Campylobacter: from microbiology to prevention. J Prev Med Hyg. 2017;58:E79–92.
Carbonero A, Torralbo A, Borge C, García-Bocanegra I, Arenas A, Perea A. Campylobacter spp., C. jejuni and C. upsaliensis infection-associated factors in healthy and ill dogs from clinics in Cordoba, Spain. Screening tests for antimicrobial susceptibility. Vol. 35. Comp Immunol Microbiol Infect Dis. 2012;35:505–12.
Chen JH, Ren Y, Seow J, Liu T, Bang WS, Yuk HG. Intervention Technologies for Ensuring Microbiological Safety of Meat: Current and Future Trends. Compr Rev Food Sci Food Saf. 2012;11:119–32.
Martin H, Manzanilla EG, More SJ, O’Neill L, Bradford L, Carty CI, et al. Current antimicrobial use in farm animals in the Republic of Ireland. Ir Vet J. 2020. https://doi.org/10.1186/s13620-020-00165-z.
Baede VO, Wagenaar JA, Broens EM, Duim B, Dohmen W, Nijsse R, et al. Longitudinal study of extended-spectrum-β-lactamase- and AmpC-producing Enterobacteriaceae in household dogs. Antimicrob Agents Chemother. 2015;59:3117–24.
Acknowledgments
This work was funded by the Department of Agriculture, Food and the Marine (DAFM). The authors gratefully acknowledge the participating knackeries and the veterinary inspectors in facilitating this 12-month study. Thanks especially to Dr John Griffin and Tom Loftus DAFM. This research could not have been performed without the expert technical assistance of many staff at DAFM laboratories.
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
N/A
Author information
Authors and Affiliations
Contributions
The study's conception and design were done by J. E, F. L, Montserrat Gutierrez and D. P who also contributed to writing and editing of the manuscript. S.McD carried out testing and contributed to writing the manuscript. T.O’B and P. K in part supervised testing. D. P also supervised AMR testing and interpreted AMR results. G. M and E. B tested AMR samples. M. G and J’McL typed Salmonella isolates. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/A
Consent for publication
N/A
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McDonnell, S., Gutierrez, M., Leonard, F.C. et al. A survey of food-borne and antimicrobial resistance-harbouring bacteria in meat by-products from knackeries and associated equipment and kennels. Ir Vet J 75, 9 (2022). https://doi.org/10.1186/s13620-022-00219-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13620-022-00219-4