Abstract
Objectives
To identify the prevalence and associated factors of cognitive dysfunction, 1 year after ICU discharge, among adult patients, and it´s relation with quality of life.
Methods
Multicenter, prospective cohort study including ICUs of 10 tertiary hospitals in Brazil, between May 2014 and December 2018. The patients included were 452 adult ICU survivors (median age 60; 47.6% women) with an ICU stay greater than 72 h.
Results
At 12 months after ICU discharge, a Montreal Cognitive Assessment (tMOCA) telephone score of less than 12 was defined as cognitive dysfunction. At 12 months, of the 452 ICU survivors who completed the cognitive evaluation 216 (47.8%) had cognitive dysfunction.
In multivariable analyses, the factors associated with long-term (1-year) cognitive dysfunction were older age (Prevalence Ratio–PR = 1.44, P < 0.001), absence of higher education (PR = 2.81, P = 0.005), higher comorbidities on admission (PR = 1.089; P = 0.004) and delirium (PR = 1.13, P < 0.001). Health-related Quality of life (HRQoL), assessed by the mental and physical dimensions of the SF-12v2, was significantly better in patients without cognitive dysfunction (Mental SF-12v2 Mean difference = 2.54; CI 95%, − 4.80/− 0.28; p = 0.028 and Physical SF-12v2 Mean difference = − 2.85; CI 95%, − 5.20/− 0.50; P = 0.018).
Conclusions
Delirium was found to be the main modifiable predictor of long-term cognitive dysfunction in ICU survivors. Higher education consistently reduced the probability of having long-term cognitive dysfunction. Cognitive dysfunction significantly influenced patients’ quality of life, leading us to emphasize the importance of cognitive reserve for long-term prognosis after ICU discharge.
Similar content being viewed by others
Background
Brain dysfunction related with critical illness [1] encompasses a broad spectrum of pathology from acute dysfunction as delirium, to long-term cognitive dysfunction [2]. Surviving ICU carries a burden related with brain dysfunction and poor quality of life [3,4,5], but despite the increasing amount of evidence, cognitive dysfunction natural history remains unclear.
Cognitive dysfunction develops through a complex interaction between patient’s baseline vulnerability (i.e. age, genetic predisposition, preexisting cognitive dysfunction) [6, 7] and precipitating factors (i.e. delirium, sepsis, surgery/anesthetics, metabolic derangement). Its prevalence is highly heterogeneous and influenced by the cognitive assessment test used, the time of analysis and also by the population studied (disease specific or mixed populations of medical and surgical ICU patients) [8] Cognitive dysfunction assessed early after hospital discharge has been described to affect up to 100% of the ICU survivors [9], and, even though cognitive dysfunction prevalence decreases over time after ICU discharge, long-term follow-up reveals high levels of long-term cognitive impairment several years after ICU discharge, in some series affecting 80% of the ICU survivors after one year and 45% after 2 years [8, 10].
Worse cognition has been described to be associated with worse quality of life scores [4] but the attributable impact of pre-ICU health, critical illness, and post-ICU disabilities on long-term cognitive function is not clear, especially in a resource-limited context like Brazil.
Early identification of patients at risk and the promotion of interventions on the associated factors may eventually improve outcome by reducing both acute and long-term cognitive dysfunction, ultimately improving quality of life.
In this study, the authors aim to investigate the prevalence of cognitive dysfunction 12 months after ICU discharge. The second objective is to identify factors associated with cognitive dysfunction 12 months after ICU discharge, including health related quality of life.
Methods
Study design
The present study is part of the Quality of life after intensive care unit: a multicenter cohort study for assessment of long-term outcomes among ICU survivors in Brazil. The study protocol has been published previously [11,12,13] The study was conducted from May 2014 to December 2018 in 10 Brazilian tertiary hospitals. Patients were recruited while still in the hospital and followed-up by telephone interviews at 3, 6 and 12 months after ICU discharge [12].
The study was planned under the Brazilian National Health Council Resolution no. 466/12 and approved by the research ethics committees of all participating centers. Informed consent was obtained from all study participants or their legal representatives [12].
Participants
Patients over 18 years old with an ICU stay exceeding 72 h for medical or emergency surgery or 120 h for elective surgery, were consecutively screened for eligibility. Patients were included in the analysis if cognitive follow-up at 12 months was successful. Exclusion criteria were: previous dementia diagnosis, transfer between hospitals; direct discharge home from ICU; < 24 h ICU readmission after discharge; absence of proxy for patients with communication difficulties; impossibility of assessing the patient during the first 5 days after ICU discharge, refusal or withdrawal of agreement to participate; previous enrollment in the study; no available telephone contact, failure to complete one year follow-up [12].
Associated factors
When considering associated factors for cognitive dysfunction, 5 sets of variables were evaluated:
-
1.
Sociodemographic characteristics: age, sex, educational attainment, household income;
-
2.
Health state 3 months before ICU admission: physical functional status; comorbidities; lifetime history of anxiety or depression;
-
3.
Acute illness characteristics: ICU admission type, risk of death at ICU admission, presence of sepsis or ARDS, organ dysfunction during ICU stay, ICU acquired infections, length of ICU and hospital stay;
-
4.
ICU discharge status: muscular strength, symptoms of anxiety and depression, cognitive function;
-
5.
Status 12 months after ICU discharge: vital status; HRQoL.
Independent variables (1 to 4) were collected using structured face-to-face interviews, physical examination, and retrospective review of medical records performed at the moment of patient enrollment (24–120 h after ICU discharge) and during telephone interviews (variables 5).
Physical functional status was assessed by Barthel index [14], where physical dependence was defined as a score of less than or equal to 75 [15, 16]. Comorbidities were collected using the Charlson Comorbidity Index [17] dichotomized as low (score 0 or 1) or high comorbidity (≥ 2). The risk of death at ICU admission, was derived from the Acute Physiology and Chronic Health Evaluation II [18] or the Simplified Acute Physiology Score 3 [19]. Sepsis and acute respiratory distress syndrome were defined according to the sepsis-II [20] and Berlin [21] definitions, respectively. Organ dysfunction was defined as the presence of invasive mechanical ventilation, vasopressor, renal replacement therapy (except for patients under chronic dialysis treatment), parenteral nutrition, blood or blood products transfusion, and delirium (measured according the Confusion Assessment Method for the ICU [22]). ICU-acquired infections were defined, by chart review, as pneumonia, bloodstream or urinary tract infection occurring > 48 h of ICU admission according to the European Centre for Disease Prevention and Control criteria [23]. Muscular strength was assessed using the Medical Research Council Scale [24], with a cut off of < 48 for ICU acquired weakness (ICUAW) [25]. Anxiety and depression were assessed using the Hospital Anxiety and Depression Scale [23]. After ICU discharge, the Mini Mental State Examination (MMSE) [26] was applied. No higher education was defined as not holding a university degree. Some continuous variables were categorized using predefined relevant cut-off points to facilitate interpretation.
Outcomes and follow-up
Researchers, not associated with patient care, assessed outcomes using a structured telephone interviews 3, 6 and 12 months after ICU discharge within a 30-day window (15 days before and 15 days after due date). Patients were categorized as follow-up losses after 10 unsuccessful attempts of telephone contact, at different times on several days within the window.
Family members were allowed to answer objective questions when patients lacked adequate physical or cognitive conditions. For subjective outcomes, like cognition or health related quality of life, family members were not allowed to interfere [12].
Cognitive function
To establish cognitive dysfunction, patients underwent a comprehensive neuropsychological evaluation at 12 months after ICU discharge. Immediately after ICU discharge was applied the Mini Mental State Examination (MMSE) [26] and twelve months after ICU discharge, cognitive function was assessed using the Brazilian version validated for telephone administration of the Montreal Cognitive Assessment (tMoCA) [27]. In tMoCA, the domains analyzed are short-term memory; executive function; attention, concentration, and working memory; language; orientation to time and place. It enables subject evaluation for mild cognitive impairment, irrespective of etiology. tMoCA scores range from 0 to 22; higher scores indicate better cognitive status. There is no specific data regarding tMoCa average score for cognitive impairment in ICU patients. In other populations, the MoCa average score for mild cognitive impairment is described to be 22, and 17 for moderate/severe cognitive impairment. In the literature, it has been described a tMoCA score of 12 as equivalent to a MoCA Full score of 17 [28, 29]. For clinical relevance, in the trade-off between sensitivity Vs specificity, and in order to identify the more severe patients, a tMoCA score of 12 was used as a cut-off for moderate/severe cognitive impairment. For reference, a tMoCa score of 16 was used as a cut off for mild cognitive impairment.
Health-related quality of life
The HRQoL was assessed at 12 months using the Short-Form Health Survey version 2 (SF-12v2) [30] The SF-12v2 addresses HRQoL in eight domains: general health, physical functioning, physical role function, bodily pain, vitality, emotional role function, mental health, and social functioning. These 8 domains are then summarized in 2 dimensions, physical and mental, and each domain scores ranges from 0 to 100, where higher scores indicate better HRQoL. A score of 42 or less on the mental SF-12v2 may be indicative of "clinical depression," whereas a score of 50 or less on the physical SF-12v2 has been recommended as a cut-off to indicate a physical condition [31].
Statistical analysis
Continuous variables were registered as mean and standard deviation or median and interquartile range as appropriate. Categorical variables were expressed as absolute and relative frequencies. Associated factors for 12-month cognitive dysfunction were based on premorbid condition, during ICU stay, and in the immediate post-discharge period. They were assessed by calculating Prevalence Ratio (PR) as association measures, using Generalized Estimating Equations (GEE) Poisson models, in order to adjust for the effect of patients’ clustering within the 10 different centers/hospitals participating in the study. In the GEE models, a Poisson distribution was used for the binary response variable (primary outcome – presence of cognitive dysfunction), we assumed an exchangeable covariance matrix, and robust sandwich variance estimators were used to estimate the model coefficients. In this context, appropriately corrected robust variance estimators are essential to overcome the possible misspecification of the variance of Poisson distributions and of the working covariance matrix [32, 33]. Variables with P-value less than 0.20 were considered in the multivariable model and a stepwise backward selection method was used for variable selection.
In order to assess survival bias (influence of patients’ survival on the results), a sensitivity analysis was performed). In this analysis we also included patients who died during the 12 months follow-up by giving them a MoCA score of zero; thus, changing the primary outcome to a composite outcome of death or cognitive dysfunction.
All analyzes were conducted in the R software, version 4.2.2. A significance level of 5% was considered.
Results
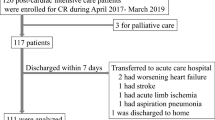
Among the 1,616 patients included in the Post-ICU Quality of Life Project [12], 98 patients were excluded due to previous dementia; of the 1108 patients alive after 12 months of follow-up, 656 patients were excluded due to lack of cognitive assessment (Supplemental Figure 1 and Supplemental Table S1). A total of 452 patients were analyzed (Table 1). The characteristics of the 10 participating hospitals that recruited patients are shown in Supplemental Table S2.
Characteristics of the Cohort
In Table 1 we describe the characteristics of the 452 participants who completed the 12 months cognitive assessment. The median age was 60 years and 47.6% were women. Only 28.2% (n = 127/450) of the patients had higher education. Half the patients had high comorbidity (46.2%); 17.1% had past history of depression and 19,5% of anxiety. Medical condition accounted for 67.7% of all admissions. The need for invasive mechanical ventilation and vasopressor were the most frequent organ dysfunction [47.6% and 52% respectively]. Delirium was present in 19.9% of the patients. The median ICU and hospital length of stay (LOS) was 6 (IQR 4–10) and 21 (IQR 13–36) days. Early after ICU discharge, 39.1% of the patients presented anxiety symptoms; 21.6% depression symptoms; 32.5% cognitive dysfunction and 21.1% had ICUAW.
12 Months prevalence of cognitive dysfunction and associated factors
Twelve months after ICU discharge, of the 452 patients who were able to complete cognitive evaluation, 351 (77.7%) had some degree of cognitive dysfunction (tMOCA < 16) of whom 216 (47.8%) had moderate to severe cognitive dysfunction (tMOCA < 12). Up to different extent, all the subdomains of tMOCA were affected both in patients with or without cognitive dysfunction. In patients with cognitive dysfunction the least affected was orientation (correct response rate over 70%) and the most severely affected were delayed recall (incorrect response rate over 90%) and serial subtraction (incorrect response rate over 75%). Abstraction accounted for the higher difference in correct responses in patients with or without cognitive dysfunction. (Fig. 1).
In the univariable analysis (Table 2), factors identified to be associated with higher risk for cognitive dysfunction at 1 year are as follows: increasing age (PR 1.02; P < 0.001), no higher education (PR 2.07, P < 0.001), and pre-ICU high comorbidity (PR 1.2, P < 0.001). On the other hand, educational attainment (PR 0.92, P < 0.001) and household income (independent of number of minimum wages considered) were considered protective.
When considering organ dysfunction only the need of parenteral nutrition (PR 1.3, P = 0.008) and delirium (PR 1.11, P = 0.005) were significant for increased risk of cognitive dysfunction. On the other hand, invasive mechanical ventilation (PR 0.83, P = 0.01); vasopressor use (PR 0.87, P = 0.043) and blood products use (PR 0.82, P = 0.021) appeared to be protective against cognitive dysfunction. Also, the presence of ICU-acquired infection (PR 0.69, P = 0.021) and hospital LOS appear to be protective towards cognitive dysfunction (0.99, p = 0.046).
Contrary to anxiety after ICU discharge (PR 1.19, P < 0.001), past history of anxiety (PR 0.84; p = 0.001) appear to be protective towards cognitive dysfunction.
Cognitive dysfunction early after ICU discharge (PR 1.27, P < 0.001) was positively associated with long-term cognitive dysfunction, unlike muscular weakness (PR 0.96, p = 0.718).
Table 3 shows the multivariable analysis of factors independently associated with cognitive dysfunction. Higher education was consistently protective against long-term cognitive dysfunction both in univariate (no Higher education: PR 2.07, P < 0.001) and in multivariable analysis (no Higher education: PR 1.98, p = 0.005). Older age (PR 1.44, P < 0.001), delirium (PR 1.13, p < 0.001) and pre-ICU high comorbidity (PR 1.09, p = 0.004) were also associated with the probability of having long-term cognitive dysfunction.
The sensitivity analysis, aimed at assessing the risk of survival bias, showed similar results to those of the main analyses (Supplemental Table S6) except for the fact that functional dependence and muscular strength now appear associated with cognitive dysfunction, and de novo also the risk of death at ICU admission. Delirium maintained its association with cognitive dysfunction, while ARDS at ICU appears to be protective against cognitive dysfunction.
Health-related quality of life
The HRQoL assessed at 12 months by the mental dimension of the SF-12v2, was significantly better in patients who did not have cognitive dysfunction (Mean difference = − 2.54; CI 95%, − 4.80/− 0.28; p = 0.028). The physical dimension was also significantly better in patients who did not have cognitive dysfunction at 12 months (Mean difference = − 2.85; CI 95%, − 5.20/− 0.50; P = 0.018). (Fig. 2; Supplemental Table S3).
When analyzing the SF-12v2 domains, patients with cognitive dysfunction showed worse scores in the domains of general health, physical functioning, physical role function, bodily pain, vitality, mental health, and social functioning, but not in emotional role function (Supplemental Table S4).
When analyzing functional impairment, the study found no differences between patients with or without cognitive dysfunction at any time point (3mo: p = 0.09; 6mo: p = 0.07; 12mo: p = 0.33). (Supplemental Table S5).
Discussion
Among the patients evaluated for cognitive dysfunction twelve months after ICU discharge, 351 (77.7%) had some degree of cognitive dysfunction (tMOCA < 16) and considering the study population with a tMOCA < 12, 216 (47.8%) patients had moderate to severe cognitive dysfunction. In the univariate analysis several factors were associated with an increased or decreased risk for cognitive dysfunction, but in the multivariate analysis only older age, delirium during ICU stay and pre-ICU high comorbidity were associated with an increased risk of having long-term cognitive dysfunction. Higher education was consistently protective against long-term cognitive dysfunction. The overall HRQoL assessed at 12 months was significantly better in patients who did not have cognitive dysfunction. Functional impairment and cognitive dysfunction were not associated throughout the natural history of ICU survivors.
The long-term cognitive dysfunction prevalence in our sample is worse than other studies conducted in high-resource/income contexts [8, 10, 34]. Still, we consider that it may be underestimated, both because in our study, we only considered moderate and severe cognitive dysfunction and also because the severity of functional or cognitive impairment may have prevented survivors to complete the assessment.
Results show an increase in cognitive dysfunction between discharge and 12 months follow up. The author interpretation is that the results found are secondary to the sensitivity of the chosen test and the use of MMSE at ICU discharge may have underestimated the true impact of early cognitive impairment, when compared to tMoCA or MoCA [8]. In accordance with previous published data [9] and clinical experience, author believe that the natural history of ICU acquired cognitive dysfunction is that almost all patients discharged from ICU experience different degree of cognitive dysfunction related to ICU admission and that it decreases throughout time. Authors decision to apply different tests was based on the assumption that the use of MoCa test at ICU discharge would result in a low response rate due to MoCa test complexity. Telephone assessment at 12 months did not allow the application of the MMSE in the same time frame.
We may interpret the prevalence of cognitive dysfunction found as a result of the historical economic evolution of Brazil, starting from a low-income country to becoming one of the largest economies in the world, but still having a middle class that represents 1/3 of the population [35]. In our cohort, the median household income per capita is comprised in the interval considered as middle-income class. Also, and, even though Brazil has, since 2009, one of the world’s longest duration of compulsory education, it is still paying the burden of years of non-investment and social discrepancies, as 1/4 of the population did not attend or finish high school, elementary school or are illiterate [35]. In our cohort, the average number of years of schooling, 11 years, suggests this reality. It is noteworthy that education level influenced the performance on tMOCA, sustainably as a protective factor. This may be explained through the concept of brain and cognitive reserve, that refers to the individuals ability to tolerate the age and disease-related changes without developing cognitive deterioration signs or symptoms [36, 37]. Our study evokes evidence of the importance of cognitive reserve, represented by a protective effect of higher education in the cognitive performance after ICU. The amount of cognitive reserve is likely acquired through educational attainment, physical and mental activity, occupational performance and successful social relationships. The association between higher household income and better cognitive outcome [38], may also be indicative of higher educational attainment.
Consistent with previous evidence, we found increasing age and comorbidity before ICU as associated factors for cognitive impairment [39,40,41]. Older age was consistently associated with worse cognitive outcome and may be a proxy for lower brain and cognitive reserve.
In a non-fragmented population of ICU survivors, and despite its low [6] incidence, the authors confirmed previous evidence that delirium is a predictor of worse cognitive outcome after ICU discharge [10, 42,43,44]. Delirium during ICU stay may as well be the only modifiable factor towards better cognitive outcome. When analyzing organ dysfunction, even though others dysfunctions have been previously implicated in long-term cognitive dysfunction [10, 45, 46], in our study only delirium was implicated in worse cognitive outcome. The dichotomized nature of the collected variables may have underestimated the true impact of acute organ dysfunction on long-term cognitive dysfunction.
Functional impairment after ICU depends on a myriad of causes and is currently described in the spectrum of ICU acquired weakness. In non-ICU patients, physical performance is an important predictor of cognitive performance [47]. In our cohort, muscle weakness early after ICU discharge was not statistically related to long-term cognitive dysfunction except in the sensitivity analysis. When analyzing functional impairment as a composite outcome, which include physical functioning, at 3 and 6 months, although it does not reach statistical significance, we can hypothesize that it may be clinically significant, and that only at 12 months does functional dependence loses a clear significance towards the cognitive outcome. This data is particularly relevant, as this points out to a possible modifiable associated factor for long-term cognitive dysfunction and for one of the possible early interventions during ICU admission that may improve long term outcome: early physical rehabilitation.
Quality of life measured by SF-12v2 is better for patients without cognitive dysfunction [4]. It can be hypothesized that quality of life after ICU depends on a prior construct and personal behaviors, with cognitive and brain reserve appearing to play a preemptive role in cognitive outcomes. If we think of brain and neural connections as something we can train, then the same is true for what should be the focus of rehabilitation after ICU: we should rehabilitate both the brain as well as the body [48, 49].
Potentially modifiable factors such as delirium and physical impairment must be screened during hospital stay. Early identification of ICU patients at increased risk for cognitive impairment, who might benefit from preventive measures or early rehabilitation, should be a future area of investment.
Strengths and limitations
Strengths
The study has several major strengths: its prospective multicenter design, the inclusion of a large mixed population of ICU survivors, the prior definition of outcomes, the joint assessment of variables before, during and after ICU discharge in the same study and the use of standardized and validated instruments to measure cognitive outcomes [12]. Sensitivity analyses was performed to deal with possible bias.
Weaknesses
This study has several limitations. The study’s observational design may introduce inherent biases such as unmeasured confounders, selection bias, response and survival bias.
The study´s high sample size may have mitigated potential bias, but 59.2% of patients did not complete cognitive evaluation, potentially underestimated the prevalence and significance of the actual dysfunction. A significant limitation of the study is the large proportion of patients excluded for absence of cognitive evaluation as 12 months thus introducing a selection bias.
Another limitation is that tests used to evaluate cognitive function between discharge and 12 months follow-up were different making it difficult to understand the evolution of cognitive function. Also, the use of MMSE at ICU discharge may have underestimated the true impact of early cognitive impairment, when compared to tMoCA ou MoCA. Authors decision to apply different tests was based on the assumption that the use of MoCa test at ICU discharge would result in a low response rate due to MoCa test complexity.
In our cohort, for the purpose of a pragmatic study, except for dementia, we did not exclude patients with known medical diagnosis that might contribute to a worse cognitive outcome, and also potentially exacerbate the role of age as an associated factor.
Another limitation is the lack of pre-ICU cognitive assessment. Another study that assessed baseline cognitive status showed that in pre-ICU admission only 6% of patients had evidence of mild-to- moderate cognitive impairment [39, 50], suggesting that extrapolating pre-ICU cognitive dysfunction in our sample could yield similar results.
Finally, and even though psychological disorders can influence cognitive performance, the long-term outcomes specified in the study protocol [12] were planned to be mental illness at 6 month and cognitive dysfunction at 12 months. For that, authors cannot provide data concerning mental illness at 1 year.
Conclusion
ICU-related cognitive impairment is a topic that requires continued attention, not only because cognitive function is a predictor of quality of life, but essentially because survivors won’t be able to return to their previous life if they do not recover their cognitive function.
The only clear potential modifiable associated factor for long-term cognitive dysfunction among ICU survivors was delirium. Higher education was consistently protective against long-term cognitive dysfunction, leading us to consider the importance of cognitive reserve and of the social and educational politics towards improving educational attainment. Regarding pre-ICU comorbidity, a call for action must take place towards a healthier lifestyle in order to decrease this potential modifiable associated factor.
The continuum of brain and physical dysfunction must be addressed from the outset. The importance of preventing and treating cognitive and physical dysfunction during ICU stay should be paralleled by rehabilitation after ICU discharge aiming to reduce ICU sequelae. Future clinical trials focusing on physical and cognitive rehabilitation could demonstrate the potential benefits of such interventions.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APACHE-II:
-
Acute Physiology and Chronic Health Evaluation II
- ARDS:
-
Acute respiratory distress syndrome
- BI:
-
Barthel Index
- CAM-ICU:
-
Confusion Assessment Method for the ICU
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence Interval
- GEE:
-
Generalized Estimative Equations
- GLM:
-
Generalized Linear Model
- HADS-a::
-
Hospital Anxiety and Depression Scale Anxiety
- HADS-d::
-
Hospital Anxiety and Depression Scale Depression
- HRQoL:
-
Health-Related Quality of Life
- ICU:
-
Intensive care unit
- ICUAW:
-
ICU acquired weakness
- IQR:
-
Interquartile range
- ME:
-
Mean difference
- MMSE:
-
Mini Mental State Examination
- MRC:
-
Medical Resuscitation Council Scale
- PR:
-
Prevalence Ratio
- SAPS-3:
-
Simplified Acute Physiology Score 3
- SF-12v2:
-
Short Form Survey: Short Form 12 Version 2
- tMOCA:
-
Telephone Montreal Cognitive Assessment
References
Petzold A, Downie P, Smith M. Critical illness brain syndrome (CIBS): an underestimated entity? Crit Care Med. 2005;33(6):1464.
Morandi A, Pandharipande PP, Jackson JC, Bellelli G, Trabucchi M, Ely EW. Understanding terminology of delirium and long-term cognitive impairment in critically ill patients. Best Pract Res Clin Anaesthesiol. 2012. https://doi.org/10.1016/j.bpa.2012.08.001.
Duggan MC, Wang L, Wilson JE, Dittus RS, Ely EW, Jackson JC. The relationship between executive dysfunction, depression, and mental health-related quality of life in survivors of critical illness: results from the BRAIN-ICU investigation. J Crit Care. 2017;37(615):72–9.
Gorgoraptis N, Zaw-Linn J, Feeney C, Tenorio-Jimenez C, Niemi M, Malik A, et al. Cognitive impairment and health-related quality of life following traumatic brain injury. NeuroRehabilitation. 2019;44(3):321–31.
Hopkins RO, Ely EW, Jackson JC. The role of future longitudinal studies in ICU survivors: understanding determinants and pathophysiology of brain dysfunction. Curr Opin Crit Care. 2007;13(5):497–502.
Ely EW, Girard TD, Shintani AK, Jackson JC, Gordon SM, Thomason JWW, et al. Apolipoprotein E4 polymorphism as a genetic predisposition to delirium in critically ill patients. Crit Care Med. 2007;35(1):112–7.
Maldonado JR. Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry. 2013;21(12):1190–222.
Honarmand K, Lalli RS, Priestap F, Chen JL, McIntyre CW, Owen AM, et al. Natural history of cognitive impairment in critical illness survivors a systematic review. Am J Respir Crit Care Med. 2020;202:193–201.
Hopkins RO, Weaver LK, Pope D, Orme JF, Bigler ED, Larson-LOHR V. Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 1999;160(1):50–6. https://doi.org/10.1164/ajrccm.160.1.9708059.
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16.
Rosa RG, Falavigna M, Robinson CC, Sanchez EC, Kochhann R, Schneider D, et al. Early and late mortality following discharge from the ICU: a multicenter prospective cohort study. Crit Care Med. 2020;48(1):64–72.
Robinson CC, Rosa RG, Kochhann R, Schneider D, Sganzerla D, Dietrich C, et al. Quality of life after intensive care unit: a multicenter cohort study protocol for assessment of long-term outcomes among intensive care survivors in Brazil. Rev Bras Ter Intensiva. 2018;30(4):405–13.
Teixeira C, Rosa RG, Sganzerla D, Sanchez EC, Robinson CC, Dietrich C, et al. The burden of mental illness among survivors of critical care—risk factors and impact on quality of life: a multicenter prospective cohort study. Chest. 2021;160(1):157–64.
Mahoney FI, Barthel D. Functional evaluation: the Barthel Index. Md State Med J. 1965;14(9):61–5.
Pournajaf S, Pellicciari L, Proietti S, Agostini F, Gabbani D, Goffredo M, et al. Which items of the modified Barthel Index can predict functional independence at discharge from inpatient rehabilitation? A secondary analysis retrospective cohort study. Int J Rehabil Res. 2023;46(3):230–7.
Uyttenboogaart M, Stewart RE, Vroomen PCAJ, De Keyser J, Luijckx GJ. Optimizing cutoff scores for the Barthel Index and the modified Rankin Scale for defining outcome in acute stroke trials. Stroke. 2005;36(9):1984–7.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–83.
Gil Cebrian J, Bello Cámara MP, Diaz-Alersi R. Apache Ii. Intensive Care Med. 1987;13(2):143.
Moreno RP, Metnitz PGH, Almeida E, Jordan B, Bauer P, Campos RA, et al. SAPS 3-from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005;31(10):1345–55.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International sepsis definitions conference. Crit Care Med. 2003;31(4):1250–6.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33.
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the intensive care unit (CAM-ICU). Crit Care Med. 2001;29(7):1370–9.
European Centre for Disease Prevention and Control. European surveillance of healthcare-associated infections in intensive care units-HAI-Net ICU protocol, version 1.02. Stockholm: ECDC; 2015.
Jellinger KA. Aids to the examination of the peripheral nervous system. Eur J Neurol. 2001;8(4):377–377.
Stevens RD, Marshall SA, Cornblath DR, Hoke A, Needham DM, De Jonghe B, et al. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med. 2009;37(SUPPL. 10):299–308.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state. J Psychiatr Res. 1975;12(3):189–98.
Pendlebury ST, Welch SJV, Cuthbertson FC, Mariz J, Mehta Z, Rothwell PM. Telephone assessment of cognition after transient ischemic attack and stroke: modified telephone interview of cognitive status and telephone montreal cognitive assessment versus face-to-face montreal cognitive assessment and neuropsychological battery. Stroke. 2013;44(1):227–9.
Melikyan ZA, Malek-Ahmadi M, O’Connor K, Atri A, Kawas CH, Corrada MM. Norms and equivalences for MoCA-30, MoCA-22, and MMSE in the oldest-old. Aging Clin Exp Res. 2021;33(12):3303–11.
Katz MJ, Wang C, Nester CO, Derby CA, Zimmerman ME, Lipton RB, et al. T-MoCA: a valid phone screen for cognitive impairment in diverse community samples. Alzheimer Dement. 2021;13(1):1–11.
Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Ware J, Kisinski M, Keller S. How to score SF-12 physical mental health summary scales. Boston: Health Institute, New England Medical Center; 1995. p. 1–93.
Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–70.
Pedroza C, Truong VTT. Estimating relative risks in multicenter studies with a small number of centers—which methods to use? A simulation study Trials. 2017;18(1):1–10.
Hopkins RO, Jackson JC. Short- and long-term cognitive outcomes in intensive care unit survivors. Clin Chest Med. 2009. https://doi.org/10.1016/j.ccm.2008.11.001.
Roser M. Our world in data. https://ourworldindata.org/. Accessed 11 Mar 2023.
Meng X, D’Arcy C. Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS ONE. 2012;7(6): e38268.
Fratiglioni L, Wang HX. Brain reserve hypothesis in dementia. J Alzheimers Dis. 2007;12(1):11–22.
Jain S, Murphy TE, O’Leary JR, Leo-Summers L, Ferrante LE. Association between socioeconomic disadvantage and decline in function, cognition, and mental health after critical illness among older adults a cohort study. Ann Intern Med. 2022;175(5):644–55.
Rengel KF, Hayhurst CJ, Pandharipande PP, Hughes CG. Long-term cognitive and functional impairments after critical illness. Anesth Analgesia. 2019;128:772–80.
Sakusic A, Rabinstein AA. Cognitive outcomes after critical illness. Curr Opin Crit Care. 2018;24(5):410–4.
Wilson ME, Barwise A, Heise KJ, Loftsgard TO, Dziadzko M, Cheville A, et al. Long-term return to functional baseline after mechanical ventilation in the ICU. Crit Care Med. 2018;46(4):562–9.
Müller A, von Hofen-Hohloch J, Mende M, Saur D, Fricke C, Bercker S, et al. Long-term cognitive impairment after ICU treatment: a prospective longitudinal cohort study (Cog-I-CU). Sci Rep. 2020;10(1):15518.
Van Den Boogaard M, Schoonhoven L, Evers AWM, Van Der Hoeven JG, Van Achterberg T, Pickkers P. Delirium in critically ill Patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012;40(1):112–8.
Salluh JIF, Wang H, Schneider EB, Nagaraja N, Yenokyan G, Damluji A, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350: h2538.
Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF. Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171(4):340–7.
Kohler J, Borchers F, Endres M, Weiss B, Spies C, Emmrich JV. Cognitive deficits following intensive care. Dtsch Arztebl Int. 2019;116(38):627–34. https://doi.org/10.3238/arztebl.2019.0627.
Song R, Park M, Seo J. Predicting quality of life with physical and cognitive functioning among older adults with cognitive impairment. Innov Aging. 2021;5(1):409–10.
Jackson JC, Ely EW, Morey MC, Anderson VM, Denne LB, Clune J, et al. Cognitive and physical rehabilitation of intensive care unit survivors. Crit Care Med. 2012;40(4):1088–97.
Cheng ST. Cognitive reserve and the prevention of dementia: the role of physical and cognitive activities. Curr Psychiatry Rep. 2016. https://doi.org/10.1007/s11920-016-0721-2.
Geense WW, Van Den Boogaard M, Peters MAA, Simons KS, Ewalds E, Vermeulen H, et al. Physical, mental, and cognitive health status of ICU survivors before ICU admission: a cohort study. Crit Care Med. 2020;48(9):1271–9.
Acknowledgements
Not applicable.
Funding
The present study was funded by the Brazilian Ministry of Health through the Brazilian Unified Health System Institutional Development Program (PROADI-SUS). Representatives of Brazilian Ministry of Health were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the manuscript. The decision to submit the manuscript for publication was made by the authors, and the sponsor had no veto right to publish or to control the decision to which journal to submit. This article was supported by National Funds through FCT - Fundação para a Ciência e a Tecnologia, I.P., within CINTESIS, R&D Unit (reference UIDB/4255/2020).
Author information
Authors and Affiliations
Contributions
The authors have contributed substantially to the conception and design of the study, the acquisition of data, or the analysis and interpretation of the data. All authors have read, provided critical revision of the article and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was planned under the Brazilian National Health Council Resolution no. 466/12 and approved by the research ethics committees of all participating centers. Informed consent was obtained from all study participants or their legal representatives [12].
Consent for publication
Not applicable.
Competing interests
RGR discloses receiving Pfizer honorary and Pfizer and MSD grant to the institution. The remaining authors disclose not having financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jesus Pereira, I., Santos, M., Sganzerla, D. et al. Long term cognitive dysfunction among critical care survivors: associated factors and quality of life—a multicenter cohort study. Ann. Intensive Care 14, 116 (2024). https://doi.org/10.1186/s13613-024-01335-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01335-w