Abstract
Purpose
The recent epidemiology of Pneumocystis pneumonia (PCP) requiring intensive care unit (ICU) admission and the associated spectrum of immunocompromising conditions are poorly described.
Methods
We analyzed all adult PCP cases admitted to French ICUs via the French medical database system (PMSI), over the period from 2013 to 2019.
Results
French ICUs admitted a total of 4055 adult patients with PCP. Among all hospitalized PCP cases, the proportion requiring ICU admission increased from 17.8 in 2014 to 21.3% in 2019 (P < 0.001). The incidence of severe PCP rose from 0.85 in 2013 to 1.32/100,000 adult inhabitants in 2019 (P < 0.0001), primarily due to the proportion of HIV-negative patients that increased from 60.6% to 74.4% (P < 0.0001). Meanwhile, the annual number of severe PCP cases among patients with HIV infection remained stable over the years. In-hospital mortality of severe PCP cases was 28.5% in patients with HIV infection and 49.7% in patients without.
Multivariable logistic analysis showed that patients with HIV infection had a lower adjusted risk of death than patients without HIV infection (Odds Ratio [OR]: 0.30, 95% confidence interval [95CI]: 0.17–0.55). Comorbidities or conditions strongly associated with hospital mortality included the patient’s age, Simplified Acute Physiologic Score II, congestive heart failure, coagulopathy, solid organ cancer, and cirrhosis. A vast array of autoimmune inflammatory diseases affected 19.9% of HIV-negative patients.
Conclusions
The number of PCP cases requiring ICU admission in France has risen sharply. While the yearly count of severe PCP cases in HIV-infected patients has remained steady, this rise predominantly affects cancer patients, with a recent surge observed in patients with autoimmune inflammatory diseases, affecting one in five individuals.
Similar content being viewed by others
Background
Pneumocystis jirovecii pneumonia (PCP) is an opportunistic fungal pneumonia that affects immunocompromised individuals [1]. Initially, it was identified in pre-term newborns in the 1950s and later in adults in the 1970s [2,3,4,5,6]. An epidemic phase was observed in the 1980s among patients with human immunodeficiency virus (HIV) infection [6]. This wave was greatly reduced by the introduction of antibiotic prophylaxis in the late 1980’s [6, 7] and by the advent of highly active antiretroviral therapy in the mid-1990’s [6, 8]. In the US, the prevalence of PCP among hospitalized HIV-positive patients showed a constant decline from 2002 to 2014 [9]. Despite this, PCP remains the second most common infection that defines AIDS in HIV-positive patients [10, 11]. The increasing use of immunosuppressive therapies (including corticosteroids) to treat conditions like cancer, hematologic malignancies, organ transplantation and autoimmune inflammatory diseases has led to an increased PCP incidence, with cases among patients with cancer or autoimmune diseases exceeding cases in HIV-positive patients [12,13,14]. While PCP is still considered a rare disease based on the European definition of fewer than five cases per 10,000 inhabitants annually, its annual number of cases worldwide could approach 500,000 cases [15]. It also remains the most common opportunistic respiratory infection in immunocompromised individuals [16], accounting for 12% of cases of community pneumonia in renal transplant patients, for example [17]. Numerous studies have shown that inflammatory diseases place patients at risk of PCP, and recommendations concerning prophylaxis have been developed in the last decades. However, comprehensive epidemiological studies that identified all potentially at-risk diseases are rare, and some inflammatory diseases still lack prophylaxis recommendations [18]. Even in the presence of prophylaxis recommendations, their application is imperfect [18, 19].
In this context, we aimed to evaluate the burden of severe PCP, defined as PCP cases requiring intensive care unit (ICU) admission during their hospitalization, in the French population during the years 2013 to 2019 by taking a comprehensive inventory of potentially predisposing diseases, comparing hospital outcome between HIV and non-HIV infected patients, and identifying the most important predisposing factors for in-hospital mortality.
Methods
This retrospective cohort study utilized de-identified data from the national Programme de médicalisation des systèmes d’information (PMSI) database, which is maintained by the French national agency for the management of hospitalization data (Agence technique de l’information sur l’hospitalisation, ATIH). The database includes all discharge summaries of patients from both private and public acute care hospitals in France, providing information such as patient demographics, length of stay, discharge conditions (including vital status at hospital discharge), cause of admission, and underlying diseases coded according to the tenth revision of the International Classification of Diseases (ICD-10).
Our study focused on discharge summaries from the years 2013 to 2019 that contained the diagnosis of PCP (i.e., the ICD-10 codes B485, B59, or B206) and an ICU stay in patients aged 18 years or older. Along with all acute and chronic patient’s conditions, these discharge summaries also include the diagnosis declared as the main cause of ICU admission, as well as the Simplified Acute Physiology Score II (SAPS II) [20] at ICU admission. We converted the ICD-10 codes for associated diagnoses into Elixhauser classes [21], using algorithms provided by the Agency for Healthcare Research and Quality (https://hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp). We also added detailed diagnoses of autoimmune, inflammatory, rheumatoid diseases, solid organ or hematologic malignancies, and organ transplantation (ICD-10 codes used are provided in the Online Supplemental material). For patients with multiple ICU stays during hospital stay, only the last ICU admission was considered.
Furthermore, to determine the frequency of ICU admissions among all patients diagnosed with PCP, and potentially identify patient subgroups more prone to ICU admission, we gathered hospitalization data of all PCP patients, regardless of ICU utilization. However, because of privacy policy restrictions inherent to the ATIH platform at the time of data extraction, these data were not available for the year 2013.
This study adhered to the French legal regulations for observational retrospective studies involving de-identified data, which are classified as non-human subject research. The investigators were authorized by the Commission Nationale Informatique et Liberté (CNIL, the National Data Protection Commission) to access the national PMSI database for scientific research purposes, to extract and analyze datasets without the need to inform the patients (which would not have been possible because of the de-identification of the data). The study protocol was approved by the ethics committee of the French Society of Critical Care (#CE SRLF 23-031).
This article adheres to the STROBE guidelines for the reporting of observational studies using routinely collected health data (RECORD statement) [22].
Statistical analysis
We expressed categorical variables as counts and percentages and continuous variables as mean (SD) or median (interquartile range) depending on their normal or non-normal distribution as graphically checked on quantile–quantile and density plots. Groups were compared by the χ2 test, t-test, Mann–Whitney U test, Cochran-Armitage test or analysis of variance, as appropriate. The incidence of severe adult PCP was calculated for each year using the national demographic data that are made publicly available by the National Institute of Statistics and Economic Studies (INSEE) (https://www.insee.fr/fr/statistiques/).
To identify the patients’ characteristics associated with in-hospital mortality, we used a multivariable binary logistic regression model. For the selection of variables, we used augmented backward elimination (ABE) that combines the standardized change-in-estimate criterion with significance-based backward elimination [23, 24]. The procedure was parameterized to minimize the risk of eliminating important variables (see Online Supplemental material for details). All interactions of each Elixhauser category of diseases with age and with HIV infection were considered and kept in the final model if significantly associated with in-hospital death. We use the aera under the receiver operating characteristics (AUCROC) curve and cross-validation to assess the discriminative power and calibration of the final logistic model, respectively.
For each variable retained in the final model, the association with in-hospital death was expressed as the adjusted odds ratio (OR) and its 95% confidence interval (95CI).
A 2-tailed P < 0.05 was considered statistically significant. However, P-values were not adjusted for multiple testing and should be considered exploratory. The analyses were performed using R software version 4.2.2 (R Foundation for Statistical Computing, http://www.R-project.org).
Results
Overall population of patients hospitalized with PCP over the period 2014–2019, and rate of ICU admission
Over the 2014–2019 period, a total of 18,306 patients were hospitalized with PCP. The number of cases increased steadily from 2821 cases in 2014 to 3119 cases in 2019, resulting in a significant rise from 5.7 to 6.2 cases per 100,000 adult inhabitants (P < 0.001) (Table 1). Concurrently, the proportion of PCP patients requiring ICU admission increased from 17.8 in 2014 to 21.3% in 2019 (P < 0.001), with 19.9% of all PCP patients (3541/18,306) admitted to the ICU over the 2014–2019 period. Notably, patients with HIV infection constituted 33.1% (6059/18,306) of PCP cases during this period, yet their proportion declined significantly each year, from 42.8 in 2014 to 27.3% in 2019 (P < 0.001). On average, patients with HIV infection were less frequently admitted to the ICU (18.1%) compared to those without HIV infection (20.7%) (P < 0.001). However, the percentage of HIV-infected patients requiring ICU admission increased significantly over the years, from 14.3 in 2014 to 19.9% in 2019 (P < 0.001). In-hospital mortality rates significantly rose from 6.5 in 2014 to 9.3% in 2019 among patients not admitted to the ICU (P < 0.001), while showing a slight and non-significant decrease among ICU-admitted patients (from 44.4 in 2014 to 40.0% in 2019; P = 0.29). (Table 1). The proportions of PCP cases admitted to the ICU did not significantly differ across various categories of immunosuppression aside from HIV infection (see Table 1).
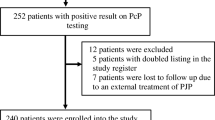
PCP cases admitted to the ICU over the period 2013–2019
Over the 2013–2019 period, 4,055 adult patients had a diagnosis of PCP and were admitted to an ICU during their hospital stay. They had a mean age of 60.8 (SD:14.6) years and 66.5% were male. There were 1,261 (31.1%) patients with HIV infection, who were significantly younger and were more frequently male than the non-HIV patients (Table 2). The incidence of severe PCP significantly increased from 0.85/100,000 in 2013 to 1.32/100,000 adult inhabitants in 2019 (P < 0.0001), a 55.3% percent rise related to the progression of cases in patients with other cause of immunosuppression than HIV infection. The proportion of patients without HIV infection significantly increased from 251/414 (60.6%) to 494/664 (74.4%) between 2013 and 2019 (P < 0.0001) (Fig. 1).
Chronic cardiac diseases, chronic respiratory diseases and diabetes were significantly more prevalent in HIV-negative patients than in patients with HIV infection (Table S1).
Hospital and intensive care unit mortality
The in-hospital mortality rate was 43.1% over the study period. It was significantly lower in patients with HIV infection (28.5%) than without (49.7%) (P < 0.0001) (Table 2). There was no significant change in in-hospital mortality between years, either in patients with or without HIV infection (P = 0.14 for both cohorts) (Fig. 2).
Among hospital decedents, 88.1% died in the ICU. Death rate in the ICU was 38.0% over the entire study period and did not change significantly between years (P = 0.48). Patients with HIV infection less often died in the ICU (25.0%) than patients without (43.8%) (P < 0.0001) (Table 2).
The severity of disease on admission to the ICU, as expressed by the SAPSII score, remained stable over the years (46.4 ± 16.5 in 2013 to 47.1 ± 16.4 in 2019; P = 0.44), and was not different between patients with and without HIV infection (P = 0.67).
In severe PCP cases not related to HIV infection, the hospital mortality was consistently 10 percentage points higher than the mortality predicted by the SAPSII score, while SAPSII consistently overestimated hospital mortality by 10 to 20 percentage points for patients with HIV infection (Figure S1).
Causes of immunosuppression
Among the 4,055 included patients, the percentage of HIV infection steadily and significantly declined from 2013 to 2019 and the percentage of solid organ cancer grew significantly (P < 0.001) to reach 24.2% in 2019. Meanwhile the proportion of autoimmune inflammatory diseases showed a significant rise only between 2018 and 2019 (P < 0.001), reaching 23.2% in 2019 (Fig. 3).
Over the study period, immunodeficiency in HIV-negative patients was caused by hematologic malignancies (38.9%), solid organ cancer (21.7%), autoimmune inflammatory diseases (19.9%), organ transplantation (12.3%), and idiopathic lung fibrosis (4.3%) (Table S2). Almost all types of hematologic malignancies were represented (Table S2).
Among the autoimmune inflammatory diseases recorded, rheumatoid arthritis, ulcerative colitis, Crohn's disease, psoriasis, and polymyalgia rheumatica affected 10.3% of patients. All other autoimmune inflammatory diseases, considered rare diseases, affected 13.2% of HIV-negative patients.
No cause of immunodeficiency was recorded for 286 patients, representing 7.1% of the overall population and 10.2% of patients without HIV infection. Among the later, chronic respiratory diseases (17.1% vs. 11.8%; P = 0.011) and cirrhosis (22.4% vs. 3.3%; P < 0.001) were significantly more prevalent than in patients with a recorded cause of immunodeficiency (Table 3).
Among HIV-positive patients, causes of immunodeficiency other than HIV infection were not infrequent (Table S2).
Factors associated with in-hospital mortality
The final logistic model retained to identify predictors of in-hospital death was constructed on a population of 4052 patients instead of 4055, because 3 patients (< 0.1%) had no SAPS II value recorded, which we did not replace. The model had a discriminative power as assessed by the AUCROC of 0.80 (95CI: 0.78–0.81) and was well calibrated (Figure S2).
Patient’s age (OR: 1.15 [95CI: 1.12–1.19]; per 1-yr increase), SAPSII score (OR: 1.04 [95CI: 1.03–1.04]; per 1-point increase) on admission to the ICU, and the number of hospital wards in which the patient stayed before being admitted to the ICU (OR: 1.19 [95CI: 1.12–1.27]) were associated with an increased risk of death (Table 4).
In contrast with the above unadjusted analysis, the risk of in-hospital death, when adjusted for all other covariables, has decreased significantly over time (OR: 0.94 [95CI: 0.91–0.98]; for each year after 2013).
The comorbidities with the strongest association with in-hospital mortality were congestive heart failure (OR: 23.17 [95CI: 8.34–64.38]), coagulopathy (OR: 9.98 [95CI: 3.90–25.54]), solid organ neoplasm (with or without metastasis) (OR: 6.56 [95CI: 2.55–16.86]), and cirrhosis (OR: 3.30 [95CI: 2.20–4.95]).
Patients with HIV infection had a lower adjusted risk of death than patients without HIV infection (OR: 0.30 [95CI: 0.17–0.55]).
In the entire study population, hematologic malignancies were found to be associated with a reduced risk of death (OR: 0.44 [95CI: 0.25–0.77]) and to interact with the presence of HIV infection (Table 4). This association was primarily driven by the larger subset of patients without HIV infection. In contrast, patients with HIV infection who also had hematologic malignancy had a higher risk of death (see interaction plot in Figure S3).
There was a strong interaction between age and congestive heart failure (Table 4), whereby the presence of congestive heart failure placed patients at a high risk of death of roughly 40–60% irrespective of age, while in patients without congestive heart failure, the risk of death grew in parallel with age (Figure S4). Somewhat similar interactions were found between the presence of coagulopathy and age (Figure S5) and between the presence of solid organ cancer and age (Figure S6).
Septic shock was the only acute condition present at ICU admission to be retained in the logistic model as associated with in-hospital mortality (OR: 1.56 [95CI: 1.01–2.41]).
Discussion
In France, there was an increase in the number of hospitalized cases of PCP over the study period, observed in both overall PCP cases from 2014 to 2019 and in those admitted to the ICU between 2013 and 2019. This rise was attributed to the consistent increase in the incidence of the disease among HIV-negative patients and an increase in the proportion of PCP cases in patients with HIV infection necessitating ICU admission.
In patients admitted to the ICU, the in-hospital mortality rate was high (43.1%) and remained stable throughout the study period. HIV-infected patients had a lower mortality rate compared to non-HIV-infected patients.
In patients admitted to the ICU, the risk of in-hospital death was associated with the patients’ age and disease severity at ICU admission, but also with coexisting comorbidities, such as congestive heart failure, solid organ cancer, and cirrhosis. This study identified a vast array of autoimmune inflammatory diseases as the cause of immunodeficiency.
Our finding of an overall increased incidence of PCP cases aligns with other recent epidemiological studies conducted at the national level in England, Germany, Spain, and Norway [25,26,27,28].
We noted a significant increase in the proportion of patients hospitalized in the ICU in parallel with the year of admission, rising from 17.8 in 2014 to 21.3% in 2019. These percentages are lower than in a French study conducted in the 1990’s where half of the hospitalized patients with PCP required ICU admission [29], or the ICU admission rate of 36.6% reported in another French study conducted from 2007 to 2010 [30]. More recently, a German study reported an ICU admission rate of 44% [26]. Discrepancies in these rates may be attributed to changes in the general care approach to PCP cases over the years in France, as well as differing admission policies across countries. In any case, the increase in ICU admissions of patients with PCP still imposes a significant burden on the French healthcare system.
A high mortality rate was observed among adult patients with severe PCP, which was found to be higher in HIV-negative patients (49.7%) compared to those with HIV infection (28.5%). This finding was consistent with some small, retrospective studies that focused on PCP in the ICU. For instance, one study conducted in France during the late 1990s and early 2000s reported an ICU mortality rate of 29% for all PCPs, with higher rates observed in HIV-negative patients (48%) than in patients with HIV infection (17%) [31]. Another study conducted in the US during the same period reported in-hospital mortality of 67% for 30 HIV-negative patients [32]. In 2013, a study combining three small retrospective cohorts from the same period found an in-hospital mortality rate of 25% for HIV-negative patients with PCP [33]. In the largest, more recent retrospective study that included 554 patients with PCP, regardless of ICU admission, the in-hospital mortality was 4% in patient with HIV infection and 27% without [30]. Currently, there is no available recent data on hospital mortality rates for patients with PCP admitted to the ICU.
Our findings confirm that severe PCP nowadays affects more HIV-negative patients than patients with HIV infection, particularly cancer patients [12,13,14, 34]. HIV-negative patients had a higher in-hospital mortality rate compared to HIV-positive patients with PCP. This observation is consistent with other studies that have examined hospital outcomes of all PCP patients admitted, regardless of ICU status [1, 30, 31, 34, 35]. Notwithstanding the fact that immunodeficiency in HIV-negative patients was primarily due to hematologic or solid organ malignancies, worse outcome in these patients may also be ascribed to severe comorbidities like chronic cardiac and respiratory diseases that were more prevalent than in patients with HIV infection (see Table S1). It is important to note that the predominant proportion of HIV-negative patients among severe PCP cases should not obscure the fact that the number of severe PCP cases in patients with HIV infection remains stable (Fig. 1), highlighting the ongoing HIV epidemic as a continuing major public health concern.
The most common immunocompromising condition observed in our cohort of severe PCP patients was hematologic malignancies, which is consistent with findings in hospitalized patients with PCP in general [36]. It is worth noting that almost all types of hematologic malignancies were present, including acute and chronic myeloid leukemias, which accounted for 44% of hematologic malignancies in HIV-negative patients (Table S2). As also observed in many studies [1, 25,26,27], solid organ cancer was the second most prevalent underlying condition in our population.
Autoimmune inflammatory diseases accounted for approximately 20% of the underlying conditions associated with severe PCP in HIV-negative patients. This proportion has exhibited a steady rise in several studies conducted over the last two decades [12, 28, 30, 34, 35]. This group of conditions encompasses a diverse set of rare diseases that often require immunosuppressive or immunomodulatory therapy. However, recommendations for PCP prophylaxis have been scarce, were only recently established [37,38,39], and are subject to debate [40], in contrast to the well-established guidelines for hematologic or solid organ malignancies and transplant recipients [41,42,43,44,45,46,47]. These findings collectively suggest a need for more systematic consideration of PCP antibiotic prophylaxis in these patient populations.
For 4.3% of HIV-negative patients, idiopathic lung fibrosis, which is a rare disease [48], was the sole condition that may make them more susceptible to PCP. Although it does not strictly weaken the immune system, it frequently necessitates the use of immunosuppressive treatment, such as high-dose corticosteroids. Some researchers also have recognized idiopathic lung fibrosis as an independent risk factor for PCP [35, 49,50,51] and as a risk factor for death from PCP [52] as observed in the present study (Table 4).
Our cohort of severe PCP cases comprised 7.1% patients with no identified cause of immunodeficiency. This proportion was less than that observed in recent Spanish (14.5%) and German (16.8%) nationwide studies also based on coding data [26, 27]. Although this proportion may still have been due to imperfect coding, it is noteworthy that patients with no identified cause of immunodeficiency suffered more frequently from chronic respiratory diseases or cirrhosis. These two conditions might be added to the list of conditions predisposing to PCP, as already suggested by others [53, 54].
This study has some limitations. First, the data relied on ICD-10 codes and administrative records, which may have resulted in inaccuracies when estimating the incidence and proportions of specific diseases. While this limitation typically has minimal impact on the outcomes of population-based studies [55], we cannot dismiss the possibility of such inaccuracies. For instance, as shown in Table S2, we observed 65 cases of PCP in patients with solid organ cancer and HIV infection, whereas such occurrences were considerably less frequent in a prospective cohort analysis conducted across 23 French hospitals over a 14-year period [56]. Second, the study did not provide details about the ICU procedures employed, such as mechanical ventilation, renal replacement therapy, or vasopressor use. However, this did not affect the estimation of in-hospital mortality. Third, the data did not allow for the calculation of the proportion of patients who received antibiotic prophylaxis for PCP, precluding an estimation of how the prophylaxis guidelines were followed. Fourth, the study, like other nationwide studies based on administrative records, did not have information about the type of sampling and laboratory test used for the diagnosis of PCP. Since the 2000s, PCR testing on respiratory samples has become increasingly utilized for diagnosing PCP [28]. However, while PCR is highly sensitive in detecting P. jirovecii, its specificity in confirming PCP rather than colonization in patients without HIV infection is suboptimal [57]. Large-scale prospective data are lacking to determine the proportion of true, confirmed PCP cases among all instances reported as such, both in ICUs and in the general hospitalized patient population. Hence, our finding that the incidence of PCP is increasing in non-HIV patients, while aligning with most recent epidemiological studies conducted at the national level in developed countries [25,26,27,28], warrants careful consideration until large-scale prospective studies are undertaken. Fifth, despite being recent, our data did not extend to the years 2020, 2021 and 2022. This was a deliberate decision because in many French hospitals, units administering intensive care were variable in size, location, and target population during the COVID-19 pandemic. Such variability had the potential to distort administrative data and affect ICU admission policies for patients with respiratory issues unrelated to COVID-19.
Conclusions
There is a rise in the number of severe PCP cases requiring ICU admission in France. The mortality rate is high for these patients, especially those without HIV-related PCP. One in five patients had an underlying autoimmune inflammatory disease, suggesting a need for systematic consideration of PCP antibiotic prophylaxis in these patients.
Availability of data and materials
The authors are not authorized by French law to export data extracted and analyzed within the secure ATIH platform to other sites. ATIH is the only party that can authorize data sharing with users they have not already authorized. All requests for data access must therefore be addressed directly to ATIH (https://www.atih.sante.fr/nous-contacter).
Abbreviations
- ABE:
-
Augmented backward elimination
- ATIH:
-
Agence technique de l’information sur l’hospitalisation
- CNIL:
-
Commission Nationale Informatique et Liberté
- COPD:
-
Chronic obstructive pulmonary disease
- HIV:
-
Human immunodeficiency virus
- ICD-10:
-
Tenth revision of the International Classification of Diseases
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- PCP:
-
Pneumocystis jirovecii Pneumonia
- PMSI:
-
Programme de médicalisation des systèmes d’information
- SAPS II:
-
Simplified Acute Physiology Score II
References
Sokulska M, Kicia M, Wesołowska M, Hendrich AB. Pneumocystis jirovecii—from a commensal to pathogen: clinical and diagnostic review. Parasitol Res. 2015;114(10):3577–85. https://doi.org/10.1007/s00436-015-4678-6.
Gormsen H. On interstitial plasma cell pneumonia in infants. Acta Paediatr (Stockh). 1950;39(4–5):291–314. https://doi.org/10.1111/j.1651-2227.1950.tb08530.x.
Walther T. Interstitial plasma cell pneumonia; report of 2 cases. Acta Paediatr (Stockh). 1950;39(6):545–53. https://doi.org/10.1111/j.1651-2227.1950.tb08550.x.
Vanek J. Parasitic pneumonia caused by Pneumocystis carinii in a 60-year-old woman. Cas Lek Cesk. 1952;91(44):1260–2.
Nouza M. Pneumocystis carinii pneumonia after 40 years. Infection. 1992;20(3):113–7. https://doi.org/10.1007/BF01704594.
Morris A, Lundgren JD, Masur H, Walzer PD, Hanson DL, Frederick T, Huang L, Beard CB, Kaplan JE. Current epidemiology of Pneumocystis pneumonia. Emerg Infect Dis. 2004;10(10):1713–20. https://doi.org/10.3201/eid1010.030985.
Fischl MA, Dickinson GM, La Voie L. Safety and efficacy of sulfamethoxazole and trimethoprim chemoprophylaxis for Pneumocystis carinii pneumonia in AIDS. JAMA. 1988;259(8):1185–9. https://doi.org/10.1001/jama.259.8.1185.
Kaplan JE, Hanson D, Dworkin MS, Frederick T, Bertolli J, Lindegren ML, Holmberg S, Jones JL. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clin Infect Dis. 2000;30(Suppl 1):S5-14. https://doi.org/10.1086/313843.
Elango K, Mudgal M, Murthi S, Yella PR, Nagrecha S, Srinivasan V, Sekar V, Koshy M, Ramalingam S, Gunasekaran K. Trends in the epidemiology and outcomes of pneumocystis pneumonia among human immunodeficiency virus (HIV) hospitalizations. Int J Environ Res Public Health. 2022;19(5):2768. https://doi.org/10.3390/ijerph19052768.
Kovacs JA, Masur H. Evolving health effects of Pneumocystis: one hundred years of progress in diagnosis and treatment. JAMA. 2009;301(24):2578–85. https://doi.org/10.1001/jama.2009.880.
Antiretroviral Therapy Cohort Collaboration (ART-CC), Mocroft A, Sterne JA, Egger M, May M, Grabar S, Furrer H, Sabin C, Fatkenheuer G, Justice A, Reiss P, d'Arminio Monforte A, Gill J, Hogg R, Bonnet F, Kitahata M, Staszewski S, Casabona J, Harris R, Saag M. Variable impact on mortality of AIDS-defining events diagnosed during combination antiretroviral therapy: not all AIDS- defining conditions are created equal. Clin Infect Dis. 2009;48(8):1138–51. https://doi.org/10.1086/597468.
Maini R, Henderson KL, Sheridan EA, Lamagni T, Nichols G, Delpech V, et al. Increasing Pneumocystis pneumonia, England, UK, 2000–2010. Emerg Infect Dis. 2013;19(3):386–92. https://doi.org/10.3201/eid1903.121151.
Patterson L, Coyle P, Curran T, Verlander NQ, Johnston J. Changing epidemiology of Pneumocystis pneumonia, Northern Ireland, UK and implications for prevention, 1 July 2011-31 July 2012. J Med Microbiol. 2017;66(11):1650–5. https://doi.org/10.1099/jmm.0.000617.
White PL, Price JS, Backx M. Pneumocystis jirovecii pneumonia: epidemiology, clinical manifestation and diagnosis. Curr Fungal Infect Rep. 2019;13:260–73. https://doi.org/10.1007/s12281-019-00349-3.
Bongomin F, Gago S, Oladele RO, Denning DW. Global and multi-national prevalence of fungal diseases-estimate precision. J Fungi (Basel). 2017;3(4):57. https://doi.org/10.3390/jof3040057.
Di Pasquale MF, Sotgiu G, Gramegna A, Radovanovic D, Terraneo S, Reyes LF, Rupp J, González Del Castillo J, Blasi F, Aliberti S, Restrepo MI, GLIMP Investigators. Prevalence and etiology of community-acquired pneumonia in immunocompromised patients. Clin Infect Dis. 2019;68(9):1482–93. https://doi.org/10.1093/cid/ciy723.
Schwartz B, Dupont V, Dury S, Carsin-Vu A, Guillard T, Caillard S, Frimat L, Sanchez S, Schvartz B, Bani-Sadr F, Jolly D, Rieu P, Goury A. Aetiology, clinical features, diagnostic studies, and outcomes of community-acquired pneumonia in kidney transplant recipients admitted to hospital: a multicentre retrospective French cohort study. Clin Microbiol Infect. 2023;29(4):542.e1-542.e5. https://doi.org/10.1016/j.cmi.2022.12.014.
Schmajuk G, Jafri K, Evans M, Shiboski S, Gianfrancesco M, Izadi Z, Patterson SL, Aggarwal I, Sarkar U, Dudley RA, Yazdany J. Pneumocystis jirovecii pneumonia (PJP) prophylaxis patterns among patients with rheumatic diseases receiving high-risk immunosuppressant drugs. Semin Arthritis Rheum. 2019;48(6):1087–92. https://doi.org/10.1016/j.semarthrit.2018.10.018.
Redjoul R, Robin C, Foulet F, Leclerc M, Beckerich F, Cabanne L, di Blasi R, Pautas C, Toma A, Botterel F, Maury S, Cordonnier C. Pneumocystis jirovecii pneumonia prophylaxis in allogeneic hematopoietic cell transplant recipients: can we always follow the guidelines? Bone Marrow Transplant. 2019;54(7):1082–8. https://doi.org/10.1038/s41409-018-0391-2.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplifed Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42(4):355–60. https://doi.org/10.1097/01.mlr.0000118861.56848.ee.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sørensen HT, von Elm E, Langan SM, RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10): e1001885. https://doi.org/10.1371/journal.pmed.1001885.
Dunkler D, Plischke M, Leffondré K, Heinze G. Augmented backward elimination: a pragmatic and purposeful way to develop statistical models. PLoS ONE. 2014;9(11): e113677. https://doi.org/10.1371/journal.pone.0113677.
Heinze G, Wallisch C, Dunkler D. Variable selection—a review and recommendations for the practicing statistician. Biom J. 2018;60(3):431–49. https://doi.org/10.1002/bimj.201700067.
Pates K, Periselneris J, Russell MD, Mehra V, Schelenz S, Galloway JB. Rising incidence of Pneumocystis pneumonia: a population-level descriptive ecological study in England. J Infect. 2023. https://doi.org/10.1016/j.jinf.2023.02.014.
Kolbrink B, Scheikholeslami-Sabzewari J, Borzikowsky C, von Samson-Himmelstjerna FA, Ullmann AJ, Kunzendorf U, Schulte K. Evolving epidemiology of pneumocystis pneumonia: Findings from a longitudinal population-based study and a retrospective multi-center study in Germany. Lancet Reg Health Eur. 2022;15(18): 100400. https://doi.org/10.1016/j.lanepe.2022.100400.
Pereira-Diaz E, Moreno-Verdejo F, de la Horra C, Guerrero JA, Calderon EJ, Medrano FJ. Changing trends in the epidemiology and risk factors of pneumocystis pneumonia in Spain. Front Public Health. 2019;7:275.
Grønseth S, Rogne T, Hannula R, Åsvold BO, Afset JE, Damås JK. Epidemiological and clinical characteristics of immunocompromised patients infected with Pneumocystis jirovecii in a twelve-year retrospective study from Norway. BMC Infect Dis. 2021;21:659. https://doi.org/10.1186/s12879-021-06144-1.
Roblot F, Godet C, Le Moal G, Garo B, Faouzi Souala M, Dary M, De Gentile L, Gandji JA, Guimard Y, Lacroix C, Roblot P, Becq-Giraudon B. Analysis of underlying diseases and prognosis factors associated with Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2002;21(7):523–31. https://doi.org/10.1007/s10096-002-0758-5.
Roux A, Canet E, Valade S, Gangneux-Robert F, Hamane S, Lafabrie A, Maubon D, Debourgogne A, Le Gal S, Dalle F, Leterrier M, Toubas D, Pomares C, Bellanger AP, Bonhomme J, Berry A, Durand-Joly I, Magne D, Pons D, Hennequin C, Maury E, Roux P, Azoulay É. Pneumocystis jirovecii pneumonia in patients with or without AIDS. France Emerg Infect Dis. 2014;20(9):1490–7. https://doi.org/10.3201/eid2009.131668.
Monnet X, Vidal-Petiot E, Osman D, Hamzaoui O, Durrbach A, Goujard C, Miceli C, Bourée P, Richard C. Critical care management and outcome of severe Pneumocystis pneumonia in patients with and without HIV infection (Erratum in: Crit Care. 2009;13(2)407). Crit Care. 2008;12(1):R28. https://doi.org/10.1186/cc6806.
Festic E, Gajic O, Limper AH, Aksamit TR. Acute respiratory failure due to pneumocystis pneumonia in patients without human immunodeficiency virus infection: outcome and associated features. Chest. 2005;128(2):573–9. https://doi.org/10.1378/chest.128.2.573.
Lemiale V, Debrumetz A, Delannoy A, Alberti C, Azoulay E. Adjunctive steroid in HIV-negative patients with severe Pneumocystis pneumonia. Respir Res. 2013;14(1):87. https://doi.org/10.1186/1465-9921-14-87.
Cillóniz C, Dominedò C, Álvarez-Martínez MJ, Moreno A, García F, Torres A, Miro JM. Pneumocystis pneumonia in the twenty-first century: HIV-infected versus HIV-uninfected patients. Expert Rev Anti Infect Ther. 2019;17(10):787–801. https://doi.org/10.1080/14787210.2019.1671823.
Bienvenu AL, Traore K, Plekhanova I, Bouchrik M, Bossard C, Picot S. Pneumocystis pneumonia suspected cases in 604 non-HIV and HIV patients. Int J Infect Dis. 2016;46:11–7. https://doi.org/10.1016/j.ijid.2016.03.018.
Fillatre P, Decaux O, Jouneau S, Revest M, Gacouin A, Robert-Gangneux F, Fresnel A, Guiguen C, Le Tulzo Y, Jégo P, Tattevin P. Incidence of Pneumocystis jiroveci pneumonia among groups at risk in HIV-negative patients. Am J Med. 2014;127(12):1242.e11-7. https://doi.org/10.1016/j.amjmed.2014.07.010.
Braga BP, Prieto-González S, Hernández-Rodríguez J. Pneumocystis jirovecii pneumonia prophylaxis in immunocompromised patients with systemic autoimmune diseases. Med Clin (Barc). 2019;152(12):502–7. https://doi.org/10.1016/j.medcli.2019.01.010. (English, Spanish).
Wolfe RM, Beekmann SE, Polgreen PM, Winthrop KL, Peacock JE Jr. Practice patterns of pneumocystis pneumonia prophylaxis in connective tissue diseases: a survey of infectious disease physicians. Open Forum Infect Dis. 2019;6(9):ofz315. https://doi.org/10.1093/ofid/ofz315.
Rúa-Figueroa Fernández de Larrinoa Í, Carreira PE, Brito García N, Díaz Del Campo Fontecha P, Pego Reigosa JM, Gómez Puerta JA, Ortega-Castro R, Tejera Segura B, Aguado García JM, Torre-Cisneros J, Valencia-Martín JL, Pereda CA, Nishishinya-Aquino MB, Otón Sánchez MT, Silva Fernández L, Maese Manzano J, Chamizo Carmona E, Correyero Plaza M. Recommendations for prevention of infection in systemic autoimmune rheumatic diseases. Reumatol Clin (Engl Ed). 2022;18(6):317–330. https://doi.org/10.1016/j.reumae.2021.04.003.
Pereda CA, Nishishinya-Aquino MB, Brito-García N, Del Campo D, Fontecha P, Rua-Figueroa I. Is cotrimoxazole prophylaxis against Pneumocystis jirovecii pneumonia needed in patients with systemic autoimmune rheumatic diseases requiring immunosuppressive therapies? Rheumatol Int. 2021;41(8):1419–27. https://doi.org/10.1007/s00296-021-04808-4.
Christopeit M, Schmidt-Hieber M, Sprute R, Buchheidt D, Hentrich M, Karthaus M, Penack O, Ruhnke M, Weissinger F, Cornely OA, Maschmeyer G. Prophylaxis, diagnosis and therapy of infections in patients undergoing high-dose chemotherapy and autologous haematopoietic stem cell transplantation. 2020 update of the recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Hematol. 2021;100(2):321–36. https://doi.org/10.1007/s00277-020-04297-8.
Cooley L, Dendle C, Wolf J, Teh BW, Chen SC, Boutlis C, Thursky KA. Consensus guidelines for diagnosis, prophylaxis and management of Pneumocystis jirovecii pneumonia in patients with haematological and solid malignancies, 2014. Intern Med J. 2014;44(12b):1350–63. https://doi.org/10.1111/imj.12599.
Fishman JA, Gans H, AST Infectious Diseases Community of Practice. Pneumocystis jiroveci in solid organ transplantation: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33: e13587.
Classen AY, Henze L, von Lilienfeld-Toal M, Maschmeyer G, Sandherr M, Graeff LD, Alakel N, Christopeit M, Krause SW, Mayer K, Neumann S, Cornely OA, Penack O, Weißinger F, Wolf HH, Vehreschild JJ. Primary prophylaxis of bacterial infections and Pneumocystis jirovecii pneumonia in patients with hematologic malignancies and solid tumors: 2020 updated guidelines of the Infectious Diseases Working Party of the German Society of Hematology and Medical Oncology (AGIHO/DGHO). Ann Hematol. 2021;100(6):1603–20. https://doi.org/10.1007/s00277-021-04452-9.
Olson AL, Politikos I, Brunstein C, Milano F, Barker J, Hill JA, American Society for Transplantation and Cellular Therapy Cord Blood Special Interest Group. Guidelines for infection prophylaxis, monitoring and therapy in cord blood transplantation. Transplant Cell Ther. 2021;27(5):359–62. https://doi.org/10.1016/j.jtct.2021.01.024.
Yakoub-Agha I, Chabannon C, Bader P, Basak GW, Bonig H, Ciceri F, Corbacioglu S, Duarte RF, Einsele H, Hudecek M, Kersten MJ, Köhl U, Kuball J, Mielke S, Mohty M, Murray J, Nagler A, Robinson S, Saccardi R, Sanchez-Guijo F, Snowden JA, Srour M, Styczynski J, Urbano-Ispizua A, Hayden PJ, Kröger N. Management of adults and children undergoing chimeric antigen receptor T-cell therapy: best practice recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE). Haematologica. 2020;105(2):297–316. https://doi.org/10.3324/haematol.2019.229781.
Paul F, Vicente C, Courbon C, Moreau AS, Picard M, Pochon C, Sterin A, Tudesq JJ, Yakoub-Agha M, Bay JO, Yakoub-Agha I. Prise en charge prophylactique, thérapeutique des complications infectieuses et vaccination des patients traités par CAR-T cells : recommandations de la Société francophone de greffe de moelle et de thérapie cellulaire (SFGM-TC) [Prevention and management of infections in patients undergoing CAR T-cell therapy: Recommendations of the Francophone Society of Bone Marrow Transplantation and Cellular Therapy (SFGM-TC)]. Bull Cancer. 2021;108(12S):S90–7. https://doi.org/10.1016/j.bulcan.2021.11.001. (in French).
Cottin V, Bonniaud P, Cadranel J, Crestani B, Jouneau S, Marchand-Adam S, Nunes H, Wémeau-Stervinou L, Bergot E, Blanchard E, Borie R, Bourdin A, Chenivesse C, Clément A, Gomez E, Gondouin A, Hirschi S, Lebargy F, Marquette CH, Montani D, Prévot G, Quetant S, Reynaud-Gaubert M, Salaun M, Sanchez O, Trumbic B, Berkani K, Brillet PY, Campana M, Chalabreysse L, Chatté G, Debieuvre D, Ferretti G, Fourrier JM, Just N, Kambouchner M, Legrand B, Le Guillou F, Lhuillier JP, Mehdaoui A, Naccache JM, Paganon C, Rémy-Jardin M, Si-Mohamed S, Terrioux P. French practical guidelines for the diagnosis and management of idiopathic pulmonary fibrosis—2021 update. Full-length version. Respir Med Res. 2022;4(83): 100948. https://doi.org/10.1016/j.resmer.2022.100948.
Shimizu Y, Sunaga N, Dobashi K, et al. Serum markers in interstitial pneumonia with and without Pneumocystis jirovecii colonization: a prospective study. BMC Infect Dis. 2009;22:47.
Kim TO, Lee JK, Kwon YS, Kim YI, Lim SC, Kim MS, Kho BG, Park CK, Oh IJ, Kim YC, Park HY, Shin HJ. Clinical characteristics and prognosis of patients with Pneumocystis jirovecii pneumonia without a compromised illness. PLoS ONE. 2021;16(2): e0246296. https://doi.org/10.1371/journal.pone.0246296.
Sun Y, Shao C, Huang H, Chen R, Xu K, Li M, Zhang X, Xu Z. Prognostic analysis of Pneumocystis Jirovecii pneumonia in interstitial lung disease patients: a retrospective clinical study. Diagnostics (Basel). 2022;12(12):2925. https://doi.org/10.3390/diagnostics12122925.
Hamada S, Ichiyasu H, Inaba M, Takahashi H, Sadamatsu T, Akaike K, Masunaga A, Tashiro Y, Hirata N, Yoshinaga T, et al. Prognostic impact of pre-existing interstitial lung disease in non-HIV patients with Pneumocystis pneumonia. ERJ Open Res. 2020;6:00306–2019.
Calderón EJ, Regordan C, Medrano FJ, Ollero M, Varela JM. Pneumocystis carinii infection in patients with chronic bronchial disease. Lancet. 1996;347:977.
Franceschini E, Dolci G, Santoro A, Meschiari M, Riccò A, Menozzi M, Burastero GJ, Cuffari B, De Maria N, Serio L, Biagioni E, Catellani B, Sandro SD, Colecchia A, Girardis M, Benedetto FD, Mussini C. Pneumocystis jirovecii pneumonia in patients with decompensated cirrhosis: a case series. Int J Infect Dis. 2023;128:254–6. https://doi.org/10.1016/j.ijid.2022.12.027.
Henderson T, Shepheard J, Sundararajan V. Quality of diagnosis and procedure coding in ICD-10 administrative data. Med Care. 2006;44(11):1011–9. https://doi.org/10.1097/01.mlr.0000228018.48783.34.
Pansu N, Le Moing V, Poizot-Martin I, Joly V, Allavena C, Hocqueloux L, Duvivier C, Lourenco J, Jovelin T, Reynes J, Makinson A. Pneumocystis jirovecii Pneumonia and Toxoplasmosis in PWH with HIV-controlled disease treated for solid malignancies: a DAT’AIDS study. Open Forum Infect Dis. 2022;9:109. https://doi.org/10.1093/ofid/ofac109.
Giacobbe DR, et al; JIR-ICU investigators (collaborators); Critically Ill Patients Study Group of the European Society of Clinical Microbiology and Infectious Diseases (ESGCIP), and the Fungal Infection Study Group of the European Society of Clinical Microbiology and Infectious Diseases (EFISG). Pneumocystis Jirovecii pneumonia in intensive care units: a multicenter study by ESGCIP and EFISG. Crit Care. 2023;27:323. https://doi.org/10.1186/s13054-023-04608-1.
Acknowledgements
The authors sincerely thank Drs Sixtine Brabant (MD) and Antoine Valéry (MD) from the department of Medical Information of the Centre Hospitalier Universitaire d’Orléans, for their help in obtaining access authorization to the national PMSI database.
Funding
Financial support was provided only by the Centre Hospitalier Universitaire d’Orléans, France. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval.
Author information
Authors and Affiliations
Contributions
Drs Kamel and Boulain had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Kamel and Boulain, Acquisition, analysis, or interpretation of data: Kamel and Boulain. Drafting of the manuscript: Kamel and Boulain, Critical revision of the manuscript for important intellectual content: Kamel and Boulain, Statistical analysis: Boulain. Administrative, technical, or material support: Kamel, Boulain, Supervision: Kamel, Boulain.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the French Intensive Care Society Ethical Committee number CE SRLF 23-031.
Consent for publication
Not applicable.
Competing interests
The authors declare that they do not have any financial, academic, or personal competing interest related to the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kamel, T., Boulain, T. Pneumocystis pneumonia in French intensive care units in 2013–2019: mortality and immunocompromised conditions. Ann. Intensive Care 14, 80 (2024). https://doi.org/10.1186/s13613-024-01309-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01309-y