Abstract
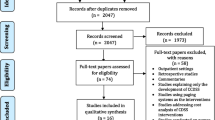
Healthcare expenses are increasing, as is the utilization of laboratory resources. Despite this, between 20% and 40% of requested tests are deemed inappropriate. Improper use of laboratory resources leads to unwanted consequences such as hospital-acquired anemia, infections, increased costs, staff workload and patient stress and discomfort. The most unfavorable consequences result from unnecessary follow-up tests and treatments (overuse) and missed or delayed diagnoses (underuse). In this context, several interventions have been carried out to improve the appropriateness of laboratory testing. To date, there have been few published assessments of interventions specific to the intensive care unit. We reviewed the literature for interventions implemented in the ICU to improve the appropriateness of laboratory testing. We searched literature from 2008 to 2023 in PubMed, Embase, Scopus, and Google Scholar databases between April and June 2023. Five intervention categories were identified: education and guidance (E&G), audit and feedback, gatekeeping, computerized physician order entry (including reshaping of ordering panels), and multifaceted interventions (MFI). We included a sixth category exploring the potential role of artificial intelligence and machine learning (AI/ML)-based assisting tools in such interventions. E&G-based interventions and MFI are the most frequently used approaches. MFI is the most effective type of intervention, and shows the strongest persistence of effect over time. AI/ML-based tools may offer valuable assistance to the improvement of appropriate laboratory testing in the near future. Patient safety outcomes are not impaired by interventions to reduce inappropriate testing. The literature focuses mainly on reducing overuse of laboratory tests, with only one intervention mentioning underuse. We highlight an overall poor quality of methodological design and reporting and argue for standardization of intervention methods. Collaboration between clinicians and laboratory staff is key to improve appropriate laboratory utilization. This article offers practical guidance for optimizing the effectiveness of an intervention protocol designed to limit inappropriate use of laboratory resources.
Similar content being viewed by others
Background
Healthcare spending is increasing in the US and Europe, faster than economic growth [1, 2]. The use of clinical laboratory tests has also increased, due in part to greater accessibility and affordability [3, 4]. Despite accounting for a small proportion of healthcare expenses, clinical laboratories are involved in the majority of medical decisions, making them central players in healthcare [5,6,7]. However, there is indication of inappropriate use of laboratory resources, with 20% to 40% of overall tests deemed inappropriate [8, 9], and with estimates as high as 60% of coagulation tests and 70% of chemistry tests considered of doubtful clinical significance [10]. Overuse can cause hospital acquired-anemia and subsequent need for transfusion, increased costs, staff overload, patient discomfort and stress, incidental findings, additional unnecessary interventions, and infections (e.g., central line-associated bloodstream infection), whereas underuse can lead to missed or delayed diagnosis [8, 10,11,12,13,14,15,16]. Several techniques can reduce the volume of blood drawn for laboratory testing. These include utilizing small-volume tubes [17, 18], non-invasive measures, and residual blood from previous samples [19]. In a wider context, interventions could be conducted to improve the appropriateness of laboratory testing and ordering.
Multiple reviews have assessed the published literature of interventions led in non-intensive care units (ICU) wards and among primary care physicians [3, 4, 11, 20,21,22,23,24,25,26,27,28,29,30,31,32,33]. However, there are few published assessments of ICU-specific interventions to date. Of note, two systematic reviews have been previously published. The first, from Foster et al. [34], reviewed audit and feedback interventions to improve laboratory test and transfusion practice from inception to 2016, but did not evaluate other types of interventions. The second, from Hooper et al. [35], evaluated safety and efficacy of routine diagnostic tests (including mixed laboratory tests and radiographs ordering data) reduction in the ICU between 1993 and 2018, with a subsequent meta-analysis of costs savings. Based on our knowledge, there are no other reviews focusing on laboratory tests in the ICU for all types of interventions. Furthermore, artificial intelligence and machine learning (AI/ML) assisting tools are destined to be increasingly used in laboratory medicine [36,37,38]. Mrazek et al. [4] reviewed several AI-centered studies of relevance for laboratory medicine as they call it “the next logical step” in the pursuit of appropriateness. No review has explored so far the role of AI/ML-based solutions in interventions to improve the appropriateness of laboratory use in the ICU to the best of our knowledge.
We hence decided to review the available literature on interventions to reduce inappropriate testing in the ICU. As well as evaluating their effectiveness and costs savings, we try here to provide an assessment of their feasibility and persistence over time. The complete methodology for this review can be found in Additional file 1.
Interventions to improve laboratory testing appropriateness in the ICU
Education and guidance
Education and/or guidance (E&G) is one of the most common approaches used to limit the number of inappropriate tests in ICU (Table 1) as in non-ICU wards [4, 11, 20, 32, 33, 39]. E&G account for more than 40% of all interventions, with evidence of good effectiveness [23]. This strategy has long been used to regulate prescription of laboratory tests [24], as well as in more recent ICU interventions [40,41,42,43,44,45,46,47,48,49,50,51], even if E&G is often associated with other strategies (Table 1).
Education can take various forms: formal sessions, staff meetings, peer group discussions, emails, flyers, posters, bedside reminders, content in the intranet, educational content on electronic devices such as tablets, etc. The fundamental purpose of an educational approach is to raise awareness of the need to change practice change towards more appropriate use of laboratory resources [52]. Educational strategies are frequently used because they are relatively accessible and inexpensive, can reach many people at once and generally fit within the logical framework of the intervention—the intervention is often explicitly explained to clinicians.
In the broadest sense, guidance for laboratory testing includes advice for clinicians on selecting the "right test, at the right time, for the right patient" [53]. In recent years, guidance has increasingly considered the principle that “less is more” [14, 54, 55], aiming to limit inappropriate tests. In France, there are national ICU guidelines on appropriateness of requesting laboratory tests and chest radiographs [56]. Guidance are developed with the assistance of (local) experts [41, 44, 50], following literature review [46], or a combination thereof [40, 42, 49, 51], or sometimes in response to an internal quality improvement study [46] (Table 2). Few interventions have used a guidance-based strategy alone. E&G-based interventions are effective, depending on the test (Table 1). They may even have relatively permanent effect over time [46].
Few studies have looked at education alone or as a main strategy [57,58,59,60]. Maguet et al. [58] achieved a sustained tests reduction of 7% per patient-day by providing daily information, indications for testing, prices information and reminders at the patient bedside. Similarly, Adhikari et al. [57] provided care staff with a feedback of an audit on prescription patterns, along with literature data, flyers, posters and formal education on appropriate prescription. Analyzing 153 records post-intervention, they reported an increase in appropriate prescription from 60 to 79% for full blood count (FBC). However, the effect was not statistically significant on basic metabolic panel (BMP) requests.
E&G strategies have several limitations. First, low-intensity education-based interventions are not effective enough to induce substantial change in prescribing behavior. Yorkgitis et al. [60] investigated the impact of a “gentle reminder” (i.e., the question “What laboratory tests are medically necessary for tomorrow?”) during morning round. The intervention had no significant effect on test reduction. Second, an important factor of success in education-based interventions is repetition, for example, weekly or daily [52, 58, 61]. This can prove difficult to maintain over time. A solution could involve the development of continuing education for young residents and rotating staff [20, 62], as required in ISO15189:2022 [63]. Third, there is significant heterogeneity in guidance and test(s) considered in the interventions we retrieved. The guidance was locally established and, as local behaviors vary widely between hospitals [64,65,66], practices also exhibit high variability between studies. Some guidelines focus on first-test indications, while others focus on retest indications. Some consider certain elements as always appropriate for routine testing, such as BMP and FBC [46], whereas others are tailored to a specific test [50] (Table 2). Finally, adherence is an issue in E&G-based interventions: sending emails, handing out flyers or hanging posters does not mean that they are being read, and if they are, it does not mean that their content is understood and applied. This challenge must encourage the realization of clear, pragmatic, and actionable educational content. Examples of educational protocols are shown in Table 1. Formal sessions, visual aids such as flyers and posters and emails are the most commonly used methods for education. If E&G is the only used strategy, it is recommended to expand the range of tools, including flyers, emails and sessions, as well as increase their frequency over time, e.g., with weekly or monthly repetitions, to maximize efficiency.
Audit and feedback
Audit and/or feedback (A&F) is an effective strategy to reduce inappropriate testing, especially when used in combination with other strategies [67]. The definition of A&F varies, but it typically involves an audit of tests requested, with feedback provided on the tests’ selection practice. A&F can be collective (i.e., anonymous) or individual, the latter being more efficient [34]. Foster et al. [34] systematically reviewed A&F-based interventions to improve laboratory test and transfusion ordering in the ICU, regardless of whether the strategy was used alone or integrated with others in a multifaceted study design. They documented that A&F was an efficient strategy to enhance appropriateness of testing, although the overall quality and methodology design was poor. By contrast, in one 81-patient controlled study [68], the impact of an intervention combining feedback (presence of an acute care nurse practitioner during multidisciplinary rounds to discuss next 24 h tests requests) and education (reminders on checklist, reminders on computers and at bedside) did not reach the threshold of statistical significance between intervention and control groups, suggesting that A&F-based interventions may be only moderately effective.
Rachakonda et al. [69] combined feedback from clinicians themselves with an educational approach, the latter consisting of monthly formal education on the relevance of testing and pricing information. They achieved a 12% reduction of total costs. The authors measured adherence to feedback by dividing the number of tests authorized the day before (during audit) by the real number of tests effectively requested. Compliance was low (51%), indicating that twice as many tests were requested as the previous day. Compliance to feedback is an interesting parameter to measure, and would be instructive to assess in interventional studies using A&F strategies. Likewise, safety outcomes and effect persistence over time are rarely measured [34], which can nevertheless provide interesting information.
Gatekeeping
Gatekeeping strategies refer to a constraint on the choice of laboratory tests, usually set by the central (reference) laboratory [11]. This strategy is, for example, used when the laboratory discontinues the possibility of scheduling routine daily tests, and instead imposes lab requests on a test-by-test, day-to-day basis [62].
Few intervention studies used this strategy alone in the ICU (Table 1). In a 48-bed setting, de Bie et al. [70] withdrew the daily routine panel (aPTT, INR/PT, blood urea nitrogen [BUN], serum chloride, sodium, albumin, and C-reactive protein [CRP]) and the additional weekly panel (AST, alanine transaminase [ALT], alkaline phosphatase [ALP], amylase, and total bilirubin). They also altered the post-cardiac surgery pre-made panel and the arterial blood gas (ABG) point-of-care testing (POCT) device panels. The total number of tests performed decreased by 24%, whereas the demand rate remained unchanged, thus suggesting that a blood test was indeed indicated in the clinical context, but that one test out of four had previously been inappropriately ordered. The most impacted tests were aPTT, INR/PT, albumin, BUN, serum calcium, chloride, and CRP. The removal of weekly panels had a moderate effect (−18%). Regarding post-cardiac surgery panels, the effect was moderate on creatine kinase isoenzyme MB (−10%) but significant on cardiac troponin (−50%). Finally, the study showed interesting results on ABG stewardship: potassium and glucose were performed in 90% of cases; pH, PO2, PCO2, hemoglobin and sodium were ordered in only 70–80% of analyses; chloride, ionized calcium and lactate were prescribed in only 30–40% of all ABGs.
Gatekeeping can also take the form of a self-imposed limitation set by the clinicians themselves. In a 191-patient study, Sugarman et al. [71] evaluated the adherence to a local standard on seven commonly performed tests (CRP, BUN and electrolytes, serum magnesium, phosphate, liver function tests (LFT), coagulation [not otherwise specified] and FBC), with a self-imposed limit of maximum 25% inappropriate tests. They managed to remain under the 25% limit for CRP, FBC, BUN and creatinine, but exceeded the threshold for LFT (51% of non-indicated tests), magnesium (42%), phosphate (42%) and coagulation tests (40%), ultimately estimating that a quarter of the total costs of the tests were due to inappropriate requests.
Certain gatekeeping principles can help in a more comprehensive strategy. For example, it may be appropriate to define a minimum retesting interval (MRI) for commonly prescribed tests. Tyrrell et al. [72] set a 72-h and 24-h MRI on LFT and bone profile respectively, leading to a 23% reduction in tests requested. Prescriptions of bone profile panel dropped by 76% during intervention, whereas prescriptions of calcium and albumin tests increased by 110%, suggesting that clinicians sometimes request an entire panel when only a few tests provide the same clinical information. The authors also compared MRI with a scheduled routine panel testing strategy (i.e., a predefined bundling of tests performed three times a week), along with continuous education and feedback by both clinicians and biochemistry staff. The results showed that scheduled routine panel testing is even more effective than MRI.
Computerized physician order entry
Interventions to reduce inappropriate testing can focus on computerized physician order entry (CPOE) systems. Reshaping of the electronic request form is a classic intervention that can be coupled with other strategies [73,74,75]. Alternatively, it takes the form of “prompts” which may appear when selecting a particular test [76,77,78,79], choosing a test with MRI [80], or requesting two tests which are redundant in terms of clinical information. Prompts can be set as an indication to the clinician, allowing to override the alert (“soft stop”) with or without needing a written reason for doing so, or can block the test prescription altogether (“hard stop”). Therefore, CPOE prompts can have a gatekeeping component in hard stops or an educational content in soft stops; they can also display indications for testing. For this reason, this category is rather transversal and generally associated with other strategies in MFI [73,74,75,76,77,78,79,80].
Notably, some interventions assessed the effectiveness of CPOE-based strategies alone. In a procalcitonin-specific study, Aloisio et al. [81] programmed the CPOE to display a notification when an 80% reduction in initial procalcitonin level had been reached. Procalcitonin is especially used in the ICU for diagnosing severe infection and/or antibiotic stewardship daily, at least until the level is significantly decreases. The authors noted that clinicians tended to mechanically continue testing procalcitonin beyond the threshold of clinically significant variation set at 80% reduction. Automatic notification helped reducing procalcitonin testing by 10%, saving EUR ~ 750 (2019) per bed-year.
CPOE alerts should be used with caution. Repeated alerts may gradually lead clinicians to ignore them, a phenomenon known as “alert fatigue” [82] which often results in alert overriding [83]. Conversely, fear of over-alerting can lead to under-alerting [84]. Therefore, it is important to ensure the right balance when deciding to use these CPOE alerts.
Multifaceted interventions
Multifaceted interventions (MFI) are studies, where multiples strategies are used concomitantly to manage inappropriate laboratory use. If MFI are considered a category of their own, it is one of the most widely used strategy (Table 1). Several large MFI have been conducted in the ICU, showing strong effectiveness (Table 1). Raad et al. [85] led an intervention based on education, gatekeeping and feedback in a 18-bed setting, and observed a one-third reduction of tests over a 9-month period, along with a reduction of POCT testing from 7 to 1 (−83%) test-patient-day and a decrease in the percentage of patients sampled daily from 100 to 12%. This led to an estimated savings of USD 123000 in direct and USD 258000 in indirect costs, with no increase in mortality or length of stay (LOS). Similarly, a study [74] on 3250 patients combined education, guidance, CPOE and feedback-based strategies on routine hematology (FBC), chemistry (BUN and creatinine, electrolytes, magnesium, phosphate, calcium, LFT) and coagulation (INR/PT, aPTT, fibrinogen), and achieved a 28% reduction in test ordered with a sustained 26% reduction over a year, estimating an overall USD 213000 and USD 175000 savings during intervention (6 months) and post-intervention (6 months) periods, respectively. They failed to observe an increase in mortality or LOS, or in morbidity (number of ventilated patients and hemoglobin levels). Merkeley et al. [78] designed a 1440-patient study with education on prices, gatekeeping and feedback, demonstrating a total reduction of FBC and electrolytes (not otherwise specified) tests, with a decrease in routine tests (−14% for FBC and -13% for electrolytes) compounded by an increase in non-routine (i.e., punctual) tests (+ 8% for FBC and + 6% for electrolytes), thus suggesting a less frequent use of “ready-made” panels. It led to a CAD 11200 annual saving with no additional adverse outcome. Clouzeau et al. [86] conducted a controlled, non-randomized study on 5707 patients (3315 intervention vs. 2392 control) with education, feedback and gatekeeping strategies, achieving a 59% reduction in tests ordered, sustained over a 1-year period, and leading to an annual EUR 500000 cost savings. Recently, Litton et al. [87] observed a reduction of 50,000 tests per year with an education, guidance, gatekeeping and feedback-based intervention. They estimated savings up to AUD 800000 per year (30-bed setting) and observed no impact on mortality and LOS. These data suggest that MFI can have lasting effects on the ordering of tests and lead to significant costs savings.
Several interventions are test-specific. Lo et al. [76, 77] assessed serum magnesium testing with educational, guidance and CPOE-based interventions. They educated rotating medical and nursing staff in conjunction with a CPOE prompt displaying indications for testing. Non-routine magnesium testing remained stable, while routine testing dropped from 0.71 to 0.57 tests/patient/day (20% decrease) over a 46-week period, with no increase of adverse effects or mortality. Other studies have focused on ABG. Martinez-Balzano et al. [88] established local guidance for ABG testing (Table 2) following a literature review, along with educational content (classic educative sessions, posters, stickers on POCT devices, monthly emails), and provided monthly feedback on the intervention. They were able to decrease the ABG performed by 43%. This coincides with another study that coupled education with guidance and reduced inappropriate ABG testing from 54 to 28% [89]. Likewise, a controlled study [90] focused on three common coagulation tests (INR/PT, aPTT and fibrinogen) combining education (face-to-face, posters, emails, prices information) and guidance (via posters), showed that coagulation tests ordering decreased by 64%, whereas control tests only decreased by 15%. The authors did not observe any complications and calculated an approximate AUD ~ 3.8 million (2016) annual economy across Australia and New Zealand. Finally, Viau-Lapointe et al. [91] focused on LFT and coagulation testing (not otherwise specified) in a sequential MFI: an audit (interview and online survey) was performed, followed by educational sessions, development of guidance, ending with a gatekeeping strategy on these tests. LFT were reduced from 0.65 to 0.25 (−60%) tests/patient/day, but the reduction in coagulation tests was not statistically significant.
AI/ML-based assisting tools as future interventions
Recent years have witnessed a growing interest in artificial intelligence and machine learning (AI/ML) algorithms, which are becoming increasingly complex and accurate. There are already various successful examples of AI/ML use in laboratory medicine [92]. Improvement of laboratory testing can be the desired end goal of the algorithm, e.g., when it predicts the amount of information that a test will provide [93], or it is designed to achieve optimization of laboratory resources [94]. Alternatively, improvement of appropriateness can be an indirect consequence, e.g., when the algorithm aim to characterize ICU patients, and that subsequent information on appropriate tests to select can be derived from it [95]. AI/ML models can assist laboratory medicine in achieving appropriateness in multiple ways [96]. For instance, they can predict laboratory test values or identify tests that are likely to give normal results, thus reducing the amount of blood volume. Some models are developed specifically to advise clinicians on which tests to perform, and could thus become a decision-making assisting tool. Models could also be trained on data interpretation to prevent inaccurate interpretation of appropriately prescribed tests, which is a part of the realm of inappropriateness.
Several studies have specifically investigated the use of AI/ML models to limit unnecessary laboratory testing in ICU patients. Cismondi et al. [97, 98] applied fuzzy systems algorithms on patients hospitalized in the ICU for gastrointestinal (GI) bleeding with an input of 11 physiological variables (such as heart rate, temperature, oxygen saturation, urine output, etc.). They aimed at assessing if eight GI bleeding-related laboratory tests (namely serum calcium, aPTT, PT, hematocrit, fibrinogen, lactate, platelet count and hemoglobin levels) would provide valuable clinical information for decision-making, with the goal of reducing unnecessary tests. The algorithm was able to reduce the tests used by 50% with a false-negative rate of 11.5% (meaning that in 1 case out of 10, the algorithm predicted that the test would yield no information, whereas it would have induced a change in clinicians' decision-making). More recently, Mahani and Pajoohan [99] built an algorithm intended to predict the numeric value of the test requested. They used twelve inputs’ data extracted from the ICU-specific freely available MIMIC-III database [100] including heart and respiratory rates, arterial blood pressure, oxygen saturation, etc. Focusing on two laboratory tests (calcium and hematocrit) they used two cohorts of GI bleeding patients (upper versus unspecified) and applied two prediction models (with and without k-means clustering). Prediction error indicator was selected as outcome to better represent effectiveness of prediction models. Calcium had inferior prediction error indicator (~ 9% for upper GI bleeding cohort and ~ 13% for unspecified cohort, respectively) than hematocrit (~ 27% for upper and unspecified GI bleeding cohorts). The model without clustering slightly outperformed the clustering model.
A challenge with prediction algorithms is that they mostly lack dynamicity and adaptability, i.e., they provide a probability for the next test without considering the fact that current decisions will have an impact on future decision-making. In other words, it is particularly important that algorithms consider the fact that a test had previously been omitted because of a certain probability of normality of the test result. To tackle this issue, a team built a deep learning algorithm trained on MIMIC-III database that was at first able to reduce 15% of the twelve most frequently prescribed tests (serum sodium, potassium, chloride, bicarbonate, total calcium, magnesium, phosphate, BUN, creatinine, hemoglobin, platelet count and white blood cells count) at a 5% accuracy cost [101]. They then improved the algorithm by introducing a corruption strategy leading to omission of 20% of laboratory tests requested, while maintaining 98% accuracy in predicting (ab)normal results and transition from normal to abnormal (and vice-versa) [102]. They recently performed an external validation of their algorithm on real-world adult ICU data on the same twelve tests, supporting a possible generalization of their algorithm in the clinical setting [94].
Other approaches have tried to apply information theory’s principles into machine learning algorithms to improve laboratory tests request. An ICU blood draw can yield a large volume of information. The question is whether all this information is clinically relevant, or in other words, whether some of the information in the blood test is redundant, especially over multiple days. Valderrama et al. [103] integrated information theory’s concepts of conditional entropy and pretest probability techniques with machine learning to predict whether a test result was likely to be normal or abnormal. They compared the performance of two machine learning algorithms (one with, the second without conditional entropy and pretest probability), showing that the second model had better sensitivity and negative predictive value while being less specific and precise, and that better prediction relies mainly on the pretest probability feature.
Innovative methods involving machine learning are also used to characterize ICU patients. Categorizing patients into subgroups can be useful for predicting outcome or need of intervention, as it can be for selecting laboratory tests. Hyun et al. [95] implemented k-means clustering on data from approximately 1500 patients, which included administrative, demographic, medication, and procedural information, in addition to laboratory test data on nine biomarkers (BUN, creatinine, glucose, hemoglobin, platelet count, red and white blood cells count, serum sodium and potassium). They found that three was the optimal number of clusters, with significant difference in mortality and morbidity (intubation, cardiac medications and blood administration during ICU stay). They also identified three tests of particular interest for discriminating patients’ outcomes, namely creatinine, BUN and potassium, the values of which were significantly increased in the higher mortality cluster. This suggests that patients clustering could lead to personalized clinical pathways, and thereby identify tests to be performed or avoided in specific subgroups.
Discussion
This review addresses five intervention categories aimed at enhancing the appropriateness of laboratory testing in the ICU. We include a sixth category exploring the potential of AI in such interventions. Overall, the interventions proved to be effective, as they resulted in a reduction in tests of approximately 30%, depending on the type of intervention, methodology, setting, and tests studied (Table 1). This coincides with the estimated 20–40% of inappropriate tests reported in the literature [8]. The most prevalent categories are MFI and E&G-based interventions (Table 1), in line with other non-ICU-specific reviews [20, 23].
Each strategy has relative benefits and drawbacks (Fig. 1). Education is an accessible and inexpensive approach to elicit a test reduction behavior. However, it requires an effortful and consistent application to effect a notable change in prescribing behavior. There is variation in reported efficacy of education-based interventions in the literature [3, 4, 21, 32, 33]. We found a good effectiveness of E&G-based interventions with low persistence of effect over time if the intervention is not re-enforced (Table 1). These observations are consistent with those of a systematic review [30] on interventions conducted among primary care physicians. Possible solutions include continuous training for rotating staff (e.g., residents) and displaying costs of laboratory tests [4, 11, 32, 104]. Providing indications for testing is an often used and effective strategy. In the unique context of ICU, it is challenging to establish one-fit-all guidance because of the wide disparity of complex clinical conditions. Therefore, indications for testing frequently differ between countries, or even locally, among hospitals [64, 66, 105]. Yet, implementing locally established guidance alone seems not sufficient to overcome the problem of inappropriateness [106]. Moreover, this heterogeneity complicates the generalization of results of guidance-based interventions. There is evidence that adherence to guidelines is suboptimal [107], which may lead to undesirable outcomes [108]. Several barriers to guideline adherence have been identified, namely awareness of these guidelines, familiarity and agreement with their content, resistance to change (“normal practice inertia”), external barriers (equipment, financial resources), conflicts between guidelines, or simply because they do not adequately reflect real-world situations [107, 108]. Finally, guidance may be subject to bias [109]. A&F is an effective strategy, but it tends to be more effective when individual feedback is provided. Compliance to A&F could prove to be an important determinant of success, and should be ideally assessed. Furthermore, providing regular and consistent feedback is complex and time-consuming [33]. Gatekeeping is among the most effective strategies. However, in the long term, it can impair the relationship between the laboratory and the clinicians. Collaboration with clinicians (e.g., via education and bilateral good practice standards establishment) should prevail over an unilateral stewardship from the central laboratory [106]. Gatekeeping can be integrated into a broader policy, e.g., by implementing MRI or scheduled routine panel testing in consultation with clinicians, or to limit particular tests to certain wards [11]. Collaboration with care staff is an important element for gatekeeping strategies’ long-term success. CPOE-based strategies have proven to be successful and can be used either alone (e.g., modification of the ordering form) or as a support for other types of interventions (e.g., education or gatekeeping). Caution should be taken when using alert systems to find the optimum alert level, in order to prevent alert fatigue [25, 83, 84]. MFI appear to be the most used and effective strategy to reduce inappropriateness of laboratory requests (Table 1), as already reported [20, 21, 23, 30, 39]. They lead to significant costs savings and show the higher persistence of effect over time (Table 1). Nonetheless, many MFI focused on a single analyte or type of tests. It would be worthwhile to conduct rigorous multifaceted studies on large panels of tests. Few studies have evaluated the long-term effectiveness of interventions. Only 10 out of the 45 studies retrieved addressed the persistent effect of intervention at 1 year, only 2 beyond 1 year (Table 1). Therefore, further studies are needed to evaluate the persistence of long-term effects of intervention.
Qualitative comparison of interventions to improve the appropriateness of laboratory testing in the ICU. Comparison is given for education, guidance, audit & feedback, gatekeeping, computerized physician order entry (CPOE) and multifaceted interventions in terms of feasibility, effectiveness, persistence over time (sustainability), cost-effectiveness, and patient safety. AI-based interventions are not represented
In the near future, AI/ML-based assisting tools will probably be an important ally for laboratory medicine [36,37,38]. It could be applied to enhancement of appropriate testing in various ways. By predicting the amount of information that the repetition of a test provide, ‘AI/ML-based MRI’ could be considered. Regarding commonly prescribed pairs (e.g., sodium/chloride), we could think of performing only one of the two tests (e.g., sodium) and predicting the result of the second (in our example, chloride) with AI/ML prediction models. AI-based clustering of patients could be another way of improving appropriateness of laboratory testing, by defining the most relevant tests to select for each phenotype. If so, AI/ML-based tools will have to be compliant with the European in vitro diagnostic medical devices regulation (IVDR) [110]. For the moment, this poses several challenges, the most critical of which being interpretability and transparency due to the inherent “black box” design of AI tools [111, 112]. AI/ML algorithms pose other challenges for the future of laboratory medicine in both technical and ethical perspectives. As Pennestri and Banfi [113] state, “The performance of AI technologies highly depends on the quality of inputs, the context in which they are collected and the way they are interpreted”. For example, an AI/ML model may produce biased output due to input data [114]. The use of AI/ML models also raises the question of responsibility when a necessary test is not performed due to the model's failure to recommend it, potentially jeopardizing patient safety [115]. Some authors have also expressed concern about whether or not to inform the patient that a decision was based on AI/ML suggestions [36, 116]. Pennestri and Banfi also highlight a subtle ethical challenge of AI/ML implementation regarding patient autonomy, as AI/ML models are not currently taking patient preference into account: the test that the patient need the most may not necessarily reflect what patient prefers [113]. In addition, the use of AI/ML models raises concerns about the acquisition and safe storage of big data, both in technical, financial, and ethical terms [36]. Currently, the implementation of AI/ML models in healthcare still faces a major challenge due to the doubtful inclination or even rejection from healthcare professionals [116]. This seems mainly due to concerns about job security and quality of care after AI implementation [117]. At present, it is unlikely that AI will replace specialists in laboratory medicine in many laboratory processes. Evidence shows that combined human/AI processes in detection of breast cancer cells are more efficient than human pathologists- or AI-alone processes, respectively [4, 118]. This synergy effect suggests that AI-based tools would for now be assisting ones.
An important aspect of appropriate testing improvement is to safeguard patient safety. On the one hand overuse should be minimized without omitting tests important for the clinical management. On the other hand, underuse should drive the necessary tests to be performed without requesting additional inappropriate tests. Achieving the optimal balance is inherently challenging. Nevertheless, no successful intervention that assessed safety outcomes in our review has led to a deterioration in patient safety (Table 1). Although we cannot exclude publication bias, it is a strong argument in advocating for inappropriate tests reduction.
A major challenge in interpreting data from these interventions is the overall poor quality of design, lack of standardization in methodology and diversity of outcomes [23, 27, 30, 104]. Table 3 summarizes various confounding factors that explain this heterogeneity. For example, studies have shown that size (reflected by the number of involved healthcare workers) is a significant confounding factor for the effectiveness of an intervention [119]. Other confounding effects may include geographical location, local culture about appropriateness of laboratory use, or teaching versus non-teaching status of the hospital. The International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) and its European counterpart (EFLM) have put great effort towards the standardization process [120, 121]. For example, the EFLM is working on harmonization of MRI across European countries [122]. However, there is no clear standardization on conducting and reporting interventions to reduce inappropriate laboratory testing. Standardization of the methodology design of interventions would benefit to the more efficient generalization of data collected.
The definition of inappropriateness varies across studies [34], each with its own strengths and weaknesses. Nevertheless, it is crucial to define whether a laboratory test is appropriate or not, because it determines the outcome measured in the study. According to some authors, a laboratory test is considered inappropriate when it has no meaningful impact on therapy or yields a normal result [123]. However, this definition may not always apply, especially in conditions such as the acute coronary syndrome, where a negative cardiac troponin level is a significant finding. In comparison, Lundberg suggested that an intervention is inappropriate when harm outweighs benefits [124]. Appropriateness has also been associated with adherence to organizational guidelines [106, 125] or self-referral [126]. Often, appropriateness is defined using literature or expert opinion [125]. Some authors have suggested to refine it by distinguishing between inappropriate requests (the question asked is clinically inappropriate), inappropriate tests (the question asked is clinically relevant, but the wrong test is selected by the clinician, or the wrong test is performed by the laboratory) and unnecessary requests (the question asked may have been clinically appropriate, but may no longer be so at the time of testing) [33]. The value-based healthcare (VBHC) approach offers a more objective definition of appropriateness. VBHC is focused on determining the value that an intervention provides, which means evaluating the outcomes achieved per money spent [127]. A test can be considered inappropriate if it is of low value. According to Colla et al. [67], low value care refers to application of care that is unlikely to benefit the patient considering the cost, alternative options available, and patient preferences. To determine the appropriateness of a test, we emphasize the need for comprehensive evaluation of the clinical utility of prescribing the test in conjunction with physiological or pharmacological principles (e.g., half-life) of the molecular target of the test.
Test ordering decision-making is a complex task that requires time and high-intensity attention. When interviewed, ICU physicians disclose that they do not have the necessary time to thoroughly assess the appropriate tests to order from the unnecessary ones [84]. In this context, interventions to reduce inappropriateness can be perceived as an additional strain. On the contrary, well-executed interventions can influence physicians’ test-ordering behavior [22]. For example, by making appropriate tests easier and inappropriate tests more difficult to select, guidance- and CPOE-based interventions favor efficiency. In contrast, education, financial incentives, and A&F interventions favor thoroughness. It also highlights the role of laboratory staff in the pursuit of appropriateness. As physicians have little time to devote to the proper utilization of laboratory resources, specialists in laboratory medicine should intensify the collaboration to reduce inappropriate testing and to proactively become “knowledge manager[s]” [128]. Specialists in laboratory medicine have the responsibility to ensure communication with users in order to provide education on latest evidence for tests selection and advice on appropriate interpretation of tests [129,130,131,132].
Inappropriate laboratory testing concerns over—as much as underuse. It seems that underuse is even twice as frequent as its counterpart [8]. However, there is a bias toward the reduction of overuse in the literature of interventions aimed at improving testing appropriateness. This may be because of the easier assessment of tests reduction and direct costs savings in reduction of overuse. In the interventions we reviewed, only one [84] mentioned underuse. Notably, it was not in accordance with Zhi et al.’s estimations [8], as the results showed an overuse of procalcitonin in one out of five tests, whereas underuse was estimated to occur in one out of 38 tests [84]. It is likely that underuse vary depending on the test concerned [133,134,135]. Future studies assessing consequences of reducing underuse are needed.
Several limitations of this review deserve mention. Although comprehensive, our literature search was not systematic. We did not systematically evaluate the quality of studies, or their potential biases. Yet, a 2015 systematic review emphasizes the poor quality of interventional studies in the general setting [23]. Our study found an overall poor quality of methodology and reporting. Forty-one percent (18 out of 44) of the studies we retrieved were conference abstracts or letters to editors that often lacked full details of the methodology used. This study may therefore have limitations in terms of its breadth, depth, and comprehensiveness. We decided to include conference abstracts to increase comprehensiveness. As discussed above, the lack of standardization in study design complicates data generalization, and we cannot exclude the presence of publication bias. Caution is thus advised with certain numbers, particularly with costs savings. Nevertheless, most of the numbers are estimates, and the central message remains the trend towards reduction in the number of inappropriate tests, and potential savings made, while preserving patient safety. Delimiting studies into categories can introduce bias, and this division can appear artificial for certain studies that do not clearly fall into one category or another. We had to balance between facilitating understanding through a more general classification and the rigor of a more specific but numerous classifications. However, we classified our data according to literature standards as closely as possible [4, 11, 32, 33, 39]. Our review focused on ICU adult patients. We did not investigate microbiology, in that it is a highly specific diagnostic area, with its own methods, tests and body of literature.
The plan–do–study–act (PDSA) cycle is a frequently used model for improving process and practice, such as reducing inappropriate use of laboratory resources. The first stage involves defining objectives, linking them to desired changes, determining necessary actions to bring about change, and planning how to measure the success of the change. In the second stage, the planned actions are performed and data is collected. During the third stage, the effectiveness of the actions is evaluated, and their relevance to the desired objective is assessed. In the fourth stage, the data analyzed in the previous stage is used to determine whether the change can be adopted and to plan the next PDSA cycle. In a broader sense, the PDSA model provides an analogy to describe the process involved in an intervention to limit inappropriate use of laboratory resources, and can be used to develop effective and sustainable interventions (Fig. 2). Based on our literature review, we recommend utilizing a multi-strategy approach. The first step towards improvement is recognizing a problem or an area for improvement and committing to acting. We suggest starting any intervention by defining the desired objective and possible options, as well as meeting with stakeholders regarding the objectives. The initial logical step of an intervention would be to explicitly state the need for change by explaining the problem, the reasons for change, and the available solutions through stakeholder education. We advise educating about the problem (e.g., raising awareness about inappropriateness), as well as the selected solutions to face it (e.g., the strategies that will be used to address the problem). Conducting a literature review can provide objective facts to support problem definition, evaluate existing solutions from the literature, and identify available guidance (see Table 2). At this stage, an audit can evaluate current standard practices. From there actions can be taken, which may include the various strategies discussed such as implementing MRI or reshaping ordering forms or panels (i.e., CPOE), and imposing new restrictions on certain tests (i.e., gatekeeping) (Fig. 1). It is important to evaluate the impact of initial strategies and make the necessary changes. An audit and feedback strategy can be used to assess the change brought about by the intervention compared to the pre-intervention situation. Although this strategy may be complex and time-consuming, it is an effective way to assess progress and make necessary corrections. The audit results can determine whether to maintain current actions or adapt the intervention. If necessary, the education and guidance cycle can be renewed to increase effectiveness. The cycle can be repeated until the desired outcome is achieved, or even indefinitely. Few studies have assessed the effectiveness of interventions beyond 1 year. Therefore, we suggest frequent renewal of PDSA cycles and/or long-term evaluation of intervention effectiveness. Throughout the entire process, AI/ML models can assist in selecting, implementing, or optimizing strategies, and even provide additional support through future applications. Finally, we emphasize that maintaining ongoing communication with clinicians and other stakeholders throughout the entire process is key to ensure successful implementation of the changes. We believe that this framework can lead to interventions that maximize effectiveness in reducing inappropriate use of laboratory tests.
Conclusions
We reviewed interventions aimed at improving appropriate laboratory resources utilization in the ICU. We identified six discrete categories of interventions: education and guidance (E&G)e, audit and feedback (A&F), gatekeeping, computerized physician order entry, multifaceted and AI/ML-based interventions. We provided an assessment of respective benefits and drawbacks. The most represented categories of interventions are E&G-based and MFI. The most efficient and long-lasting interventions are MFI. AI/ML-based assisting tools interventions could be promising for enhancing the appropriate of testing in the future. Collaboration between clinicians and laboratory staff is key to improve rational laboratory utilization. Reduction of overuse is overrepresented in the literature in comparison to improvement of underuse. Moreover, overall methodological quality is poor and study designs lack standardization. Further studies on underuse of laboratory testing in the ICU as well as standardization of methodology for interventions are needed. We provide practical guidance for optimizing the effectiveness of an intervention protocol designed to limit inappropriate use of laboratory resources.
Abbreviations
- A&F:
-
Audit and feedback
- ABG:
-
Arterial blood gas
- AI/ML:
-
Artificial intelligence and machine learning
- ALP:
-
Alkaline phosphatase
- ALT:
-
Aspartate aminotransferase
- aPTT:
-
Activated partial thromboplastin time
- AST:
-
Alanine transaminase
- AUD:
-
Australian dollar
- BMP:
-
Basic metabolic panel
- BUN:
-
Blood urea nitrogen
- CAD:
-
Canadian dollar
- CPOE:
-
Computerized physician order entry
- CRP:
-
C-reactive protein
- EUR:
-
Euro
- FBC:
-
Full blood count
- GI:
-
Gastrointestinal
- INR:
-
International normalized ratio
- ICU:
-
Intensive care unit
- LFT:
-
Liver function tests
- LOS:
-
Length of stay
- MFI:
-
Multifaceted intervention
- MRI:
-
Minimum retesting interval
- POCT:
-
Point-of-care testing
- PT:
-
Prothrombin time
- USD:
-
US dollar
References
World Health Organization (WHO). Spending on health in Europe: entering a new era. Copenhagen: WHO Regional Office for Europe; 2021.
Centers for Medicare & Medicaid Services. National health expenditure data: projected: CMS.gov. 2023. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountsprojected. Accessed 14 June 2023.
Smellie WS. Demand management and test request rationalization. Ann Clin Biochem. 2012;49(Pt 4):323–36.
Mrazek C, Haschke-Becher E, Felder TK, Keppel MH, Oberkofler H, Cadamuro J. Laboratory demand management strategies-an overview. Diagnostics (Basel). 2021;11(7):1141.
Arshoff L, Hoag G, Ivany C, Kinniburgh D. Laboratory medicine: the exemplar for value-based healthcare. Healthc Manage Forum. 2021;34(3):175–80.
Hallworth MJ. The “70% claim”: what is the evidence base? Ann Clin Biochem. 2011;48(Pt 6):487–8.
Lippi G, Plebani M. The add value of laboratory diagnostics: the many reasons why decision-makers should actually care. J Lab Precis Med. 2017;2:100.
Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The landscape of inappropriate laboratory testing: A 15-Year meta-analysis. PLoS ONE. 2013;8(11):e78962.
Lippi G, Bovo C, Ciaccio M. Inappropriateness in laboratory medicine: an elephant in the room? Ann Transl Med. 2017;5(4):82.
Cadamuro J, Gaksch M, Wiedemann H, Lippi G, von Meyer A, Pertersmann A, et al. Are laboratory tests always needed? Frequency and causes of laboratory overuse in a hospital setting. Clin Biochem. 2018;54:85–91.
Cadamuro J, Ibarz M, Cornes M, Nybo M, Haschke-Becher E, von Meyer A, et al. Managing inappropriate utilization of laboratory resources. Diagnosis (Berl). 2019;6(1):5–13.
Epner PL, Gans JE, Graber ML. When diagnostic testing leads to harm: a new outcomes-based approach for laboratory medicine. BMJ Qual Saf. 2013;22:ii6–10.
Carpenter CR, Raja AS, Brown MD. Overtesting and the downstream consequences of overtreatment: implications of “preventing overdiagnosis” for emergency medicine. Acad Emerg Med. 2015;22(12):1484–92.
Gopalratnam K, Forde IC, O’Connor JV, Kaufman DA. less is more in the ICU: resuscitation, oxygenation and routine tests. Semin Respir Crit Care Med. 2016;37(1):23–33.
Grieme CV, Voss DR, Olson KE, Davis SR, Kulhavy J, Krasowski MD. Prevalence and clinical utility of “incidental” critical values resulting from critical care laboratory testing. Lab Med. 2016;47(4):338–49.
van Daele PL, van Saase JL. Incidental findings; prevention is better than cure. Neth J Med. 2014;72(7):343–4.
Siegal DM, Belley-Côté EP, Lee SF, Robertson T, Hill S, Benoit P, et al. Small-volume tubes to reduce anemia and transfusion (STRATUS): a pilot study. Can J Anaesth. 2023. https://doi.org/10.1007/s12630-023-02548-6.
Wu Y, Spaulding AC, Borkar S, Shoaei MM, Mendoza M, Grant RL, et al. Reducing blood loss by changing to small volume tubes for laboratory testing. Mayo Clin Proc Innov Qual Outcomes. 2021;5(1):72–83.
Smeets TJL, Van De Velde D, Koch BCP, Endeman H, Hunfeld NGM. Using residual blood from the arterial blood gas test to perform therapeutic drug monitoring of vancomycin: an example of good clinical practice moving towards a sustainable intensive care unit. Crit Care Res Pract. 2022;2022:1–5.
Bindraban RS, Berg MJT, Naaktgeboren CA, Kramer MHH, Solinge WWV, Nanayakkara PWB. Reducing test utilization in hospital settings: a narrative review. Ann Lab Med. 2018;38(5):402–12.
Rubinstein M, Hirsch R, Bandyopadhyay K, Madison B, Taylor T, Ranne A, et al. Effectiveness of practices to support appropriate laboratory test utilization: a laboratory medicine best practices systematic review and meta-analysis. Am J Clin Pathol. 2018;149(3):197–221.
Duddy C, Wong G. Efficiency over thoroughness in laboratory testing decision making in primary care: findings from a realist review. BJGP Open. 2021;5(2):bjgpopen20X1011.
Kobewka DM, Ronksley PE, McKay JA, Forster AJ, van Walraven C. Influence of educational, audit and feedback, system based, and incentive and penalty interventions to reduce laboratory test utilization: a systematic review. Clin Chem Lab Med. 2015;53(2):157–83.
Solomon DH, Hashimoto H, Daltroy L, Liang MH. Techniques to improve physicians’ use of diagnostic tests: a new conceptual framework. JAMA. 1998;280(23):2020–7.
Delvaux N, Van Thienen K, Heselmans A, De Velde SV, Ramaekers D, Aertgeerts B. The effects of computerized clinical decision support systems on laboratory test ordering: a systematic review. Arch Pathol Lab Med. 2017;141(4):585–95.
Maillet É, Paré G, Currie LM, Raymond L, Ortiz de Guinea A, Trudel MC, et al. Laboratory testing in primary care: a systematic review of health IT impacts. Int J Med Inform. 2018;116:52–69.
Zhelev Z, Abbott R, Rogers M, Fleming S, Patterson A, Hamilton WT, et al. Effectiveness of interventions to reduce ordering of thyroid function tests: a systematic review. BMJ Open. 2016;6(6):e010065.
Thomas RE, Vaska M, Naugler C, Chowdhury TT. Interventions to educate family physicians to change test ordering. Acad Pathol. 2016;3:237428951663347.
Thomas RE, Vaska M, Naugler C, Turin TC. Interventions at the laboratory level to reduce laboratory test ordering by family physicians: systematic review. Clin Biochem. 2015;48(18):1358–65.
Cadogan SL, Browne JP, Bradley CP, Cahill MR. The effectiveness of interventions to improve laboratory requesting patterns among primary care physicians: a systematic review. Implement Sci. 2015. https://doi.org/10.1186/s13012-015-0356-4.
Main C, Moxham T, Wyatt JC, Kay J, Anderson R, Stein K. Computerised decision support systems in order communication for diagnostic, screening or monitoring test ordering: systematic reviews of the effects and cost-effectiveness of systems. Health Technol Assess. 2010. https://doi.org/10.3310/hta14480.
Huck A, Lewandrowski K. Utilization management in the clinical laboratory: an introduction and overview of the literature. Clin Chim Acta. 2014;427:111–7.
Fryer AA, Smellie WSA. Managing demand for laboratory tests: a laboratory toolkit. J Clin Pathol. 2013;66(1):62–72.
Foster M, Presseau J, McCleary N, Carroll K, McIntyre L, Hutton B, et al. Audit and feedback to improve laboratory test and transfusion ordering in critical care: a systematic review. Implement Sci. 2020;15(1):46. https://doi.org/10.1186/s13012-020-00981-5.
Hooper KP, Anstey MH, Litton E. Safety and efficacy of routine diagnostic test reduction interventions in patients admitted to the intensive care unit: a systematic review and meta-analysis. Anaesth Intensive Care. 2021;49(1):23–34.
Gruson D, Helleputte T, Rousseau P, Gruson D. Data science, artificial intelligence, and machine learning: opportunities for laboratory medicine and the value of positive regulation. Clin Biochem. 2019;69:1–7.
Cadamuro J, Cabitza F, Debeljak Z, De Bruyne S, Frans G, Perez SM, et al. Potentials and pitfalls of ChatGPT and natural-language artificial intelligence models for the understanding of laboratory medicine test results. An assessment by the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) Working Group on Artificial Intelligence (WG-AI). Clin Chem Lab Med. 2023;61(7):1158–66.
Carobene A, Cabitza F, Bernardini S, Gopalan R, Lennerz JK, Weir C, et al. Where is laboratory medicine headed in the next decade? Partnership model for efficient integration and adoption of artificial intelligence into medical laboratories. Clin Chem Lab Med. 2023;61(4):535–43.
Panteghini M, Dolci A, Birindelli S, Szoke D, Aloisio E, Caruso S. Pursuing appropriateness of laboratory tests: a 15-year experience in an academic medical institution. Clin Chem Lab Med. 2022;60(11):1706–18.
Blum FE, Lund ET, Hall HA, Tachauer AD, Chedrawy EG, Zilberstein J. Reevaluation of the utilization of arterial blood gas analysis in the Intensive Care Unit: effects on patient safety and patient outcome. J Crit Care. 2015;30(2):438.e1-5.
Cahill C, Blumberg N, Pietropaoli A, Maxwell M, Wanck A, Refaai MA. Program to reduce redundant laboratory sampling in an intensive care unit leads to non-inferior patient care and outcomes. Anesth Analg. 2018;127(3):15.
DellaVolpe JD, Chakraborti C, Cerreta K, Romero CJ, Firestein CE, Myers L, et al. Effects of implementing a protocol for arterial blood gas use on ordering practices and diagnostic yield. Healthc (Amst). 2014;2(2):130–5.
Fresco M, Demeilliers-Pfister G, Merle V, Brunel V, Veber B, Dureuil B. Can we optimize prescription of laboratory tests in surgical intensive care unit (ICU)? Study of appropriateness of care. Ann Intensive Care. 2016;6(Suppl 1):52.
Goddard K, Austin SJ. Appropriate regulation of routine laboratory testing can reduce the costs associated with patient stay in intensive care. Crit Care. 2011;15(Suppl 1):P133.
Kotecha N, Cardasis J, Narayanswami G, Shapiro J. Reducing unnecessary lab tests in the MICU by incorporating a guideline in daily ICU team rounds. Am J Respir Crit Care Med. 2015;191:A1091.
Kotecha N, Shapiro JM, Cardasis J, Narayanswami G. Reducing unnecessary laboratory testing in the medical ICU. Am J Med. 2017;130(6):648–51.
Kumwilaisak K, Noto A, Schmidt UH, Beck CI, Crimi C, Lewandrowski K, et al. Effect of laboratory testing guidelines on the utilization of tests and order entries in a surgical intensive care unit. Crit Care Med. 2008;36(11):2993–9.
Leydier S, Clerc-Urmes I, Lemarie J, Maigrat CH, Conrad M, Cravoisy-Popovic A, et al. Impact of the implementation of guidelines for laboratory testing in an intensive care unit. Ann Intensive Care. 2016;6(Suppl 1):53.
Prat G, Lefèvre M, Nowak E, Tonnelier J-M, Renault A, L’Her E, et al. Impact of clinical guidelines to improve appropriateness of laboratory tests and chest radiographs. Intensive Care Med. 2009;35(6):1047–53.
Shen JZ, Hill BC, Polhill SR, Evans P, Galloway DP, Johnson RB, et al. Optimization of laboratory ordering practices for complete blood count with differential. Am J Clin Pathol. 2019;151(3):306–15.
Vezzani A, Zasa M, Manca T, Agostinelli A, Giordano D. Improving laboratory test requests can reduce costs in ICUs. Eur J Anaesthesiol. 2013;30(3):134–6.
Berlet T. Rationalising standard laboratory measurements in the Intensive Care Unit. ICU Management. 2015;15:33.
Thomas KW. Right test, right time, right patient. Crit Care Med. 2014;42(1):190–2.
Huang DT, Ramirez P. Biomarkers in the ICU: less is more? Yes Intensive Care Med. 2021;47(1):94–6.
Marik PE. “Less Is More”: the new paradigm in critical care. In: Marik PE, editor. Evidence-based critical care. Cham: Springer International Publishing; 2015. p. 7–11.
Lehot JJ, Clec’h C, Bonhomme F, Brauner M, Chemouni F, de Mesmay M, et al. Pertinence de la prescription des examens biologiques et de la radiographie thoracique en réanimation RFE commune SFAR-SRLF. Méd Intensive Réa. 2019;28(2):172–189. https://doi.org/10.3166/rea-2018-0004.
Adhikari N, Suwal K, Khadka S, Dahal B, Thomas L, Dadeboyina C, et al. Decreasing unnecessary laboratory testing in medical critical care. Adv Clin Med Res Healthc Deliv. 2022. https://doi.org/10.53785/2769-2779.1113.
Maguet PL, Asehnoune K, Autet L-M, Gaillard T, Lasocki S, Mimoz O, et al. Transitioning from routine to on-demand test ordering in intensive care units: a prospective, multicenter, interventional study. Br J Anaesth. 2015. https://doi.org/10.1093/bja/el_12998.
Malalur P, Greenberg C, Lim MY. Limited impact of clinician education on reducing inappropriate PF4 testing for heparin-induced thrombocytopenia. J Thromb Thrombolysis. 2019;47(2):287–91.
Yorkgitis BK, Loughlin JW, Gandee Z, Bates HH, Weinhouse G. Laboratory tests and X-ray imaging in a surgical intensive care unit: checking the checklist. J Am Osteopath Assoc. 2018;118(5):305–9.
Thakkar RN, Kim D, Knight AM, Riedel S, Vaidya D, Wright SM. Impact of an educational intervention on the frequency of daily blood test orders for hospitalized patients. Am J Clin Pathol. 2015;143(3):393–7.
Kleinpell RM, Farmer JC, Pastores SM. Reducing unnecessary testing in the intensive care unit by choosing wisely. Acute Crit Care. 2018;33(1):1–6.
International Organization for Standardization (ISO). ISO 15189:2022: Medical Laboratories: Requirements for quality and competence. 2022. https://www.iso.org/standard/76677.html. Accessed 10 Sept 2023
Ellenbogen MI, Ma M, Christensen NP, Lee J, O’Leary KJ. Differences in routine laboratory ordering between a teaching service and a hospitalist service at a single academic medical center. South Med J. 2017;110(1):25–30.
Larsson A, Palmer M, Hultén G, Tryding N. Large differences in laboratory utilisation between hospitals in Sweden. Clin Chem Lab Med. 2000;38(5):383–9.
Spence J, Bell DD, Garland A. Variation in diagnostic testing in ICUs: a comparison of teaching and nonteaching hospitals in a regional system. Crit Care Med. 2014;42(1):9–16.
Colla CH, Mainor AJ, Hargreaves C, Sequist T, Morden N. Interventions aimed at reducing use of low-value health services: a systematic review. Med Care Res Rev. 2017;74(5):507–50.
Jefferson BK, King JE. Impact of the acute care nurse practitioner in reducing the number of unwarranted daily laboratory tests in the intensive care unit. J Am Assoc Nurse Pract. 2018;30(5):285–92.
Rachakonda KS, Parr M, Aneman A, Bhonagiri S, Micallef S. Rational clinical pathology assessment in the intensive care unit. Anaesth Intensive Care. 2017;45(4):503–10.
de Bie P, Tepaske R, Hoek A, Sturk A, van Dongen-Lases E. Reduction in the number of reported laboratory results for an adult intensive care unit by effective order management and parameter selection on the blood gas analyzers. Point of Care. 2016;15(1):7.
Sugarman J, Malik J, Hill J, Morgan P. Unindicated daily blood testing on ICU: An avoidable expense? Intensive Care Med Exp. 2020; 8(SUPPL 2). Accessed 10 Sept 2023
Tyrrell S, Roberts H, Zouwail S. A comparison of different methods of demand management on requesting activity in a teaching hospital intensive care unit. Ann Clin Biochem. 2015;52(Pt 1):122–5.
Bodley T, Levi O, Chan M, Friedrich JO, Hicks LK. Reducing unnecessary diagnostic phlebotomy in intensive care: a prospective quality improvement intervention. BMJ Qual Saf. 2023. https://doi.org/10.1136/bmjqs-2022-015358.
Dhanani JA, Barnett AG, Lipman J, Reade MC. Strategies to reduce inappropriate laboratory blood test orders in intensive care are effective and safe: a before-and-after quality improvement study. Anaesth Intensive Care. 2018;46(3):313–20.
Khan M, Perry T, Smith B, Ernst N, Droege C, Garber P, et al. Reducing lab testing in the medical ICU through system redesign using improvement science. Crit Care Med. 2019;47(1):639.
Dodek PM, Lo A, Zhao T, Rajapakse S, Leung A, Chow J, et al. Improving the appropriateness of serum magnesium testing in an intensive care unit. Am J Respir Crit Care Med. 2018; 197(MeetingAbstracts).
Lo A, Zhao T, Rajapakse S, Leung A, Chow J, Wong R, et al. Improving the appropriateness of serum magnesium testing in an intensive care unit. Can J Anesth. 2020;67(9):1274–5.
Merkeley HL, Hemmett J, Cessford TA, Amiri N, Geller GS, Baradaran N, et al. Multipronged strategy to reduce routine-priority blood testing in intensive care unit patients. J Crit Care. 2016;31(1):212–6.
Iosfina I, Merkeley H, Cessford T, Geller G, Amiri N, Baradaran N, et al. Implementation of an on-demand strategy for routine blood testing in ICU patients. Am J Respir Crit Care Med. 2013;187:A5322.
Conroy M, Homsy E, Johns J, Patterson K, Singha A, Story R, et al. Reducing unnecessary laboratory utilization in the medical ICU: a fellow-driven quality improvement initiative. Crit Care Explor. 2021;3(7):e0499.
Aloisio E, Dolci A, Panteghini M. Managing post-analytical phase of procalcitonin testing in intensive care unit improves the request appropriateness. Clin Chim Acta. 2019;493:S706–7.
Lo HG, Matheny ME, Seger DL, Bates DW, Gandhi TK. Impact of non-interruptive medication laboratory monitoring alerts in ambulatory care. J Am Med Inform Assoc. 2009;16(1):66–71.
Baysari MT, Tariq A, Day RO, Westbrook JI. Alert override as a habitual behavior - a new perspective on a persistent problem. J Am Med Inform Assoc. 2017;24(2):409–12.
Castellanos I, Kraus S, Toddenroth D, Prokosch H-U, Bürkle T. Using arden syntax medical logic modules to reduce overutilization of laboratory tests for detection of bacterial infections-success or failure? Artif Intell Med. 2018;92:43–50.
Raad S, Elliott R, Dickerson E, Khan B, Diab K. Reduction of laboratory utilization in the intensive care unit. J Intensive Care Med. 2017;32(8):500–7.
Clouzeau B, Caujolle M, San-Miguel A, Pillot J, Gazeau N, Tacaille C, et al. The sustainable impact of an educational approach to improve the appropriateness of laboratory test orders in the ICU. PLoS ONE. 2019;14(5):e0214802.
Litton E, Hooper K, Edibam C. Targeted testing safely reduces diagnostic tests in the intensive care unit: an interventional study. Tasman Med J. 2020;2(4):74–9.
Martínez-Balzano CD, Oliveira P, O’Rourke M, Hills L, Sosa AF, Critical Care Operations Committee of the UMHC. An educational intervention optimizes the use of arterial blood gas determinations across ICUs from different specialties: a quality-improvement study. Chest. 2017;151(3):579–85.
Walsh O, Davis K, Gatward J. Reducing inappropriate arterial blood gas testing in a quaternary intensive care unit. Anaesth Intensive Care. 2020;48(2 SUPPL):33.
Musca S, Desai S, Roberts B, Paterson T, Anstey M. Routine coagulation testing in intensive care. Crit Care Resusc. 2016;18(3):213–7.
Viau-Lapointe J, Geagea A, Alali A, Artigas RM, Al-Fares AA, Hamidi M, et al. Reducing routine blood testing in the medical-surgical intensive care unit: a single center quality improvement study. Am J Respir Crit Care Med. 2018;197(MeetingAbstracts). Accessed 10 Sept 2023
Herman DS, Rhoads DD, Schulz WL, Durant TJS. Artificial intelligence and mapping a new direction in laboratory medicine: a review. Clin Chem. 2021;67(11):1466–82.
Lee J, Maslove DM. Using information theory to identify redundancy in common laboratory tests in the intensive care unit. BMC Med Inform Decis Mak. 2015;15(1):59.
Li LT, Huang T, Bernstam EV, Jiang X. External validation of a laboratory prediction algorithm for the reduction of unnecessary labs in the critical care setting. Am J Med. 2022;135(6):769–74.
Hyun S, Kaewprag P, Cooper C, Hixon B, Moffatt-Bruce S. Exploration of critical care data by using unsupervised machine learning. Comput Methods Programs Biomed. 2020;194:105507.
Rabbani N, Kim GYE, Suarez CJ, Chen JH. Applications of machine learning in routine laboratory medicine: current state and future directions. Clin Biochem. 2022;103:1–7.
Cismondi F, Celi LA, Fialho AS, Vieira SM, Reti SR, Sousa JMC, et al. Reducing unnecessary lab testing in the ICU with artificial intelligence. Int J Med Inform. 2013;82(5):345–58.
Cismondi FC, Fialho AS, Vieira SM, Celi LA, Reti SR, Sousa JM, et al. Reducing ICU blood draws with artificial intelligence. Crit Care. 2012;16:S156.
Mahani GK, Pajoohan M-R. Predicting lab values for gastrointestinal bleeding patients in the intensive care unit: a comparative study on the impact of comorbidities and medications. Artif Intell Med. 2019;94:79–87.
Johnson AEW, Pollard TJ, Shen L, Lehman L-WH, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3(1):160035.
Yu L, Zhang Q, Bernstam EV, Jiang X. Predict or draw blood: an integrated method to reduce lab tests. J Biomed Inform. 2020;104:103394.
Yu L, Li L, Bernstam E, Jiang X. A deep learning solution to recommend laboratory reduction strategies in ICU. Int J Med Inform. 2020;144:104282.
Valderrama CE, Niven DJ, Stelfox HT, Lee J. Predicting abnormal laboratory blood test results in the intensive care unit using novel features based on information theory and historical conditional probability: observational study. JMIR Med Inform. 2022;10(6):e35250.
Silvestri MT, Bongiovanni TR, Glover JG, Gross CP. Impact of price display on provider ordering: a systematic review. J Hosp Med. 2016;11(1):65–76.
Larsson A, Tynngård N, Kander T, Bonnevier J, Schött U. Comparison of point-of-care hemostatic assays, routine coagulation tests, and outcome scores in critically ill patients. J Crit Care. 2015;30(5):1032–8.
Ferraro S, Panteghini M. The role of laboratory in ensuring appropriate test requests. Clin Biochem. 2017;50(10–11):555–61.
Williamson T, Gomez-Espinosa E, Stewart F, Dean BB, Singh R, Cui J, et al. Poor adherence to clinical practice guidelines: a call to action for increased albuminuria testing in patients with type 2 diabetes. J Diabetes Complicat. 2023;37(8):108548.
Barth JH, Misra S, Aakre KM, Langlois MR, Watine J, Twomey PJ, et al. Why are clinical practice guidelines not followed? Clin Chem Lab Med. 2016;54(7):1133–9.
Misra S, Barth JH. How good is the evidence base for test selection in clinical guidelines? Clin Chim Acta. 2014;432:27–32.
European Parliament, Council of the European Union. Regulation (EU) 2017/746 of the European Parliament and of the Council of 5 April 2017 on in vitro diagnostic medical devices and repealing Directive 98/79/EC and Comissions Decision 2010/227/EU. 2017. https://eur-lex.europa.eu/eli/reg/2017/746/oj. Accessed 20 Mar 2023.
Müller H, Holzinger A, Plass M, Brcic L, Stumptner C, Zatloukal K. Explainability and causability for artificial intelligence-supported medical image analysis in the context of the European in vitro diagnostic regulation. N Biotechnol. 2022;70:67–72.
Li B, Qi P, Liu B, Di S, Liu J, Pei J, et al. Trustworthy AI: From Principles to Practices. ArXiv. 2022.
Pennestrì F, Banfi G. Artificial intelligence in laboratory medicine: fundamental ethical issues and normative key-points. Clin Chem Lab Med. 2022;60(12):1867–74.
Jackson BR, Ye Y, Crawford JM, Becich MJ, Roy S, Botkin JR, et al. The ethics of artificial intelligence in pathology and laboratory medicine: principles and practice. Acad Pathol. 2021;8:2374289521990784.
Lippi G. Machine learning in laboratory diagnostics: valuable resources or a big hoax? Diagnosis (Berl). 2019;8(2):133–5.
Paranjape K, Schinkel M, Hammer RD, Schouten B, Nannan Panday RS, Elbers PWG, et al. The value of artificial intelligence in laboratory medicine. Am J Clin Pathol. 2021;155(6):823–31.
Ardon O, Schmidt RL. Clinical laboratory employees’ attitudes toward artificial intelligence. Lab Med. 2020;51(6):649–54.
Wang D, Khosla A, Gargeya R, Irshad H, Beck AH. Deep Learning for Identifying Metastatic Breast Cancer. ArXiv. 2016;abs/1606.05718.
Mrazek C, Stechemesser L, Haschke-Becher E, Hölzl B, Paulweber B, Keppel MH, et al. Reducing the probability of falsely elevated HbA1c results in diabetic patients by applying automated and educative HbA1c re-testing intervals. Clin Biochem. 2020;80:14–8.
Plebani M. Harmonization in laboratory medicine: requests, samples, measurements and reports. Crit Rev Clin Lab Sci. 2016;53(3):184–96.
Plebani M, Astion ML, Barth JH, Chen W, De Oliveira Galoro CA, Escuer MI, et al. Harmonization of quality indicators in laboratory medicine. A preliminary consensus. Clin Chem Lab Med. 2014. https://doi.org/10.1515/cclm-2014-0142.
Ceriotti F, Barhanovic NG, Kostovska I, Kotaska K, Perich Alsina MC. Harmonisation of the laboratory testing process: need for a coordinated approach. Clin Chem Lab Med. 2016;54(12):e361–3.
van Walraven C, Naylor CD. Do we know what inappropriate laboratory utilization is? A systematic review of laboratory clinical audits. JAMA. 1998;280(6):550–8.
Lundberg GD. The need for an outcomes research agenda for clinical laboratory testing. JAMA. 1998;280(6):565–6.
Hauser RG, Shirts BH. Do we now know what inappropriate laboratory utilization is? An expanded systematic review of laboratory clinical audits. Am J Clin Pathol. 2014;141(6):774–83.
Mikhaeil M, Day AG, Ilan R. Non-essential blood tests in the intensive care unit: a prospective observational study. Can J Anesth. 2017;64(3):290–5.
Schmidt RL, Ashwood ER. Laboratory medicine and value-based health care. Am J Clin Pathol. 2015;144(3):357–8.
Beastall GH. Adding value to laboratory medicine: a professional responsibility. Clin Chem Lab Med. 2013;51(1):221–7.
Orth M, Averina M, Chatzipanagiotou S, Faure G, Haushofer A, Kusec V, et al. Opinion: redefining the role of the physician in laboratory medicine in the context of emerging technologies, personalised medicine and patient autonomy ('4P medicine’). J Clin Pathol. 2019;72(3):191–7.
Unsworth DJ, Lock RJ. Consultant leaders and delivery of high quality pathology services. J Clin Pathol. 2013;66(5):361.
Ferraro S, Braga F, Panteghini M. Laboratory medicine in the new healthcare environment. Clin Chem Lab Med. 2016;54(4):523–33.
Plebani M, Laposata M, Lippi G. A manifesto for the future of laboratory medicine professionals. Clin Chim Acta. 2019;489:49–52.
Cadamuro J, Simundic A-M, Von Meyer A, Haschke-Becher E, Keppel MH, Oberkofler H, et al. Diagnostic workup of microcytic anemia: an evaluation of underuse or misuse of laboratory testing in a hospital setting using the AlinIQ system. Arch Pathol Lab Med. 2023;147(1):117–24.
Sarkar MK, Botz CM, Laposata M. An assessment of overutilization and underutilization of laboratory tests by expert physicians in the evaluation of patients for bleeding and thrombotic disorders in clinical context and in real time. Diagnosis (Berl). 2017;4(1):21–6.
Vyas N, Carman C, Sarkar MK, Salazar JH, Zahner CJ. Overutilization and underutilization of thyroid function tests are major causes of diagnostic errors in pregnant women. Clin Lab. 2021. https://doi.org/10.7754/Clin.Lab.2020.201019.
Bosque MD, Martínez M, Barbadillo S, Lema J, Tomás R, Ovejero M, et al. Impact of providing laboratory tests data on clinician ordering behavior in the intensive care unit. Intensive Care Med Exp. 2019;7(Suppl 3):161.
Gray R, Baldwin F. Targeting blood tests in the ICU may lead to a significant cost reduction. Crit Care. 2014;18:S6.
Hall T, Wykes K, Jack J, Ngu WC, Morgan P. Are daily blood tests on icu necessary? How can we reduce them? Intensive Care Med Exp. 2016; 4. Accessed 10 Sept 2023
Han SJ, Saigal R, Rolston JD, Cheng JS, Lau CY, Mistry RI, et al. Targeted reduction in neurosurgical laboratory utilization: resident-led effort at a single academic institution. J Neurosurg. 2014;120(1):173–7.
Simvoulidis L, Costa RC, Ávila CA, Sória TS, Menezes MM, Rangel JR, et al. Reducing unnecessary laboratory testing in an intensive care unit of a tertiary hospital-what changed after one year? Crit Care. 2020;24(Suppl 1):138.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization, literature searching strategy and data extraction: LD, EC, FM, MC additional references and validation of data extraction: EC, PMH, AM, GL, FM, MC. Writing—original draft: LD. Writing—review, editing and enhancement: LD, EC, PMH, AM, GL, FM, MC. Preparation of figure: LD. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
. Methodological details of the review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Devis, L., Catry, E., Honore, P.M. et al. Interventions to improve appropriateness of laboratory testing in the intensive care unit: a narrative review. Ann. Intensive Care 14, 9 (2024). https://doi.org/10.1186/s13613-024-01244-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01244-y