Abstract
Background
in COVID-19 acute respiratory failure, the effects of CPAP and FiO2 on respiratory effort and lung stress are unclear. We hypothesize that, in the compliant lungs of early Sars-CoV-2 pneumonia, the application of positive pressure through Helmet-CPAP may not decrease respiratory effort, and rather worsen lung stress and oxygenation when compared to higher FiO2 delivered via oxygen masks.
Methods
In this single-center (S.Luigi Gonzaga University-Hospital, Turin, Italy), randomized, crossover study, we included patients receiving Helmet-CPAP for early (< 48 h) COVID-19 pneumonia without additional cardiac or respiratory disease. Healthy subjects were included as controls. Participants were equipped with an esophageal catheter, a non-invasive cardiac output monitor, and an arterial catheter. The protocol consisted of a random sequence of non-rebreather mask (NRB), Helmet-CPAP (with variable positive pressure and FiO2) and Venturi mask (FiO2 0.5), each delivered for 20 min. Study outcomes were changes in respiratory effort (esophageal swing), total lung stress (dynamic + static transpulmonary pressure), gas-exchange and hemodynamics.
Results
We enrolled 28 COVID-19 patients and 7 healthy controls. In all patients, respiratory effort increased from NRB to Helmet-CPAP (5.0 ± 3.7 vs 8.3 ± 3.9 cmH2O, p < 0.01). However, Helmet’s pressure decreased by a comparable amount during inspiration (− 3.1 ± 1.0 cmH2O, p = 0.16), therefore dynamic stress remained stable (p = 0.97). Changes in static and total lung stress from NRB to Helmet-CPAP were overall not significant (p = 0.07 and p = 0.09, respectively), but showed high interpatient variability, ranging from − 4.5 to + 6.1 cmH2O, and from − 5.8 to + 5.7 cmH2O, respectively. All findings were confirmed in healthy subjects, except for an increase in dynamic stress (p < 0.01). PaO2 decreased from NRB to Helmet-CPAP with FiO2 0.5 (107 ± 55 vs 86 ± 30 mmHg, p < 0.01), irrespective of positive pressure levels (p = 0.64). Conversely, with Helmet’s FiO2 0.9, PaO2 increased (p < 0.01), but oxygen delivery remained stable (p = 0.48) as cardiac output decreased (p = 0.02). When PaO2 fell below 60 mmHg with VM, respiratory effort increased proportionally (p < 0.01, r = 0.81).
Conclusions
In early COVID-19 pneumonia, Helmet-CPAP increases respiratory effort without altering dynamic stress, while the effects upon static and total stress are variable, requiring individual assessment. Oxygen masks with higher FiO2 provide better oxygenation with lower respiratory effort.
Trial registration Retrospectively registered (13-May-2021): clinicaltrials.gov (NCT04885517), https://clinicaltrials.gov/ct2/show/NCT04885517.
Similar content being viewed by others
Background
Randomized controlled trials have suggested that CPAP may reduce the rate of intubation in COVID-19, without affecting mortality or length of stay [1,2,3,4]. However, these studies did not assess the effects of CPAP on respiratory effort and lung stress, which may contribute to the progression of lung injury [5, 6].
Theoretically, CPAP has the potential to alleviate respiratory effort and lung stress in acute respiratory failure (ARF) [7, 8], by improving oxygenation [9, 10] and lung recruitment [11]. However, early COVID-19 pneumonia may be characterized by ventilation-perfusion inequalities [12], with little alveolar collapse and, hence, low recruitability [13, 14]. In this context, CPAP may induce overdistention [6], whereas a higher FiO2 may provide adequate oxygenation and avoid potentially harmful effects of positive pressure.
Indeed, the few prospective investigations available in early COVID-19 pneumonia have suggested that CPAP does not reduce respiratory effort, nor the total lung stress [6, 15, 16]. However, CPAP was not compared with lower degrees of respiratory support (e.g., oxygen masks), and the isolated effects of FiO2 titration were not evaluated.
Here, in patients with early COVID-19 pneumonia, we used Helmet-CPAP and oxygen masks to investigate the effects of positive pressure and FiO2 on respiratory effort, lung stress, gas exchange and hemodynamics. We hypothesized that Helmet-CPAP would not reduce respiratory effort, and rather worsen lung stress and oxygenation when compared to oxygen masks with higher FiO2.
Methods
Experimental setting
This study was conducted in the COVID-19 High-Dependency Unit (HDU) of the University Hospital San Luigi Gonzaga, Orbassano-Turin (Italy) from February 1st to June 30th, 2021. Ethical approval (San Luigi Gonzaga 1565/2021) and trial registration (clinicaltrials.gov: NCT04885517) were obtained. The experimental procedure is summarized in Fig. 1.
Experimental procedure. A: Enrolment flowchart. Of note, 12 of the 28 COVID-19 patients were recruited prior to trial registration, but with ethics approval; B: experimental equipment and monitoring of (1) Helmet’s pressure (Paw) and (2) esophageal pressure (Pes) through OptiVent™ monitor, (3) arterial blood gases (ABG) through radial line, (4) blood pressure (BP), cardiac output (CO) and heart rate (HR) through CNAP® monitor consisting of a finger cuff and a brachial cuff; Panel C: experimental protocol
Inclusion and exclusion criteria
We included all confirmed SARS-CoV-2 patients with interstitial pneumonia (chest X-Ray or CT scan) who had been commenced on Helmet-CPAP by the treating clinicians within < 48 h (early pneumonia). We excluded patients with severe chronic pulmonary or cardiac disease, concomitant bacterial pneumonia, lobar or segmental pulmonary embolism at CT scan, or patients requiring immediate intubation (Additional file). Healthy volunteers were included as control group. All participants were non-sedated and provided written informed consent prior to enrolment.
Experimental equipment and monitoring systems
Participants were equipped with:
-
A nasogastric catheter with an esophageal balloon (NutriVent™) advanced 35–40 cm from the nostrils and filled with 4 ml of air as per manufacturer instructions.
-
A non-invasive device (CNAP® CNSystems-Medizintechnik-GmbH) for continuous arterial pressure and cardiac output measurement.
-
A radial artery catheter for blood-gas analysis (patients only).
Experimental protocol
In the seated decubitus (trunk at 60°, legs down at 45°), participants underwent a random sequence of 20 min steps:
-
(1)
Non-rebreather mask (NRB), 15 L/min, FiO2 ~ 0.9
-
(2)
Helmet-CPAP, 7 cmH2O, FiO2 0.9, 60–70 L/min
-
(3)
Helmet-CPAP, 7 cmH2O, FiO2 0.5, 60–70 L/min
-
(4)
Helmet-CPAP 12 cmH2O, FiO2 0.9, 60–70 L/min
-
(5)
Helmet-CPAP 12 cmH2O, FiO2 0.5, 60–70 L/min
-
(6)
Venturi mask (VM), 12 L/min, FiO2 ~ 0.5 (performed in only a subset of patients)
The levels of Helmet-CPAP (7 and 12 cmH2O) reflected our institution clinical guidance.
As all relevant variables except for the arterial oxygen tension (PaO2) and saturation (SaO2) were not significantly different between steps 2,3,4 and 5 (Additional file 1: Table S1), results related to these steps will be averaged and presented as a single step named “Helmet-CPAP”. PaO2 and SaO2 will be also presented relatively to single steps.
Measurements and calculations
The naso-gastric catheter (NutriVent™) and the Helmet (Dimar s.r.l.) were connected to a monitoring system (OptiVent™) continuously displaying esophageal and airway pressures. To ensure reproducibility, the esophageal balloon was deflated and reinflated before each measurement, and cardiac artifacts on the esophageal trace were sought to confirm its correct placement. At the end of each step, a stable breathing pattern for at least 2 minutes was sought before freezing the OptiVent™ monitor (Additional file 1: Figure S1). Esophageal and airway pressures were measured in five consecutive breaths and subsequently averaged. The work of breathing (WOB) scale [17], the Borg’s dyspnea scale [18], hemodynamics and blood gases were concomitantly evaluated.
Respiratory effort, the inspiratory Helmet’s pressure drop, and dynamic stress were computed, respectively, as the tidal swings in esophageal, airway, and their difference, i.e., the transpulmonary pressure [19]. The static stress associated with Helmet-CPAP was calculated as the change in end-expiratory transpulmonary pressure from NRB [20, 21]. Total stress was the sum of static and dynamic stress [6]. Oxygen delivery (DO2) was calculated from cardiac index and the arterial oxygen content [22]. All equations are reported in the Additional file 1.
Study outcomes
The main outcome was the effect of positive pressure (NRB vs Helmet-CPAP) on respiratory effort and lung stress. Secondary outcomes were the effects of positive pressure on gas-exchange and hemodynamics, and the isolated effects of FiO2 (NRB vs VM) on the same variables.
Sample size
Due to the physiological design of the study, and to the lack of comparable investigations at the time it was performed, a formal sample size was not calculated. Consistent with similar physiological studies [15, 16, 23, 24], we aimed to recruit a convenience sample size of 30 patients and 7 healthy controls.
Statistical analysis
Data are presented as mean ± standard deviation (SD). Normality was assessed with histograms and QQ plots, sphericity with Mauchly’s Tests. The effects of positive pressure (NRB vs Helmet-CPAP) and FiO2 (NRB vs VM) were assessed with paired Student’s t-test or Wilcoxon signed rank test as appropriate. Multiple steps were compared with one-way repeated measures ANOVA or its nonparametric equivalent the Friedman test. Appropriate post-hoc tests were corrected for multiple comparisons using Holm’s p adjustment method. Pearson’s r coefficient of linear regressions was used to evaluate correlations between variables. Two-sided p values < 0.05 were considered statistically significant. R studio version 4.2.2 was used for statistical analysis.
Results
A flowchart describing patients’ enrolment is available in Fig. 1. As shown, among the 30 patients enrolled, 2 withdrew their consent because of discomfort, thereby 28 were eventually studied. Their characteristics are reported in Table 1. All 7 healthy controls were successfully studied. This group will be described separately.
Effects of positive pressure (NRB vs Helmet-CPAP)
Respiratory effort and lung stress
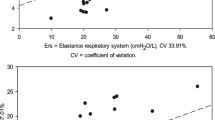
As shown in Table 2 and Fig. 2A, the esophageal swing increased in all but one patient from NRB to Helmet-CPAP (5.0 ± 3.7 vs 8.3 ± 3.9 cmH2O, p < 0.01), while clinical signs of effort (i.e., respiratory rate, the WOB scale, and the Borg dyspnea scale) were not affected by positive pressure. The increase in esophageal swing (3.3 ± 1.5 cmH2O) was paralleled by a comparable (p = 0.16) inspiratory drop in Helmet’s pressure (− 3.1 ± 1.0 cmH2O, Additional file 1: Figure S1), thereby dynamic stress remained stable (Fig. 2B). Similarly, the static lung stress did not significantly change from NRB to Helmet-CPAP, but a high variability was observed: the change ranged from − 4.5 to + 6.1 cmH2O, with a decrease in 10 patients (36%) and an increase in 18 patients (64%) (Fig. 2C). The total lung stress showed similar variability (range of change from − 5.8 to + 5.7 cmH2O), remaining overall stable from NRB to Helmet-CPAP (Fig. 2D).
Effects of positive pressure on respiratory effort and lung stress. Differences in respiratory effort (A), dynamic B, static C and total lung stress D between NRB and Helmet-CPAP in COVID-19 patients and Healthy subjects. Of note, measurement of airway pressure was missing in one patientBlack dots: single patients; Red bars: mean values; NRB Non-rebreather mask
Determinants of respiratory effort and lung stress
During NRB, respiratory effort was higher in patients with lower PaO2 (Additional file 1: Figure S2). The increase in respiratory effort from NRB to Helmet-CPAP correlated with the inspiratory Helmet’s pressure drop (Additional file 1: Figure S3). Conversely, neither the PaO2 nor the respiratory effort during NRB predicted changes in respiratory effort and lung stress due to the application of Helmet-CPAP (Additional file 1: Figure S4).
Gas exchange and hemodynamics
PaO2 decreased from NRB (107 ± 55 mmHg) to Helmet-CPAP with FiO2 0.5 (86 ± 30 mmHg), while it increased with Helmet-CPAP with FiO2 0.9 (232 ± 92 mmHg). Positive pressure levels (7 vs 12 cmH2O) did not affect the PaO2 (Fig. 3A). Cardiac index significantly decreased from NRB to Helmet-CPAP (Table 2), thereby oxygen delivery remained unchanged even when PaO2 increased (Fig. 3B).
Changes in PaO2 and DO2 with positive pressure and FiO2. Changes in PaO2 A and DO2 B between steps in COVID-19 patients; The overall p value for the change in PaO2 between the five steps was < 0.01 (not shown). Black dots: single patients; Boxplots: medians and interquartile ranges; PaO2 arterial oxygen tension. NRB Non-rebreather mask. DO2 oxygen delivery
Effects of FiO2 (NRB vs VM)
The VM step was available in 15 patients. Compared to NRB, PaO2 decreased, while respiratory effort, lung stress, and hemodynamics remained overall stable (Additional file 1: Table S2). However, when PaO2 fell below 60 mmHg, we observed an increase in respiratory effort proportional to the degree of hypoxemia (Fig. 4A).
Relationship between oxygenation and respiratory effort. A: relationship between PaO2 during VM, and the change in respiratory effort from VM to NRB (n = 15): only in patients with PaO2 < 60 mmHg (n = 8, red dots), a strong, significant relationship was found. B: relationship between PaO2 and respiratory effort with oxygen masks (NRB and, when available, VM); PaO2: arterial oxygen tension. NRB Non-rebreather mask, VM Venturi mask, AIC Akaike information criterion
Healthy controls
The seven healthy controls had a mean age of 30 ± 2 years, 2 (29%) were female, BMI was 22.2 ± 2.9 kg/m2. Table 2 and Fig. 2 report their response to Helmet-CPAP: the esophageal swing increased by 4.1 ± 1.3 cmH2O, and an inspiratory Helmet’s pressure drop was observed in all participants. The total lung stress increased by 3.1 ± 1.7 cmH2O, due to an increase in dynamic stress with an overall stable, but highly variable, static stress. The Helmet elicited expiratory abdominal contraction in 5 subjects, increasing the WOB scale. Cardiac output did not change with Helmet-CPAP.
Discussion
In this physiological study we investigated the effects of positive pressure and FiO2, delivered with Helmet-CPAP and oxygen masks, on respiratory effort, lung stress, gas-exchange and hemodynamics in early COVID-19 pneumonia. We found that:
-
(1)
Helmet-CPAP increases respiratory effort without altering dynamic stress;
-
(2)
The effect of Helmet-CPAP on static and total stress is highly variable;
-
(3)
High FiO2 has a greater impact than positive pressure on oxygenation;
-
(4)
FiO2 affects respiratory effort only in the most hypoxic conditions.
Helmet-CPAP increases respiratory effort without altering dynamic stress
To the best of our knowledge, this is the first study reporting a systematic increase in respiratory effort associated with the application of Helmet-CPAP. Furthermore, by measuring Helmet’s pressure, we could demonstrate a dissociation between the increased respiratory effort and an unaltered dynamic stress. This finding is new, as the two variables are generally considered equivalent during CPAP [6, 8, 15].
While the inability of Helmet-CPAP to reduce dynamic stress was previously reported [6, 15, 16], and likely reflects low potential for lung recruitment in early COVID-19 pneumonia [13, 14], the increase in esophageal swing is less intuitive. A possible explanation is that the Helmet added an inspiratory load by not maintaining its pressure throughout the respiratory cycle [25, 26]. Indeed, to generate pressure in our Helmets, we used spring-loaded adjustable valves, which have been shown to cause airway pressure instability, similar to the one we observed in this study [27]. Interestingly, Menga et al. reported an increasing trend in respiratory effort with Helmet-CPAP compared to high flow nasal oxygen, but airway pressure was not monitored [15]. Conversely, no other study investigating the effects of Helmet-CPAP on respiratory effort had a baseline esophageal swing available for comparison, as patients kept breathing through the Helmet even when CPAP was set at zero cmH2O [6, 16].
Although it would be tempting to solely ascribe the increase in esophageal swing to the concomitant inspiratory decrease in Helmet’s pressure, the correlation between the two variables was rather weak (r = 0.36, Additional file 1: Figure S2). Another contributing factor may be expiratory muscle activation to limit increases in end expiratory lung volume (EELV) [28,29,30,31]. Indeed, relaxation of expiratory muscles at the onset of inspiration would increase the esophageal swing, mimicking inspiratory effort [32]. Although a gastric pressure trace would be required for confirmation, the lower than expected static stress associated with Helmet-CPAP in our patients might support this hypothesis (see below).
The effect of Helmet-CPAP on static and total stress is highly variable
Static stress represents the static transpulmonary pressure associated with CPAP. It has been previously estimated from passive properties of the respiratory system (normal lung to chest wall elastance ratio: ER = 0.7) [6, 33]. However, in spontaneously breathing patients with possible expiratory muscles activation [28,29,30,31, 34], direct assessment of changes in end-expiratory transpulmonary pressure (PL(exp)), a proxy of changes in EELV [20, 21], might be a better option. Using this method, we found that Helmet-CPAP did not change static stress as would be predicted from the passive properties of the respiratory system (Additional file 1: Figure S5). Moreover, we observed a high variability between patients: some decreased or did not change static stress, suggesting expiratory muscle activation “protecting” their EELV [25, 28, 35]; others increased static stress, suggesting an increase in EELV. Such variability reflected on the total lung stress, which, overall, remained stable from NRB to Helmet-CPAP. This is at variance with previous studies estimating PL(exp) from passive properties of the respiratory system and concluding that Helmet-CPAP inevitably increased the static, and thereby total lung stress [6]. Our findings suggest that the effects of Helmet-CPAP on PL(exp) should be directly measured, as a high variability exists at a single patient level. Moreover, the response to Helmet-CPAP in terms of lung stress did not seem predictable from the baseline oxygenation or respiratory effort in our patients (Additional file 1: figure S4), further stressing the need for individualized assessment.
High FiO2 has a greater impact than positive pressure on oxygenation
The preponderant role of FiO2 over positive pressure in improving oxygenation in our patients is depicted in Fig. 3. Indeed, PaO2 decreased from NRB to Helmet-CPAP with FiO2 0.5, and was not affected by increasing CPAP levels. This is in line with ventilation-perfusion inequalities as major contributors to hypoxemia [12, 36], and with low potential for lung recruitment [13, 14] at this disease stage. Moreover, even with the higher PaO2 reached during Helmet-CPAP with FiO2 0.9, the concomitant decrease in cardiac output blunted any increase in oxygen delivery [22]. Taken together, these findings suggest that oxygen masks with high FiO2 provide better oxygenation than Helmet-CPAP in early COVID-19 pneumonia.
FiO2 affects respiratory effort only in the most hypoxic conditions
By altering FiO2 in the absence of positive pressure (NRB vs VM), we observed an increase in respiratory effort only when PaO2 fell below 60 mmHg (Fig. 4A). This supports that hypoxic drive plays a role only at very low oxygen tensions [9, 10, 37]. Indeed, the roughly hyperbolic relationship between respiratory effort and PaO2 in our patients (Fig. 4B) resembles that obtained from carotid bodies in vitro [10] (details can be found in the Additional file). Interestingly, despite the very low PaO2 reached during the VM step, no patient reported dyspnea, in line with the observed “silent hypoxemia” of early COVID-19 pneumonia [38].
Healthy subjects
The vast majority of our findings were confirmed in healthy subjects. Namely, the increase in esophageal swing, the inspiratory Helmet’s pressure drop, and the variable change in static stress with Helmet-CPAP. The visible contraction of abdominal muscles further suggests expiratory activation. The only notable difference in healthy controls was a significant increase in dynamic stress with Helmet-CPAP, suggesting that positive pressure might have increased their tidal volume, as previously reported [24, 39, 40].
Strengths and limitations
Strengths and novelties of this study are (1) the baseline step with oxygen masks, allowing detection of the inspiratory load added by the Helmet; (2) the contemporaneous measurement of esophageal and airway pressure, differentiating respiratory effort from dynamic stress during Helmet-CPAP; (3) the direct measurement of end-expiratory transpulmonary pressure to evaluate the static stress associated with Helmet-CPAP; (4) the simultaneous evaluation of blood gases and cardiac output to assess the effects of Helmet-CPAP on oxygen delivery; (5) the inclusion of a control group of healthy subjects. Limitations include the small sample size which, however, was similar to previous studies [15, 16, 23], in keeping with the complexity of these experiments. Other limitations are the lack of assessment of static lung volumes, tidal volume, inspiratory flow and gastric pressure, and the limited duration of the protocol steps (20 min): although this is similar to previous studies [6, 16], adaptation to CPAP (for example, reducing expiratory muscles activation) may require more time.
Conclusions
In early COVID-19 pneumonia, Helmet-CPAP increases respiratory effort, likely due to airway pressure instability during inspiration. A higher FiO2 with oxygen masks provides better oxygenation with lower respiratory effort. The dynamic lung stress is not reduced by Helmet-CPAP, questioning its role in alleviating lung injury at this disease stage. The response of static and, thereby, total lung stress to Helmet-CPAP is highly variable, and cannot be predicted from the passive properties of the respiratory system. Multimodal monitoring of esophageal and airway pressure, blood gases and cardiac output allows thorough evaluation of the appropriateness of respiratory support at a single patient level.
Availability of data and materials
The dataset is available from the corresponding author on reasonable request.
Abbreviations
- CPAP:
-
Continuous positive airway pressure
- FiO2 :
-
Inspired oxygen fraction
- NRB:
-
Non-rebreather mask
- VM:
-
Venturi mask
- COVID-19:
-
Coronavirus infectious disease-19
- ARF:
-
Acute respiratory failure
- EELV:
-
End expiratory lung volume
- ER :
-
Elastance ratio
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- SOFA:
-
Sequential organ failure assessment
- SpO2 :
-
Peripheral oxygen saturation
- ICU:
-
Intensive care unit
- WOB:
-
Work of breathing
- PaO2 :
-
Partial pressure of arterial oxygen
- SaO2 :
-
Percentage of hemoglobin saturated with arterial oxygen
- PaCO2 :
-
Partial pressure of arterial carbon dioxide
- CI:
-
Cardiac index
- DO2 :
-
Oxygen delivery
References
Perkins GD, Ji C, Connolly BA, Couper K, Lall R, Baillie JK, et al. Effect of noninvasive respiratory strategies on intubation or mortality among patients with acute hypoxemic respiratory failure and COVID-19: the recovery-rs randomized clinical trial. JAMA. 2022;327:546–58.
Grieco DL, Menga LS, Cesarano M, Rosà T, Spadaro S, Bitondo MM, et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA. 2021;325:1731–43.
Sakuraya M, Okano H, Masuyama T, Kimata S, Hokari S. Efficacy of non-invasive and invasive respiratory management strategies in adult patients with acute hypoxaemic respiratory failure: a systematic review and network meta-analysis. Crit Care. 2021;25:414.
Kumar V, Malik UA, Kumari R, Berkha KV, Kumar M, et al. Effectiveness of non-invasive respiratory support strategies in patients with COVID-19: a systematic review and meta analysis. Ann Med Surg. 2022;84:104827.
Yoshida T, Torsani V, Gomes S, De Santis RR, Beraldo MA, Costa ELV, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188:1420–7.
Coppola S, Chiumello D, Busana M, Giola E, Palermo P, Pozzi T, et al. Role of total lung stress on the progression of early COVID-19 pneumonia. Intensive Care Med. 2021;47:1130–9.
Cesarano M, Grieco DL, Michi T, Munshi L, Menga LS, Delle Cese L, et al. Helmet noninvasive support for acute hypoxemic respiratory failure: rationale, mechanism of action and bedside application. Ann Intensive Care. 2022;12:94.
Grieco DL, Maggiore SM, Roca O, Spinelli E, Patel BK, Thille AW, et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med. 2021;47:851–66.
Dripps RD, Comroe JH. The effect of the inhalation of high and low oxygen concentrations on respiration, pulse rate, ballistocardiogram and arterial oxygen saturation (oximeter) of normal individuals. Am J Physiol. 1947;149:277–91.
López-Barneo J, González-Rodríguez P, Gao L, Fernández-Agüera MC, Pardal R, Ortega-Sáenz P. Oxygen sensing by the carotid body: mechanisms and role in adaptation to hypoxia. Am J Physiol Cell Physiol. 2016;310:C629-642.
Morais CCA, Koyama Y, Yoshida T, Plens GM, Gomes S, Lima CAS, et al. High positive end-expiratory pressure renders spontaneous effort noninjurious. Am J Respir Crit Care Med. 2018;197:1285–96.
Busana M, Giosa L, Cressoni M, Gasperetti A, Di Girolamo L, Martinelli A, et al. The impact of ventilation-perfusion inequality in COVID-19: a computational model. J Appl Physiol. 1985;2021(130):865–76.
Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–102.
Pan C, Chen L, Lu C, Zhang W, Xia J-A, Sklar MC, et al. Lung recruitability in COVID-19–associated acute respiratory distress syndrome: a single-center observational study. Am J Respir Crit Care Med. 2020;201:1294–7.
Menga LS, delle Cese L, Rosà T, Cesarano M, Scarascia R, Michi T, et al. Respective effects of helmet pressure support, continuous positive airway pressure and nasal high-flow in hypoxemic respiratory failure: a randomized crossover clinical trial. Am J Respir Crit Care Med. 2023;207:1310–23.
Lassola S, Miori S, Sanna A, Menegoni I, De Rosa S, Bellani G, et al. Assessment of inspiratory effort in spontaneously breathing COVID-19 ARDS patients undergoing helmet CPAP: a comparison between esophageal, transdiaphragmatic and central venous pressure swing. Diagnostics. 2023;13:1965.
Apigo M, Schechtman J, Dhliwayo N, Al Tameemi M, Gazmuri RJ. Development of a work of breathing scale and monitoring need of intubation in COVID-19 pneumonia. Crit Care. 2020;24:477.
Borg GV. Psychophysical bases of perceived exertion. Med Sci Sports Exercise. 1982;14:377.
Gattinoni L, Giosa L, Bonifazi M, Pasticci I, Busana M, Macri M, et al. Targeting transpulmonary pressure to prevent ventilator-induced lung injury. Expert Rev Respir Med. 2019;13:737–46.
Schlobohm RM, Falltrick RT, Quan SF, Katz JA. Lung volumes, mechanics, and oxygenation during spontaneous positive-pressure ventilation: the advantage of CPAP over EPAP. Anesthesiology. 1981;55:416–22.
Layon J, Banner MJ, Jaeger MJ, Peterson CV, Gallagher TJ, Modell JH. Continuous positive airway pressure and expiratory positive airway pressure increase functional residual capacity equivalently. Chest. 1986;89:517–21.
Barthélémy R, Beaucoté V, Bordier R, Collet M, Gall AL, Hong A, et al. Haemodynamic impact of positive end-expiratory pressure in SARS-CoV-2 acute respiratory distress syndrome: oxygenation versus oxygen delivery. Br J Anaesth. 2021;126:e70–2.
Tonelli R, Busani S, Tabbì L, Fantini R, Castaniere I, Biagioni E, et al. Inspiratory effort and lung mechanics in spontaneously breathing patients with acute respiratory failure due to covid-19: a matched control study. Am J Respir Crit Care Med. 2021;204:725–8.
Patroniti N, Foti G, Manfio A, Coppo A, Bellani G, Pesenti A. Head helmet versus face mask for non-invasive continuous positive airway pressure: a physiological study. Intensive Care Med. 2003;29:1680–7.
Katz J, Kraemer R, Gjerde G. Inspiratory work and airway pressure with continuous positive airway pressure delivery systems. Chest. 1985;88:519–26.
L’Her E, Deye N, Lellouche F, Taille S, Demoule A, Fraticelli A, et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med. 2005;172:1112–8.
Isgrò S, Zanella A, Giani M, El Aziz Abd, El Sayed DS, Pesenti A, Patroniti N. Performance of different PEEP valves and helmet outlets at increasing gas flow rates: a bench top study. Minerva Anestesiol. 2012;78:1095–100.
Shi Z-H, Jonkman A, de Vries H, Jansen D, Ottenheijm C, Girbes A, et al. Expiratory muscle dysfunction in critically ill patients: towards improved understanding. Intensive Care Med. 2019;45:1061–71.
Gothe B, Cherniack NS. Effects of expiratory loading on respiration in humans. J Appl Physiol. 1980;49:601–8.
Martin JG, De Troyer A. The behaviour of the abdominal muscles during inspiratory mechanical loading. Respir Physiol. 1982;50:63–73.
Jansen D, Jonkman AH, de Vries HJ, Wennen M, Elshof J, Hoofs MA, et al. Positive end-expiratory pressure affects geometry and function of the human diaphragm. J Appl Physiol. 1985;2021(131):1328–39.
Lessard MR, Lofaso F, Brochard L. Expiratory muscle activity increases intrinsic positive end-expiratory pressure independently of dynamic hyperinflation in mechanically ventilated patients. Am J Respir Crit Care Med. 1995;151:562–9.
Weaver L, Das A, Saffaran S, Yehya N, Chikhani M, Scott TE, et al. Optimising respiratory support for early COVID-19 pneumonia: a computational modelling study. Br J Anaesth. 2022;128:1052–8.
Chandra A, Coggeshall JW, Ravenscraft SA, Marini JJ. Hyperpnea limits the volume recruited by positive end-expiratory pressure. Am J Respir Crit Care Med. 1994;150:911–7.
Gherini S, Peters RM, Virgilio RW. Mechanical work on the lungs and work of breathing with positive end-expiratory pressure and continuous positive airway pressure. Chest. 1979;76:251–6.
Giosa L, Payen D, Busana M, Mattei A, Brazzi L, Caironi P. Orthodeoxia and its implications on awake-proning in COVID-19 pneumonia. Crit Care. 2021;25:429.
Vaporidi K, Akoumianaki E, Telias I, Goligher EC, Brochard L, Georgopoulos D. Respiratory drive in critically Ill patients. pathophysiology and clinical implications. Am J Respir Crit Care Med. 2020;201:20–32.
Busana M, Gasperetti A, Giosa L, Forleo GB, Schiavone M, Mitacchione G, et al. Prevalence and outcome of silent hypoxemia in COVID-19. Minerva Anestesiol. 2021;87:325–33.
Urbscheit N, Bishop B, Bachofen H. Immediate effects of continuous positive pressure breathing on abdominal expiratory activity, minute ventilation, and end-tidal P CO2 of conscious man. Phys Ther. 1973;53:258–66.
Xiao S, Lu Y, Guo H-X, Qiu Z, Luo Y. Effect of expiratory load on neural inspiratory drive. Chin Med J (Engl). 2012;125:3629–34.
Acknowledgements
Not Applicable.
Funding
No part of the work presented has received financial support from any source.
Author information
Authors and Affiliations
Contributions
LG, PC and AP designed the study; LG, MS, FC, SDB, MMM, LD, AL, FG, RP and MM performed the protocol; LG, IS, PDC and VR analyzed the data, prepared the tables and formulated the figures; LC and GB contributed to the interpretation of the findings; LG, PC, LC, PDC and GB drafted the manuscript which was then critically revised and approved by all authors. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the local authority (San Luigi Gonzaga 1565/202). The study was performed according to local ethical standards and to the Helsinki Declaration of 1957. All participants signed a written informed consent prior to enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. Esophageal and airway pressure measurement. Figure S2. Relationship between PaO2 and respiratory effort with NRB. Figure S3. Relationship between the Helmet’s inspiratory pressure drop and the increase in respiratory effort from NRB to Helmet-CPAP. Figure S4. Relationship between PaO2 or respiratory effort with NRB and changes in respiratory effort or lung stress from NRB to Helmet-CPAP. Figure S5. Measured vs estimated static stress. Table S1. Invariance of variables during Helmet-CPAP steps. Table S2. Effects of FiO2 (NRB vs VM).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giosa, L., Collins, P.D., Sciolla, M. et al. Effects of CPAP and FiO2 on respiratory effort and lung stress in early COVID-19 pneumonia: a randomized, crossover study. Ann. Intensive Care 13, 103 (2023). https://doi.org/10.1186/s13613-023-01202-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01202-0