Abstract
Background
Acute hypoxemic respiratory failure (AHRF) is a leading concern in critically ill patients. Experimental and clinical data suggest that early sedation with volatile anesthestics may improve arterial oxygenation and reduce the plasma and alveolar levels of markers of alveolar epithelial injury and of proinflammatory cytokines.
Methods
An a priori hypothesis substudy of a multicenter randomized controlled trial (The Sedaconda trial, EUDRA CT Number 2016-004551-67). In the Sedaconda trial, 301 patients on invasive mechanical ventilation were randomized to 48 h of sedation with isoflurane or propofol in a 1:1 ratio. For the present substudy, patients with a ratio of arterial pressure of oxygen (PaO2) to inspired fraction of oxygen (FiO2), PaO2/FiO2, of ≤ 300 mmHg at baseline were included (n = 162). The primary endpoint was the change in PaO2/FiO2 between baseline and the end of study sedation. A subgroup analysis in patients with PaO2/FiO2 ≤ 200 mmHg was performed (n = 82).
Results
Between baseline and the end of study sedation (48 h), oxygenation improved to a similar extent in the isoflurane vs. the propofol group (isoflurane: 199 ± 58 to 219 ± 76 mmHg (n = 70), propofol: 202 ± 62 to 236 ± 77 mmHg (n = 89); p = 0.185). On day seven after randomization, PaO2/FiO2 was 210 ± 79 mmHg in the isoflurane group (n = 41) and 185 ± 87 mmHg in the propofol group (n = 44; p = 0.411). In the subgroup of patients with PaO2/FiO2 ≤ 200 mmHg, PaO2/FiO2 increase between baseline and end of study sedation was 152 ± 33 to 186 ± 54 mmHg for isoflurane (n = 37), and 150 ± 38 to 214 ± 85 mmHg for propofol (n = 45; p = 0.029). On day seven, PaO2/FiO2 was 198 ± 69 mmHg in patients randomized to isoflurane (n = 20) and 174 ± 106 mmHg in patients randomized to propofol (n = 20; p = 0.933). Both for the whole study population and for the subgroup with PaO2/FiO2 ≤ 200 mmHg, no significant between-group differences were observed for PaCO2, pH and tidal volume as well as 30-day mortality and ventilator-free days alive.
Conclusions
In patients with AHRF, inhaled sedation with isoflurane for a duration of up to 48 h did not lead to improved oxygenation in comparison to intravenous sedation with propofol.
Trial registration The main study was registered in the European Medicines Agency’s EU Clinical Trial register (EudraCT), 2016-004551-67, before including the first patient. The present substudy was registered at German Clinical Trials Register (DRKS, ID: DRKS00018959) on January 7th, 2020, before opening the main study data base and obtaining access to study results.
Similar content being viewed by others
Background
Long before the onset of the current Covid-19 pandemic, the acute respiratory distress syndrome (ARDS) has been recognized as a major cause of morbidity and mortality in critically ill patients [1, 2]. ARDS is defined as acute hypoxemic respiratory failure (AHRF) of non-cardiac origin with a ratio of arterial partial pressure of oxygen (PaO2) to inspired fraction of oxygen (FiO2), PaO2/FiO2 ratio, of less than or equal to 300 mmHg in combination with bilateral opacities on chest X-ray, or CT scan not fully explained by cardiac failure or fluid overload [3]. A recent secondary analysis of the LUNG SAFE study found that AHRF with unilateral opacities or congestive heart failure carries a similar prognosis, even though it does not meet all criteria for ARDS [4].
Since many patients with AHRF require invasive ventilation, some level of sedation may be necessary to establish and maintain endotracheal tube tolerance and to control respiratory drive [5]. According to national and international guidelines, intravenous drugs like propofol, benzodiazepines or alpha-2-agonists are preferably used in this context [6]. As an alternative to intravenous sedatives, the use of volatile anaesthetic agents has gained importance in the recent decades [7, 8].
In addition to their favourable pharmacokinetic properties for sedation, volatile anaesthetics may have particularly favourable effects in patients with or at risk for AHRF, reducing endotoxin-induced lung injury [9, 10] as well as ventilator-induced lung injury [11] and contribute to maintaining the integrity of the alveolar–capillary barrier [12].
In a pilot study, Jabaudon and co-workers randomized 50 patients with moderate-to-severe ARDS to sedation with sevoflurane or midazolam in a 1:1 ratio. 48 h after randomization, they found improved oxygenation and decreased levels of the soluble receptor for advanced glycation end-products (sRAGE), a marker of epithelial injury, with sevoflurane in comparison to midazolam [13].
In the recently published Sedaconda randomized trial [14], 301 patients who received invasive ventilation for various reasons were randomized in a 1:1 ratio to 48 h of sedation with isoflurane or propofol. The Sedaconda trial primarily investigated sedation efficacy and safety, including mechanically ventilated adult patients who were expected to require continuous invasive ventilation and sedation for at least 24 h following randomization and has since then led to European market approval of isoflurane for sedation of patients requiring invasive mechanical ventilation.
ARDS or AHRF were no inclusion criteria in the Sedaconda trial and the influence of volatile anaesthetics on gas exchange and duration of invasive mechanical ventilation in patients with PaO2/FiO2 ≤ 300 mmHg was not studied. Nevertheless, we expected that a considerable number of patients included in this present study would be suffering from ARDS or AHRF. We therefore conceived a substudy to examine the effects of inhaled sedation with isoflurane on gas exchange and other outcome parameters in patients with PaO2/FiO2 ≤ 300 mmHg randomized in the Sedaconda trial.
Methods
An a priori hypothesis substudy of a multicenter randomized controlled trial (the Sedaconda trial, 12). In this trial, patients who had been on invasive mechanical ventilation and sedated with propofol for less than 48 h were randomized to 48 h of sedation with isoflurane or propofol in a 1:1 ratio. For the present substudy, patients with a PaO2/FiO2 ratio ≤ 300 mmHg at baseline (before randomization) were included.
Study endpoints
The primary endpoint studied was the change in PaO2/FiO2 between baseline and the end of study sedation (end ot treatment, EOT, as assessed from the last arterial blood gas (ABG) sample taken before the end of study sedation, usually after 48 h).
Secondary outcome parameters included 30-day mortality, ventilator-free days alive during the first 30 days after randomization, arterial partial pressure of carbon dioxide (PaCO2) and pH at end of study sedation, PaO2/FiO2 (worst value within 24 h) at day seven after randomization, time to extubation in 30-day survivors, the average odds of achieving assisted spontaneous breathing assessed by applied ventilator mode, and the average tidal volume (VT) delivered.
A prespecified subgroup analysis was also performed of the predefined outcome parameters in patient with PaO2/FiO2 of ≤ 200 mmHg.
Statistical analysis
A partial post hoc power analysis was performed to analyse the power of this substudy for detecting statistical significance of a clinically relevant difference in PaO2/FiO2 ratio of 40 mmHg between isoflurane and propofol (similar to the difference detected by Jabaudon et al.), using the actually observed pooled PaO2/FiO2 ratio standard deviation and treatment group sizes of this substudy.
Numerical results are presented as mean ± standard deviation unless specified otherwise.
For numerical endpoints presented in the manuscript, change from baseline was analysed by selected key visits using mixed-effects models with treatment group as fixed effect and centre/pseudo-centre as a random effect. The Sedaconda study was randomized by centre and as for the study report, the centre/pseudo-centre effect were included in analysis models used for this manuscript. Pseudo-centres were established to avoid small strata in the analyses. This was managed by merging sites with less than ten patients into pseudo-centres, by site type. The site types were defined prior to database lock. Site types in the study were: Neurological ICU, Surgery ICU, Internal medicine ICU and General or other. For analysing the primary endpoint, our substudy solely focused on delta between baseline and end of study sedation, not taking into account other timepoints in between. If one PaO2/FiO2 ratio at end of study sedation was missing, we used the next available value within a time frame of ± 12 h. If PaO2/FiO2 ratio was not available at end of study sedation ± 12 h, the patient was excluded from the substudy.
Mortality and time to extubation were analysed using the log-rank tests and the comparisons are presented using Kaplan–Meier curves.
Proportion of ventilator-free days alive during the 30 days after randomization was analysed using a mixed-effects model with treatment group as fixed effect and centre/pseudo-centre as a random effect.
Assisted spontaneous breathing was analysed in terms of the odds for a patient achieving the event, assessed from applied ventilator mode.
To assess the on average advantage of isoflurane over propofol, regarding the likelihood of spontaneous breathing across repeated measurements, a generalized linear mixed-effects model (GLMM) with a logistic link function was used.
In the GLMM, the repeated dichotomous assessments (Spontaneous breathing: Yes/No) were modelled using the following explanatory variables: treatment group, timepoint (every 4 h) and timepoint*treatment group interaction. Pseudo-centre was added to the model as a random effect.
An autoregressive covariance structure was used to model the within-subject error.
Results
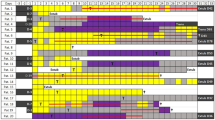
Out of 301 patients who had been randomized in the Sedaconda trial [12], a total of 162 patients (72 in the isoflurane group, 90 in the propofol group) fulfilled the criterion of PaO2/FiO2 ≤ 300 mmHg at baseline and were thus included in the present substudy. Baseline patient characteristics were balanced between study groups (Table 1). 82 patients had a PaO2/FiO2 ratio ≤ 200 mmHg (37 in the isoflurane group, 45 in the propofol group). The average duration of study treatment was 38 ± 12 h. Patient flow is depicted in Fig. 1.
Oxygenation from baseline to the end of study sedation improved to a similar extent in the isoflurane vs. the propofol group and was 20 vs. 34 mmHg (p = 0.185; isoflurane: 199 ± 58 to 219 ± 76 mmHg, propofol: 202 ± 62 to 236 ± 77 mmHg). On day seven after randomization, oxygenation was still similar (isoflurane: 210 ± 79 mmHg vs. propofol: 185 ± 87 mmHg; p = 0.411).
The partial post hoc power analysis resulted in an estimated power for detecting a clinically relevant difference of 40 mmHg in PaO2/FiO2 ratio between isoflurane and propofol of 90.1%.
We found no between-group differences in 30-day mortality (Fig. 2), ventilator-free days alive during the first 30 days (15.8 ± 11.9 with isoflurane vs. 15.9 ± 12.0 with propofol, p = 0.931), PaCO2 and pH at end of study sedation, time to extubation (Fig. 3) and tidal volume (Table 2).
The odds ratio for successfully achieving assisted spontaneous breathing with isoflurane was 1.596 (95% CI 0.880–2.897; p = 0.123) and 1.382 (95% CI 0.690–2.768, p = 0.358) for the first and second 24 h of study treatment, respectively.
In the subgroup of patients with PaO2/FiO2 ≤ 200 mmHg, the increase in PaO2/FiO2 ratio between baseline and end of study sedation was 152 ± 33 to 186 ± 54 mmHg with isoflurane, and 150 ± 38 to 214 ± 85 mmHg with propofol (p = 0.029). At day seven after randomization, PaO2/FiO2 was 198 ± 69 mmHg in the isoflurane group and 174 ± 106 mmHg in the propofol group (p = 0.933). All other respiratory parameters did not significantly differ between both groups as shown in Table 3.
In this subgroup, the respective odds ratios for successfully achieving assisted spontaneous breathing with isoflurane during the first 24 and second 24 h of study treatment were 1.722 (95% CI 0.729–4.069; p = 0.212) and 1.355 (95% CI 0.492–3.735, p = 0.552).
Discussion
There were no significant differences in arterial oxygenation between propofol and isoflurane in patients with baseline PaO2/FiO2 ≤ 300 mmHg. There were also no significant differences pH, pCO2, VT, mortality and ventilator-free days. In the subgroup of patients with baseline PaO2/FiO2 ≤ 200 mmHg, however, there was a significantly lower PaO2/FiO2 ratio with isoflurane as compared to propofol. During the 7-day follow-up, no significant differences in oxygenation were observed in the study population as well as the subgroup with baseline PaO2/FiO2 ≤ 200 mmHg. This observed difference in oxygenation subsided during the first 5 days after the end of study treatment.
The findings are in contrast to the ones by Jabaudon et al., who found better oxygenation and lower levels of sRAGE (a marker of endothelial damage) in ARDS patients sedated with sevoflurane in comparison to midazolam [13]. Multiple possible reasons for this have to be taken into account. First of all Jabaudon et al. were using sevoflurane in contrast to isoflurane in our study. Most previous investigations demonstrating lung-protective effects of volatile anaesthetics were conducted with sevoflurane [13, 15, 16]. Sevoflurane is the only volatile agent that is transformed in a phase II-reaction in about 3–5% into hexafluoro-2-propanol (HFIP) and fluoride. Especially HFIP has shown immunomodulatory effects in both in vitro and animal studies from Urner et al. [17]. These effects have not been demonstrated for isoflurane and its metabolites. Laboratory studies have shown that sevoflurane alters the lipopolysaccharide-induced inflammatory response by downregulation of chemokines and adhesion molecules [18] and decreases the inflammatory response of alveolar macrophages [19].
Another reason for the differing results could be the etiologies and severity of ARDS/AHRF. At least 80% of the patients included in the study by Jabaudon et al. [13] suffered from pneumonia, with a significantly lower PaO2/FiO2 ratio at inclusion in contrast to our patients. Additionally, our SAPS-II was almost 10 points lower demonstrating a reduced severity of illness in our population.
In an animal study investigating the effects of isoflurane and sevoflurane in pulmonary and extrapulmonary ARDS, Araújo and co-workers found that in pulmonary, but not in extrapulmonary ARDS, sevoflurane reduced interleukin-6 expression, improved respiratory mechanics, led to increased expression of regulators protecting against oxidative stress and epithelial damage and reduced alveolar collapse to a greater degree than isoflurane [20]. This could partly explain our results because it can be assumed that a significant proportion of patients included in our substudy suffered from pulmonary ARDS.
In summary, our results imply that inhaled sedation with isoflurane may not have the same pulmonary protective effects as sevoflurane.
Another plausible explanation for our results is that the lung-protective effects of possible effects of isoflurane inhalation sedation were offset by adverse effects of isoflurane on hypoxic pulmonary vasoconstriction. In comparison to different types of volatile anaesthetics, reductions in shunt volume and increases in oxygenation have been demonstrated for various intravenous sedatives including propofol, diazepam and sodium thiopental [21,22,23]. This is in line with the results of a study conducted by Abe et al., where propofol improved oxygenation and decreased shunt fraction during one-lung ventilation compared with volatile anaesthetics [24].
Strengths
This substudy investigated a comparatively large sample of 162 patients with AHRF randomized to isoflurane or propofol. The partial post hoc power analysis revealed the power of the study for detecting statistical significance of a difference in PaO2/FiO2 ratio of 40 mmHg (as observed by Jabaudon et al. [12]) to be above 90%. Baseline patient characteristics as well as ventilator settings were well-balanced between groups. In addition to the official registration of the Sedaconda trial in the EudraCT database, the present substudy was registered in the German Clinical Trials Registry before opening the study database, minimizing the risk for data selection bias.
Limitations
This study has certain limitations. As this was a substudy of a larger randomized controlled trial, no a priori sample size calculation could be performed. Even though the partial post hoc power analysis revealed the power of the study for detecting statistical significance of a difference in PaO2/FiO2 ratio of 40 mmHg between isoflurane and propofol to be 0.901, this substudy may be underpowered for detecting smaller differences in PaO2/FiO2. In contrast to the study of Jabaudon et al. [13], plasma levels of sRAGE or other markers of endothelial injury were not assessed in our study. Therefore, we had to rely on changes in oxygenation as primary endpoint, a potentially weak surrogate for epi- or endothelial damage that may have been confounded by the possibly opposing effects of isoflurane on hypoxic pulmonary vasoconstriction. The duration of study drug administration was relatively short and the exposure time to isoflurane may have been too short to lead to a clinically manifest reduction in ventilator-induced lung injury. Important ventilation parameters such as respiratory system compliance, airway resistance and presence or absence of auto-PEEP could not be evaluated for the present substudy, as they were not recorded in the main Sedaconda study.
As chest X-ray data were not available for this substudy, we were unable to determine the exact number of patients who met ARDS criteria as defined by the Berlin definition. Even though AHRF due to pneumonia with unilateral opacities or due to congestive heart failure carries a similar prognosis [4], it may still differ from ARDS in pathophysiology. Therefore, a study including only ARDS patients might have resulted in different findings. Moreover, we cannot exclude the possibility that some patients with chronic respiratory impairment may have been included in the present substudy.
Conclusions
In conclusion, the results show that in patients with ARDS or AHRF, inhaled sedation with isoflurane for a duration of up to 48 h does not lead to improved oxygenation in comparison to intravenous sedation with propofol.
Availability of data and materials
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Abbreviations
- ABG:
-
Arterial blood gas
- ARDS:
-
Acute respiratory distress syndrome
- ΔP:
-
Driving pressure
- FiO2:
-
Inspired fraction of oxygen
- HFIP:
-
Hexafluoro-2-propanol
- HPV:
-
Hypoxic pulmonary vasoconstriction
- HR:
-
Heart rate
- ICU:
-
Intensive care unit
- PaCO2:
-
Arterial partial pressure of carbon dioxide
- PaO2:
-
Arterial partial pressure of oxygen
- PEEP:
-
Positive end-expiratory pressure
- RR:
-
Respiratory rate
- VT:
-
Tidal volume
References
Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1334–49. https://doi.org/10.1056/NEJM200005043421806.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, Ranieri M, Rubenfeld G, Thompson BT, Wrigge H, Slutsky AS, Pesenti A, LUNG SAFE Investigators ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. https://doi.org/10.1001/jama.2016.0291.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS, ARDS Definition Task Force. Acute respiratory distress syndrome the Berlin Definition. JAMA. 2012;307(23):2526–33. https://doi.org/10.1001/jama.2012.5669.
Pham T, Pesenti A, Bellani G, Rubenfeld G, Fan E, Bugedo G, Lorente JA, Fernandes ADV, Van Haren F, Bruhn A, Rios F, Esteban A, Gattinoni L, Larsson A, McAuley DF, Ranieri M, Thompson BT, Wrigge H, Brochard LJ, Laffey JG, LUNG SAFE Investigators and the European Society of Intensive Care Medicine Trials Group. Outcome of acute hypoxaemic respiratory failure: insights from the LUNG SAFE Study. Eur Respir J. 2021;57(6):2003317. https://doi.org/10.1183/13993003.03317-2020.
Chanques G, Constantin JM, Devlin JW, Ely EW, Fraser GL, Gélinas C, Girard TD, Guérin C, Jabaudon M, Jaber S, Mehta S, Langer T, Murray MJ, Pandharipande P, Patel B, Payen JF, Puntillo K, Rochwerg B, Shehabi Y, Strøm T, Olsen HT, Kress JP. Analgesia and sedation in patients with ARDS. Intensive Care Med. 2020;46(12):2342–56. https://doi.org/10.1007/s00134-020-06307-9.
Müller A, Weiß B, Spies CD. Symptomatic treatment of delirium, anxiety and stress, and protocol based analgesia, sedation and management of sleep in intensive care patients. Anasthesiol Intensivmed Notfallmed Schmerzther. 2015;50(12):698–703. https://doi.org/10.1055/s-0041-107321.
Sackey PV, Martling CR, Granath F, Radell PJ. Prolonged isoflurane sedation of intensive care unit patients with the Anesthetic Conserving Device. Crit Care Med. 2004;32(11):2241–6. https://doi.org/10.1097/01.ccm.0000145951.76082.77.
Bellgardt M, Bomberg H, Herzog-Niescery J, Dasch B, Vogelsang H, Weber TP, Steinfort C, Uhl W, Wagenpfeil S, Volk T, Meiser A. Survival after long-term isoflurane sedation as opposed to intravenous sedation in critically ill surgical patients: retrospective analysis. Eur J Anaesthesiol. 2016;33(1):6–13. https://doi.org/10.1097/EJA.0000000000000252.
Reutershan J, Chang D, Hayes JK, Ley K. Protective effects of isoflurane pretreatment in endotoxin-induced lung injury. Anesthesiology. 2006;104(3):511–7. https://doi.org/10.1097/00000542-200603000-00019.
Fortis S, Spieth PM, Lu WY, Parotto M, Haitsma JJ, Slutsky AS, Zhong N, Mazer CD, Zhang H. Effects of anesthetic regimes on inflammatory responses in a rat model of acute lung injury. Intensive Care Med. 2012;38(9):1548–55. https://doi.org/10.1007/s00134-012-2610-4.
Faller S, Strosing KM, Ryter SW, Buerkle H, Loop T, Schmidt R, Hoetzel A. The volatile anesthetic isoflurane prevents ventilator-induced lung injury via phosphoinositide 3-kinase/Akt signaling in mice. Anesth Analg. 2012;114(4):747–56. https://doi.org/10.1213/ANE.0b013e31824762f0.
Englert JA, Macias AA, Amador-Munoz D, Pinilla Vera M, Isabelle C, Guan J, Magaoay B, Suarez Velandia M, Coronata A, Lee A, Fredenburgh LE, Culley DJ, Crosby G, Baron RM. Isoflurane ameliorates acute lung injury by preserving epithelial tight junction integrity. Anesthesiology. 2015;123(2):377–88. https://doi.org/10.1097/ALN.0000000000000742.
Jabaudon M, Boucher P, Imhoff E, Chabanne R, Faure JS, Roszyk L, Thibault S, Blondonnet R, Clairefond G, Guérin R, Perbet S, Cayot S, Godet T, Pereira B, Sapin V, Bazin JE, Futier E, Constantin JM. Sevoflurane for sedation in acute respiratory distress syndrome a randomized controlled pilot study. Am J Respir Crit Care Med. 2017;195(6):792–800. https://doi.org/10.1164/rccm.201604-0686OC.
Meiser A, Volk T, Wallenborn J, Guenther U, Becher T, Bracht H, Schwarzkopf K, Knafelj R, Faltlhauser A, Thal SC, Soukup J, Kellner P, Drüner M, Vogelsang H, Bellgardt M, Sackey P, Sedaconda study group. Inhaled isoflurane via the anaesthetic conserving device versus propofol for sedation of invasively ventilated patients in intensive care units in Germany and Slovenia: an open-label, phase 3, randomised controlled, non-inferiority trial. Lancet Respir Med. 2021;S2213–2600(21):00323–4. https://doi.org/10.1016/S2213-2600(21)00323-4.
Kellner P, Müller M, Piegeler T, Eugster P, Booy C, Schläpfer M, Beck-Schimmer B. Sevoflurane abolishes oxygenation impairment in a long-term rat model of acute lung injury. Anesth Analg. 2017;124(1):194–203. https://doi.org/10.1213/ANE.0000000000001530.
Voigtsberger S, Lachmann RA, Leutert AC, Schläpfer M, Booy C, Reyes L, Urner M, Schild J, Schimmer RC, Beck-Schimmer B. Sevoflurane ameliorates gas exchange and attenuates lung damage in experimental lipopolysaccharide-induced lung injury. Anesthesiology. 2009;111(6):1238–48. https://doi.org/10.1097/ALN.0b013e3181bdf857.
Urner M, Schläpfer M, Herrmann IK, Hasler M, Schimmer RR, Booy C, Roth Z’graggen B, Rehrauer H, Aigner F, Minshall RD, Stark WJ, Beck-Schimmer B. Insight into the beneficial immunomodulatory mechanism of the sevoflurane metabolite hexafluoro-2-propanol in a rat model of endotoxaemia. Clin Exp Immunol. 2015;181(3):468–79. https://doi.org/10.1111/cei.12648.
Suter D, Spahn DR, Blumenthal S, Reyes L, Booy C, Zgraggen BR, Beck-Schimmer B. The immunomodulatory effect of sevoflurane in endotoxin-injured alveolar epithelial cells. Anesth Analg. 2007;104(3):638–45. https://doi.org/10.1213/01.ane.0000255046.06058.58.
Steurer M, Schläpfer M, Steurer M, Zgraggen BR, Booy C, Reyes L, Spahn DR, Beck-Schimmer B. The volatile anaesthetic sevoflurane attenuates lipopolysaccharide-induced injury in alveolar macrophages. Clin Exp Immunol. 2009;155(2):224–30. https://doi.org/10.1111/j.1365-2249.2008.03807.x.
Araújo MN, Santos CL, Samary CS, Heil LBB, Cavalcanti VCM, Cruz FF, Felix NS, Silva JD, Morales MM, Pelosi P, Fernandes FC, Villela NR, Silva PL, Rocco PRM. Sevoflurane, compared with isoflurane, minimizes lung damage in pulmonary but not in extrapulmonary acute respiratory distress syndrome in rats. Anesth Analg. 2017;125(2):491–8. https://doi.org/10.1213/ANE.0000000000001927.
Marshall C, Lindgren L, Marshall BE. Effects of halothane, enflurane, and isoflurane on hypoxic pulmonary vasoconstriction in rat lungs in vitro. Anesthesiology. 1984;60(4):304–8. https://doi.org/10.1097/00000542-198404000-00006.
Benumof JL, Augustine SD, Gibbons JA. Halothane and isoflurane only slightly impair arterial oxygenation during one-lung ventilation in patients undergoing thoracotomy. Anesthesiology. 1987;67(6):910–5. https://doi.org/10.1097/00000542-198712000-00006.
Wang JY, Russell GN, Page RD, Jackson M, Pennefather SH. Comparison of the effects of sevoflurane and isoflurane on arterial oxygenation during one lung ventilation. Br J Anaesth. 1998;81(6):850–3. https://doi.org/10.1093/bja/81.6.850.
Abe K, Shimizu T, Takashina M, Shiozaki H, Yoshiya I. The effects of propofol, isoflurane, and sevoflurane on oxygenation and shunt fraction during one-lung ventilation. Anesth Analg. 1998;87(5):1164–9. https://doi.org/10.1097/00000539-199811000-00035.
Acknowledgements
The authors are indebted to all patients and their relatives who volunteered to participate in this study.
Funding
Open Access funding enabled and organized by Projekt DEAL. The main study was funded by Sedana Medical, Danderyd, Sweden. The present substudy received no particular funding but logistical and statistical support was provided by Sedana.
Author information
Authors and Affiliations
Contributions
Conception and design: TB, AM, UG, MB, PS, PK. Data acquisition: TB, AM, UG, MB, JB, KK, HB, AF, PK. Statistical analysis: JN. Interpretation: TB, PK, PS. Drafting the manuscript for important intellectual content: TB, PK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was provided by Ethikkommission der Ärztekammer des Saarlandes, Germany, during the ethics approval meeting on Feb 16, 2017, with final approval on April 18, 2017. Ethical approval was also provided by National Medical Ethics Committee Komisija republike Slovenije za medicinsko etiko, Slovenia on June 6, 2019. Written informed consent was obtained from the patient or the patient’s representative, as appropriate. The study was done in accordance with International Conference on Harmonisation Good Clinical Practice (ICH-GCP) standards and the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
AM reports consultancy fees from Sedana Medical. TV reports grant support from B Braun. UG reports lecture fees from MT Monitor Technik and Getinge and reimbursement of clinical study expenses from Bayer Healthcare. TB reports personal lecture fees from Sedana Medical and Vyaire and institutional funding from Löwenstein Medical. PK reports personal fees and travel costs from Sedana Medical. MD reports lecture fees and travel costs from Cytosorbents Europe. PS reports employment by Sedana Medical and shareholding in Sedana Medical. All other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Becher, T., Meiser, A., Guenther, U. et al. Isoflurane vs. propofol for sedation in invasively ventilated patients with acute hypoxemic respiratory failure: an a priori hypothesis substudy of a randomized controlled trial. Ann. Intensive Care 12, 116 (2022). https://doi.org/10.1186/s13613-022-01090-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01090-w