Abstract
Background
Lung reactivations of Herpesviridae, herpes simplex virus (HSV) and cytomegalovirus (CMV) have been reported in COVID-19 patients. Whether or not those viral reactivations are more frequent than in other patients is not known.
Methods
Retrospective monocentric cohort study of 145 patients with severe COVID-19 pneumonia requiring invasive mechanical ventilation and who were tested for HSV and CMV in bronchoalveolar lavage performed during fiberoptic bronchoscopy for ventilator-associated pneumonia suspicion. Rates of HSV and CMV lung reactivations, and HSV bronchopneumonitis were assessed and compared with an historical cohort of 89 patients with severe influenza pneumonia requiring invasive mechanical ventilation.
Results
Among the 145 COVID-19 patients included, 50% and 42% had HSV and CMV lung reactivations, respectively, whereas among the 89 influenza patients, 63% and 28% had HSV and CMV lung reactivations, respectively. Cumulative incidence of HSV lung reactivation (taking into account extubation and death as competing events) was higher in influenza than in COVID-19 patients (p = 0.03), whereas the rate of HSV bronchopneumonitis was similar in both groups (31% and 25%, respectively). Cumulative incidence of CMV lung reactivation (taking into account extubation and death as competing events) was similar in COVID-19 and influenza patients (p = 0.07). Outcomes of patients with HSV or CMV lung reactivations were similar to that of patients without, whatever the underlying conditions, i.e., in COVID-19 patients, in influenza patients, or when all patients were grouped.
Conclusions
HSV and CMV lung reactivations are frequent in COVID-19 patients, but not more frequent than in patients with influenza-associated severe pneumonia, despite a higher severity of illness at intensive care unit admission of the latter and a longer duration of mechanical ventilation of the former. Although no impact on outcome of HSV and CMV lung reactivations was detected, the effect of antiviral treatment against these Herpesviridae remains to be determined in these patients.
Similar content being viewed by others
Background
Viral reaction of herpes simplex virus (HSV) is common in the respiratory tract of mechanically ventilated patients, with frequency ranging from 30% to 60%, depending on case mix [1, 2]. Cytomegalovirus (CMV) blood reactivation is also frequent, occurring in 30% of seropositive intensive care unit (ICU) patients, whereas CMV lung reactivation/infection is less frequent [2,3,4]. Although several data suggest that Herpesviridae [HSV, CMV, but also Epstein–Barr virus (EBV) or human herpesvirus (HHV-6)] reactivation/detection in the blood and/or in the lower respiratory tract (LRT) is frequent in patients with severe coronavirus infectious disease-19 (COVID-19) pneumonia [5,6,7,8,9,10], it is not known whether these reactivations/infections/detections are more frequent in COVID-19 patients than in patients with pneumonia of other origins. Yet, it has been shown that patients with severe COVID-19 pneumonia hospitalized in the ICU and receiving mechanical ventilation (MV) are prone to develop bacterial or fungal ventilator-associated LRT infection with higher incidence rates than patients with pneumonia due to other causes [11,12,13]. Whether or not Herpesviridae reactivations are also more frequent in severe COVID-19 patients requiring MV, as compared to patients receiving MV for other causes, remains to be determined.
We, therefore, conducted a retrospective monocentric cohort study to evaluate frequencies and outcomes of HSV and CMV reactivations and infections in the LRT of patients with severe COVID-19 pneumonia, as compared to historical cohort of patients with severe influenza-associated pneumonia. Our hypothesis was that COVID-19 patients and influenza patients had similar rates of HSV and CMV reactivations.
Methods
Patients
All consecutive ICU-admitted patients, with confirmed COVID-19 pneumonia, based on reverse-transcriptase–polymerase-chain reaction (RT–PCR) performed on a respiratory specimen, between March 2020 and June 2021, and having received MV (MV), were included in this retrospective, monocenter, observational study. COVID-19 patients without MV were not included, because testing for Herpesviridae infection in the LRT of non-intubated patients is not routinely performed. Among screened patients, those having at least one lower respiratory tract sample tested for Herpesviridae (HSV and CMV) during their ICU stay were included. This group is hereafter called “COVID-19 group”.
Patients with confirmed influenza pneumonia admitted to our ICU between January 2013 and March 2020, having received invasive MV and having at least one LRT sample tested for Herpesviridae (HSV and CMV) served as controls (hereafter called “Influenza group”) [14].
Procedures
In our ICU, mechanically ventilated patient clinically suspected of having developed ventilator-associated pneumonia (VAP) undergo fiberoptic bronchoscopy and bronchoalveolar lavage (BAL) [2, 15]. BAL fluid samples are processed in the bacteriological laboratory, looking for bacterial pneumonia, and in the virological laboratory, looking for viral reactivation/infection (HSV and CMV). The same procedures were performed in patients with COVID-19- and influenza-associated acute respiratory distress syndrome (ARDS).
Some patients had HSV or CMV blood testing at the time of BAL, the indication for HSV or CMV blood testing was driven by the physician in charge of the patient.
Virological analysis
BAL fluid and whole blood samples were processed in the virology laboratory for HSV and CMV genome quantification. For BAL fluid samples, HSV and CMV genomes, together with albumin gene, were quantified using in-house real-time PCRs, as previously described, and viral loads were calculated and expressed in copies (for HSV) or international units (IU, for CMV) per million of cells collected by BAL [16, 17]. For whole blood samples, HSV and CMV genomes were quantified using HSV1&2 VZV R-GENE® kit (BIOMERIEUX) and artus® CMV QS-RGQ kit (Qiagen), respectively. Results were expressed in copies/mL (HSV) or in IU/mL (CMV).
Outcomes
The primary outcomes were prevalence of HSV and CMV lung reactivations and HSV bronchopneumonitis in patients with COVID-19 and patients with influenza. Secondary outcomes were ICU length of stay and ICU mortality in both groups.
Definitions
Herpesviridae reactivations
HSV and CMV LRT reactivations were defined as a positive PCR in BAL, for HSV or CMV, respectively, whatever the virus loads.
For patients with viral blood testing, HSV and CMV blood reactivations were defined as a PCR positive for the corresponding virus in blood, whatever the virus load.
HSV bronchopneumonitis
HSV bronchopneumonitis was defined as a clinical suspicion of VAP associated with a PCR positive for HSV with a virus load ≥ 105 copies per million of cells. This cutoff was chosen according to previous publications, which found that it was associated with HSV bronchopneumonitis, diagnosed on histology or cytology [18]. Since no data exist regarding the relationship between CMV load in the LRT and CMV lung disease, this latter could not be defined in the present study.
ICU-acquired infections
VAP was diagnosed in patients having received MV for at least 48 h when the following two criteria were met: (1) clinically suspected VAP, defined as a new and persistent pulmonary infiltrate on chest radiograph associated with at least two of the following: temperature ≥ 38 °C, white blood cell count ≥ 10 Giga/L, purulent tracheal secretions, increased minute ventilation, arterial oxygenation decline requiring modifications of the ventilator settings and/or need for increased vasopressor infusion. For patients with ARDS, for whom demonstration of radiologic deterioration is difficult, at least two of the preceding criteria sufficed; and (2) significant quantitative growth (≥ 104 colony-forming units/mL) of distal BAL fluid samples [19, 20].
Bloodstream infection (BSI) was defined as a bacterial infection identified on blood cultures. If coagulase-negative Staphylococcus were identified, it was considered as a BSI only if 2 sets of blood cultures grew with the same pathogen exhibiting the same resistance profile [21].
Data collection and analysis
The following data were prospectively recorded in each patient’s medical chart: age, sex, presence of immunosupression (defined as one of the following condition: solid organ transplantation, hematological malignancy or treatment with immunosuppressant drug, including corticosteroids at a dose ≥ 0.5 mg/kg/d for ≥ 1 month). Simplified Acute Physiology Score (SAPS) II and Sequential Organ-Failure Assessment (SOFA) score at ICU admission, date COVID-19 or influenza symptoms started, date of hospital and ICU admission, date of MV onset, bacterial coinfection at ICU admission, presence or not of ARDS according to Berlin definition [22], need for extracorporeal membrane oxygenation (ECMO) device and its type (veno-venous or veno-arterial), episodes of bacterial VAP and episodes of BSI. ICU mortality was also recorded.
Study endpoints
Study endpoints were rates of HSV lung reactivation, HSV bronchopneumonitis and CMV lung reactivation in COVID-19 and influenza patients. These frequencies were compared between COVID-19 and influenza patients. Secondary endpoint was the impact of HSV and CMV reactivations on ICU mortality in all patients and in each group separately.
Statistical analyses
Data are expressed as median (interquartile range [IQR]) or n (%). Between-group comparisons were analyzed using Student’s t test or Mann–Whitney U tests according to variable’s distribution, i.e., normal or not, respectively, for continuous variables. Between-group differences were assessed with chi-square test or Fisher’s exact test for nominal variables. Incidences of HSV and CMV reactivations, as well as HSV and bronchopneumonitis in the 2 groups (primary outcomes) were compared using an estimated cumulative incidence function to take into account competing factors (death or extubation), as previously described [23]: cumulative incidence of viral reactivation, extubation and death were estimated in each group, taking into account only the first event, and compared. No sample size was calculated. Univariable analyses of factors associated with ICU mortality were performed. For this analysis, Herpesviridae reactivation was converted into a 4 categories variable: no viral reactivation, HSV reactivation, CMV reactivation, and both HSV and CMV reactivations (corresponding to patients having both reactivations). Thereafter, multiple logistic-regression analyses using backward-stepwise variable elimination were run (with the variable-exit threshold set at p < 0.05). Factors achieving p ≤ 0.10 in our univariable analyses were entered into the multivariable model. Herpesviridae reactivation was forced into the multivariable models. All potential explanatory variables included in the multivariable analyses were subjected to collinearity analysis with a correlation matrix. Variables associated with one another were not included in the model: because the SAPS II was strongly associated with the SOFA score, the former was not included in the final model. All reported P values are two-sided, and p < 0.05 was considered statistically significant. Analyses were computed using SPSS Version 23 (IBM SPSS, Chicago, IL) and R software, version 3.5.1 (R Foundation).
Ethics
In accordance with current French law, informed written consent for demographic, physiologic and hospital-outcome data analyses was not obtained, because this observational study did not modify existing diagnostic or therapeutic strategies. Nonetheless, patients and/or relatives were informed about the anonymous data collection and told that they could decline inclusion. The database is registered with the Commission Nationale l’Informatique et des Libertés (CNIL, registration no. 1950673).
Results
During the study period, 312 patients were admitted to our ICU for COVID-19. Among them, 264 were mechanically ventilated, and 145 had at least one LRT sample tested for Herpesviridae (Fig. 1). Baseline characteristics and outcomes of these patients are given in Table 1. All were severely ill, requiring ECMO support for all except one; they had prolonged MV duration and ICU length of stay and their ICU-mortality rate was 43%.
Among the 146 patients with influenza admitted in our ICU during the 2013–2020 periods, 134 were mechanically ventilated, and 89 had at least one LRT sample tested for Herpesviridae (Fig. 1). Baseline characteristics and outcomes of these patients are displayed in Table 1. Among these 89 patients, 79 (89%) were infected with influenza A virus (subtypes H1N12009 for 62, H3N2 for 3, and not known for 14) and 10 (11%) with influenza B virus. Whereas influenza patients were sicker at ICU admission than COVID-19 patients, their duration of MV and ICU length of stay were shorter (Table 1). ICU-mortality rates were similar among the 2 groups.
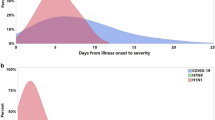
HSV lung reactivation and bronchopneumonitis
Although the proportion of patients with HSV lung reactivation was similar in patients with COVID-19 and influenza (50% and 63%, respectively, p = NS), estimated cumulative incidence of HSV reactivation (taking into account death and extubation as competing factors) was significantly higher in influenza patients than in COVID-19 patients (p = 0.03), whereas death and extubation did not differ between these 2 groups (p = 0.53 and 0.87, respectively) (Fig. 2). HSV reactivation occurred later in the COVID-19 group, but the highest virus loads among patients with HSV reactivation were similar in both groups (Table 2). Among the 73 COVID-19 patients with HSV lung reactivation, 32 (44%) were isolated and 41 (56%) were associated with CMV lung reactivation. Among the 53 influenza patients with HSV lung reactivation, 32 (60%) were isolated and 21 (40%) were associated with CMV lung reactivation (Table 3).
Estimated cumulative incidence of herpes simplex virus (HSV) lung reactivation, extubation or death in COVID-19 and influenza patients, taking into account only the first event that occurred. HSV reactivation refers to patients whose first event was HSV reactivation in lung; extubation refers to patients whose first event was extubation, and death refers to patients whose first event was death. p values for differences between COVID-19 and influenza patients were 0.03 for HSV reactivation, 0.53 for death and 0.87 for extubation
Proportion of patients developing HSV bronchopneumonitis was similar in COVID-19 and influenza patients, within similar time interval from MV start to HSV bronchopneumonitis diagnosis (Table 2) and with similar viral loads (Fig. 3).
Herpes simplex virus (HSV loads in COVID-19 and influenza patients with (grey boxes) and without (white boxes) HSV bronchopneumonitis, respectively. The box plots report: the internal horizontal line is the median; the lower and upper box limits are the quartile 1 and quartile 3, respectively; bars represent the 95% confidence interval. The black circles are outliers
Proportion of patients having received aciclovir (all because of virus load ≥ 105 copies per million of cells, at a dosing of 10 mg/kg every 8 h during 10 to 15 days, dosing adjusted on renal function) was similar among COVID-19 and influenza patients; 35/145 (24%) and 27/89 (30%), respectively (p = 0.3).
CMV lung reactivation
Although the proportion of patients with COVID-19 had more frequent CMV lung reactivation than patients with influenza (42% vs. 28%, p = 0.03), estimated cumulative incidence of CMV lung reactivation (taking into account death and extubation as competing factors) was similar in influenza patients and in COVID-19 patients (p = 0.07, see Fig. 4). CMV reactivation occurred later in COVID-19 patients but with a same peak in virus load (Table 2). Among the 61 COVID-19 patients with CMV lung reactivation, 41 (67%) had previous or concomitant HSV lung reactivation and 20 (33%) CMV reactivation alone. Among the 25 influenza patients with CMV lung reactivation, 21 (84%) had previous or concomitant HSV lung reactivation and 4 (16%) had CMV reactivation only (Table 3).
Estimated cumulative incidence of cytomegalovirus (CMV) lung reactivation, extubation or death in COVID-19 and influenza patients, taking into account only the first event that occurred. CMV reactivation refers to patients whose first event was CMV reactivation in lung; extubation refers to patients whose first event was extubation, and death refers to patients whose first event was death. p values for differences between COVID-19 and influenza patients were 0.07 for HSV reactivation, 0.03 for death and 0.49 for extubation
No patients received ganciclovir.
HSV and CMV blood reactivation
Only few patients had HSV and CMV blood testing. Results are presented in the online supplement (Additional file 1: Table S1).
Herpesviridae reactivation and immunosuppressive treatment
Among the COVID-19 patients, 13 received tocilizumab and none received an Il-1 inhibitor, whereas 127 (88%) received corticosteroids at a dosing ≥ 40 mg/day for at least 5 days (Table 1). The use of tocilizumab and corticosteroids were not associated with an increased risk of HSV or CMV reactivation: among the 93 COVID-19 patients who had at least one Herpesviridae reactivation (HSV, CMV or both), 11 (12%) received tocilizumab and 81 (88%) received corticosteroids (at a dosing ≥ 40 mg/day for at least 5 days), whereas among the 50 COVID-19 patients without any Herpesviridae reactivation, 2 (4%) received tocilizumab and 46 (88%) received corticosteroids (p = 0.18 for tocilizumab and p > 0.99 for corticosteroids).
Similar results were found regarding influenza patients: none received tocilizumab or another anti-interleukine-6 or anti-interleukine-1; but among the 60 patients who had at least one Herpesviridae reactivation (HSV, CMV or both), 10 (17%) received corticosteroids, whereas among the 29 patients without any Herpesviridae reactivation, 3 (10%) received corticosteroids (p = 0.53 for between groups comparison).
Herpesviridae reactivation and outcomes
Outcomes of patients according to type of Herpesviridae reactivation (HSV alone, CMV alone, both viruses, or none) in each group (COVID-19 and influenza) are reported in Table 3: duration of MV, ICU length of stay and ICU mortality rate were similar in patients with or without Herpesviridae reactivation. ICU mortality rate of patients with HSV bronchopneumonitis was not different from ICU mortality of patients without HSV bronchopneumonitis (53% vs. 43%, respectively, p = 0.16 for between groups difference).
In univariable and multivariable analysis, Herpesviridae LRT reactivation (whatever the type of reactivation, i.e. HSV reactivation, CMV reactivation or both CMV and HSV reactivation) was not associated with ICU mortality in patients with COVID-19 and influenza (Additional file 1: Table S2).
Discussion
In this study, we found that HSV and CMV reactivations in the LRT were frequent in patients with severe COVID-19, affecting 50% and 42% of patients, respectively. However, this high rate of Herpesviridae reactivation was close to that of patients with influenza-associated ARDS; taking into account death and extubation as competing events, HSV reactivation was more frequent in influenza patients than in COVID-19 patients, whereas rates of CMV reactivation were similar in both conditions. We also found that Herpesviridae reactivation (whatever the reactivation, i.e., HSV, CMV or both viruses) had no impact on outcomes.
To the best of our knowledge, only 6 studies have evaluated Herpesviridae reactivations in the blood and/or in the LRT of COVID-19 patients, and all found a high rate of Herpesviridae reactivation [5,6,7,8,9,10]. Results of these observational studies are summarized in Table 4. HSV was detected in the blood of 8–30% and in the LRT of 42–83% of ICU patients, whereas CMV was detected in the blood of 15–41% and in the LRT of 24% of ICU patients. Our results are in accordance with these reports and reinforce them, although the case mix was not similar (our study is the largest study on patients on MV, and most had ECMO support). In addition to HSV and CMV, some studies evaluated other Herpesviridae: Saade et al. found, that among 100 ICU patients (38 being immunocompromised), DNA of EBV was detectable in the blood of 58 [5]; Simonnet et al. found that among 34 ICU patients, EBV, and HHV-6 DNA were detected in the blood of their patients in 28 (82%) and 7 (22%), respectively [8].
One of the originality of our work is to have compared patients with COVID-19 to patients with severe influenza. COVID-19 have been initially compared to influenza, since both virus may induce pneumonia and ARDS; however, it seems that COVID-19 is associated with significantly greater severity of illness, longer hospital stays, higher rate of ventilator-associated pneumonia and higher mortality rate [12, 24, 25]. As a matter of fact, in our patients, despite greater severity of influenza patients than COVID-19 patients (with higher severity scores at admission and higher rate of documented bacterial coinfection), the former spent less time on MV, on ECMO, and in the ICU. Whatever these differences, the rates of HSV and CMV reactivations in the LRT were close in the 2 groups, as well as the rate of HSV bronchopneumonitis. Although rates of HSV lung reactivation and HSV bronchopneumonitis were high in COVID-19 but also in influenza patients, they are similar to that of previous studies in different populations [18, 26]. Interestingly, despite 88% of our COVID-19 patients received corticosteroids vs. only 20% of influenza patients, the rate of Herpesviridae reactivations were close in both groups, suggesting that use of corticosteroids [mostly dexamethasone at a dosing of 6 mg/day during 10 days)] in COVID-19 patients may perhaps not be a risk factor for viral reactivation. However, our study was not designed to explore risk factors for Herpesviridae reactivation in COVID-19 patients; therefore, no formal conclusion on this particular point can be drawn.
In our study, 42% of patients with COVID-19 had CMV lung reactivation. Whereas CMV blood reactivation is well-described and occurs in roughly 30% of CMV-seropositive patients [3, 27], CMV lung reactivation has been poorly investigated. Moreover, the exact significance of CMV detection in the LRT remains controversial: apart in biopsies or autopsies findings, where CMV pneumonia has been diagnosed histologically [28, 29], no study has evaluated the relevance of CMV lung reactivation in ICU patients. In other words, whereas CMV lung detection is associated with lung disease is probable, but has never been confirmed.
Surprisingly, we found no impact on outcome of HSV or CMV reactivation, whereas previous studies have shown the opposite: indeed, HSV reactivation and bronchopneumonitis have been associated with increased mortality [18, 30], as well as CMV blood reactivation [3, 27, 30]. Moreover, although not reaching statistical significance, we observed a trend toward higher duration of MV and ICU length of stay in COVID-19 patients and Herpesviridae reactivation, as compared to COVID-19 patients without reactivation. This was previously described by others in similar patients, namely, VV-ECMO patients: Hraiech et al. found an association between Herpesviridae reactivation and duration of MV [31]. However, the population of the previous studies was not the same as ours, since we included patients with severe respiratory failure, almost all requiring ECMO support. In these patients, prognosis is probably driven more by the underlying condition (namely, ARDS and other organ failures) than by HSV or CMV reactivation. Similarly, in their randomized, double-blind, placebo-controlled study evaluating preemptive acyclovir, Luyt et al. found a positive effect of acyclovir on mortality only in the less severe patients, i.e., those with one organ failure or less at randomization, whereas acyclovir treatment had no impact on outcome in the most severe patients [32]. Last, the lack of power of our study may explain the difference between Hraiech study and ours. However, the significance of Herpesviridae reactivation and duration of MV is still matter of debate: it might be either a causative link (Herpesviridae reactivation has its own morbidity/mortality), or a bystander association (Herpesviridae reactivate in the most severe patients, with prolonged duration of MV).
Our study has several limitations that should be underlined. First is its retrospective monocenter design that included the most severe COVID-19 patients, almost all of whom requiring VV-ECMO, making our results difficult to extrapolate to other ICUs with different case-mixes. However, the frequencies of HSV and CMV detection found here were close to those previously reported. Second, we included only patients on MV, because HSV and CMV lung sampling are performed only when a patient is suspected of having developed VAP. Therefore, we are not sure that patients who were not sampled did not have HSV or CMV lung reactivation, and our results cannot be extrapolated to patients without MV. Third, we included patients who had HSV and CMV testing in BAL: 44/134 (33%) influenza patients and 119/264 (45%) COVID-19 patients were not tested for Herpesviridae, which is a selection bias. Therefore, the frequencies of HSV or CMV lung reactivations given in the present study may not be representative of those occurring in all ICU patients. Fourth, HSV and CMV serologic status of our patients is not known. Since it is obvious that rate of HSV or CMV reactivation depends on the rate of positive serologic status, our results are, therefore, not applicable in a different population with different serologic status. Fifth, COVID-19 and influenza patients were not strictly comparable, since the latter were more severely ill at admission, had more bacterial coinfection and spent less days on MV and ECMO; therefore, the comparisons or Herpesviridae reactivations between the 2 groups may be inappropriate. Sixth, we acknowledge that our study lacks of power, as well as lack of correction of alpha risk for multiple comparisons. Therefore, difference between the 2 groups may occur and not be detected. Finally, only a small proportion of our patients had HSV or CMV blood testing. Therefore, the exact frequencies of these blood reactivations in COVID-19 or influenza patients cannot be determined, as well as their impact on outcome.
Conclusions
HSV and CMV lung reactivation are frequent in COVID-19 patients, but as frequent as in patients with influenza-associated severe pneumonia. HSV bronchopneumonitis is also frequent in COVID-19 patients, but similar to that of previously described frequency. HSV or CMV lung reactivations are not associated with impaired outcome, as compared to patient without HSV or CMV reactivation, but probably because our study included the most severe patients. Whereas an antiviral treatment may improve outcome in these patients remains to be determined.
Availability of data and materials
The data sets generated during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- ARF:
-
Acute respiratory failure
- BAL:
-
Bronchoalveolar lavage
- COVID-19:
-
Coronavirus infection disease 2019
- ECMO:
-
Extracorporeal membrane oxygenation
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- SAPS:
-
Simplified Acute Physiology Score
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome coronavirus 2
- SOFA:
-
Sequential organ failure assessment
- VAP:
-
Ventilator-associated pneumonia
- WBC:
-
White blood cell
References
Cantan B, Luyt C-E, Martin-Loeches I. Influenza infections and emergent viral infections in intensive care unit. Semin Respir Crit Care Med. 2019;40:488–97.
Luyt C-E, Bouadma L, Morris AC, Dhanani JA, Kollef M, Lipman J, et al. Pulmonary infections complicating ARDS. Intensive Care Med. 2020;46:2168–83.
Li X, Huang Y, Xu Z, Zhang R, Liu X, Li Y, et al. Cytomegalovirus infection and outcome in immunocompetent patients in the intensive care unit: a systematic review and meta-analysis. BMC Infect Dis. 2018;18:289.
Luyt C-E, Bréchot N, Chastre J. What role do viruses play in nosocomial pneumonia? Curr Opin Infect Dis. 2014;27:194–9.
Saade A, Moratelli G, Azoulay E, Darmon M. Herpesvirus reactivation during severe COVID-19 and high rate of immune defect. Infect Dis Now. 2021;51:676–9.
Seeßle J, Hippchen T, Schnitzler P, Gsenger J, Giese T, Merle U. High rate of HSV-1 reactivation in invasively ventilated COVID-19 patients: immunological findings. PLoS ONE. 2021;16: e0254129.
Franceschini E, Cozzi-Lepri A, Santoro A, Bacca E, Lancellotti G, Menozzi M, et al. Herpes simplex virus re-activation in patients with SARS-CoV-2 pneumonia: a prospective observational study. Microorganisms. 2021;9:1896.
Simonnet A, Engelmann I, Moreau A-S, Garcia B, Six S, El Kalioubie A, et al. High incidence of Epstein–Barr virus, cytomegalovirus, and human-herpes virus-6 reactivations in critically ill patients with COVID-19. Infect Dis Now. 2021;51:296–9.
Meyer A, Buetti N, Houhou-Fidouh N, Patrier J, Abdel-Nabey M, Jaquet P, et al. HSV-1 reactivation is associated with an increased risk of mortality and pneumonia in critically ill COVID-19 patients. Crit Care. 2021;25:417.
Le Balc’h P, Pinceaux K, Pronier C, Seguin P, Tadié J-M, Reizine F. Herpes simplex virus and cytomegalovirus reactivations among severe COVID-19 patients. Crit Care. 2020;24:530.
Rouzé A, Martin-Loeches I, Povoa P, Makris D, Artigas A, Bouchereau M, et al. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: a European multicenter cohort study. Intensive Care Med. 2021;47:188–98.
Luyt C-E, Sahnoun T, Gautier M, Vidal P, Burrel S, Pineton de Chambrun M, et al. Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: a retrospective cohort study. Ann Intensive Care. 2020;10:158.
Gangneux J-P, Dannaoui E, Fekkar A, Luyt C-E, Botterel F, De Prost N, et al. Fungal infections in mechanically ventilated patients with COVID-19 during the first wave: the French multicentre MYCOVID study. Lancet Respir Med. 2021;S2213–2600(21):00442–52.
Rozencwajg S, Bréchot N, Schmidt M, Hékimian G, Lebreton G, Besset S, et al. Co-infection with influenza-associated acute respiratory distress syndrome requiring extracorporeal membrane oxygenation. Int J Antimicrob Agents. 2018;51:427–33.
Papazian L, Klompas M, Luyt C-E. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46:888–906.
Burrel S, Fovet C, Brunet C, Ovaguimian L, Hamm N, Conan F, et al. Routine use of duplex real-time PCR assays including a commercial internal control for molecular diagnosis of opportunistic DNA virus infections. J Virol Methods. 2012;185:136–41.
Boutolleau D, Fernandez C, André E, Imbert-Marcille B-M, Milpied N, Agut H, et al. Human herpesvirus (HHV)-6 and HHV-7: two closely related viruses with different infection profiles in stem cell transplantation recipients. J Infect Dis. 2003;187:179–86.
Luyt C-E, Combes A, Deback C, Aubriot-Lorton M-H, Nieszkowska A, Trouillet J-L, et al. Herpes simplex virus lung infection in patients undergoing prolonged mechanical ventilation. Am J Respir Crit Care Med. 2007;175:935–42.
Chastre J, Fagon J-Y. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903.
Chastre J, Luyt C-E. Does this patient have VAP? Intensive Care Med. 2016;42:1159–63.
Massart N, Maxime V, Fillatre P, Razazi K, Ferré A, Moine P, et al. Characteristics and prognosis of bloodstream infection in patients with COVID-19 admitted in the ICU: an ancillary study of the COVID-ICU study. Ann Intensive Care. 2021;11:183.
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–33.
Gray RJ. A class of K-Sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–54.
Talbot HK, Martin ET, Gaglani M, Middleton DB, Ghamande S, Silveira FP, et al. Coronavirus disease 2019 (COVID-19) versus influenza in hospitalized adult patients in the United States: differences in demographic and severity indicators. Clin Infect Dis. 2021;73:2240–7.
Faury H, Courboulès C, Payen M, Jary A, Hausfater P, Luyt C, et al. Medical features of COVID-19 and influenza infection: a comparative study in Paris, France. J Infect. 2021;82:e36–9.
Bruynseels P, Jorens PG, Demey HE, Goossens H, Pattyn SR, Elseviers MM, et al. Herpes simplex virus in the respiratory tract of critical care patients: a prospective study. Lancet. 2003;362:1536–41.
Limaye AP, Kirby KA, Rubenfeld GD, Leisenring WM, Bulger EM, Neff MJ, et al. Cytomegalovirus reactivation in critically ill immunocompetent patients. JAMA. 2008;300:413–22.
Papazian L, Fraisse A, Garbe L, Zandotti C, Thomas P, Saux P, et al. Cytomegalovirus. An unexpected cause of ventilator-associated pneumonia. Anesthesiology. 1996;84:280–7.
Papazian L, Doddoli C, Chetaille B, Gernez Y, Thirion X, Roch A, et al. A contributive result of open-lung biopsy improves survival in acute respiratory distress syndrome patients. Crit Care Med. 2007;35:755–62.
Coisel Y, Bousbia S, Forel J-M, Hraiech S, Lascola B, Roch A, et al. Cytomegalovirus and herpes simplex virus effect on the prognosis of mechanically ventilated patients suspected to have ventilator-associated pneumonia. PLoS ONE. 2012;7: e51340.
Hraiech S, Bonnardel E, Guervilly C, Fabre C, Loundou A, Forel J-M, et al. Herpes simplex virus and Cytomegalovirus reactivation among severe ARDS patients under veno-venous ECMO. Ann Intensive Care. 2019;9:142.
Luyt C-E, Forel J-M, Hajage D, Jaber S, Cayot-Constantin S, Rimmelé T, et al. Acyclovir for mechanically ventilated patients with herpes simplex virus oropharyngeal reactivation: a randomized clinical trial. JAMA Intern Med. 2020;180:263–72.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
CEL designed the study, collected, compiled, analyzed and interpreted the data and wrote the manuscript. DM, MPdC, JC, VG, NB, MS, GH and AC collected data. SB and DB performed the virological analysis and collected data. DL performed statistical analysis. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In accordance with current French law, informed written consent for demographic, physiologic and hospital-outcome data analyses was not obtained, because this observational study did not modify existing diagnostic or therapeutic strategies. Nonetheless, patients and/or relatives were informed about the anonymous data collection and told that they could decline inclusion. The database is registered with the Commission Nationale l’Informatique et des Libertés (CNIL, registration no. 1950673).
Consent for publication
Not applicable.
Competing interests
C.-E. L. received lecture fees from MSD, Aerogen and AdvanzPharma, outside the submitted work. The other authors have no conflicts of interest to declare in relationship to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
HSV and CMV blood reactivation. Table S2. Univariable and multivariable analysis of factors associated with intensive care unit mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luyt, CE., Burrel, S., Mokrani, D. et al. Herpesviridae lung reactivation and infection in patients with severe COVID-19 or influenza virus pneumonia: a comparative study. Ann. Intensive Care 12, 87 (2022). https://doi.org/10.1186/s13613-022-01062-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01062-0