Abstract
Rationale
Sepsis is a life-threatening, dysregulated response to infection. Lipid biomarkers including cholesterol are dynamically regulated during sepsis and predict short-term outcomes. In this study, we investigated the predictive ability of lipid biomarkers for physical function and long-term mortality after sepsis.
Methods
Prospective cohort study of sepsis patients admitted to a surgical intensive-care unit (ICU) within 24 h of sepsis bundle initiation. Samples were obtained at enrollment for lipid biomarkers. Multivariate regression models determined independent risk factors predictive of poor performance status (Zubrod score of 3/4/5) or survival at 1-year follow-up.
Measurements and main results
The study included 104 patients with surgical sepsis. Enrollment total cholesterol and high-density lipoprotein (HDL-C) levels were lower, and myeloperoxidase (MPO) levels were higher for patients with poor performance status at 1 year. A similar trend was seen in comparisons based on 1-year mortality, with HDL-C and ApoA-I levels being lower and MPO levels being higher in non-survivors. However, multivariable logistic regression only identified baseline Zubrod and initial SOFA score as significant independent predictors of poor performance status at 1 year. Multivariable Cox regression modeling for 1-year survival identified high Charlson comorbidity score, low ApoA-I levels, and longer vasopressor duration as predictors of mortality over 1-year post-sepsis.
Conclusions
In this surgical sepsis study, lipoproteins were not found to predict poor performance status at 1 year. ApoA-I levels, Charlson comorbidity scores, and duration of vasopressor use predicted 1 year survival. These data implicate cholesterol and lipoproteins as contributors to the underlying pathobiology of sepsis.
Similar content being viewed by others
Introduction
Sepsis is a dysregulated response to infection that leads to organ dysfunction and potentially death [1]. Sepsis mortality is substantial at 20% worldwide, though this figure is improved from prior decades [2]. However, focusing on initial survival alone is not adequate for understanding patient-oriented outcomes after sepsis. Our group and others have demonstrated that the long-term outcomes of early sepsis survivors are frequently poor [3, 4]. Sepsis survivors frequently experience persistent and long-term organ dysfunction as well as recurrent sepsis [4, 5]. In addition, a subset of patients (up to 40%) develop a syndrome of chronic critical illness (CCI), defined as ICU stay ≥ 14 days with continued organ dysfunction, and clinically result in lean muscle wasting, cachexia, and a 1-year mortality approaching 50% [3, 6, 7]. This group of patients requires high levels of post-discharge care, with most of them experiencing limitations in performing activities of daily living, and frequently limited to a bed or chair for most of the day [3].
The term persistent inflammation immunosuppression and catabolism syndrome (PICS) was coined to describe the presumed underlying pathobiology of CCI that occurred in over one-third surgical ICU patients treated for sepsis [7]. It is characterized by persistent inflammation (elevation of IL-6 and IL-8 levels), immunosuppression [lymphopenia, elevated soluble programmed death ligand-1 (sPDL-1), and nosocomial infections], and catabolism [8]. Compared to medical ICU sepsis patients, the PICS-CCI phenotype may be more common in surgical ICU sepsis patients for several reasons. First, because of surgeon selection bias surgery, patients have lower likelihood of having severe comorbidities and thus have early sepsis care terminated for perceived futility. Second, surgical patients frequently undergo source control interventions that can dramatically improve organ dysfunction and short-term survival. Third, surgical patients may require repeat source controls interventions and have surgical wounds that prolong inflammation and dysregulated immunity. These observations have been described and elucidated in our prior publications, from a large prospective observational study of surgical sepsis [9,10,11].
Endogenous lipids and lipoproteins are highly metabolically active during sepsis and critical illness [12, 13]. High-density lipoprotein (HDL) and low-density lipoprotein (LDL) have both been shown to have protective roles in sepsis [14, 15]. HDL is a major source of cholesterol for endogenous corticosteroid production in the adrenal glands [16, 17], and prevents tissue damage in sepsis, a function mediated by several of HDLs proteins including paraoxonase-1 (PON-1) and apolipoprotein A-I (Apo A-I) [13]. Toxins from both Gram-negative bacteria (endotoxin) and Gram-positive bacteria (lipoteichoic acid) are neutralized by HDL via Apo A-I [13, 18,19,20,21] and LDL has also been shown to bind and clear endotoxin via the liver [22,23,24]. However, we have shown that HDL becomes pro-inflammatory or dysfunctional (Dys-HDL) when subjected to inflammation in sepsis, and that Dys-HDL correlates with and predicts organ failure severity in sepsis [25]. We have also demonstrated disparate outcomes associated with cholesterol levels and function, with the most severe organ failure being associated with the lowest early cholesterol levels [26, 27]. Based on these and other studies, we hypothesize that an interplay between inflammation, organ failure, and lipid metabolism exists that is predictive of poor performance status and long-term mortality after sepsis [25, 28]. The objectives of the proposed of study were to evaluate the predictive ability of early lipid indicators for poor performance status and 1-year mortality after surgical sepsis.
Methods
Design
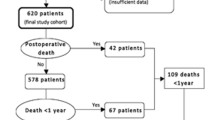
This study was a subgroup analysis of a 5-year prospective, longitudinal cohort study of patients with surgical sepsis. Patients were included in the subgroup analysis if they had data on lipid and oxidative biomarkers sent as part of the prospective study. Additional file 1: Tables S1 and Additional file 2: Table S2 compare the subgroup cohort to the overall cohort. Surgical sepsis was defined as patients admitted to a surgical or trauma ICU who were treated for sepsis with our institutional evidence-based sepsis bundle. Patient enrollment was approved by the University of Florida Institutional Review Board and registered with clinicaltrials.gov (NCT02276417).
Patient selection and enrollment
UF Health Gainesville patients admitted to the surgical ICU and entered into the standard-of-care sepsis protocol and meeting Sepsis-2 criteria were considered potential study candidates for the P50 sepsis study. Sepsis-2 criteria were used as the study began in 2015 prior to the development of Sepsis-3. Interim analysis of this cohort in 2017 demonstrated that only 7% of study patients that were classified as sepsis by Sepsis-2 would have been reclassified as infection by Sepsis-3 (because of lack attributable organ dysfunction) [29]. When various equivalent strata of Sepsis-2 and Sepsis-3 cohorts were compared, no significant difference in immune biomarkers, SOFA scores, inpatient clinical outcomes, discharge disposition, mortality, and long-term Zubrod performance status were found. A study research nurse assessed patients for study criteria and consented and enrolled appropriate candidates 24 h/day, 7 days a week [30]. A detailed description of the study design with specific inclusion and exclusion criteria as well as the clinical and laboratory standard operating procedure (SOPs) utilized has been published [29]. Exclusion criteria eliminated patients whose baseline immunosuppression, end-stage comorbidities, or severe functional disabilities would be a primary determinant of their long-term outcomes and thus confound outcome assessment.
Enrollment blood sampling and testing
While hospitalized, blood was drawn 12 h after enrollment on the first day of the study. Measures of lipid and lipoprotein levels and function included the following: 1) cholesterol levels, 2) HDL function and oxidation status (cell-free assay for Dys-HDL), and 3) HDL anti-oxidant activity (PON-1, ApoA-I). Myeloperoxidase (MPO), a pro-oxidant peroxidase enzyme released by neutrophils for bacterial killing, was also measured as it is known to contribute to oxidation of HDL and ApoA-I [31]. PON-1 is an HDL-associated esterase that protects lipoproteins, most likely by hydrolyzing lipid peroxides including oxidized cholesteryl esters and phospholipids [32].
Serum total cholesterol, HDL-C, and triglyceride levels were directly measured from serum samples. LDL-C was calculated using the Friedewald formula from total cholesterol, HDL-C, and triglyceride [33]. Dys-HDL and PON-1 activity were measured and reported as in prior studies [27]. Briefly, the cell-free assay for Dys-HDL requires HDL isolation from blood samples using dextran sulfate precipitation and LDL prepared from a normal donor. After incubating experimental (patient HDL plus control LDL) and control subject samples (control LDL only) with dichlorofluorescein, the ability of sample HDL to protect LDL from oxidation was quantitated by the decline in fluorescence and expressed as a ratio of the fluorescence released, the HDL inflammatory index (HII) [28]. PON-1 activity was quantified using paraoxon as the substrate and measuring the increase in absorbance at 405 nm due to the formation of 4-p-nitrophenol over a period of 12 min (at 20-s intervals). Paraoxon was purchased from Sigma-Aldrich (St. Louis, MO) and was further purified using chloroform extraction. One unit of PON-1 activity was defined as the formation of 1 nmole of 4-p-nitrophenol per minute per milliliter of sample used. Enzyme activity was measured with 40-fold-diluted plasma (final concentration) in a reaction mixture containing 4 mM paraoxon working solution, 500 mM glycine/10 mM CaCl2 buffer at pH 10.5, and 155 mM NaCl/3 mM NaN3 buffer at pH 8.2 [34]. Quantikine™ ELISA kits (R&D Systems, Inc, Minneapolis, MN) were used to measure plasma Apo A-I. Plasma MPO levels were measured using the MPO ELISA kit from Mercodia (Sweden).
Performance status assessments
Performance status was assessed using the ECOG/WHO/Zubrod Scale. Zubrod is calculated based on a 5-point scale that measures the performance status of a patients ambulatory abilities: 0, asymptomatic (fully active); 1, symptomatic but completely ambulatory (restricted in physically strenuous activity); 2, symptomatic, less than 50% in bed during the day (ambulatory and capable of all self-care but unable to perform any work activities); 3, symptomatic, greater than 50% in bed, but not bedbound (capable of only limited self-care); 4, bedbound (completely disabled, incapable of any self-care); and 5, death [3, 8]. Pre-sepsis baseline Zubrod scores were established via patient or surrogate interviews at 3 month follow-up visits and independently adjudicated by three members of the research team. Zubrod estimates were completed for participants with missing follow-up data based on qualitative notes taken during monthly phone calls or during clinic visits.
Data collection
All data were entered by trained research nurses and coordinators with investigator oversight. Study data were prospectively collected and included demographics, place of residence, source of infection, and Charlson comorbidities and score. Clinical variables including enrollment vital signs, timing of antibiotics, volume of intravenous fluids administered in the first six and 24 h, vasopressor use and duration in hours, mechanical ventilation use, central venous pressures (CVP), and urine output in the first six hours. Home medications including statin use were recorded. Admission disposition, hospital length of stay (LOS), and ICU LOS were documented. On the 4th day of admission, repeat clinical assessments were performed including repeat vital signs, hemodynamic and ventilator requirements, and SOFA score. Chart reviews after enrollment were performed to confirm source of infection and sepsis diagnosis, culture results, ICU and hospital LOS, and discharge disposition. Mortality information was acquired by monthly follow-up phone calls or from the social security death index.
Clinical outcomes and adjudication
The two primary outcomes of interest were (1) poor performance status outcomes at 1 year (defined as Zubrod score of 3/4/5) and (2) 1-year survival. Based on our previous studies, there were three short-term study endpoints (clinical trajectories) included: (1) incidence of early death (within 2 weeks of hospital admission), (2) CCI (total ICU stay > 14 days or total ICU ≤ 14 days but discharged to long-term acute care, another hospital, or hospice), or (3) rapid recovery (all others) [35]. Patients were further classified as having a good disposition if they were discharged to home or a rehabilitative facility, and poor disposition if they were discharged to LTAC, skilled nursing facility, another hospital, hospice, or died. The senior author (FAM) and his team of surgical intensivist co-investigators performed adjudications via weekly group adjudication meetings [36]. Data were only included for patients who had values for lipid biomarkers and functional outcomes measured included as part of the prospective study.
Sample size and data analysis
The study was powered to detect a correlation between HII and SOFA score. We calculated that a sample size of 160 patients, accounting for 15% early mortality (resulting in at least 136 living), would have 84% power to detect a Pearson correlation coefficient of 0.25 between change in HII and change in SOFA score over the first 48–72 h. These correlations are not presented in this manuscript as they were previously published [25].
Data are presented as frequency and percentages or medians with interquartile ranges for categorical and continuous variables, respectively. Zubrod plots were created by plotting Zubrod score at enrollment, 3, 6, and 12 months by quartiles of lipid levels, functional, and MPO levels. The first quartile contained patients with the lowest biomarker levels, while the fourth quartile had patients with the highest biomarker levels. We used Fisher’s exact test for comparison of categorical variables and the Kruskal–Wallis test for comparison of continuous variables. The log-rank test was used to compare Kaplan–Meier product limit estimates of survival between groups. Following univariate analysis, multivariate stepwise logistic regression models were used to determine independent risk factors predictive of (1) poor performance status (Zubrod 3/4/5) at 1 year and (2) 1-year survival. ApoA-I values were large, and therefore, log-transformed values were used in statistical modeling to generate interpretable confidence intervals. Multivariate stepwise cox regression models were used to determine factors associated with 1-year survival time. For both logistic regression and Cox regression models, we first examined the association between various parameters of interest and the outcomes of poor physical function and mortality at 1-year follow-up, respectively. Parameters found statistically significant on univariate analysis were considered for inclusion in the multivariate models. We list the parameters considered for inclusion in each model below each respective section of Table 5. Stepwise selection was used to determine the final multivariable models with a p value of 0.1 used for entry and retention into the model. Otherwise, significance tests were two-sided, with p value ≤ 0.05 considered statistically significant. Statistical analyses were performed with SAS version 9.4 (Cary, NC; U.S.A.).
Results
The study included 104 patients with surgical sepsis. Patient demographics and reason for hospital admission for this cohort are depicted in Table 1. The same comparisons to 363 patients enrolled to the larger P50 grant study are depicted in Additional file 1: Table S1. There was no demonstrable selection bias for this sub-study compared to the overall cohort. The median age of the 104 study patients was 63 years (IQR 51, 72), there were more males than females (55%), and patients were predominantly White. The most common comorbidities were hypertension, followed by diabetes mellitus, and coronary artery disease. The majority of patients were admitted for an active infection (60%), followed by planned surgery (20%) as the second most common reason for hospital admission. A large proportion of patients were transferred from other institutions (41%).
Table 2 displays data on source of infection, disease severity, and surgical interventions. The most common infection type was surgical site infection, followed by intra-abdominal, and urinary tract. Just over half of patients were culture positive. Most patients had sepsis present at the time of admission, while 41% had hospital-acquired infections. Median Apache II and SOFA scores were high, reflecting the severity of illness as all patients were admitted to the ICU. Just over half of patients had an emergency surgery within 24 h of hospital presentation, and two-thirds had a source control procedure at some point in their hospital stay.
Table 3 displays data on inpatient care and patient outcomes. The median hospital length of stay (LOS) was nearly 2 weeks and most patients were on mechanical ventilation at some point during the hospitalization. A surprising small number of patients died early (7%). The majority of patients had rapid recovery (60%), however, of note just over one-third progressed into CCI. Sixty percent of study patients were discharged with a good disposition (home or rehab facility), and 40% percent were discharged with a poor disposition (LTAC, skilled nursing facility, another hospital, hospice, or death). A substantial proportion of patients (37%) had poor performance status (Zubrod 3/4/5) 1 year after sepsis. Mortality at one year was 23%.
Lipid levels, function, and oxidative biomarkers are presented in Table 4. Enrollment total cholesterol and high-density lipoprotein (HDL-C) levels were lower and myeloperoxidase (MPO) levels were higher for patients with poor performance status at 1 year. Plots of Zubrod scores at enrollment, 3, 6, and 12 months by lipid levels, function, and MPO level quartiles are displayed in Fig. 1. From Fig. 1, patients with the lowest quartile total cholesterol levels had significantly higher Zubrod scores at 3 and 6 months, while patients with higher HDL-C levels had lower Zubrod scores at 3 and 12 months. Similar trends were seen with LDL-C levels, in which lower quartiles were associated with higher Zubrod scores at 3 and 6 months. Lower ApoA-I levels were also associated with higher Zubrod scores at 3 months. A similar trend was seen in comparisons based on 1-year mortality, with HDL-C and ApoA-I levels being lower and MPO levels being higher in non-survivors.
Quartiles of ECOG/WHO/Zubrod score plotted at baseline, 3, 6, and 12 months for: a TC (total cholesterol), b high-density lipoprotein-cholesterol (HDL-C), c low-density lipoprotein-cholesterol (LDL-C), d triglycerides (TG), e HDL inflammatory index (HII), f paraoxonase-1 (PON-1), g apolipoprotein A-I (ApoA-I), and h myeloperoxidase (MPO). Differences at each time point are represented by colored lines for lipid biomarker quartiles with standard error bars, with asterisks indicating significant differences per timepoint
After adjusting for other covariates including disease severity, multivariable logistic regression identified baseline Zubrod score and initial SOFA score as significant independent predictors of poor performance status at 1 year. Survival curves based on quartiles of lipid levels, function, and oxidative biomarkers are presented in Fig. 2. Multivariable Cox regression modeling for 1-year survival identified high Charlson comorbidity score, low ApoA-I levels, and longer vasopressor duration use as predictors of mortality over 1 year. Regression model results are presented in Table 5.
: Kaplan–Meier survival curves over 1 year after sepsis are presented by quartiles for a TC (total cholesterol), b high-density lipoprotein-cholesterol (HDL-C), c low-density lipoprotein-cholesterol (LDL-C), d triglycerides (TG), e HDL inflammatory index (HII), f paraoxonase-1 (PON-1), g apolipoprotein A-I (ApoA-I), and h myeloperoxidase (MPO)
Discussion
In this study of lipid biomarkers in patients with surgical sepsis, only Apo A-I was a significant independent predictor of 1-year survival. None of our lipid markers were found to be significant independent predictors of poor performance status at 1 year. After adjustment for other factors, only baseline Zubrod score and SOFA score predicted poor performance status. In the multivariable Cox regression model, higher Charlson score, longer duration of vasopressor use, and lower ApoA-I levels predicted 1-year mortality. Both greater chronic comorbidities and septic shock are known to portend poor long-term outcomes both in terms of organ function and mortality [4, 35, 37].
To our knowledge, this is the first study to evaluate the relationship between lipid biomarkers and physical performance status and long-term morbid outcomes in surgical sepsis patients. Functional outcomes and long-term mortality are highly relevant outcomes for modern sepsis research as in-hospital survival has improved due to advances in sepsis management. Recently, early recognition and evidence-based care have led to improved short-term outcomes [38,39,40]. However, a large proportion of patients are left with considerable residual morbidity, and much of the burden of disease is transferred to the post-hospital setting where mortality and physical function data are not reported [3, 4]. Our group has recently demonstrated the breadth and severity of poor functional outcomes after surgical sepsis across the spectrum of patients, and has shown the discordance between seemingly low short-term mortality rates and the prevalence of poor performance status and high mortality at 1 year [3, 35, 41] This may be attributed to PICS as the underlying pathobiology of the CCI phenotype, where inflammation, immunosuppression, and catabolism contribute to these outcomes. In surgical sepsis, repeated exposures to inflammation-propagating procedures contribute to the maladaptive cycle of persistent inflammation involving reduced host protective immunity, continued organ injury, which include loss of muscle mass and function, change in bone marrow function, and failure of metabolic adaptation [9]. In this study, we had the ability to perform long-term follow-up assessments on our patients, which provided valuable data on quality of life and mortality after discharge. Of the patients who survived hospital discharge, roughly half of the patients either had poor physical function or were dead 1 year after sepsis. Emergency surgery contributes to and perpetuates this vicious cycle, which likely contributes to the very high incidence of CCI and poor physical function reported in this study.
Lipid biomarkers have long been shown to be highly associated and predictive of outcomes in sepsis [42, 43]. Low LDL-C, total cholesterol, and HDL-C levels have been associated with increased sepsis risk and poor outcomes [28, 42,43,44,45]. High-density lipoprotein-cholesterol (HDL-C) is protective against sepsis by several mechanisms including bacterial toxin binding [13, 18], suppression of inflammatory cell migration, prevention of inflammatory cytokine release [46, 47], inhibition of vascular and intercellular adhesion molecules expression [31, 48], and stimulation of endogenous corticosteroid release [16, 17]. ApoA-I has been shown to be a potent anti-oxidant and anti-inflammatory, a mechanism that may provide an explanation for the association of low levels with poor sepsis outcomes. In a recent study of rats, an ApoA-I mimetic peptide (4F) was administered to rats with induced sepsis via cecal ligation and puncture. Rats treated with 4F were found to have suppression of sepsis-induced changes in serum cholesterol, LDL, HDL, and ApoA-I levels, reduced inflammation, and protection of cardiac and renal function [49]. The use of HDL and ApoA-I mimetics has been proposed as potential therapeutic options for improving sepsis outcomes [14, 49, 50]. Others have focused on LDL-C and its ability to bind and clear endotoxin via hepatocytes in models of Gram-negative sepsis [22,23,24]. Specific to this idea is the concept of PCSK9 inhibition, and the resultant maintenance of LDL-C receptors on the surface of hepatocytes allowing for increased endotoxin clearance from circulation and elimination via the biliary tract. This implies the potential use of PCSK9 inhibitors to improve outcomes from sepsis, though this has not been tested.
In this study, we report results of the functional and anti-oxidant status of HDL. The HII provides an index of HDL’s oxidation status, while PON-1 activity and ApoA-I levels provide data on HDL’s function as an anti-oxidant. MPO activity, which is known to play a role in oxidizing HDL, was also reported. Though HII and PON-1 activity were not significantly different for patients with poor functional outcomes and long-term mortality, MPO and ApoA-I levels were significantly different in univariate comparisons, while only ApoA-I was predictive in multivariable analyses. MPO is elevated in infection and has been shown to contribute to the generation of dysfunctional HDL with impaired cholesterol efflux mediated by HDL [51]. The overall body of literature in this arena supports our findings that ApoA-I may be central to the dysregulated metabolism of sepsis.
In our review, we were unable to find other studies reporting on the predictive ability of lipids for long-term physical function in sepsis survivors. There are a few studies, however, that report on lipid prediction of long-term outcomes after sepsis. Wei and colleagues recently showed the predictive ability of low HDL-C levels and ApoA-I levels in predicting long-term mortality in patients with infective endocarditis [52]. Genga and colleagues also recently reported that patients with low HDL had greater frequency of worsened acute kidney injury, and long-term decreases in glomerular filtration rate (eGFR) up to 2 years after sepsis [53]. We have previously shown that low LDL-C levels, after adjusting for other factors, lead to increased sepsis risk over the subsequent years in a study of 30,000 community dwelling adults in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study [26]. Future studies should explore the mechanisms of lipid metabolism and dysregulation, the presence of bioactive lipid metabolites over time, and the genomic changes in lipid regulatory genes to deepen our understanding of lipid dysregulation in sepsis. In addition, studies should continue to focus on physical performance status as a meaningful indicator of sepsis recovery as well as long-term mortality.
There were two main limitations to this study. First, this was a small cohort of patients with surgical sepsis. Because of the small sample size, we may have been underpowered to detect additional differences and lipid predictors that would have been detected in a larger sample of patients. Second, this was a study of surgical sepsis patients that were treated for predominantly surgical infections. As such, these outcomes may not be necessarily generalized to a broader sepsis population and findings should be validated in a large more diverse cohort.
Conclusions
In this study of patients with surgical sepsis, ApoA-I was the only lipid or lipoprotein biomarker found to be predictive of 1-year mortality after adjusting for other variables including disease severity. None of our lipid or lipoprotein biomarkers were found to be predictive of poor performance status at 1 year. Large studies in a more diverse cohort of community and hospital-acquired sepsis patients should be undertaken to validate these findings. Mechanistic studies should also be performed to better understand mechanisms of lipid dysregulation in sepsis.
Availability of data and materials
Supporting data from this study can be obtained by emailing the corresponding author Dr. Faheem W. Guirgis, MD.
References
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801. https://doi.org/10.1001/jama.2016.0287.
Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–11. https://doi.org/10.1016/S0140-6736(19)32989-7.
Gardner AK, Ghita GL, Wang Z, et al. The development of chronic critical illness determines physical function, quality of life, and long-term survival among early survivors of sepsis in surgical ICUs*. Crit Care Med. 2019;47(4):566–73. https://doi.org/10.1097/CCM.0000000000003655.
Guirgis FW, Brakenridge S, Sutchu S, et al. The long-term burden of severe sepsis and septic shock: Sepsis recidivism and organ dysfunction. J Trauma Acute Care Surg. 2016. https://doi.org/10.1097/TA.0000000000001135.
Guirgis FW, Khadpe JD, Kuntz GM, Wears RL, Kalynych CJ, Jones AE. Persistent organ dysfunction after severe sepsis: a systematic review. J Crit Care. 2014;29:3. https://doi.org/10.1016/j.jcrc.2013.10.020.
Mira JC, Gentile LF, Mathias BJ, et al. Sepsis pathophysiology, chronic critical illness, and persistent inflammation-immunosuppression and catabolism syndrome. Crit Care Med. 2016. https://doi.org/10.1097/CCM.0000000000002074.
Gentile LF, Cuenca AG, Efron PA, et al. Persistent inflammation and immunosuppression: a common syndrome and new horizon for surgical intensive care. J Trauma Acute Care Surg. 2012;72(6):1491–501. https://doi.org/10.1097/TA.0b013e318256e000.
Hawkins RB, Raymond SL, Stortz JA, et al. Chronic critical illness and the persistent inflammation, immunosuppression, and catabolism syndrome. Front Immunol. 2018;9:1511. https://doi.org/10.3389/fimmu.2018.01511.
Rb H, Sl R, Ja S, et al. Chronic critical illness and the persistent inflammation, immunosuppression, and catabolism syndrome. Front Immunol. 2018;9:1511. https://doi.org/10.3389/FIMMU.2018.01511.
Stortz JA, Mira JC, Raymond SL, et al. Benchmarking clinical outcomes and the immunocatabolic phenotype of chronic critical illness after sepsis in surgical intensive care unit patients. J Trauma Acute Care Surg. 2018;84(2):342–9. https://doi.org/10.1097/TA.0000000000001758.
Moore LJ, Moore FA. Epidemiology of sepsis in surgical patients. Surg Clin North Am. 2012;92(6):1425–43. https://doi.org/10.1016/J.SUC.2012.08.009.
Green P, Theilla M, Singer P. Lipid metabolism in critical illness. Curr Opin Clin Nutr Metab Care. 2016;19(2):111–5. https://doi.org/10.1097/MCO.0000000000000253.
Khovidhunkit W, Kim M-S, Memon RA, et al. Effects of infection and inflammation on lipid and lipoprotein metabolism: mechanisms and consequences to the host. J Lipid Res. 2004;45:1169–96. https://doi.org/10.1194/jlr.R300019-JLR200.
Morin EE, Guo L, Schwendeman A, Li X-A. HDL in sepsis - risk factor and therapeutic approach. Front Pharmacol. 2015;6:244. https://doi.org/10.3389/fphar.2015.00244.
Walley KR. Role of lipoproteins and proprotein convertase subtilisin/kexin type 9 in endotoxin clearance in sepsis. Curr Opin Crit Care. 2016;22(5):464–9. https://doi.org/10.1097/MCC.0000000000000351.
Guo L, Ai J, Zheng Z, et al. High density lipoprotein protects against polymicrobe-induced sepsis in mice. J Biol Chem. 2013;288(25):17947–53. https://doi.org/10.1074/jbc.M112.442699.
Guo L, Zheng Z, Ai J, et al. Scavenger receptor BI and high-density lipoprotein regulate thymocyte apoptosis in sepsis. Arterioscler Thromb Vasc Biol. 2014;34(5):966–75. https://doi.org/10.1161/ATVBAHA.113.302484.
Catapano AL, Pirillo A, Bonacina F, Norata GD. HDL in innate and adaptive immunity. Cardiovasc Res. 2014.
Beutler B, Hoebe K, Du X, Ulevitch RJ. How we detect microbes and respond to them: the Toll-like receptors and their transducers. J Leukoc Biol. 2003;74:479–85. https://doi.org/10.1189/jlb.0203082.
Parrillo JE. Pathogenetic mechanisms of septic shock. N Engl J Med. 1993;328:1471–7.
Kitchens RL, Wolfbauer G, Albers JJ, Munford RS. Plasma lipoproteins promote the release of bacterial lipopolysaccharide from the monocyte cell surface. J Biol Chem. 1999;274(48):34116–22.
Topchiy E, Cirstea M, Kong HJ, et al. Lipopolysaccharide is cleared from the circulation by hepatocytes via the low density lipoprotein receptor. PLoS ONE. 2016;11(5):e0155030. https://doi.org/10.1371/journal.pone.0155030.
Boyd JH, Fjell CD, Russell JA, Sirounis D, Cirstea MS, Walley KR. Increased Plasma PCSK9 levels are associated with reduced endotoxin clearance and the development of acute organ failures during sepsis. J Innate Immun. 2016;8(2):211–20. https://doi.org/10.1159/000442976.
Walley KR, Thain KR, Russell JA, et al. PCSK9 is a critical regulator of the innate immune response and septic shock outcome. Sci Transl Med. 2014;6(258):258143. https://doi.org/10.1126/scitranslmed.3008782.
Guirgis FW, Dodani S, Leeuwenburgh C, et al. HDL inflammatory index correlates with and predicts severity of organ failure in patients with sepsis and septic shock. PLoS ONE. 2018;13(9):e0203813. https://doi.org/10.1371/journal.pone.0203813.
Guirgis FW, Donnelly JP, Dodani S, et al. Cholesterol levels and long-term rates of community-acquired sepsis. Crit Care. 2016;20(1):408. https://doi.org/10.1186/s13054-016-1579-8.
Guirgis FW, Leeuwenburgh C, Grijalva V, et al. HDL cholesterol efflux is impaired in older patients with early sepsis: a subanalysis of a prospective pilot study. Shock. 2018;50:1. https://doi.org/10.1097/SHK.0000000000001030.
Guirgis FW, Dodani S, Moldawer L, et al. Exploring the predictive ability of dysfunctional high density lipoprotein for adverse outcomes in emergency department patients with sepsis. Shock. 2017. https://doi.org/10.1097/SHK.0000000000000887.
Brakenridge SC, Lysak N, Ghita G, et al. Comparison of sepsis-2 and sepsis-3 clinical criteria in critically ill patients: is there any impact on discrimination of immunophenotype and clinical outcomes? Shock. 2018. https://doi.org/10.1097/SHK.0000000000001158.
Loftus TJ, Mira JC, Ozrazgat-Baslanti T, et al. Sepsis and critical illness research center investigators: protocols and standard operating procedures for a prospective cohort study of sepsis in critically ill surgical patients. BMJ Open. 2017. https://doi.org/10.1136/bmjopen-2016-015136.
Rosenson RS, Brewer HB, Ansell BJ, et al. Dysfunctional HDL and atherosclerotic cardiovascular disease. Nat Rev Cardiol. 2015;13(1):48–60. https://doi.org/10.1038/nrcardio.2015.124.
Wu A, Hinds CJ, Thiemermann C. High-density lipoproteins in sepsis and septic shock: metabolism, actions, and therapeutic applications. Shock. 2004;21(3):210–21. https://doi.org/10.1097/01.shk.0000111661.09279.82.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Charles-Schoeman C, Lee YY, Shahbazian A, et al. Association of paraoxonase-1 gene polymorphism and enzyme activity with carotid plaque in rheumatoid arthritis. Arthritis Rheum. 2013;65(11):2765–72. https://doi.org/10.1002/art.38118.
Brakenridge SC, Efron PA, Cox MC, et al. Current epidemiology of surgical sepsis: discordance between inpatient mortality and 1-year outcomes. Ann Surg. 2019;270(3):502–10. https://doi.org/10.1097/SLA.0000000000003458.
Loftus TJ, Mira JC, Ozrazgat-Baslanti T, et al. Sepsis and Critical Illness Research Center investigators: protocols and standard operating procedures for a prospective cohort study of sepsis in critically ill surgical patients. BMJ Open. 2017;7(7):e015136. https://doi.org/10.1136/bmjopen-2016-015136.
Linder A, Lee T, Fisher J, et al. Short-term organ dysfunction is associated with long-term (10-Yr) mortality of septic shock. Crit Care Med. 2016. https://doi.org/10.1097/CCM.0000000000001843.
Guirgis FW, Jones L, Esma R, et al. Managing sepsis: Electronic recognition, rapid response teams, and standardized care save lives. J Crit Care. 2017;40:296–302. https://doi.org/10.1016/j.jcrc.2017.04.005.
Croft CA, Moore FA, Efron PA, et al. Computer versus paper system for recognition and management of sepsis in surgical intensive care. J Trauma Acute Care Surg. 2014;76(2):311–9. https://doi.org/10.1097/TA.0000000000000121.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign. Crit Care Med. 2017. https://doi.org/10.1097/CCM.0000000000002255.
Mankowski RT, Anton SD, Ghita GL, et al. Older sepsis survivors suffer persistent disability burden and poor long-term survival. J Am Geriatr Soc. 2020. https://doi.org/10.1111/jgs.16435.
Chien J-Y, Jerng J-S, Yu C-J, Yang P-C. Low serum level of high-density lipoprotein cholesterol is a poor prognostic factor for severe sepsis. Crit Care Med. 2005;33(8):1688–93.
Chien Y-F, Chen C-Y, Hsu C-L, Chen K-Y, Yu C-J. Decreased serum level of lipoprotein-cholesterol is a poor prognostic factor for patients with severe community-acquired pneumonia that required intensive care unit admission. J Crit Care. 2015;30(3):506–10. https://doi.org/10.1016/j.jcrc.2015.01.001.
van Leeuwen HJ, Heezius ECJM, Dallinga GM, van Strijp JAG, Verhoef J, van Kessel KPM. Lipoprotein metabolism in patients with severe sepsis. Crit Care Med. 2003;31(5):1359–66. https://doi.org/10.1097/01.CCM.0000059724.08290.51.
Lagrost L, Girard C, Grosjean S, et al. Low preoperative cholesterol level is a risk factor of sepsis and poor clinical outcome in patients undergoing cardiac surgery with cardiopulmonary bypass. Crit Care Med. 2014;42(5):1065–73. https://doi.org/10.1097/CCM.0000000000000165.
Murphy AJ, Woollard KJ, Hoang A, et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol. 2008;28(11):2071–7. https://doi.org/10.1161/ATVBAHA.108.168690.
Murphy AJ, Woollard KJ, Suhartoyo A, et al. Neutrophil activation is attenuated by high-density lipoprotein and apolipoprotein A-I in in vitro and in vivo models of inflammation. Arterioscler Thromb Vasc Biol. 2011;31(6):1333–41. https://doi.org/10.1161/ATVBAHA.111.226258.
Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation. 2001;104:2673–8. https://doi.org/10.1161/hc4601.099485.
Moreira RS, Irigoyen M, Sanches TR, et al. Apolipoprotein A-I mimetic peptide 4F attenuates kidney injury, heart injury, and endothelial dysfunction in sepsis. Am J Physiol Regul Integr Comp Physiol. 2014;307(5):R514–24. https://doi.org/10.1152/ajpregu.00445.2013.
Sharifov OF, Xu X, Gaggar A, et al. Anti-inflammatory mechanisms of apolipoprotein A-I mimetic peptide in acute respiratory distress syndrome secondary to sepsis. PLoS ONE. 2013;8(5):e64486. https://doi.org/10.1371/journal.pone.0064486.
Shao B, Tang C, Sinha A, et al. Humans with atherosclerosis have impaired ABCA1 cholesterol efflux and enhanced high-density lipoprotein oxidation by myeloperoxidase. Circ Res. 2014;114(11):1733–42. https://doi.org/10.1161/CIRCRESAHA.114.303454.
Wei X-B, Chen X-J, Li Y-L, et al. Apolipoprotein A-I: A favorable prognostic marker in infective endocarditis. J Clin Lipidol. 2018;12(2):498–505. https://doi.org/10.1016/j.jacl.2017.12.005.
Roveran Genga K, Lo C, Cirstea M, et al. Two-year follow-up of patients with septic shock presenting with low HDL: the effect upon acute kidney injury, death and estimated glomerular filtration rate. J Intern Med. 2017;281(5):518–29. https://doi.org/10.1111/joim.12601.
Acknowledgements
The authors are grateful for the contributions of the UF Emergency Medicine Research Coordinators, including Andrew Bertrand, Alexis Hester, Esteban Velasquez, Taylor Munson, and Vasili Pleqi. The authors would also like to acknowledge the invaluable contributions of the UF Sepsis and Critical Illness Research Center staff, including Jennifer Lanz, Ruth Davis, Jillianne Brakenridge, Ashley McCray, Bridget Baisden, Ricky Ungaro, Dina Nacionales, Marvin Dirain, Tabitha Johns, and Ada Malcolm.
Funding
This study was supported by National Institutes of General Medical Sciences K23GM115690, P50GM111152, and R01GM133815.
Author information
Authors and Affiliations
Contributions
FWG, FAM, CL, LM, LP, ED, and ST devised the study. FWG, CL, LLM, GG, LPB, MH, ED, PH, SR, and FAM contributed to the conception and design of the project, as well as drafting of the manuscript, revision of its content, and approval of the manuscript in its final form. CL, LLM, and ST provided expertise and contributed to the content regarding inflammation and pathobiology of sepsis. CL and ST provided expertise in lipid and lipoprotein metabolism. FAM supervised the data collection and chart reviews. MH and DH assisted with data cleaning and integrity. GG performed the statistical analysis with oversight from FWG and FAM. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review boards of the University of Florida College of Medicine, and all participants provided written consent before study participation.
Consent for publication
All authors have provided consent for publication of the manuscript.
Competing Interests
Authors Guirgis, Leeuwenburgh, Moldawer, Ghita, Black, Henson, DeVos, Holden, Efron, Reddy, and Moore do not report any related conflicts of interest. All authors have read Biomed Central’s section on competing interests and have no competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Demographics of lipid study cohort vs. entire P50 cohort. APACHE, acute physiology and chronic health evaluation.
Additional file 2: Table S2.
Outcomes of Lipid study cohort vs. entire P50 cohort. LOS, length of stay; ICU, intensive-care unit.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guirgis, F.W., Leeuwenburgh, C., Moldawer, L. et al. Lipid and lipoprotein predictors of functional outcomes and long-term mortality after surgical sepsis. Ann. Intensive Care 11, 82 (2021). https://doi.org/10.1186/s13613-021-00865-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-021-00865-x