Abstract
Neurodegenerative diseases represent a large group of neurological disorders including Alzheimer’s disease, amyotrophic lateral sclerosis, Parkinson’s disease, and Huntington’s disease. Although this group of diseases show heterogeneous clinical and pathological phenotypes, they share important pathological features characterized by the age-dependent and progressive degeneration of nerve cells that is caused by the accumulation of misfolded proteins. The association of genetic mutations with neurodegeneration diseases has enabled the establishment of various types of animal models that mimic genetic defects and have provided important insights into the pathogenesis. However, most of genetically modified rodent models lack the overt and selective neurodegeneration seen in the patient brains, making it difficult to use the small animal models to validate the effective treatment on neurodegeneration. Recent studies of pig and monkey models suggest that large animals can more faithfully recapitulate pathological features of neurodegenerative diseases. In this review, we discuss the important differences in animal models for modeling pathological features of neurodegenerative diseases, aiming to assist the use of animal models to better understand the pathogenesis and to develop effective therapeutic strategies.
Similar content being viewed by others
Introduction
Neurodegenerative diseases such as Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington's disease (HD), and Amyotrophic lateral sclerosis (ALS) are incurable and have been one of the most challenging health issues. The common feature of these diseases is a progressive loss of specific populations of neurons in the aging human brain [1]. With increasing life expectancies, the incidence of neurodegenerative diseases is rapidly growing worldwide.
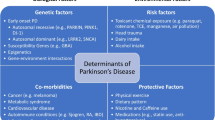
AD, which is the most common form of neurodegenerative diseases, affects about 7–8% people over age 65. The main clinical manifestations of AD include progressive memory loss, cognitive dysfunction, behavioral disorders, and other related impairments. Neuropathologically, AD is characterized by extracellular senile amyloid plaques and intracellular neurofibrillary tangles (NFTs), along with other molecular changes such as neuroinflammation, brain atrophy, synaptic pathologies, and cerebral amyloid angiopathy [2, 3].More than 90% of patients with AD are sporadic cases and show dementia in their mid-60 s and later, and less than 10% of AD cases have the early-onset form of diseases that can be caused by a single genetic mutation in the APP genes (Presenilin 1, Presenilin 2, and Amyloid precursor protein APP) [4]. Parkinson’s disease (PD) is the second most common neurodegenerative disorder that affects more than 1% people over age 60. The pathologic hallmarks of PD are the preferential loss of dopamine (DA) neurons and formation of Lewy body inclusions in the substantia nigra pars compacta [5]. Like AD, the majority of PD cases are sporadic, and mutations in the genes encoding alpha-synuclein, PINK1, Parkin, LRRK2 and others have been found in 10–15% of familial PD cases [6]. ALS is also a progressive neurodegenerative disease that particularly affects motor neurons in the brain and the spinal cord, resulting in the loss of muscle movement [7]. Similar to AD and PD, most ALS patients are sporadic, and about 5%-10% of patients suffer from the familial form of ALS. The familial ALS could be caused by various mutations of genetic loci, including TAR DNA-binding protein 43 (TDP- 43), superoxide dismutase 1 (SOD1), fused in sarcoma (FUS), and C9ORF72 [8, 9]. On the other hand, HD shows autosomal dominance with full penetration, which is caused by a CAG repeat expansion (> 36 CAGs) in exon 1 of the HD gene that is translated to a polyglutamine (polyQ) repeat in the disease protein huntingtin (HTT) [10, 11].The polyQ expansion causes HTT to misfold and aggregate in the patient brain, resulting in the preferential loss of the medium spiny neurons in the striatum and extended neurodegeneration in various brain regions as HD progresses [11]. Currently, effective therapies are still lacking for these neurodegenerative diseases, and no proven treatment can halt or slow the progression of these diseases. Animal models that can recapitulate key pathological changes that occurring in the patient brains would be important for developing effective therapeutic strategies.
The emerging need to use large animal models to study neurodegenerative diseases
The genetic mutations identified in the neurodegenerative disease genes make it possible to use genetic manipulation for modeling these diseases in animals, which are essential to our understanding of the disease pathogenesis. A variety of genetically modified animal models, mostly in rodents, have been generated to study the pathogenesis and therapeutics for neurodegenerative diseases. The rodent models have provided important insights into the pathogenesis of neurodegenerative diseases. For example, the mouse models can remarkably recapitulate protein misfolding and aggregation seen in the patient brains [12,13,14]. However, most of the mouse models cannot fully mimic the symptoms and pathologies of neurodegenerative diseases. For example, although the current HD mouse models show age-dependent accumulation of mutant HTT and associated neurological symptoms, they lack overt and selective medium spiny neuronal loss that is seen in HD patients [15, 16]. Similar to HD mouse models, the majority of AD transgenic mouse models have no overt neuronal loss in the cortex and hippocampus, and nearly all the PD transgenic mouse models have no obvious loss of dopamine (DA) neurons, a pathologic hallmark of PD [17, 18].
The differences in neuropathology between rodent models and patient brains with neurodegenerative diseases could be due to species differences determined by genomic, molecular, and anatomic differences between rodents and humans (Table 1). The brain development is considerably different in mouse and human: the human brain requires more than 10 months to fully develop, whereas the formation of mouse brain only takes 21 days [19]. As a result, the brain structures in large animals and rodents are also noticeably different. For example, the rodent brains lack gyrification that exists in the brains of large mammals (such as pig, monkey and human). Another example is that the striatum, which is the most affected region in HD, consists of the caudate nucleus and putamen in large animal brains while these two parts are indistinguishable in rodents [20]. The differences in anatomical structure and neuropathology between rodent and human brains highlight the demand for using larger animals that are closer to humans for modeling neurodegenerative diseases. Particularly, when CRISPR-Cas9 is available to edit the genes in large animals to mimic human genetic mutations, it becomes more feasible to generate large animal models of neurodegenerative diseases.
Genome editing in large animals
Although the modern transgenic methods have been used to establish large animal models, the transgene was randomly introduced into the chromosomes and may not yield the endogenous expression level of mutant genes. Furthermore, the following limitations make it difficult to create large animal models that can mimic germline transmissible mutations: the lack of embryonic stem cells (ESCs) for in vitro genome editing, the low efficiency of homologous recombination, and the long-life cycle. Thus, the recently developed nuclease-mediated genome editing technology (CRISPR/Cas9) that can modify the endogenous genome makes it feasible to expand genetic engineering to many species, especially large animals.
CRISPR/Cas9 has now been used for genome editing in non-human primates [21,22,23,24]. The development of base editor system [25, 26] is particularly useful to introduce a point mutation in the endogenous genes [27, 28]. These new gene-editing tools can efficiently modify the endogenous genome of a variety of species in vitro and in vivo and can be used with embryonic stem cell culture, somatic nuclear transfer, and brain stereotaxic injection to edit genes in embryos and adult cells (Fig. 1). Thus, although embryonic stem cells of large animals are still not available for genome editing, CRISPR/Cas9 in combination with other technology has enabled the establishment of several large animal models that harbor genetic mutations found in humans.
For generating monkey models, germline genome editing can be achieved by injection of transgene or CRISPR/Cas9 into the fertilized eggs. However, the long-life cycle and the high costs of the non-human primates prevent the widespread use of this important animal model. Since CRISPR/Cas9 can also target genes in adult neuronal cells [29,30,31], it can be applied to the brains of adult monkeys via stereotaxic injection of viral expression vectors. Such studies would allow one to explore the function of mutant genes in adult monkey and also to more rapidly generate monkey models that can mimic brain region-specific neurodegeneration (Fig. 2).
Strategies to generate monkey models of neurodegenerative diseases. Genetic modifications in monkey embryos can be achieved by microinjection of transgene or CRISPR/Cas9 to target the endogenous gene. Alternatively, stereotaxic injection of viral vectors expressing transgene or CRISPR/Cas9 into specific brain regions of adult monkey can result in brain region-dependent gene editing
Pig is another commonly used large animal that shares considerable similarities with humans in body size, organ(s) physiology and anatomical dimensions. In comparison to non-human primates, there are several advantages of pigs: generation of multiple piglets (6–12 piglets from a single sow), short gestation time (about 120 days), and relatively lower costs [32]. Importantly, pig models can be established using somatic cell nuclear transfer (SCNT) to introduce genetic mutations in the endogenous pig genes to generate knock-in and knock-out models [20, 33,34,35]. Thus, pigs have become important in modeling a number of human diseases and are also used in human organ xenotransplantation.
Large animal models of Huntington's disease
Genetically modified large animal models of HD, PD, ALS, and AD are summarized in Table 2. Of these animal models, HD transgenic monkey model was the first transgenic monkey model of human diseases, which was established by injecting lentiviruses into fertilized rhesus monkey oocytes to express exon1 (1–67) mutant HTT containing 84Q [36]. Because of the monogenetic mutation (CAG repeat expansion) in HD, expressing expanded CAG repeats in animals has been used to generate a variety of HD animal models. Unlike transgenic HD mice that express the same transgenic HTT and can survive after birth without overt neurodegeneration [37], the HD transgenic monkeys died postnatally and showed severe neurodegeneration [36]. Transgenic HD pigs that express N-terminal mutant HTT (1–208) containing 105Q were then generated via somatic nuclear transfer, and most of the transgenic HD piglets also died postnatally and showed apoptotic cells in their brains [38]. However, the transgenic mice expressing the same mutant HTT fragment could live up to 9 months [38], suggesting the N-terminal mutant HTT is more toxic in larger animal models.
Transgenic pigs expressing a large fragment of mutant HTT (1–548) containing 124Q were also generated by lentiviral infection of porcine embryos. However, these transgenic HD pigs showed much milder phenotypes and did not die after birth [39, 40]. Because transgene expression is largely controlled by the promoter that drives transgene expression and copy numbers as well as chromosomal location of the transgene, it is possible that the transgenic HTT expression level in these HD pigs is not high enough to induce early and severe neuropathology. In line with this possibility, transgenic sheep that express full-length mutant HTT with 73Q and were generated via microinjection into pronuclei of single-celled zygotes show very mild phenotypes [41]. Because somatic nuclear transfer ensures the transgene expression in each cell while viral infection or microinjection of fertilized oocytes can lead to various degrees of transgene expression in different types of cells, the different phenotypes in transgenic HD animals are clearly dependent on the transgene expression.
To overcome the limitation of transgenic approach, a HD knock-in pig model was generated via CRISPR/Cas9 and somatic nuclear transfer, which expresses an expanded polyCAG (150 CAG) in the pig HTT gene and precisely mimics the genetic mutation that occurs in the endogenous HTT gene [20]. Importantly, when full-length mutant HTT with 150Q is endogenously expressed in this HD pig model, it causes striking and selective neurodegeneration as well as movement disorders, effectively recapitulating the typical pathological and clinic features in HD patients. Furthermore, the expanded CAG repeats and neurological phenotypes of these HD KI pigs can be transmitted to next generations by germline [20], providing a valuable model for investigating the pathogenesis and therapeutics for HD.
Large animal models of Parkinson's disease
Animal models developed to investigate the pathogenesis of PD fall into two categories: neurotoxic and genetic models. The neurotoxic models are mainly induced by the neurotoxins 6-hydroxydopamine (6-OHDA) (a hydroxylated analogue of dopamine) or 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), which cause dopamine neuronal loss in the substantia nigra (SN). The neurotoxic PD models are valuable for studying the pathogenesis of PD-associated neurodegeneration [42], but these models appear to have unstable phenotypes and cannot mimic the progressive process of neuronal loss and other pathologies in PD patients.
Although transgenic mouse and monkey models that overexpress mutant alpha-synuclein have been generated for investigating PD pathology and validated the neurotoxicity of mutant proteins [43,44,45,46], the various expression levels of exogenous mutant proteins could compromise the phenotype outcomes such that it is difficult to compare the merits of each transgenic PD animal model. Based on the fact that some genetic mutations also caused PD, a variety of mouse models that carry these genetic mutations in the endogenous genome were generated. However, none of them show the typical degeneration of dopaminergic neurons seen in the brains of PD patients [47,48,49,50]. For example, mutations of the PINK1 gene can result in loss of function and cause early-onset Parkinson’s disease (PD) with selective neurodegeneration [51]. Unfortunately, current PINK1 knockout (KO) mouse cannot yield the selective and overt neurodegeneration [48,49,50]. Similarly, deletion of the gene for Parkin, which works together with Pink1 in protecting against mitochondrial damage, did not produce any obvious degeneration either in the mouse brain [47, 50, 52].
Interestingly, disrupting the PINK1 and Parkin genes in pigs via CRISPR/Cas9 targeting did not produce any neurodegeneration and severe phenotypes either [35, 53]. However, CRISPR/Cas9 targeting the PINK1 gene in the monkeys resulted in phenotypic animals, though the phenotypes are dependent on the types of PINK1 mutations created. Chen et al. utilized the paired single guide RNA (sgRNA)/Cas9-D10A nickases to disrupt the monkey PINK1 in the fertilized monkey oocytes and found that targeting PINK1 exon 2 alone is not sufficient to model PD phenotypes in the live monkeys [54]. On the other hand, direct injection of AAV into the monkey substantia nigra to co-edit the PINK1 exon 3 and DJ1 genes could result in severe nigra dopaminergic cell loss and motor function deficits [55]. To ensure that PINK1 expression and function are completely lost, we used two gRNAs to disrupt the monkey PINK1 exon 2 and exon 4, resulting in a large PINK1 DNA fragment deletion in the monkey embryos. The newborn monkeys showed severe neurodegeneration or died postnatally [24], demonstrating for the first time that PINK1 is essential for neuronal survive in the primate brain. Further investigation identified that PINK1 functions as a cytoplasmic kinase, rather than a mitochondrial protein for mitophagy, to maintain the neuronal survival in the non-human primate [31]. Thus, investigation of the non-human primate model has uncovered important function of PINK1 and the associated pathological changes due to loss of PINK1, which cannot be identified in the mouse models.
Large animal models of ALS
Because mutations in the nuclear TAR DNA-binding protein 43 (TDP-43) gene cause ALS, animal models carrying TDP-43 mutations were generated to investigate ALS pathogenesis. TDP-43 is a nuclear protein that is involved in a variety of cellular functions including gene transcription, RNA processing, and protein homeostasis [56,57,58]. In patient brains with ALS, fronto-temporal lobar degeneration (FTLD), and other neurological disorders, TDP-43 is accumulated and forms aggregates in the cytoplasm [8, 58, 59]. This cytoplasmic redistribution of TDP-43 in human brains can lead to a loss of function in nucleus and a gain of toxicity in cytoplasm [60, 61]. However, in the brains of most transgenic mice, TDP-43 is still predominantly localized in the nucleus [60,61,62,63,64]. Although some mouse models can show the minimal level of cytoplasmic TDP-43 [63, 65, 66], this minimal distribution of cytoplasmic TDP-43 does not mimic the major pathological hallmark of cytoplasmic mislocalization of TDP-43.
Our group has previously created the TDP-43 transgenic pig model that displays the cytoplasmic distribution of TDP-43 [67]. We also used the non-human primate to investigate the subcellular distribution of mutant TDP-43 via directly delivering viral vector expressing mutant TDP-43 into the rhesus monkey brain cortex and substantia nigra [68]. For comparison, we injected the same viral vector into the mouse brain. Comparison of the subcellular localization of mutant TDP-43 in the brains of mice and rhesus monkeys revealed that the majority of mutant TDP-43 remained in the nuclei of the mouse brain but was mainly distributed in the cytoplasm of the monkey brain [68]. The cytoplasmic distribution of mutant TDP-43 in the monkey brain is consistent with the previous finding that transgenic TDP-43 is distributed in the neuronal cytoplasm in the monkey spinal cord [69]. Furthermore, the primate-specific caspase-4 was found to cleave TDP-43 in the monkey brain to mediate the cytoplasmic accumulation of TDP-43 by removing its NLS-containing N-terminal domain [68]. Thus, the findings in large animal models indicate that differential subcellular localization of mutant TDP-43 is species-dependent rather than brain region-dependent.
The human copper/zinc superoxide dismutase 1 (SOD1) mutations also cause familial ALS. However, transgenic mutant SOD1 mouse models do not show the intranuclear inclusions seen in the brains of ALS patient with SOD1 mutations [70,71,72]. To investigate the effect of mutant SOD1 in large animals, Yang et. al generated the SOD1 (G93A) transgenic pigs via the SCNT method [73]. The transgenic SOD1 pigs show motor function defects and neuronal degeneration. More importantly, mutant SOD1 was accumulated in the nucleus to form ubiquitinated nuclear aggregates at the early disease stage [73]. The differences between transgenic SOD1 mice and pigs further support the idea that large animal models can more faithfully mimic the pathological changes seen in the patient brains.
Large animal models of Alzheimer's disease
According to etiology, most AD patients are sporadic, and the familial type of AD only accounts for 5–10% of the total AD cases. The familial type of AD is mostly correlated with the genetic mutations in the genes for amyloid precursor protein (APP), Presenilin-1 (PSEN1), Presenilin-2 (PSEN2) [4]. Until now, the exact mechanism of AD remains elusive, largely due to the lack of animal models that can adequately mimic the AD pathology in humans. Various species of animal models for AD have been investigated, including fruit flies [74], rodents [75], dogs [76], pigs and non-human primates [77]. Among those species, the most widely used AD models are from rodents. However, the pharmaceutical treatments that were developed and effective in rodents have consistently failed to show obvious effects on humans in clinical trials. It is also noteworthy that rodents do not express the isoforms of Tau that leads to intracellular neurofibrillary tangles (NFTs), a hallmark of AD, such that multiple transgenes were required for co-expression to model AD pathologies in rodents [78,79,80]. The mini pigs expressing APP or PSEN1 engineered by nuclear transfer technology have failed to show any pathological changes at 2 and 3 years of age [81,82,83]. Because aging is one of the biggest risk factors for the development of AD, the lack of pathology and behavioral changes of AD pig models may be due to the early time points selected for analysis.
Because the non-human primates are much closer to humans, they should be the most biologically relevant model to study Alzheimer’s disease. Interestingly, no case of AD in naturally long-lived non-human primates has been reported [84]. The older NHPs could develop natural pathogenesis with senile plaques and Tau protein aggregations, mild cognitive deficits, but do not show overt and widespread neuronal loss as seen in AD patients [84, 85]. Microinjection of soluble and fibrous amyloid beta peptide (Aβ) has also been used to induce AD in non-human primate, revealing that the neurotoxicity of Aβ injection is dose-dependent and age-related because young monkeys did not develop visible changes of neuronal bodies or axons [86, 87].
Since ageing is a crucial pathogenic factor in these neurodegeneration diseases, the disease phenotypes might take longer time to appear in large animal models. Species-specific factors are also likely to influence the disease progression. These possibilities should be explored by establishing more large animal models, especially the non-human primate models, that carry the AD genes and are able to show the AD phenotypes.
New insight from large animal models
Animal models are an important tool for studying pathogenesis, disease progression, and therapeutic treatments. A successfully established animal model of neurodegenerative disease should adequately recapitulate the clinical characteristics and pathology of patients. However, such an animal model is still lacking for most neurodegenerative disease. Rodents are the most widely used animal model for generating disease models owing to their relatively short life span, easier and rapid breeding, and lower costs. However, rodents have only 48–66% genetic homology with humans and show considerable differences to humans in brain size and development [19, 91]. The current large animal models reviewed above have demonstrated important differences in neuropathology when compared with the rodent models. The striking neurodegeneration phenotypes seen in HD KI pigs and PINK1 mutant monkeys highlight the species-dependent influences on the development of neurodegeneration. Such influences could be due to species-specific expression of the disease genes or modifiers. Comparison of PINK1 KO models of mouse, pig and monkey also underscores the unique function of PINK1 in the primate brains because PINK1 is undetectable in the mouse brain but abundantly expressed in the primate brain at the protein level, which may explain why Pink1 knock out mouse models do not have overt neurodegeneration [31]. We also found that PINK1 is expressed as a kinase form that is vital to neuronal survival in the primate brains [24, 31]. Thus, genetic mutations such as a point mutation or a mutation in the non-kinase domain of PINK1 created in other monkey models may not be able to significantly affect PINK1 kinase function to elicit obvious neurodegeneration [54].
In addition to gene editing that can induce embryonic mutations in large animals by embryo microinjection, stereotaxic injection of viral expression vectors can be applied to modify genes in specific brain regions in adult animals at different ages to assess brain regional effects or age-dependent effects [31, 43, 55]. Such studies would be particularly useful for large animals to mimic distinct and age-dependent neuronal loss in neurodegenerative diseases. Also, editing genes in different cell types (such as neurons or glia) by using specific promoters to express CRISPR/Cas9 would allow us to investigate gene functions in different types of brain cells. The findings in large animal models are expected to offer new insights into pathogenesis and therapeutics of neurodegenerative diseases.
Limitations and challenges of using large animal models
The application of gene editing technology, especially the CRISPR/Cas9 system, makes revolutionary changes in modifying genomes in large animals for investigating neurodegenerative diseases. However, there are still many challenges to overcome. One potential challenge of CRISPR/Cas9 system is the mosaic mutations, which may result from various types of mutations created by the Cas9 nuclease. The mosaicism in offspring can be reduced by outcrossing the mosaic founders with wild type animals. However, it will take years to eliminate mosaicism in large animal models, especially for the non-human primates that require 4–5 years of sexual maturity to produce next generation. Thus, the mosaic targeting issue should be considered when evaluating the phenotypes of large animal models, because the funder animals that carry CRISPR/Cas9-mediated mosaic mutations are often used for investigation. The mosaic issue could potentially be improved by shortening the half-life of Cas9 expression after cell division such as tagging Cas9 with ubiquitin proteasomal degradation signals [92]. Other possible strategies using a combined strategy in early stage zygotes or germline cells to reduce mosaicism have also been discussed in a recent review [93]. For example, the gene editing tools combined with somatic cell nuclear transfer have been successfully used in establishing the pig models that carry the same single genetic mutation as in human patients. Liu et al. has created two cynomolgus monkeys by somatic cell nuclear transfer (SCNT) [94], offering great promise for generating more gene targeting non-human primate models in the future.
Although the mosaicism often exists in the non-human primate models, it depletes gene expression to various extents, leading to various degrees of cellular phenotypes that are correlated with the extent of genetic elimination. Thus, using imaging and RNAseq analysis at the single cell resolution, one can take the advantage of mosaicism to analyze the correlation of genetic mutation and cellular phenotypes in the large animal models.
Possible off-target effects of CRISPR/Cas9 have been considered as another important issue because CRISPR/Cas9 relies on approximately 23 base pair matches [95]. Studies have reported that Cas9 could tolerate mismatches that are associated with their distribution and number [96,97,98]. Thus, designing specific sgRNAs and controlling Cas9 expression should minimize the off-targets and increase the specificity of CRSIPR/Cas9-mediated gene targeting.
An obvious concern for generating large animal models is the high cost and time consumed for such research. For example, pigs have a sexual maturity of 5–8 months and the gestation period of about 114 d. For monkeys, the sexual maturity takes 4–5 years and gestation period is about 165 d with normally delivering only one offspring per year. Alternatively, the direct administration of gRNA/Cas9 into specific brain regions in adult large animals could more rapidly recapitulate brain regional neuropathology. The important information gained from large animal models would be highly valuable for generating more humanized mouse models. For example, once we know the primate-specific factors that critically contribute to neurodegeneration, we can introduce these factors to the rodents to make rodent models to be able to display important pathological features. Such mouse models can be used to rigorously test the effects of therapeutic strategies on neurodegeneration.
Conclusions
The newly developed genome editing tool has greatly advanced the progress of generating valuable large animal models for neurodegenerative disease research. These large animal models allowed one to discover important pathological events that otherwise do not occur in small animals. However, the generation and investigation of genetically modified large animal models are still challenging, largely due to the high cost of animals and time consumed experiments. We anticipate that further optimization of the existing genome editing system or the generation of new tools will improve the efficiency and accuracy of genome modification of large animals. Moreover, important insights from large animal models would help establish small animal models that can more faithfully recapitulate important pathological features for investigating pathogenesis and developing effective therapies.
Availability of data and materials
Not applicable.
References:
Dugger BN, Dickson DW. Pathology of Neurodegenerative Diseases. Cold Spring Harb Perspect Biol. 2017. https://doi.org/10.1101/cshperspect.a028035.
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13:614–29.
Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med. 2011;1:a006189.
Lanoiselée H-M, Nicolas G, Wallon D, Rovelet-Lecrux A, Lacour M, Rousseau S, et al. APP, PSEN1, and PSEN2 mutations in early-onset Alzheimer disease: a genetic screening study of familial and sporadic cases. PLoS Med. 2017;14:e1002270.
Damier P, Hirsch EC, Agid Y, Graybiel AM. The substantia nigra of the human brain. II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain. 1999;122(Pt 8):1437–48.
Deng H, Wang P, Jankovic J. The genetics of Parkinson disease. Ageing Res Rev. 2018;42:72–85.
Grad LI, Rouleau GA, Ravits J, Cashman NR. Clinical spectrum of amyotrophic lateral sclerosis (ALS). Cold Spring Harb Perspect Med. 2017. https://doi.org/10.1101/cshperspect.a024117.
Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–3.
Turner MR, Hardiman O, Benatar M, Brooks BR, Chio A, de Carvalho M, et al. Controversies and priorities in amyotrophic lateral sclerosis. Lancet Neurol. 2013;12:310–22.
Yang H, Yang S, Jing L, Huang L, Chen L, Zhao X, et al. Truncation of mutant huntingtin in knock-in mice demonstrates exon1 huntingtin is a key pathogenic form. Nat Commun. 2020;11:2582.
Bates GP, Dorsey R, Gusella JF, Hayden MR, Kay C, Leavitt BR, et al. Huntington disease. Nat Rev Dis Prim. 2015;1:15005.
Soto C, Pritzkow S. Protein misfolding, aggregation, and conformational strains in neurodegenerative diseases. Nat Neurosci. 2018;21:1332–40.
Dugger BN, Perl DP, Carlson GA. Neurodegenerative disease transmission and transgenesis in mice. Cold Spring Harb Perspect Biol. 2017. https://doi.org/10.1101/cshperspect.a023549.
Zoghbi HY, Botas J. Mouse and fly models of neurodegeneration. Trends Genet. 2002;18:463–71.
Crook ZR, Housman D. Huntington’s disease: can mice lead the way to treatment? Neuron. 2011;69:423–35.
Levine MS, Cepeda C, Hickey MA, Fleming SM, Chesselet M-F. Genetic mouse models of Huntington’s and Parkinson’s diseases: illuminating but imperfect. Trends Neurosci. 2004;27:691–7.
Ashe KH, Zahs KR. Probing the biology of Alzheimer’s disease in mice. Neuron. 2010;66:631–45.
Dawson TM, Ko HS, Dawson VL. Genetic animal models of Parkinson’s disease. Neuron. 2010;66:646–61.
Otani T, Marchetto MC, Gage FH, Simons BD, Livesey FJ. 2D and 3D stem cell models of primate cortical development identify species-specific differences in progenitor behavior contributing to brain size. Cell Stem Cell. 2016;18:467–80.
Yan S, Tu Z, Liu Z, Fan N, Yang H, Yang S, et al. A huntingtin knockin pig model recapitulates features of selective neurodegeneration in huntington’s disease. Cell. 2018;173:989-1002.e13.
Niu Y, Shen B, Cui Y, Chen Y, Wang J, Wang L, et al. Generation of gene-modified cynomolgus monkey via Cas9/RNA-mediated gene targeting in one-cell embryos. Cell. 2014;156:836–43.
Chen Y, Cui Y, Shen B, Niu Y, Zhao X, Wang L, et al. Germline acquisition of Cas9/RNA-mediated gene modifications in monkeys. Cell Res. 2015. https://doi.org/10.1038/cr.2014.167.
Zhang W, Wan H, Feng G, Qu J, Wang J, Jing Y, et al. SIRT6 deficiency results in developmental retardation in cynomolgus monkeys. Nature. 2018;560:661–5.
Yang W, Liu Y, Tu Z, Xiao C, Yan S, Ma X, et al. CRISPR/Cas9-mediated PINK1 deletion leads to neurodegeneration in rhesus monkeys. Cell Res. 2019;2(4):334–6.
Gaudelli NM, Komor AC, Rees HA, Packer MS, Badran AH, Bryson DI, et al. Programmable base editing of A•T to G•C in genomic DNA without DNA cleavage. Nature. 2017;551:464–71.
Komor AC, Zhao KT, Packer MS, Gaudelli NM, Waterbury AL, Koblan LW, et al. Improved base excision repair inhibition and bacteriophage Mu Gam protein yields C:G-to-T: a base editors with higher efficiency and product purity. Sci Adv. 2017. https://doi.org/10.1126/sciadv.aao4774.
Xie J, Ge W, Li N, Liu Q, Chen F, Yang X, et al. Efficient base editing for multiple genes and loci in pigs using base editors. Nat Commun. 2019;10:2852.
Wang F, Zhang W, Yang Q, Kang Y, Fan Y, Wei J, et al. Generation of a Hutchinson-Gilford progeria syndrome monkey model by base editing. Protein Cell. 2020;11:809–24.
Incontro S, Asensio CS, Edwards RH, Nicoll RA. Efficient, complete deletion of synaptic proteins using CRISPR. Neuron. 2014;83:1051–7.
Swiech L, Heidenreich M, Banerjee A, Habib N, Li Y, Trombetta J, et al. In vivo interrogation of gene function in the mammalian brain using CRISPR-Cas9. Nat Biotechnol. 2015;33:102–6.
Yang W, Guo X, Tu Z, Chen X, Han R, Liu Y, et al. PINK1 kinase dysfunction triggers neurodegeneration in the primate brain without impacting mitochondrial homeostasis. Protein Cell. 2021. https://doi.org/10.1007/s13238-021-00888-x.
Zhao J, Lai L, Ji W, Zhou Q. Genome editing in large animals: current status and future prospects. Natl Sci Rev. 2019;6:402–20.
Hauschild J, Petersen B, Santiago Y, Queisser A-L, Carnwath JW, Lucas-Hahn A, et al. Efficient generation of a biallelic knockout in pigs using zinc-finger nucleases. Proc Natl Acad Sci U S A. 2011;108:12013–7.
Ryu J, Prather RS, Lee K. Use of gene-editing technology to introduce targeted modifications in pigs. J Anim Sci Biotechnol. 2018;9:5.
Zhou X, Xin J, Fan N, Zou Q, Huang J, Ouyang Z, et al. Generation of CRISPR/Cas9-mediated gene-targeted pigs via somatic cell nuclear transfer. Cell Mol Life Sci. 2015;72:1175–84.
Yang S-H, Cheng P-H, Banta H, Piotrowska-Nitsche K, Yang J-J, Cheng ECH, et al. Towards a transgenic model of Huntington’s disease in a non-human primate. Nature. 2008;453:921–4.
Davies SW, Turmaine M, Cozens BA, DiFiglia M, Sharp AH, Ross CA, et al. Formation of neuronal intranuclear inclusions underlies the neurological dysfunction in mice transgenic for the HD mutation. Cell. 1997;90:537–48.
Yang D, Wang C-E, Zhao B, Li W, Ouyang Z, Liu Z, et al. Expression of Huntington’s disease protein results in apoptotic neurons in the brains of cloned transgenic pigs. Hum Mol Genet England. 2010;19:3983–94.
Baxa M, Hruska-Plochan M, Juhas S, Vodicka P, Pavlok A, Juhasova J, et al. A transgenic minipig model of Huntington’s Disease. J Huntingtons Dis. 2013;2:47–68.
Schuldenzucker V, Schubert R, Muratori LM, Freisfeld F, Rieke L, Matheis T, et al. Behavioral testing of minipigs transgenic for the Huntington gene-A three-year observational study. PLoS ONE. 2017;12:e0185970.
Jacobsen JC, Bawden CS, Rudiger SR, McLaughlan CJ, Reid SJ, Waldvogel HJ, et al. An ovine transgenic Huntington’s disease model. Hum Mol Genet. 2010;19:1873–82.
Tieu K. A guide to neurotoxic animal models of Parkinson’s disease. Cold Spring Harb Perspect Med. 2011;1:a009316.
Yang W, Wang G, Wang C-E, Guo X, Yin P, Gao J, et al. Mutant alpha-synuclein causes age-dependent neuropathology in monkey brain. J Neurosci United States. 2015;35:8345–58.
Giasson BI, Duda JE, Quinn SM, Zhang B, Trojanowski JQ, Lee VM-Y. Neuronal alpha-synucleinopathy with severe movement disorder in mice expressing A53T human alpha-synuclein. Neuron. 2002;34:521–33.
Ip CW, Klaus L-C, Karikari AA, Visanji NP, Brotchie JM, Lang AE, et al. AAV1/2-induced overexpression of A53T-α-synuclein in the substantia nigra results in degeneration of the nigrostriatal system with Lewy-like pathology and motor impairment: a new mouse model for Parkinson’s disease. Acta Neuropathol Commun. 2017;5:11.
Lee MK, Stirling W, Xu Y, Xu X, Qui D, Mandir AS, et al. Human alpha-synuclein-harboring familial Parkinson’s disease-linked Ala-53 –> Thr mutation causes neurodegenerative disease with alpha-synuclein aggregation in transgenic mice. Proc Natl Acad Sci U S A. 2002;99:8968–73.
Perez FA, Palmiter RD. Parkin-deficient mice are not a robust model of parkinsonism. Proc Natl Acad Sci U S A. 2005;102:2174–9.
Kitada T, Pisani A, Porter DR, Yamaguchi H, Tscherter A, Martella G, et al. Impaired dopamine release and synaptic plasticity in the striatum of PINK1-deficient mice. Proc Natl Acad Sci U S A. 2007;104:11441–6.
Zhou H, Falkenburger BH, Schulz JB, Tieu K, Xu Z, Xia XG. Silencing of the Pink1 gene expression by conditional RNAi does not induce dopaminergic neuron death in mice. Int J Biol Sci. 2007;3:242–50.
Kitada T, Tong Y, Gautier CA, Shen J. Absence of nigral degeneration in aged parkin/DJ-1/PINK1 triple knockout mice. J Neurochem. 2009;111:696–702.
Valente EM, Salvi S, Ialongo T, Marongiu R, Elia AE, Caputo V, et al. PINK1 mutations are associated with sporadic early-onset parkinsonism. Ann Neurol. 2004;56:336–41.
Goldberg MS, Fleming SM, Palacino JJ, Cepeda C, Lam HA, Bhatnagar A, et al. Parkin-deficient mice exhibit nigrostriatal deficits but not loss of dopaminergic neurons. J Biol Chem. 2003;278:43628–35.
Wang X, Cao C, Huang J, Yao J, Hai T, Zheng Q, et al. One-step generation of triple gene-targeted pigs using CRISPR/Cas9 system. Sci Rep. 2016;6:20620.
Chen Z-Z, Wang J-Y, Kang Y, Yang Q-Y, Gu X-Y, Zhi D-L, et al. PINK1 gene mutation by pair truncated sgRNA/Cas9-D10A in cynomolgus monkeys. Zool Res. 2021;42:469–77.
Li H, Wu S, Ma X, Li X, Cheng T, Chen Z, et al. Co-editing PINK1 and DJ-1 genes via adeno-associated virus-delivered CRISPR/Cas9 system in adult monkey brain elicits classical parkinsonian phenotype. Neurosci Bull. 2021;37:1271–88.
Lagier-Tourenne C, Cleveland DW. Rethinking ALS: the FUS about TDP-43. Cell. 2009;136:1001–4.
Polymenidou M, Lagier-Tourenne C, Hutt KR, Huelga SC, Moran J, Liang TY, et al. Long pre-mRNA depletion and RNA missplicing contribute to neuronal vulnerability from loss of TDP-43. Nat Neurosci. 2011;14:459–68.
Weishaupt JH, Hyman T, Dikic I. Common molecular pathways in amyotrophic lateral sclerosis and frontotemporal dementia. Trends Mol Med. 2016;22:769–83.
Chen-Plotkin AS, Lee VM-Y, Trojanowski JQ. TAR DNA-binding protein 43 in neurodegenerative disease. Nat Rev Neurol. 2010;6:211–20.
Huang C, Tong J, Bi F, Zhou H, Xia X-G. Mutant TDP-43 in motor neurons promotes the onset and progression of ALS in rats. J Clin Invest. 2012;122:107–18.
Philips T, Rothstein JD. Rodent models of amyotrophic lateral sclerosis. Curr Protoc Pharmacol. 2015. https://doi.org/10.1002/0471141755.ph0567s69.
Shan X, Chiang P-M, Price DL, Wong PC. Altered distributions of Gemini of coiled bodies and mitochondria in motor neurons of TDP-43 transgenic mice. Proc Natl Acad Sci U S A. 2010;107:16325–30.
Wegorzewska I, Bell S, Cairns NJ, Miller TM, Baloh RH. TDP-43 mutant transgenic mice develop features of ALS and frontotemporal lobar degeneration. Proc Natl Acad Sci U S A. 2009;106:18809–14.
Yan S, Wang C-E, Wei W, Gaertig MA, Lai L, Li S, et al. TDP-43 causes differential pathology in neuronal versus glial cells in the mouse brain. Hum Mol Genet. 2014;23:2678–93.
Mitchell JC, Constable R, So E, Vance C, Scotter E, Glover L, et al. Wild type human TDP-43 potentiates ALS-linked mutant TDP-43 driven progressive motor and cortical neuron degeneration with pathological features of ALS. Acta Neuropathol Commun. 2015;3:36.
Wils H, Kleinberger G, Janssens J, Pereson S, Joris G, Cuijt I, et al. TDP-43 transgenic mice develop spastic paralysis and neuronal inclusions characteristic of ALS and frontotemporal lobar degeneration. Proc Natl Acad Sci U S A. 2010;107:3858–63.
Wang G, Yang H, Yan S, Wang C-E, Liu X, Zhao B, et al. Cytoplasmic mislocalization of RNA splicing factors and aberrant neuronal gene splicing in TDP-43 transgenic pig brain. Mol Neurodegener. 2015;10:42.
Yin P, Guo X, Yang W, Yan S, Yang S, Zhao T, et al. Caspase-4 mediates cytoplasmic accumulation of TDP-43 in the primate brains. Acta Neuropathol. 2019. https://doi.org/10.1007/s00401-019-01979-0.
Uchida A, Sasaguri H, Kimura N, Tajiri M, Ohkubo T, Ono F, et al. Non-human primate model of amyotrophic lateral sclerosis with cytoplasmic mislocalization of TDP-43. Brain. 2012;135:833–46.
Kakita A, Oyanagi K, Nagai H, Takahashi H. Eosinophilic intranuclear inclusions in the hippocampal pyramidal neurons of a patient with amyotrophic lateral sclerosis. Acta Neuropathol. 1997;93:532–6.
Seilhean D, Takahashi J, El Hachimi KH, Fujigasaki H, Lebre A-S, Biancalana V, et al. Amyotrophic lateral sclerosis with neuronal intranuclear protein inclusions. Acta Neuropathol. 2004;108:81–7.
Forsberg K, Andersen PM, Marklund SL, Brännström T. Glial nuclear aggregates of superoxide dismutase-1 are regularly present in patients with amyotrophic lateral sclerosis. Acta Neuropathol. 2011;121:623–34.
Yang H, Wang G, Sun H, Shu R, Liu T, Wang C-E, et al. Species-dependent neuropathology in transgenic SOD1 pigs. Cell Res. 2014;24:464–81.
Bouleau S, Tricoire H. Drosophila models of Alzheimer’s disease: advances, limits, and perspectives. J Alzheimers Dis. 2015;45:1015–38.
Götz J, Bodea L-G, Goedert M. Rodent models for Alzheimer disease. Nat Rev Neurosci. 2018;19:583–98.
Head E. A canine model of human aging and Alzheimer’s disease. Biochim Biophys Acta. 2013;1832:1384–9.
Yang M, Miao J, Rizak J, Zhai R, Wang Z, Huma T, et al. Alzheimer’s disease and methanol toxicity (part 2): lessons from four rhesus macaques (Macaca mulatta) chronically fed methanol. J Alzheimers Dis. 2014;41:1131–47.
Oddo S, Caccamo A, Shepherd JD, Murphy MP, Golde TE, Kayed R, et al. Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Abeta and synaptic dysfunction. Neuron. 2003;39:409–21.
Kent SA, Spires-Jones TL, Durrant CS. The physiological roles of tau and Aβ: implications for Alzheimer’s disease pathology and therapeutics. Acta Neuropathol. 2020;140:417–47.
Jankowsky JL, Zheng H. Practical considerations for choosing a mouse model of Alzheimer’s disease. Mol Neurodegener. 2017;12:89.
Kragh PM, Nielsen AL, Li J, Du Y, Lin L, Schmidt M, et al. Hemizygous minipigs produced by random gene insertion and handmade cloning express the Alzheimer’s disease-causing dominant mutation APPsw. Transgenic Res. 2009;18:545–58.
Søndergaard LV, Ladewig J, Dagnæs-Hansen F, Herskin MS, Holm IE. Object recognition as a measure of memory in 1–2 years old transgenic minipigs carrying the APPsw mutation for Alzheimer’s disease. Transgenic Res. 2012;21:1341–8.
Jakobsen JE, Johansen MG, Schmidt M, Dagnæs-Hansen F, Dam K, Gunnarsson A, et al. Generation of minipigs with targeted transgene insertion by recombinase-mediated cassette exchange (RMCE) and somatic cell nuclear transfer (SCNT). Transgenic Res. 2013;22:709–23.
Toledano A, Alvarez MI, López-Rodríguez AB, Toledano-Díaz A, Fernández-Verdecia CI. Does Alzheimer’s disease exist in all primates? Alzheimer pathology in non-human primates and its pathophysiological implications (I). Neurologia. 2012;27:354–69.
Heuer E, Rosen RF, Cintron A, Walker LC. Nonhuman primate models of Alzheimer-like cerebral proteopathy. Curr Pharm Des. 2012;18:1159–69.
Geula C, Wu CK, Saroff D, Lorenzo A, Yuan M, Yankner BA. Aging renders the brain vulnerable to amyloid beta-protein neurotoxicity. Nat Med. 1998;4:827–31.
McKee AC, Kowall NW, Schumacher JS, Beal MF. The neurotoxicity of amyloid beta protein in aged primates. Amyloid Int J Exp Clin Investig Off J Int Soc Amyloidosis. 1998;5:1–9.
Niu Y, Guo X, Chen Y, Wang C-E, Gao J, Yang W, et al. Early Parkinson’s disease symptoms in alpha-synuclein transgenic monkeys. Hum Mol Genet. 2015;24:2308–17.
Seita Y, Morimura T, Watanabe N, Iwatani C, Tsuchiya H, Nakamura S, et al. Generation of transgenic cynomolgus monkeys overexpressing the gene for amyloid-β precursor protein. J Alzheimers Dis. 2020;75:45–60.
Chieppa MN, Perota A, Corona C, Grindatto A, Lagutina I, Vallino Costassa E, et al. Modeling amyotrophic lateral sclerosis in hSOD1 transgenic swine. Neurodegener Dis. 2014;13:246–54.
Eaton SL, Wishart TM. Bridging the gap: large animal models in neurodegenerative research. Mamm Genome. 2017;28:324–37.
Tu Z, Yang W, Yan S, Yin A, Gao J, Liu X, et al. Promoting Cas9 degradation reduces mosaic mutations in non-human primate embryos. Sci Rep. 2017;7:42081.
Mehravar M, Shirazi A, Nazari M, Banan M. Mosaicism in CRISPR/Cas9-mediated genome editing. Dev Biol. 2019;445:156–62.
Liu Z, Cai Y, Wang Y, Nie Y, Zhang C, Xu Y, et al. Cloning of macaque monkeys by somatic cell nuclear transfer. Cell. 2018;174:245.
Hsu PD, Lander ES, Zhang F. Development and applications of CRISPR-Cas9 for genome engineering. Cell. 2014;157:1262–78.
Hsu PD, Scott DA, Weinstein JA, Ran FA, Konermann S, Agarwala V, et al. DNA targeting specificity of RNA-guided Cas9 nucleases. Nat Biotechnol. 2013;31:827–32.
Mali P, Aach J, Stranges PB, Esvelt KM, Moosburner M, Kosuri S, et al. CAS9 transcriptional activators for target specificity screening and paired nickases for cooperative genome engineering. Nat Biotechnol. 2013;31:833–8.
Fu Y, Sander JD, Reyon D, Cascio VM, Joung JK. Improving CRISPR-Cas nuclease specificity using truncated guide RNAs. Nat Biotechnol. 2014;32:279–84.
Acknowledgements
Not applicable.
Funding
This work was supported by Key Field Research and Development Program of Guangdong province (2018B030337001), The National Natural Science Foundation of China (32070534, 81830032, 31872779, 82071421); Department of Science and Technology of Guangdong Province (2021ZT09Y007; 2020B121201006), Guangzhou Key Research Program on Brain Science (202007030008), The National Key Research and Development Program of China Stem Cell and Translational Research (2017YFA0105102).
Author information
Authors and Affiliations
Contributions
WY and X-JL wrote the manuscript. XC and SL edited the manuscript. All discussed and approved the overall structure of the review. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors give their consent for the publication of this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, W., Chen, X., Li, S. et al. Genetically modified large animal models for investigating neurodegenerative diseases. Cell Biosci 11, 218 (2021). https://doi.org/10.1186/s13578-021-00729-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13578-021-00729-8