Abstract
Background
We report on the activity of anthracycline-based and high-dose prolonged-infusion ifosfamide chemotherapy in a retrospective series of patients affected by advanced myxofibrosarcoma treated at Istituto Nazionale Tumori in Milan, Italy, and within the Italian Rare Cancer Network (RTR).
Methods
Advanced myxofibrosarcoma patients treated with anthracycline + ifosfamide and high-dose prolonged-infusion ifosfamide as a single agent from November 2001 to December 2016 were retrospectively reviewed. All pathological diagnosis were centrally reviewed by at least two expert pathologists. Response was evaluated by RECIST, and survival functions were computed.
Results
Among 34 advanced myxofibrosarcoma patients, 13 were treated with front-line anthracycline + ifosfamide chemotherapy (male/female = 6/7, median age 54 years, range 33–72). Overall best response was: 4 partial responses, 3 stable diseases and 6 progressive diseases, with a median progression-free survival of 4 months. Twenty-eight patients received second/further line high-dose prolonged-infusion ifosfamide (male/female = 17/11, median age 55 years, range 27–75 years). We observed 10 partial responses, 4 stable diseases and 14 progressive diseases, with a median progression-free survival of 4 months. Median overall survival was 12 months.
Conclusions
This retrospective analysis suggests that the combination of anthracyclines and ifosfamide is active in myxofibrosarcoma. In patients already treated with a combination of anthracyclines and ifosfamide, high-dose prolonged-infusion ifosfamide showed activity as well.
Similar content being viewed by others
Background
Myxofibrosarcoma is a rare soft tissue sarcoma (STS) with an estimated incidence <0.1/100.000/years [1]. Historically, it was first described in 1977 as a part of the spectrum of myxoid fibroblastic malignancies [2, 3]. It was finally included in the WHO classification in 2002 as a distinct entity with unique clinicopathological characteristics and cytoarchitectural features [4].
Myxofibrosarcoma is more common in elderly patients and it is mainly located to the extremities, especially lower limbs, but it can arise in the trunk and in head and neck region [5,6,7]. Since a presentation in the abdominal cavity or in the retroperitoneum is extremely rare, a differential diagnosis between dedifferentiated liposarcoma and myxofibrosarcoma should be always considered [8,9,10]. In comparison to the other soft tissue sarcoma types, myxofibrosarcoma exhibits an overall better prognosis [10,11,12,13], with an overall survival (OS) of approximatively 70% and an overall risk of metastases between 20 and 25% in high-grade variants [10,11,12,13,14,15,16,17,18,19]. However, myxofibrosarcoma tends to have a remarkable rate of local recurrences compared to other soft tissue sarcomas, reported between 20 and 75% [2, 5, 6, 10, 12, 16].
Surgery alone or in combination with radiotherapy is the main treatment for localized disease [10, 12], and medical treatment is used in the advance disease. The combination of anthracyclines and ifosfamide as front-line therapy of advanced soft tissue sarcomas is associated with response rates of 20–30% in previously untreated patients. This percentage drops to 10% in second line. However, this reflects the whole group of soft tissue sarcomas, which make up a heterogeneous disease with discrepant chemosensitivity across the histological subtypes. For example, angiosarcoma or myxoid liposarcoma have been observed to be responsive to chemotherapy, while other subgroups are poorly responsive [20]. In the subgroup of myxofibrosarcomas, the precise role of chemotherapy remains undefined and no prospective trials or retrospective analyses are available [21].
Therefore, we carried out this retrospective study on a series of patients affected by advanced myxofibrosarcoma treated with chemotherapy at the Istituto Nazionale Tumori, Milano, Italy, and within the Italian Rare Cancer Network, a collaborative network sharing clinical cases and data of rare cancers in Italy.
Methods
Thirty-four patients affected by advanced myxofibrosarcoma, consecutively treated with chemotherapy between November 2001 and December 2016 at Fondazione IRCCS Istituto Nazionale Tumori, Milan, Italy, and within the Italian Rare Cancer Network, were retrospectively identified. We retrieved a subgroup of 13 patients treated with front-line anthracycline + ifosfamide chemotherapy and a subgroup of 28 patients treated with second/further line high-dose prolonged-infusion ifosfamide.
Pathological diagnosis was centrally reviewed by at least two expert pathologists in all the cases, following the most recent updated criteria [4].
Data regarding clinical and histopathological characteristics, staging, surgical and systemic treatment and survival were collected. The clinical records were reviewed and collected in one institutional database and a descriptive analysis was performed. Data on chemotherapy tolerability and adverse effects were recorded. Response to chemotherapy was evaluated with Response Evaluation Criteria in Solid Tumours (RECIST) applied to CT and/or MRI scans performed periodically (usually every 2–3 months) [22].
This retrospective analysis was approved by the Institutional Ethics Committee of our Institution.
Treatment
When an anthracycline was used in combination with ifosfamide, the regimen was epirubicin 105 mg/sqm + ifosfamide 9000 mg/sqm, i.v., in 3 days every 3 weeks, in association with equidose MESNA, and antiemetics. Prophylactic granulocyte colony stimulating factors were given. High-dose ifosfamide (HDIFX) was administered as a single agent, at the daily dose of 1 g/sqm (total dose of 14 g/sqm per cycle), as a 14-day continuous infusion with equidose MESNA, through two portable infusional devices lasting 7 days each. HDIFX regimen was administered every 4 weeks (2 weeks of infusion followed by 2 weeks off).
Statistical analysis
Progression-free Survival (PFS) and Overall Survival (OS) were estimated with Kaplan–Meier method [23]. Failure for PFS were death or progressive disease according to RECIST. Failure for OS was death due to any cause. Patients alive were censored at the time of the last contact.
Results
Anthracycline + ifosfamide chemotherapy
Thirteen patients affected by advanced myxofibrosarcoma were treated with front-line anthracycline + ifosfamide chemotherapy. Patient characteristics are shown in Table 1. Female patients were prevalent (female/male 7/6); median age at the time of the operation was 54 years (range 33–72 years).
All patients treated were assessable for response. Median number of chemotherapy cycles was 3 (range 2–6). The best response according to RECIST was: partial response (PR) in 4/13 cases (31%, 95% CI 0.09–0.61), stable disease (SD) in 3/13 (23%, 95% CI 0.05-0.53), progressive disease (PD) in 6/13 (46%, 95% CI 0.19–0.74) cases. Responses were confirmed at 3 months. Median PFS was 4 months, with 30% of patients progression-free at 6 months (Fig. 1a). Median OS was 12 months, with 12 patients dead and one patient alive at the time of this analysis (Fig. 1b).
Two patients interrupted their treatment for febrile neutropenia after 3 cycles of chemotherapy. No toxic deaths or any unexpected major toxicities were reported.
High-dose ifosfamide chemotherapy
Twenty-eight patients received second/further HDIFX. Fourteen patients received epirubicin and ifosfamide in the adjuvant setting, 9/28 patients were pretreated with first line epirubicin and ifosfamide chemotherapy combination and 5/28 were pretreated with other regimens (2/5 epirubicin alone, 1/5 dacarbazine, 1/5 docetaxel, 1/5 gemcitabine). Patient characteristics are detailed in Table 2. Male patients were prevalent (male/female 17/11); median age at the time of the treatment was 55 years (range 27–75 years). Median number of HDIFX cycles was 3 (range 2–8).
All patients treated with HDIFX were evaluable for response. The best response was: PR in 10/28 (36%, 95% CI 0.18–0.55), SD in 4/28 (14%, 95% CI 0.04–0.32) and PD in 14/28 (50%, 95% CI 0.30–0.69). Among patients pretreated with first line epirubicin–ifosfamide, we observed 4/9 PD (44%), 3/9 PR (33%), 2/9 SD (23%); all patients responding to second line HDIFX had had a PR to first-line epirubicin–ifosfamide. Median PFS was 4 months (Fig. 2a). Median OS was 12 months (Fig. 2b), with 27 patients dead and one patient alive at the time of this analysis.
No febrile neutropenia and renal failure were observed, as well as no toxic deaths or any other unexpected major toxicities.
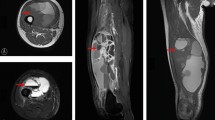
Figure 3 shows a pathological partial response to HDIFX.
On haematoxylin and eosin staining, a pathologic partial response in a patient treated with six cycles of high-dose ifosfamide. a A thoracic wall metastasis from a myxofibrosarcoma arising from the thoracic wall at baseline. b In high power and c the pathologic partial response after 6 months of treatment with high-dose ifosfamide with areas of necrosis included both vascular and avascular pattern and vital areas
Discussion
In a retrospective study on a series of 34 consecutive patients with progressing advanced myxofibrosarcoma treated with chemotherapy on a 15-year span, we observed a 30% PR rate, with a median PFS of 4 months with two chemotherapy regimens commonly used in other soft tissue sarcomas. In our series, the patients were relatively young, and the retrospectivity of the analysis makes it hard to transpose data on toxicity of these two regimens to the general population.
The benefit of multi-agent compared to single agent anthracycline-based first line chemotherapy for advanced soft tissue sarcomas remains controversial. In the biggest randomized prospective trial, the combination of doxorubicin and ifosfamide was associated with higher response rates, but a non-significant overall survival benefit [24]. However, upfront combination chemotherapy may be of benefit, even considering the increased toxicity, for selected patients, e.g. those with a high tumor burden requiring a prompt tumor shrinkage or those with a fast-growing disease, in need of obtaining a response. In terms of responses to anthracycline and ifosfamide, our results point to an antitumor activity similar to advanced soft tissue sarcomas in general [24]. However, PFS was markedly low in our series. The limited number of patients makes it difficult to speculate on this.
HDIFX is often used as a salvage regimen in synovial sarcoma and dedifferentiated liposarcoma, even in patients previously treated with standard-dose ifosfamide [25,26,27,28,29]. Furthermore, if compared with the classic ifosfamide schedule, the administration in the external portable device in a prolonged 14-days continuous infusion shows an excellent tolerability. Main toxicities are represented by mild to moderate nausea and vomiting, while myelosuppression, neurotoxicity and acute kidney failure are infrequent.
In our series, the anti-tumor activity of HDIFX as second/further chemotherapy line in myxofibrosarcoma was apparently higher than in other soft tissue sarcomas [26,27,28,30].
Among 28 patients treated with HDIFX in second/further line, the PR rate was 36% and median PFS was 4 months. We reported a similar PR rate for continuous-infusion HDIFX in well differentiated/dedifferentiated liposarcomas [25]. Nine patients were pretreated with first-line epirubicin–ifosfamide and we observed 4 PR (31% RECIST PR) out of 13 patients evaluable for response. Thus, high-dose ifosfamide was still active in patients pre-treated with anthracyclines and standard-dose ifosfamide. Again, however, median PFS was low. The previous exposure to ifosfamide may, in part, explain these results.
In advanced soft tissue sarcomas, standard chemotherapy is based on anthracyclines as the first-line treatment and the sequencing of second-line, third-line and fourth-line treatments remains open to debate [13, 31, 32]. Histological diagnosis can help guide the sequence of treatments [32]. Indeed, a histology-driven choice is feasible in some histologies (e.g., paclitaxel for angiosarcoma, gemcitabine for leiomyosarcoma, trabectedin for myxoid liposarcoma, etc.). In this perspective, the reasonably interesting PR rate seen with continuous-infusion HDIFX may be of interest.
Conclusions
This was a retrospective analysis in a relatively young small population of patients over a 15-year span. However, among soft tissue sarcomas, myxofibrosarcoma represents a rare subtype. No data are reported so far on the activity of chemotherapy and no prospective neither retrospective studies focusing on its medical treatment are available. Obviously, it is difficult to conceive prospective studies in such a rare subtype. In this sense, this report adds some information which may assist the clinicians in the choice of regimens. However, the low PFS implies that we are in need for new therapies for such a histology, when a medical treatment is required.
References
Stiller CA, Trama A, Serraino D, Rossi S, Navarro C, Chirlaque MD, for the RARECARE Working Group, et al. Descriptive epidemiology of sarcomas in Europe: report from RARECARE project. Eur J Cancer. 2013;49:684–95.
Weiss SW, Enzinger FM. Myxoid variant of malignant fibrous histiocytoma. Cancer. 1977;39:1672–85.
Angervall L, Kindblom LG, Merck C. Myxofibrosarcoma. A study of 30 cases. Acta Pathol Microbiol Scand. 1977;85A:127–40.
Fletcher CDM, Bridge JA, Pancras CW, Mertens F, editors. World Health Organization (WHO) classification of tumours of soft tissue and bone. Pathology and Genetics. Lyon: IARC Press; 2013.
Merck C, Angervall L, Kindblom LG, Odén A. Myxofibrosarcoma. A malignant soft tissue tumor of fibroblastichistiocytic origin. A clinicopathologic and prognostic study of 110 cases using multivariate analysis. Acta Pathol Microbiol Immunol Scand Suppl. 1983;282:1–40.
Mentzel T, Calonje E, Wadden C, Camplejohn RS, Beham A, Smith MA, et al. Myxofibrosarcoma. Clinicopathologic analysis of 75 cases with emphasis on the low grade variant. Am J Surg Pathol. 1996;20:391–405.
Willems SM, Debiec-Rychter M, Szuhai K, Hogendoorn PC, Sciot R. Local recurrence of myxofibrosarcoma is associated with increase in tumour grade and cytogenetic aberrations, suggesting a multistep tumour progression model. Mod Pathol. 2006;19:407–16.
Hisaoka M, Morimitsu Y, Hashimoto H, Ishida T, Mukai H, Satoh H, et al. Retroperitoneal liposarcoma with combined well-differentiated and myxoid malignant fibrous histiocytoma-like myxoid areas. Am J Surg Pathol. 1999;23:1480–92.
Meis-Kindblom JM, Sjögren H, Kindblom LG, Peydró-Mellquist A, Röijer E, Aman P, et al. Cytogenetic and molecular genetic analyses of liposarcoma and its soft tissue simulators: recognition of new variants and differential diagnosis. Virchows Arch. 2001;439:141–51.
Sanfilippo R, Miceli R, Grosso F, Fiore M, Puma E, Pennacchioli E, et al. Myxofibrosarcoma: prognostic factors and survival in a series of patients treated at a single institution. Ann Surg Oncol. 2011;18(3):720–5.
Fletcher CDM, Gustafson P, Rydholm A, Willén H, Akerman M. Clinicopathologic re-evaluation of 100 malignant fibrous histiocytomas: prognostic relevance of subclassification. J Clin Oncol. 2001;19:3045–50.
Gronchi A, Lo Vullo S, Colombo C, Collini P, Stacchiotti S, Mariani L, et al. Extremity soft tissue sarcoma in a series of patients treated at a single institution: local control directly impacts survival. Ann Surg. 2010;251:506–11.
ESMO/European Sarcoma Network Working Group. Soft tissue and visceral sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014. doi:10.1093/annonc/mdu254.
Waters B, Panicek DM, Lefkowitz RA, Antonescu CR, Healey JH, Athanasian EA, et al. Low-grade myxo-fibrosarcoma: CT and MRI patterns in recurrent disease. Am J Roentgenol. 2007;188:W193–8.
Manoso MW, Pratt J, Healey JH, Boland PJ, Athanasian EA. Infiltrative MRI pattern and incomplete initial surgery compromise local control of myxofibrosarcoma. Clin Orthop. 2006;450:89–94.
Huang HY, Lal P, Qin J, Brennan MF, Antonescu CR. Low-grade myxofibrosarcoma: a clinicopathologic analysis of 49 cases treated at a single institution with simultaneous assessment of the efficacy of 3-tier and 4-tier grading systems. Hum Pathol. 2004;35:612–21.
Haglund KE, Raut CP, Nascimento AF, Wang Q, George S, Baldini EH. Recurrence patterns and survival for patients with intermediate and high grade myxofibrosarcoma. Int J Radiat Oncol Biol Phys. 2010;82:361–7.
Fukunaga N, Fukunaga M. Low grade myxofibrosarcoma: progression in recurrence. Pathol Int. 1997;47:161–5.
Look Hong NJ, Hornicek FJ, Raskin KA, Yoon SS, Szymonifka J, Yeap B, et al. Prognostic factors and outcomes of patients with myxofibrosarcoma. Ann Surg Oncol. 2013;20(1):80–6.
Grosso F, Jones RL, Demetri GD, Judson IR, Blay JY, Le Cesne A, et al. Efficacy of trabectedin (ecteinascidin-743) in advanced pretreated myxoid liposarcomas: a retrospective study. Lancet Oncol. 2007;8(7):595–602.
Roland CL, Wang WL, Lazar AJ, Torres KE. Myxofibrosarcoma. Surg Oncol Clin N Am. 2016;25(4):775–88.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–6.
Kaplan WE, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81.
Judson I, Verweij J, Gelderblom H, Hartmann JT, Schöffski P, Blay JY, et al. Doxorubicin alone versus intensified doxorubicin plus ifosfamide for first-line treatment of advanced or metastatic soft-tissue sarcoma: a randomised controlled phase 3 trial. Lancet Oncol. 2014;15(4):415–23.
Sanfilippo R, Bertulli R, Marrari A, Fumagalli E, Pilotti S, Morosi C, et al. High-dose continuous-infusion ifosfamide in advanced well-differentiated/dedifferentiated liposarcoma. Clin Sarcoma Res. 2014;4(1):16.
Le Cesne A, Antoine E, Spielmann M, Le Chevalier T, Brain E, Toussaint C, et al. High-dose ifosfamide: circumvention of resistance to standard-dose ifosfamide in advanced soft tissue sarcomas. J Clin Oncol. 1995;13:1600–8.
Tascilar M, Loos WJ, Seynaeve C, Verweij J, Sleijfer S. The pharmacologic basis of ifosfamide use in adult patients with advanced soft tissue sarcomas. Oncologist. 2007;12:1351–60.
Rosen G, Forscher C, Lowenbraun S, Eilber F, Eckardt J, Holmes C, et al. Synovial sarcoma. Uniform response of metastases to high dose ifosfamide. Cancer. 1994;73:2506–11.
De Pas T, De Braud F, Orlando L, Nolè F, Munzone E, Zampino MG, et al. High-dose ifosfamide plus adriamycin in the treatment of adult advanced soft tissue sarcomas: is it feasible? Ann Oncol. 1998;9:917–9.
Palumbo R, Palmeri S, Antimi M, Gatti C, Raffo P, Villani G, et al. Phase II study of continuous-infusion high-dose ifosfamide in advanced and/or metastatic pretreated soft tissue sarcomas. Ann Oncol. 1997;8:1159–62.
Ratan R, Patel SR. Chemotherapy for soft tissue sarcoma. Cancer. 2016;122(19):2952–60.
Casali PG. Histology- and non-histology-driven therapy for treatment of soft tissue sarcomas. Ann Oncol. 2012;23(Suppl 10):167–9.
Authors’ contributions
VC and MF compiled the clinical data, reviewed the literature and drafted the manuscript. CM provided radiological data. MB and APDT provided the pathologic data. RS and PGC offered conceptual advice, reviewed and edited the manuscript. EF, AG and SP compiled the clinical data, offered conceptual advice, guided the composition process, reviewed and edited the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Consent for publication
Written informed consent was obtained from the patients for publication of this research and any accompanying images.
Ethics approval and consent to participate
This retrospective analysis was approved by the Institutional Ethics Committee of our Institution.
Funding
None declared.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Colia, V., Fiore, M., Provenzano, S. et al. Activity of anthracycline- and ifosfamide-based chemotherapy in a series of patients affected by advanced myxofibrosarcoma. Clin Sarcoma Res 7, 16 (2017). https://doi.org/10.1186/s13569-017-0082-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13569-017-0082-6